Abstract
Aim
Respiratory syncytial virus is the main pathogen responsible for bronchiolitis. Usually, there is no indication to perform diagnostic imaging or run laboratory tests in patients with bronchiolitis since the diagnosis is based on the clinical presentation. Chest radiogram can be useful in severe cases. So far, lung ultrasound has not been considered as an alternative in guidelines for imaging diagnosis of bronchiolitis. The aim of the study was to compare lung ultrasound and chest X-ray findings in children with bronchiolitis.
Material and methods
In our study we retrospectively compared diagnostic imaging findings in children with confirmed respiratory syncytial virus infection. The study included 23 children aged 2 weeks to 24 months and 3 children older than 24 months.
Results
Chest X-ray showed lesions in only 4 cases, whereas ultrasound abnormalities were found in 21 patients. Pathologies revealed by chest X-ray were the same for all 4 cases and consisted of an enlarged hilus and peribronchial cuffing. Sonographic lesions included inflammatory consolidations larger than 10 mm in 11 patients, small consolidations (<10 mm diameter) in 8 patients, interstitial syndromes in 6 patients, and alveolar-interstitial syndromes in 11 patients. A small amount of pleural effusion was detected in 3 patients.
Conclusions
Considering safety, short time of examination, high sensitivity in finding pleural effusion, small consolidations and signs of interstitial infiltrations, transthoracic lung ultrasound may be useful in the diagnosis of bronchiolitis.
Keywords: bronchiolitis, lung ultrasound, respiratory syncytial virus, chest X-ray
Introduction
Bronchiolitis is the most common cause of pediatric hospital admissions within the first six months of life and accounts for 20% of hospital admissions in infants(1).
Respiratory syncytial virus (RSV) is the main pathogen responsible for this type of infection. It belongs to the family Paramyxoviridae, genus Pneumovirus. It is the main pathogenic factor of upper respiratory tract infections in older children and lower respiratory tract infections in infants(1). Over 90% of children aged up to 2 years become infected, with 30% of these patients developing bronchiolitis and/or pneumonia(2). The peak incidence is observed in late autumn and early spring. The symptoms of bronchiolitis include dry cough, wheezing, dyspnea, and, in severe cases, cyanosis and apnea(1).
Laboratory and imaging studies are not indicated in children with mild bronchiolitis, who can be managed in an outpatient setting. Testing for the RS virus is justified in in-patients for epidemiological reasons. Available virology tests include rapid antigen detection, specific antibody titer, and PCR (polymerase chain reaction). Rapid tests detecting RSV antigen are characterized by both high specificity and sensitivity (about 80–90%)(1). Detecting RSV antigen may result in a lower frequency of antibiotic use in this disease.
Chest X-ray (CXR) should not be routinely performed in children with bronchiolitis; however it is indicated if there is any doubt regarding the diagnosis, in the case of persistent symptoms and severe clinical course. Nonetheless, the CXR usually does not allow to differentiate between bronchiolitis and other respiratory tract infections, and the results do not correlate with the severity of the disease(1). Despite the fact that transthoracic lung ultrasound (TLU) is increasingly popular in lung and pleural imaging, it has not been included in the guidelines on managing bronchiolitis(3–7). The aim of our study was to compare the results of lung ultrasound and chest X-ray in children with RSV infection and clinical diagnosis of bronchiolitis requiring hospital stay.
Methodology
Patients aged 0 to 24 months with symptoms of acute bronchiolitis were enrolled in the study. As a separate specific group, we also included three children over the age of 2 years who were also diagnosed with bronchiolitis based on clinical presentation and low inflammatory marker levels. All patients were hospitalized in the Department of Pediatric Infectious Diseases and Pediatric Hepatology, and the Department of Pediatric Neuroinfections and Neurology of John Paul II Specialty Hospital in Cracow. In all cases, the RSV infection was confirmed using the CerTest RSV+ Adenovirus Resp kit.
RSV tests were conducted as a part of the standard diagnostic process in children presenting with the symptoms of bronchiolitis. Lung ultrasound is a routine examination in our hospital and was performed for the patient’s best interest. A total of 26 patients in whom chest X-ray was performed due to their poor general condition were included in the study group. Transthoracic lung ultrasound (TLU) was performed within 24 hours since the radiogram was obtained. The comparison of TLU and CXR was performed retrospectively, after the patients were discharged from hospital; therefore it had no effects on the treatment.
RSV infection was confirmed based on nasopharyngeal swab. The specimen was used in a rapid immunochromatographic testing for RSV and adenovirus (CerTest RSV + Adenovirus Resp.). The test is characterized by 95% sensitivity and >99% specificity (compared to BinaxNow RSV-test).
In ambiguous cases or other epidemiological indications, further laboratory tests were conducted depending on the symptoms (rapid testing for influenza, serological tests for M. pneumoniae, PCR to detect antigens of Bordetella pertussis, Bordetella parapertussis, Mycoplasma pneumoniae, Chlamydophila pneumoniae).
All chest radiograms were interpreted by a radiologist with 25 years of experience, not engaged in the therapeutic process and employed in an independent pediatric pulmonology center. The patients’ personal and clinical data were confidential.
Ultrasound examinations were conducted by the same clinician using the Mindray DC-8 Expert with a linear 3–10 MHz transducer. Longitudinal and transverse scans of the anterior, lateral and posterior chest wall were obtained. Each time, pleural effusion was assessed in a vertical position.
In order to facilitate the analysis, ultrasound findings were classified according to V. Basile:(8)
-
1)
small subpleural consolidations < 10 mm in diameter;
-
2)
consolidations > 10 mm in diameter with air bronchogram;
-
3)
interstitial syndrome –B7 lines;
-
4)
alveolar-interstitial syndrome –B3 lines;
-
5)
pleural effusion.
Chest X-ray abnormalities were classified as follows:
-
1)
inflammatory infiltrate;
-
2)
hilar enlargement;
-
3)
peribronchial cuffing;
-
4)
pleural effusion;
-
5)
lung hyperexpansion.
Subpleural consolidations indicate focal lesions in lung tissue adjacent to the pleura. The structure and echogenicity of these lesions is similar to the liver tissue. Such changes can be caused by e.g. inflammatory infiltrate, atelectasis or pulmonary embolism.
Interstitial syndromes are characterized by an increased number of B lines, the so-called B7 lines where B lines are about 7 mm apart from each other and usually less than 7 mm. They can be observed in the initial phase of pulmonary edema, interstitial pneumonia and pulmonary fibrosis, and are as such non-specific. In contrast, alveolar-interstitial syndromes are characterized by numerous B lines at a distance of about 3 mm – B3 lines. They indicate the presence of fluid in the alveoli, e.g. respiratory distress or fluid overload / lung hemorrhage, and pulmonary fibrosis – again as such per se non-specific.
Results
In our study, the final diagnosis was based on positive tests for RSV and characteristic clinical manifestations.
The study included 23 children aged up to 2 years, with the oldest one being 24-month-old. Due to distinctive clinical image, the diagnosis was also set in 3 children older than 2 years; they were considered a separate group (marked yellow on diagrams). The youngest of infants was 2 weeks old, the mean age was 7.3 months, median of 7 months, mode of 2 months.
The average length of hospital stay was 9 days. The tests were run on day 2 to 15 since the onset of infection (on day 5 on average), depending on the time of admission to the hospital.
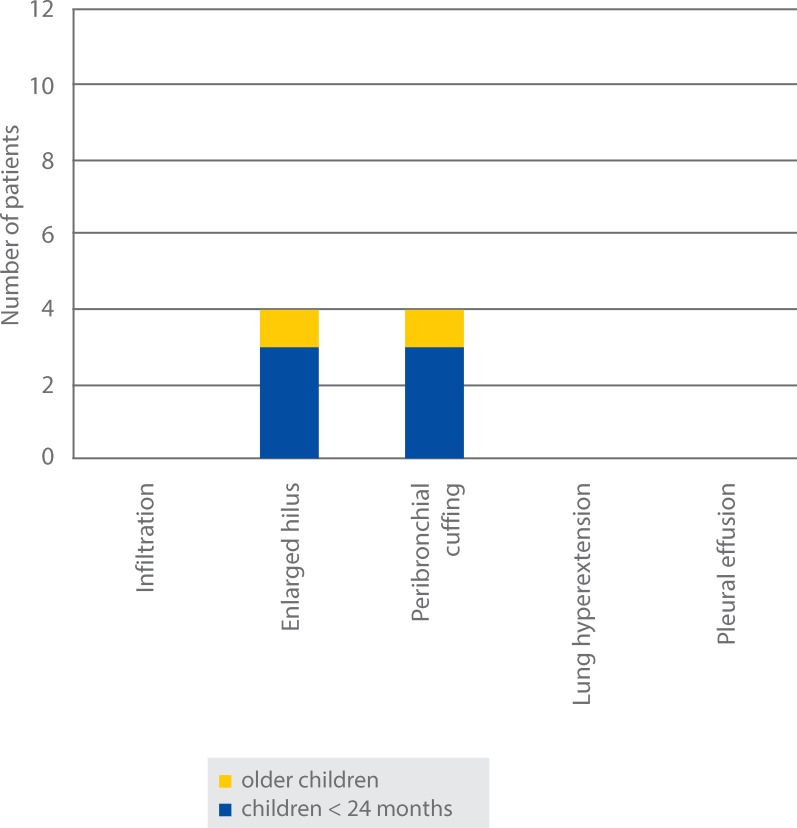
In the study we analyzed ultrasound and chest X-ray results. Inflammatory lesions in chest radiograms were observed only in 4 (15.3%) cases. These consisted of peribronchial cuffing and hilar enlargement. The lesions were located near the right hilum in three patients, and in the left lower zone in two children. CXRs revealed no inflammatory infiltrate, hyperextension or pleural effusion (Fig. 1).
Fig. 1.
Number of patients with CXR abnormalities
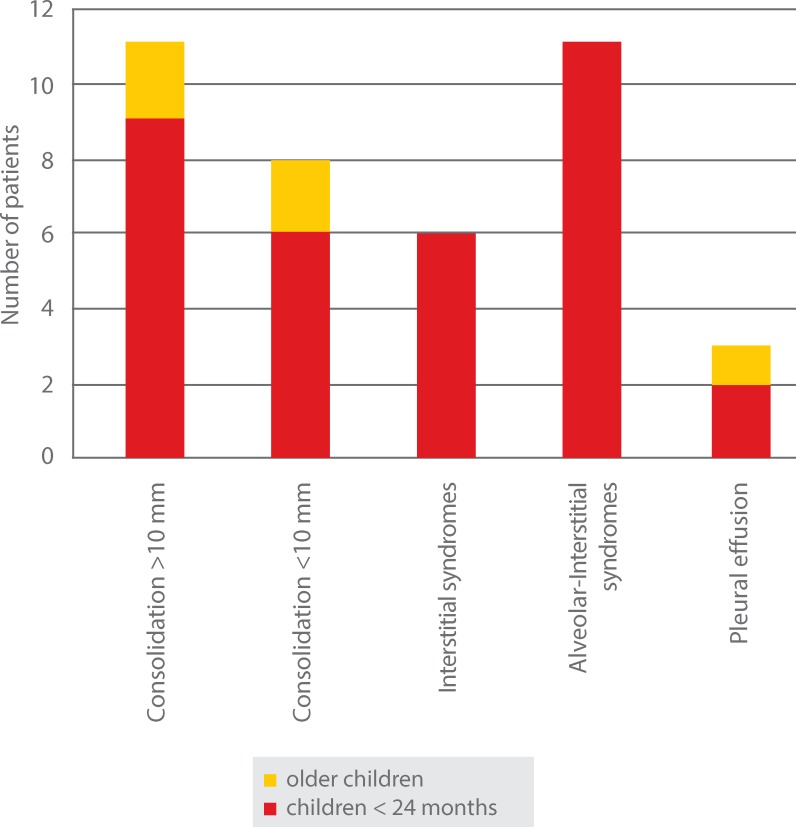
Ultrasound abnormalities were found in 18 patients and consisted of (Fig. 2):
Fig. 2.
Number of patients with lung ultrasound abnormalities
-
1)
inflammatory consolidations > 10 mm in 11/26 (42.3%) patients;
-
2)
small consolidations < 10 mm in 8/26 (30.7%) patients;
-
3)
interstitial syndromes in 6/26 (23%) patients;
-
4)
alveolar-interstitial syndromes in 11/26 (42.3%) patients;
-
5)
small amount of pleural effusion in 3/26 (11.5) patients.
No chest ultrasound abnormalities were found in five children. Also, these patients showed no abnormalities in chest X-ray.
The most prevalent ultrasound abnormalities were alveolar-interstitial syndromes (in 11 patients, including 2 children over 24 months of age), as well as medium-sized subpleural consolidations with air bronchogram with maximal diameter of 30 mm (also found in 11 patients). Small consolidations < 10 mm in diameter (in 8 patients) and interstitial syndromes (in 6 cases) were often observed. A small amount of pleural effusion was revealed in three patients.
Consolidations were more common in inferior and posterior portions of lungs, with similar rates in the right (8/26, 30.7%) and left lung (7/26, 26.9%). Interstitial and alveolar-interstitial syndromes were most frequently observed in inferior and posterior, as well as paraspinal portions of the lungs (Fig. 3).
Fig. 3.
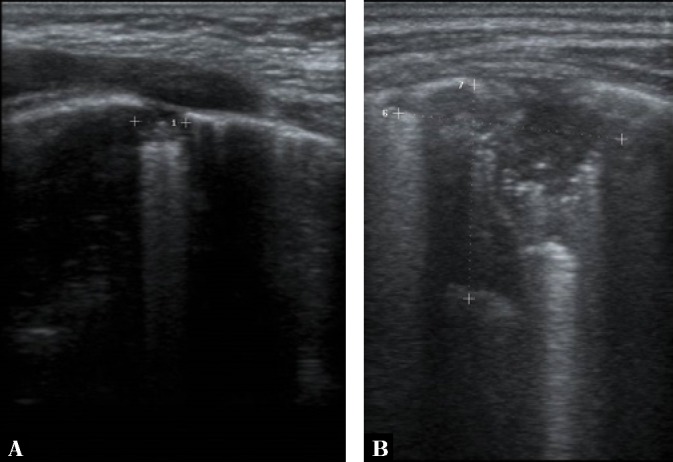
Subpleural consolidations in lung ultrasound
Discussion
RSV infections are a vital problem in pediatrics. A growing number of publications suggesting the possible use of TLU in the diagnosis of bronchiolitis call for updating clinical guidelines.
In our study, the classification of ultrasound abnormalities was based on the one presented in the study by V. Basile et al. Similar to V. Basile, we observed a higher rate of lesions (both consolidations and alveolar-interstitial syndromes) in inferior, posterior and paraspinal portions of lungs. The predominance in these spaces may be explained by gravity and supine / sitting positions of an infant.
The conclusions from the study by V.A. Caiulo et al.(8) correspond to our results. We showed higher sensitivity of ultrasound compared to CXR in detecting small amounts of pleural effusion (0 in CRX vs 3 in TLU) or lesions within the pulmonary parenchyma (a total of 11 large and 8 small consolidations in TLU vs 0 infiltrations in CRX). The most common lung ultrasound abnormalities observed by Caiulo were subpleural consolidations, mainly on anterior and lateral scans. In our study, subpleural consolidations were also common, but the localization of these lesions was different.
In our study, similar to V.A. Caiulo, we chose the model of all ultrasound examinations performed by one trained operator, which made the comparison of results easier. A different approach was chosen by V. Basile who analyzed the results of examinations performed by various operators, resulting in greater universality of his results.
Other researchers investigated the correlation between severity of clinical condition and the extent of ultrasound abnormalities. There are reports on more severe course of the disease in children with > 10 mm subpleural consolidations(9). However, a similar relationship was not established for pleural effusions(10). This aspect was impossible to analyze in our study due to the study design and therefore was omitted.
We are aware of the limitations resulting from the preconceived criteria of our study. Due to the small number of patients enrolled in our study the clear description of sonographic lesions specific for bronchiolitis was not possible. Moreover, some of the pathological findings could not be equally visualized using both analyzed methods. CXR has an advantage in showing hilar regions, which cannot be visualized in TLU, and lung hyperinflation, difficult to evaluate with lung ultrasound.
On the other hand, TLU is more sensitive in finding pleural fluid and subpleural consolidations(4). Therefore the direct comparison of specificity and sensitivity of both methods is not possible.
Following other authors, if we continued our research, we might consider other aspects of this issue. New conclusions could be drawn from the analysis of resolution of lesions in the course of treatment (requiring follow-up ultrasound every few days), as well as by comparing patients’ general condition with ultrasound image.
Conclusions
Our study confirmed that transthoracic lung ultrasound can be a reliable tool in the diagnosis of lung lesions caused by RSV infection. It allows to visualize lesions that are poorly or not visible on classic plain film chest radiograms. Also, when the lesions are present, TLU can be useful in treatment monitoring. Moreover, the safety of diagnostic methods for an infant is of utmost importance. Chest X-ray exposes the infant to ionizing radiation(11), which is a risk factor for developing cancer later in life (e.g. leukemia, lymphoma, brain tumors)(12). So far, no adverse effects of lung ultrasound have been described in humans.
Furthermore, transthoracic ultrasound can be performed directly in the emergency department equipped with an ultrasound machine. Such an approach – a point-of-care imaging test – is helpful in the diagnosis(13).
On the other hand, the majority of lesions described in TLU are non-specific for certain diseases. Therefore, similarly to other point-of-care examinations, the result of transthoracic lung ultrasound should be interpreted together with medical history, clinical condition and other diagnostic tests.
An important disadvantage of this method should also be noted: TLU cannot visualize profound structures in the chest cavity, including bronchi and hilar regions; therefore it is inconclusive in the diagnosis of obstruction, foreign body aspiration, lung cyst etc.; thus the use of TLU as the only diagnostic method involves the risk of overlooking other, underlying conditions.
Considering safety, short time of examination, high sensitivity in finding pleural effusion, small consolidations and signs of interstitial changes, transthoracic lung ultrasound may still be recommended as a potentially helpful tool in the diagnosis of bronchiolitis.
Footnotes
Conflict of interest
The authors do not report any financial or personal connections with other persons or organizations, which might negatively affect the contents of this publication and/or claim authorship rights to this publication.
References
- 1.Hryniewicz W, Albrecht P, Radzikowski A (eds.): Rekomendacje postępowania w pozaszpitalnych zakażeniach układu oddechowego. Narodowy Program Ochrony Antybiotyków 2016. Available from: http://www.antybiotyki.edu.pl.
- 2.American Academy of Pediatrics : Respiratory syncytial virus In: Kimberlin DW, Brady MT, Jackson MA, Long SS (eds.): Red Book: 2015 Report of the Committee on Infectious Diseases. American Academy of Pediatrics, Elk Grove Village, IL: 2015: 667–676. [Google Scholar]
- 3.Volpicelli G, Melniker LA, Cardinale L, Lamorte A, Frascisco MF: Lung ultrasound in diagnosing and monitoring pulmonary interstital fluid. Radiol Med 2013; 118: 196–205. [DOI] [PubMed] [Google Scholar]
- 4.Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein D, Mathis G, Kirkpatrick AW. et al. : International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 2012; 38: 577–591. [DOI] [PubMed] [Google Scholar]
- 5.Zanforlin A, Giannuzzi R, Nardini S, Testa A, Soldati G, Copetti R. et al. : The role of chest ultrasonography in the management of respiratory diseases: Document I. Multidiscip Respir Med 2013; 8: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Copetti R, Soldati G, Copetti P: Chest sonography: A useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 2008; 6: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O: The comet-tail artifact. An ultrasound sign of alveolar-intestitial syndrome. Am J Respir Crit Care Med 1997; 156: 1640–1646. [DOI] [PubMed] [Google Scholar]
- 8.Caiulo VA, Garagani L, Cailuno S, Fisicaro A, Moramarco F, Latini G. et al. : Lung ultrasound in bronchiolitis: Comparison with chest X-ray. Eur J Pediatr 2011; 170: 1427–1433. [DOI] [PubMed] [Google Scholar]
- 9.Basile V, Di Mauro A, Scalini E, Comes P, Lofù I, Mostert M. et al. : Lung ultrasound: A useful tool in diagnosis and management of bronchiolitis. BMC Pediatr 2015; 15: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yilmaz AE, Koktener A, Celik N, Akca H, Bilici M, Mete E: Frequency of pleural effusion in acute bronchiolitis and its effect on prognosis. Multidiscip Respir Med 2011; 6: 371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Research Council : Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. The National Academies Press, Washington, DC: 2006. Available from: 10.17226/11340. [DOI] [PubMed] [Google Scholar]
- 12.Shu XO, Jin F, Linet MS, Zheng W, Clemens J, Mills J. et al. : Diagnostic X-ray and ultrasound exposure and risk of childhood cancer. Br J Cancer 1994; 70: 531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xirouchaki N, Georgopoulos D: The use of lung ultrasound: A brief review for critical care physicians and pneumonologists. Pneumon 2007; 20: 134–141 [Google Scholar]