Abstract
Introduction
The patella is a sesamoid for the quadriceps, which increases its power during knee extension and thus transfers considerable forces. The etiology of patellofemoral pain is multifactorial. In the absence of injury, the commonly accepted hypothesis is associated with increased compression of articulating surfaces.
Aim
The aim of the study was to perform an ultrasound evaluation of the thickness of articular cartilage covering the medial and lateral femoral condyle in patients with an increased Q-angle.
Materials and methods
The study included 26 women aged between 35 and 45 years. A total of 13 patients with Q >15° were included in the study group, and 13 patients with Q ≤15° were included in the control group. A goniometer was used for Q-angle measurement. The thickness of articular cartilage covering the medial and lateral femoral condyle of the femoral bone was measured using a HONDA HS-2200 ultrasound with a linear HLS-584M transducer. The Shapiro–Wilk test was used for the assessment of data distribution normality; the distribution was normal. The differences in the measured parameters were assessed with the ANOVA test for independent samples. The Bonferroni test was used for a multiple comparison.
Results
The statistical analysis showed statistically significantly reduced thickness of articular cartilage on the lateral femoral condyle (p = 0.00) in the Q >15° group. No statistically significant differences were demonstrated for the thickness of articular cartilage on the medial femoral condyle (p = 0.47).
Conclusions
The thickness of the articular cartilage on the lateral femoral condyle is lower than that of the medial femoral condyle in women aged between 35 and 45 years with the Q-angle >15°.
Keywords: cartilage, Q-angle, patellofemoral joint
Introduction
The knee is considered to be one of the largest and most anatomically complex joints in the human body. Therefore, it is predisposed to multiple injuries and overloads. Knee injuries are usually associated with sports, while knee overload is mainly due to work-related activities and obesity(1). Patellofemoral pain, which, according to studies, is more common among physically active individuals, is one of the clinical problems related to the knee(2). Women are more susceptible to overload in this anatomical region(3).
The etiology of patellofemoral pain is multifactorial. Injuries and damage to knee structures are obvious determinants. However, in the absence of injury, the commonly accepted hypothesis is associated with increased compression of articulating patellar and femoral surfaces, and, consequently, premature wear of the articular cartilage(4–8). The patella is a sesamoid for the quadriceps, increasing its power during knee extension(9). This results in considerable forces being transferred through the patella, from one-half of body weight during walk up(10) to 7 times body weight during squatting(11). The direction of the force produced by the quadriceps muscle in the knee is referred to as the Q-angle. It is formed by a line drawn from the anterior superior iliac spine (ASIS) to the center of the patella and a line from the center of the patella to the tibial tubercle(12). A Q-angle >15–20° is considered to be the cause of knee-extensor apparatus dysfunction and patellofemoral pain(13). Some authors also point to an increased risk of patellar chondromalacia(14) as well as patellar dislocation and subluxation(15).
The aim of the study was to perform an ultrasound evaluation of the thickness of articular cartilage covering the medial and lateral femoral condyle in patients with an increased Q-angle.
Materials and methods
Participants
A total of 31 women aged between 35 and 45 years volunteered for the study. The volunteers experienced no knee pain during the study. A total of 26 women were enrolled in the study (mean age ± SD: 41 ± 3.7 years). A total of 13 patients with Q >15° (mean ± SD: 23.6°± 3) were included in the study group, and 13 patients with Q ≤15° (mean ± SD: 11.6° ± 1.5) were included in the control group. Exclusion criteria were as follows: a history of knee injury, knee surgery or knee pain during the last 4 weeks.
All volunteers were informed about the purpose of the research and gave voluntary informed consent to participate in the study. The study was approved by the Bioethics Committee of the University of Physical Education in Wroclaw and conducted in accordance with the 1975 Helsinki Declaration.
Measurements
A goniometer was used for Q-angle measurements. The measurements were performed in a supine position with an extended knee and fully relaxed quadriceps muscle. A washable marker was used to mark landmarks for the goniometer: the anterior superior iliac spine (ASIS), the center of the patella and the tibial tubercle. The examined limb was positioned perpendicular to the bed surface on which the volunteers were lying (the line passing through the center of the heel and the second finger was perpendicular to the plane of the table). The measurements were performed for both limbs.
HONDA HS-2200 with 6.0/8.5/11.00 MHz HLS-584M transducer (Honda, Japan) was used for the measurement of articular cartilage covering the medial and lateral femoral condyle. The knee was positioned in the maximum flexion. The transducer was applied transversely just above the patella, perpendicular to the surface of the femoral condyles. The obtained images were used to measure the thickness of homogeneous low echoic or anechoic cartilaginous structure using ultrasound software (Fig. 1). Good repeatability of the measurement of the articular cartilage covering the lateral and medial femoral condyle was shown(16). Both limbs were evaluated by the same operator.
Fig. 1.
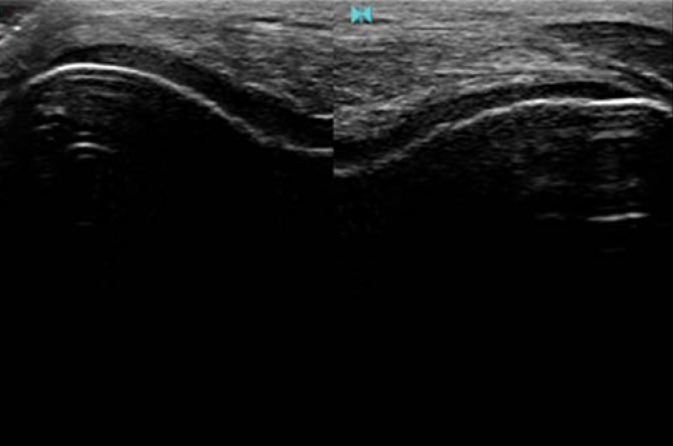
An ultrasound scan showing an articular cartilage layer covering the femoral condyle
Statistical analysis
STATISTICA 13.1 was used for statistical analysis. The Shapiro–Wilk test was used for the assessment of data distribution normality; the distribution was normal. The differences in the measured parameters were assessed with the ANOVA test for independent samples. The Bonferroni test was used for multiple comparison of cartilage thickness for both condyles. The differences between the assessed parameters were considered significant at p < 0.05.
Results
The obtained results for the thickness of the surface cartilage of the medial femoral condyle (MFC) and the lateral femoral condyle (LFC) in both groups are shown in Table 1. The mean cartilage thickness (+SD) is shown in Table 2.
Tab. 1.
The thickness of the articular cartilage covering the femoral condyle in patients
| Patients | Articular cartilage thickness [mm] | |||||||
|---|---|---|---|---|---|---|---|---|
| Q >15° | Q ≤15° | |||||||
| LFC | MFC | LFC | MFC | |||||
| LLL | RLL | LLL | RLL | LLL | RLL | LLL | RLL | |
| 1 | RLL | 1.40 | 1.60 | 1.61 | 1.72 | 1.73 | 1.67 | 1.72 |
| 2 | LLL | 1.70 | 2.14 | 2.13 | 1.97 | 2.05 | 1.95 | 2.01 |
| 3 | RLL | 1.07 | 1.64 | 1.70 | 2.33 | 2.49 | 2.37 | 2.41 |
| 4 | LLL | 2.16 | 2.39 | 2.49 | 1.94 | 1.90 | 2.00 | 1.86 |
| 5 | RLL | 1.52 | 1.76 | 2.26 | 1.64 | 1.62 | 1.64 | 1.60 |
| 6 | LLL | 1.71 | 2.04 | 2.13 | 2.44 | 2.38 | 2.41 | 2.36 |
| 7 | RLL | 1.55 | 1.83 | 2.96 | 2.27 | 2.22 | 2.30 | 2.16 |
| 8 | 1.56 | 1.45 | 2.25 | 2.64 | 2.58 | 2.55 | 2.55 | 2.60 |
| 9 | 1.67 | 1.67 | 2.14 | 2.21 | 1.90 | 1.98 | 1.86 | 1.92 |
| 10 | 1.44 | 1.56 | 2.24 | 2.01 | 1.70 | 1.67 | 1.72 | 1.70 |
| 11 | 1.85 | 2.04 | 2.01 | 2.36 | 2.29 | 2.26 | 2.30 | 2.25 |
| 12 | 1.64 | 1.32 | 2.25 | 2.01 | 2.03 | 2.37 | 1.97 | 2.41 |
| 13 | 1.56 | 1.55 | 2.24 | 2.60 | 2.10 | 2.05 | 2.12 | 2.10 |
LFC – lateral femoral condyle
MFC – medial femoral condyle
LLL – left lower limb
RLL – right lower limb
Tab. 2.
The thickness of the articular cartilage covering the condyles in the Q >15° and Q >15° groups
| Condyle | Articular cartilage thickness [mm] (mean ± SD) | |
|---|---|---|
| Q>15° (n = 13) | Q≤15° (n = 13) | |
| LFC | 1.58 ± 0.25 | 2.08 ± 0.30 |
| MFC | 2.14 ± 0.33 | 2.07 ± 0.30 |
LFC – lateral femoral condyle
MFC – medial femoral condyle
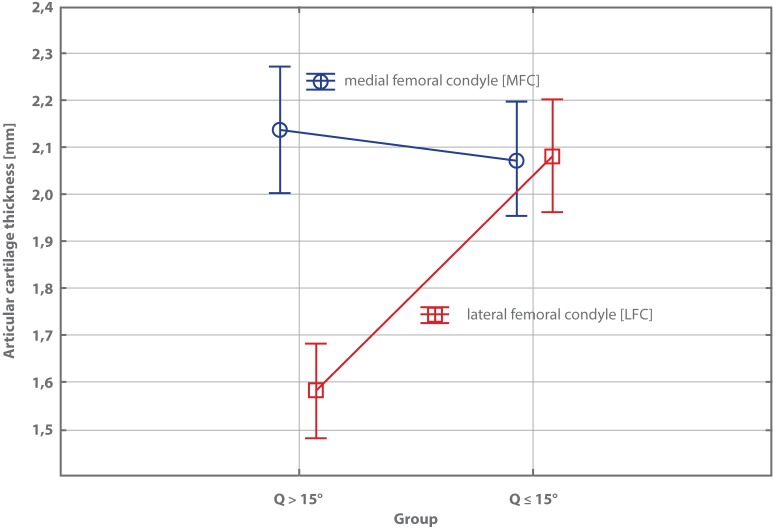
The statistical analysis showed statistically significantly reduced thickness of LFC articular cartilage (p = 0.00) in the Q >15° group. No statistically significant differences were demonstrated for the thickness of MFC articular cartilage (p = 0.47) (Fig. 2).
Fig. 2.
A relationship between the thickness of condyle articular cartilage and the Q-angle
Discussion
Ultrasonography has become a widely used imaging modality for the assessment of the musculoskeletal system due to its easy availability, short scan time and low costs. Recent technological improvements have rendered the technique increasingly precise and widely used in a number of clinical indications. Ultrasound allows for a good visualization of knee structures such as muscles, ligaments, periarticular tissues and fluid cisterns(17–19). It should be noted that magnetic resonance imaging is the method of choice for the meniscus, anterior cruciate ligament, bone marrow or articular surfaces inside the joint(20–24). However, femoral cartilage defects or thinning may be visualized and detected using ultrasonography(25,26).
Our findings indicate statistically significantly reduced thickness of LFC articular cartilage in women with an increased Q-angle. This may be due to increased compression imposed by the patellar cartilage on this condyle. The patellar movement in the patellofemoral joint has been widely described in different studies. Most of these studies indicate that the patella moves laterally and rotates medially during knee flexion(26–28). Interesting findings were presented by Mizuna et al.(27) An increase in the Q-angle in an in vitro setting led to lateral patellar movement and, consequently, increased patellar compression on the lateral condyle. A decrease in the Q-angle resulted not only in medial patellar shift, but also increased medial compression. Our findings extend this knowledge, pointing to structural changes in the patellofemoral joint in women with an increased Q-angle in an in vivo setting.
Limitations
A small sample size was one of the limitations hindering clinical inference in the presented work. The number of patients should be higher in future research devoted to this issue. Furthermore, the Q-angle and patellar position within the joint also depend on other factors, such as the antetorsion of the femur, pelvic width and other anthropometric measurements, patellar tendon tension or knee ligament tension. All these factors should be considered in order to increase the clinical value of further studies.
Conclusions
The thickness of the articular cartilage on the lateral femoral condyle is lower than that of the medial femoral condyle in women aged between 35 and 45 years with the Q-angle >15°.
Footnotes
Conflict of interest
Authors do not report any financial or personal connections with other persons or organizations, which might negatively affect the contents of this publication and/or claim authorship rights to this publication.
References
- 1.Gomes-Neto M, Araujo AD, Junqueira ID, Oliveira D, Brasileiro A, Arcanjo FL: Comparative study of functional capacity and quality of life among obese and non-obese elderly people with knee osteoarthritis. Rev Bras Reumatol Engl Ed 2016; 56: 126–130. [DOI] [PubMed] [Google Scholar]
- 2.Devereaux MD, Lachmann SM: Patello-femoral arthralgia in athletes attending a Sports Injury Clinic. Br J Sports Med 1984; 18: 18–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A: Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports 2010; 20: 725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fulkerson JP, Shea KP: Mechanical basis for patellofemoral pain and cartilage breakdown In: Ewing JW. (ed.): Articular Cartilage and Knee Joint Function: Basic Science and Arthroscopy. Raven Press, New York: 1990: 93–101. [Google Scholar]
- 5.Heino Brechter J, Powers CM: Patellofemoral stress during walking in persons with and without patellofemoral pain. Med Sci Sports Exerc 2002; 34: 1582–1593. [DOI] [PubMed] [Google Scholar]
- 6.Herzog W, Diet S, Suter E, Mayzus P, Leonard TR, Müller C. et al. : Material and functional properties of articular cartilage and patellofemoral contact mechanics in an experimental model of osteoarthritis. J Biomech 1998; 31: 1137–1145. [DOI] [PubMed] [Google Scholar]
- 7.Møller BN, Møller-Larsen F, Frich LH: Chondromalacia induced by patellar subluxation in the rabbit. Acta Orthop Scand 1989; 60: 188–191. [DOI] [PubMed] [Google Scholar]
- 8.Sanchis-Alfonso V, Rosello-Sastre E, Martinez-Sanjuan V: Pathogenesis of anterior knee pain syndrome and functional patellofemoral instability in the active young. Am J Knee Surg 1999; 12: 29–40. [PubMed] [Google Scholar]
- 9.Yamaguchi GT, Zajac FE: A planar model of the knee joint to characterize the knee extensor mechanism. J Biomech 1989; 22: 1–10. [DOI] [PubMed] [Google Scholar]
- 10.Reilly DT, Martens M: Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Orthop Scand 1972; 43: 126–137. [DOI] [PubMed] [Google Scholar]
- 11.Mason JJ, Leszko F, Johnson T, Komistek RD: Patellofemoral joint forces. J Biomech 2008; 41: 2337–2348. [DOI] [PubMed] [Google Scholar]
- 12.Hungerford DS, Barry M: Biomechanics of the patellofemoral joint. Clin Orthop Relat Res 1979; 144: 9–15. [PubMed] [Google Scholar]
- 13.Guerra JP, Arnold MJ, Gajdosik RL: Q angle: Effects of isometric quadriceps contraction and body position. J Orthop Sports Phys Ther 1994; 19: 200–204. [DOI] [PubMed] [Google Scholar]
- 14.Papageopoulos PI, Sim FH: Patellofemoralpain syndrome: Diagnosis and management. Orthopedics 1997; 20: 148–157. [DOI] [PubMed] [Google Scholar]
- 15.Barberie JE, Wong AD, Cooperberg PL, Carson WB: Extended field-of-view sonography in musculoskeletal disorders. AJR Am J Roentgenol 1998; 171: 751–757. [DOI] [PubMed] [Google Scholar]
- 16.Naredo E, Acebes C, Möller I, Canillas F, de Agustín JJ, de Miguel E. et al. : Ultrasound validity in the measurement of knee cartilage thickness. Ann Rheum Dis 2009; 68: 1322–1327. [DOI] [PubMed] [Google Scholar]
- 17.Newman JS, Adler RS, Bude RO, Rubin JM: Detection of soft-tissue hiperemia: Value of power Doppler sonography. AJR Am J Roentgenol 1994; 163: 385–389. [DOI] [PubMed] [Google Scholar]
- 18.Gibbon WW, Wakefield RJ: Ultrasound in inflammatory disease. Radiol Clin North Am 1999; 37: 633–651. [DOI] [PubMed] [Google Scholar]
- 19.Grobbelaar N, Bouffard JA: Sonography of the knee: A pictorial review. Semin Ultrasound CT MR 2000; 21: 231–274. [DOI] [PubMed] [Google Scholar]
- 20.Ptasznik R: Ultrasound in acute and chronic knee injury. Radiol Clin North Am 1999; 37: 797–830. [DOI] [PubMed] [Google Scholar]
- 21.Bouffard JA, Dhanju J: Ultrasonography of the knee. Semin Musculoskeletal Radiol 1998; 2: 245–270. [DOI] [PubMed] [Google Scholar]
- 22.Friedman L, Finlay K, Jurriaans E: Ultrasound of the knee. Skeletal Radiol 2001; 30: 361–377. [DOI] [PubMed] [Google Scholar]
- 23.Strome GM, Bouffard JA, van Holsbeeck M: Knee. Clin Diagn Ultrasound 1995; 30: 201–219. [PubMed] [Google Scholar]
- 24.Ahnied AM, Duncan NA, Tanzer M: In vitro measurement of the tracking pattern of the human patella. J Bioniech Eng 1999; 121: 222–228. [DOI] [PubMed] [Google Scholar]
- 25.Hsieh YF, Draganich LF, Ho SH, Reider B: The effects of removal and reconstruction of the anterior cruciate ligament on patellofemoral kinematics. Am J Sports Med 1998; 26: 201–208. [DOI] [PubMed] [Google Scholar]
- 26.Hsu HC, Luo ZP, Rand JA, An KN: Influence of patellar thickness on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthrop 1996: 11: 69–80. [DOI] [PubMed] [Google Scholar]
- 27.Mizuno Y, Kumagai M, Mattessich SM, Elias JJ, Ramrattan N, Cosgarea AJ. et al. : Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res 2001; 19: 834–840. [DOI] [PubMed] [Google Scholar]
- 28.Katchburian MV, Bull A, Shih YF, Heatley FW, Amis AA: Measurement of patellar tracking: Assessment and analysis of the literature. Clin Orthop Relat Res 2003; (412): 241–259. [DOI] [PubMed] [Google Scholar]