Abstract
This research examined how parenting adults with developmental disabilities affects parental well-being beyond midlife and into old age. Parents of adults with developmental disabilities (n = 249) and parents of adults without disabilities (n = 9,016), studied in their early 50s and mid-60s, were longitudinally tracked into their early 70s. Compared to parents of adults without disabilities, parents of adults with disabilities showed a pattern of normative functioning in their 50s, followed by poorer well-being in their mid-60s, and further declines in health and well-being into the early 70s. Aging parents who co-resided with their adult child with disabilities were particularly vulnerable, experiencing a steeper increase in depressive symptoms and body mass index (BMI) than parents whose child with disabilities lived away from home.
Keywords: aging parents, physical health, psychological well-being, co-residence
There is a large body of research on the effects on parents of providing care to children and adults with disabilities (e.g., Baker, Blacher, & Olsson, 2005; Ha, Hong, Seltzer, & Greenberg, 2008; Seltzer, Greenberg, Floyd, Pettee, & Hong, 2001; Smith, Seltzer, Tager-Flusberg, Greenberg, & Carter, 2008). Most of these studies have been cross-sectional, examining the effects on parents at a certain point in their life course, e.g., parenting a young child, an adolescent, or an adult with developmental disabilities. This research suggests that, overall, parents of children with developmental disabilities show a pattern of adaptation through middle-age, with comparable levels of depression, physical health, and social participation as their age peers in the general population (Baker et al., 2005, Seltzer et al., 2001), partly by exercising effective coping strategies (Smith et al., 2008). However, during their mid-60s, these parents showed a decline in health (Magana & Smith, 2006) and psychological well-being (Seltzer, Floyd, Song, Greenberg, & Hong, 2011).
Unlike cross-sectional approaches, longitudinal models capture within-subject variation as a separate factor, and therefore, reduce the error for detecting between-group effects. They also allow us to identify individual trajectories of change over time and predictors of variation in life course outcomes. Thus, longitudinal analysis is both more sensitive to change and more informative about individual variation (Menard, 2008). Specifically, longitudinal models allow us to test alternative hypotheses about the effect of parenting an adult with developmental disabilities over the parents’ life course. A cumulative stress process hypothesizes that the wear and tear of caregiving stress accumulates over time, leading to an increased vulnerability in the caregivers’ health and well-being later in life (Pearlin, Schieman, Fazio, & Meersman, 2005). On the other hand, an adaptation process suggests that parents adjust to the stress of their child’s disability, with parents showing a pattern of resiliency to the stress of caregiving as they age (Lazarus & Folkman, 1984).
Our research used data collected as part of the Wisconsin Longitudinal Study (WLS), a longitudinal survey following a randomly selected cohort who graduated from high school in 1957, and a randomly selected sibling. The results suggest that the cumulative effects of lifelong caregiving for adult children with developmental disabilities begin to become evident when parents are in their mid-60s (Seltzer et al., 2011). With the collection of an additional wave of data in the WLS, we are now in a position to examine these effects when parents are in their early 70s. Using growth curve modeling, the present study examined whether parents of adults with developmental disabilities experienced a more rapid age-related decline in their health and well-being from their early 50s to their early 70s, relative to their age peers whose adult children do not have disabilities.
Stress of Caregiving for Adult Children With Developmental Disabilities in Later Life
Some cross-sectional studies report greater vulnerability in physical health among older than midlife parents of children with developmental disabilities, suggesting a cumulative stress process. For example, using a sample of Latina and Black mothers from the National Health Interview Survey, Magana and Smith (2006) found that older mothers (aged 55 or older), who lived with a grown child with developmental disabilities, had a greater likelihood of heart problems, arthritis, and diabetes than older non-caregiving mothers. However, maternal caregivers in midlife (ages 50 to 54), did not differ in health outcomes from their age peers without such caregiving responsibilities. In contrast, other studies find no age-related health differences between midlife and aging parents of adults with developmental disabilities. In a study of female caregivers (86% were mothers) who resided in Illinois with an adult family member with intellectual and developmental disabilities, both midlife (aged 40–59) and older caregivers (aged 60 and older) were more likely to report arthritis, high blood pressure, obesity, and activity limitations than midlife and older women in the general population (Yamaki, Hsieh, & Heller, 2009). Thus, although the literature is not completely consistent regarding the onset of physical health effects, study findings converge on the conclusion that long-term caregiving for adults with developmental disabilities takes a toll on the physical health of aging parents, suggesting a cumulative stress process.
The results have shown greater variance when examining mental health. In a cross-sectional analysis using a nationally representative sample, younger parents of individuals with developmental problems were more divergent than older parents from the comparison group with respect to negative affect and psychological well-being (parental age range = 35–84 years, mean = 54 years; Ha et al., 2008). This finding suggests a narrowing of the gap between caregiving and non- caregiving parents with advancing age. Similar trends were reported by Barker and colleagues (2011) who examined the trajectories of emotional well-being in mothers (parental age range = 32–82 years, mean = 51 years at baseline) of adolescents and adults with autism. The study used data collected during five occasions over a 10-year period and found that these mothers experienced a decreased level of anxiety during the period. The Magana and Smith (2006) study mentioned above, also found significantly more depressive symptoms in midlife caregiving mothers than their age peers without caregiving responsibilities, but this difference was not found in the older age group. These findings suggest an adaptation process.
In contrast, findings from other studies suggest a cumulative stress process. Caldwell (2008) conducted a cross-sectional analysis in four age groups and found that both midlife (45–53 years old) and older mothers (65 years and older) of adults with developmental disabilities reported poorer mental health relative to population norms. Older female caregivers of adults with developmental disabilities reported significantly more mentally unhealthy days than their age peers from the general population, while no such difference was found in the midlife group (Yamaki et al., 2009).
Our prior research based on the WLS, compared parents of adults with developmental disabilities when the parents were in their early 50s and mid-60s to their age peers who were parents of adults without disabilities (Seltzer et al., 2011). We found evidence supporting the cumulative stress hypothesis. In their early 50s, parents of adolescent or adult children with developmental disabilities did not differ from their age peers whose children did not have disabilities in the areas of psychological functioning and social participation. However, the relative vulnerability of these parents became evident in their mid-60s as they reported less frequent visits with friends, more depressive symptoms, greater obesity, more functional limitations, and lower levels of health-related quality of life than the comparison group.
Parent and Adult Child Co-residence
A contextual factor that may significantly affect parental stress is whether the adult child with developmental disabilities continues to co-reside in the parental home. For example, aging parents who experienced more stressful life events and who co-resided with the child with autism reported higher levels of anxiety than parents who experienced fewer stressful life events and whose adult child had moved from the parental household (Barker et al., 2011). Similarly, in the WLS sample, we found relatively poorer functioning among parents in their early 50s and mid60s whose adult child continued to live at home (Seltzer et al., 2011). Older co-residing parents may experience increased anxiety about their child’s future living situation when the parents are no longer able to provide daily care (Yoong & Koritsas, 2012). Therefore, in the present study, we examined whether parents who lived with their adult children with developmental disabilities showed a pattern of greater vulnerability with respect to psychological well-being, physical health, and social integration, as compared to parents whose adult children with developmental disabilities lived elsewhere. Due to the small number of adult children in the comparison group living with their parents, we were only able to examine this association among parents of adults with developmental disabilities.
The Present Study
The present study aims to advance our understanding of the potential long-term effects of parenting an adult with developmental disabilities by extending the investigation over an approximately 20-year period to the time when parents are in their 70s and at increased risk of health problems. By using data from three time points, we are also able to estimate intraindividual change.
A unique strength of the WLS is its non-biased identification of caregiving parents and rich data on health and well-being. WLS participants were randomly selected for the study before they became parents (i.e., when they were seniors in high school), and thus, their participation in the study is independent of having a child with a disability. In addition, the WLS captures multiple domains of well-being (i.e., physical, psychological, and social) and allows us to compare parents of adults with developmental disabilities to parents whose adult children do not have disabilities.
Based on the cumulative stress model and the previous literature, we hypothesized that:
Parents of adults with developmental disabilities would experience a sharper decline over time in their physical and mental health relative to comparison group parents.
The gap between the physical and mental health of parents who co-resided with their adult children with developmental disabilities and parents whose children with developmental disabilities lived outside the household would become greater over time.
Methods
Data and Sample
The WLS is composed of a random sample of 10,317 women and men who graduated from Wisconsin high schools in 1957 and a sub-sample of their randomly selected siblings (Herd, Carr, & Roan, 2014). After initial data collection in 1957, follow-up surveys were conducted in 1975 with 9,138 (90.1%) surviving members of the original sample when they were in their mid-30s; in 1992 with 8,493 (87.2%) when they were 53 years old, on average; in 2004 with 7,265 (80.0%) when they were age 64, on average; and again in 2011, with 5,969 (68.4%) when they were 71 years old, on average. Parallel data collection procedures were conducted with siblings of the original respondents in 1977, 1994, 2006, and 2011 with 5,823 siblings participating in one or more of these data collection points. Over 99% the WLS sample respondents were white, reflecting the racial composition of Wisconsin in 1957.
The WLS data have been collected by the University of Wisconsin Survey Center. For the present study, we drew on data from the last three waves of the WLS (i.e., 1992–1994, 2004–2006, and 2011) in which the data on various mental and physical health measures were collected. During the 1992–1994 and the 2004–2006 rounds of data collection, data were collected via telephone interviews, whereas during the 2011 wave, data were collected via in-home interviews. At each wave, a self-administered questionnaire was also completed. Additional details of the WLS data collection and interview methods can be found at (http://www.ssc.wisc.edu/wlsresearch/documentation/flowcharts ).
The analytic sample for the present study was restricted to those who participated in the 2004–2006 survey when parents with a child with developmental disabilities were identified through a systematic screening module. The module consisted of a maximum of 31 questions that began by asking parents if any of their biological or adopted children (living or deceased) had a developmental disability or serious long-term mental health problem, and if so, the specific diagnosis. If a parent indicated that the son or daughter had a specific developmental disability (e.g., Down syndrome, cerebral palsy, fragile X syndrome, autism spectrum disorder), or used terms such as “developmental disability,” “mental retardation,” or “cognitive disability,” that child was included in the developmental disability group. In a few cases, parents did not know the child’s specific diagnosis but indicated that the condition began before age 22. In such cases, follow-up questions asked if the child was below- average in intelligence, ever attended special education classes, and/or had limitations in holding a regular job or independently carrying out other tasks of adult life. If yes, he or she was included in the developmental disabilities group. In addition, when a parent indicated that the child had epilepsy or seizures, only if the epilepsy was accompanied by below-average intelligence was the child included in the developmental disabilities group.
Using these inclusion criteria, 249 parents (n = 122 fathers, n = 127 mothers) were identified as having one or more biological or adopted child with a developmental disability in 2004–2006. Among the 249 parents, 240 previously participated in the 1992–1994 interviews and 183 subsequently participated in the 2011 interviews. The children had a range of developmental disabilities, including cerebral palsy (n = 36), Down syndrome (n = 33), autism spectrum disorder (n = 31), brain injury (n = 9), other specific developmental disabilities (n = 26), and developmental disabilities due to unspecified causes (n = 114). About 62% of the parents had a son with developmental disabilities, and the remaining 38% had a daughter with developmental disabilities. Co-residence was common in this sample. In 1992–1994, 46% (n = 107) of the children with developmental disabilities co-resided with their parents, and the proportions in 2004–2006 and 2011 were 38% (n = 88) and 31% (n = 50), respectively.
Respondents in the 2004–2006 survey (n = 9,016; n = 4,258 fathers, n = 4,758 mothers) were selected for the comparison group based on the following criteria: (1) the respondent had at least one biological or adopted child; and (2) the respondent had no identified children (living or deceased) with a developmental disability, a mental health condition, or a chronic health problem requiring ongoing care. Out of 9,016 parents in the comparison group, 8,589 participated in 1992–1994 interviews, and 6,780 participated in 2011 interviews. Although we use the terms “fathers” and “mothers,” the data are based on the primary WLS respondents, and thus, none of the sample members are married to one another.
Measures
Outcome variables.
We included six out-come measures categorized into three domains: (1) psychological functioning, (2) physical health, and (3) social integration.
To examine respondents’ psychological functioning, measures of depressive symptoms and psychological well-being were used. Depressive symptoms were measured by the Center for Epidemiological Studies Depression Scale (CES- D; Radloff, 1977) consisting of 20 items, each of which assessed how many days in the past week respondents experienced a specific symptom. The data were recoded into four categories (0 = never, 1 = 1–2 days, 2 = 3–4 days, 3 = 5–7 days), consistent with the conventional scoring of the CES-D. The total score was the sum of the ratings for the 20 items, with higher scores indicating more depressive symptoms. The internal consistency of the items was excellent; Cronbach’s alpha ranged from 0.85 to 0.86 across the three waves. The average stability coefficient across the three waves (1992–1994, 2004–2006, and 2011) was 0.68.
For psychological well-being, a modified version of Ryff’s Psychological Well-Being measure (Ryff, 1989) was used. The measure encompassed six domains of psychological well-being (1) Self-Acceptance, (2) Positive Relations with Others, (3) Autonomy, (4) Environmental Mastery, (5) Purpose in Life, and (6) Personal Growth. The Purpose in Life subscale consisted of four items, and the other sub-scales consisted of three items. Each item was rated on a scale of 1 to 6 (1 = agree strongly, 6 = disagree strongly), and the items were reverse coded so that a higher score reflected a higher level of well-being. The total score of overall well-being was the sum of the 19 items, ranging from 19 to 114. Cronbach’s alpha ranged from 0.88 to 0.89 across the three waves. The average stability coefficient across the three waves was 0.52.
Measures of physical health included (1) self-rated health, (2) self-report physical symptoms, and (3) body mass index (BMI). For self-rated health, respondents were asked to rate their health at the present time (1 = very poor, 5 = excellent). The average stability coefficient across the three waves was 0.48. The number of self-reported physical symptoms was measured by a count of the number of symptoms the respondent experienced in the past 6 months from a list of 16 symptoms—(1) a lack of energy, (2) fatigue/exhaustion, (3) headache, (4) dizziness/faintness, (5) numbness, (6) ringing in the ears, (7) upset stomach, (8) constipation, (9) diarrhea, (10) aching muscles, (11) stiff/swollen joints, (12) back pain/strain, (13) chest pain, (14) shortness of breath, (15) excessive sweating, and (16) skin problems. The average stability coefficient across the three waves was 0.53. BMI was calculated from self-reported weight and height. On average, BMI was quite stable (mean stability coefficient = 0.80) over time.
The social integration domain included frequency of contact with friends or relatives and the presence of a confidant. The respondent was asked first how many times (0 = never, 28 = every day) s/ he had gotten together socially with friends over the past four weeks, and then the number of times he/she had gotten together with relatives during the past four weeks. The mean of the response to these two items was calculated to measure the frequency of getting together with friends and relatives during the past four weeks.
The respondent was asked two questions about the presence of a confidant (1) whether s/ he has a family member with whom s/he could really share his/her very private feelings, and (2) whether s/he has such a friend. Responses to these two items were combined to indicate the presence of a confidant (2 = both a family member and a friend; 1 = either a family member or a friend; 0 = no confidant).
Independent variables.
The main independent variable was whether the parent had an adult child with developmental disabilities (1 = parent of an adult child with developmental disabilities, 0 = parent did not have any children with developmental disabilities). This was a time-invariant variable. Since there are likely long-term effects of caregiv- ing on parental health in old age, parents whose child with developmental disabilities died between 1992 and 2011 were included in the developmental disabilities group. However, as noted below, we controlled for the effects of child death on parental well-being.
For the within-disability group analysis, the living situation of the adult with developmental disabilities was included as an independent variable (1 = adult child lived in the parent’s home, 0 = adult child lived away from the parental home). This variable was coded as time-varying, given that an adult child might move in and out of the parent’s household during the 20-year period covered by this study.
Control variables.
Respondent sociodemographic characteristics were included as control variables. These included the respondent’s gender (1 = mothers, 0 =fathers), education (in years), and whether the respondent had a deceased child (1 = yes, 0 = no). The experience of losing a child was controlled given that bereaved parents are more likely to experience a higher level of depressive symptoms, poorer well-being, and more health problems (Rogers, Floyd, Seltzer, Greenberg, & Hong, 2008). This variable was coded as time- varying, as parents are more likely to experience child death as they get older. The child gender (1 = daughter, 0 = son) variable was included as a covariate in the within-disability group analysis. We controlled for child gender only in the within- group analysis because for the comparison group the target child was randomly selected. Since there are many more comparison group cases relative to cases with developmental disabilities, the effect of the child’s gender in the main analysis represents a random variable, and therefore unrelated by definition to the outcome measures.
Analysis
We used growth curve models to examine the effect of lifelong parenting for an adult child with developmental disabilities on the parent’s physical, psychological, and social well-being over an approximately 20-year period in the parent’s life course (i.e., ages 53 to 71). Growth curve models are appropriate for analyzing panel data with repeated observations nested within individuals. The models are also advantageous in incorporating all respondents who have been observed at least once over the multiple time points (Curran, Obeidat, & Losardo, 2010). We centered the parent’s age at the last point of data collection (mean age of 2011 wave = 71 years of age) because we were particularly interested in examining the effects of having an adult child with developmental disabilities in later life. We tested parental group x age interactions to assess whether parents of adults with developmental disabilities evidence a sharper decline in their health and well-being over time than the comparison group.
We tested the three-way interaction of parental group x gender x age for all of the outcome variables to estimate the differential lifelong caregiving effects in mothers and fathers over the 20-year period. However, none of the three-way interaction effects were significant, and these results are not presented in the paper. All models controlled for the parent’s gender, years of education, and whether the parent had experienced the death of a child.
Additionally, a follow-up within-group analysis was conducted to examine whether parents who lived with their child with developmental disabilities showed a different pattern of change in well-being as they aged than parents who lived apart from their child with developmental disabilities. This within-group analysis controlled for the parent’s gender, years of education, and whether the parent had experienced a child death, as well as the gender of the child with developmental disabilities.
Our sample of parent respondents included 2,233 sibling pairs (i.e., one respondent from the original sample, and the other from the sibling sub-sample). We adjusted standard errors of all models under the assumption of correlation within sibling pairs. We employed multiple imputation (mi impute) for missing data in STATA statistical software. The variable measuring the frequency of visits with friends or relatives was the variable that was missing most frequently (20%). The results present the estimates pooled across twenty imputed datasets given the recommendation to impute at least one data set per percentage of data missing (Anderson, 2010).
Results
Sample characteristics are reported in Table 1 separately for parents of an adult child with developmental disabilities and the comparison group. There were no differences between the two groups with respect to parental age, gender, or education. Across all three time periods, parents who have a child with developmental disabilities were more likely to experience the death of a child than parents in the comparison group.
Table 1.
Descriptive Statistics of Parents of an Adult Child With Developmental Disabilities (Developmental Disabilities) and Parents of Adults Without Disabilities (Comparison)
| Variables | Wave | Developmental Disabilities M (SD) or % |
Comparison M (SD) or % |
t or x2 |
|---|---|---|---|---|
| Age in 1992–1994 (years) | 53.60 (4.57) | 53.12 (4.09) | −1.76† | |
| Female (%) | 51.00 | 52.77 | 0.30 | |
| Education in 1992–1994 (years) | 13.81 (2.61) | 13.62 (2.32) | −1.26 | |
| Have a deceased child (%) | 1992 | 10.00 | 4.96 | 12.26*** |
| 2004 | 17.27 | 7.48 | 32.55*** | |
| 2011 | 24.59 | 10.68 | 35.10*** | |
p ≤ .10
p ≤ .05
p ≤ .01
p ≤ .001.
Table 2 presents results from a series of growth curve models of health and well-being over an approximately 20-year period in the parent’s life course (i.e., 53 to 71 years old, on average). The main effect of parental status (developmental disabilities vs. comparison group) indicates whether parents of adults with developmental disabilities differ from comparison group parents when respondents were 71 years old, on average. The parental group x age interaction is a test of our hypothesis that the group of aging parents of children with developmental disabilities would differ from the comparison group over time in their rate of change with respect to the outcome of interest.
Table 2.
Trajectories in Midlife and Old Ages Among Parents of an Adult Child With Developmental Disabilities and Parents of Adults Without Disabilities (Polled Results From Multiple Imputed Data)
| Depressive Symptoms |
Psychological Well-being |
Self-rated Health |
Physical Symptoms |
Body Mass Index |
Friend/Relative Visits |
Having a Confidant |
|
|---|---|---|---|---|---|---|---|
| Fixed Part | |||||||
| Intercept | 10.79*** (0.41) | 77.17*** (0.75) | 3.15***(0.04) | 6.01*** (0.20) | 32.42*** (0.32) | 2.69*** (0.16) | 1.30***(0.03) |
| Developmental | 1.34** (0.51) | −1.92* (0.92) | −0.09*(0.04) | 1.10*** (0.23) | 0.66 (0.46) | −0.65*** (0.18) | −0.02(0.05) |
| Disabilities (DD) | |||||||
| Linear slope (age) | 0.13*** (0.01) | −0.12*** (0.01) | −0.01*** (0.00) | 0.05*** (0.00) | 0.11*** (0.00) | −0.00 (0.00) | −0.01*** (0.00) |
| Quadratic slope (age2) | 0.01*** (0.00) | ||||||
| Female | 1.15*** (0.13) | 1.36*** (0.25) | 0.08*** (0.01) | 0.52*** (0.06) | −1.51*** (0.10) | 0.88*** (0.05) | 0.25*** (0.01) |
| Education | −0.27*** (0.03) | 0.94*** (0.05) | 0.05*** (0.00) | −0.07*** (0.01) | −0.21*** (0.02) | 0.03** (0.01) | 0.01* (0.00) |
| Have a deceased child | 0.56** (0.22) | −0.80* (0.35) | −0.02 (0.02) | −0.11 (0.10) | 0.18 (0.14) | −0.10 (0.09) | 0.02 (0.02) |
| DD x age | 0.03 (0.03) | —0.08† (0.04) | −0.00 (0.00) | 0.04* (0.01) | −0.00 (0.02) | −0.01 (0.01) | 0.00 (0.00) |
| Random Part | |||||||
| Level 1 residual | 4.69 (0.07) | 6.41 (0.08) | 0.44 (0.00) | 2.08 (0.02) | 1.99 (0.05) | 2.40 (0.03) | 0.46 (0.00) |
| Level 2 age | 0.21 (0.01) | 0.35 (0.01) | 0.02 (0.00) | 0.11 (0.00) | 0.13 (0.00) | 0.06 (0.01) | 0.01 (0.00) |
| Level 2 intercept | 5.62 (0.11) | 10.65 (0.13) | 0.55 (0.01) | 2.94 (0.04) | 5.37 (0.06) | 1.96 (0.06) | 0.38 (0.00) |
p ≤ .10
p ≤ .05
p ≤ .01
p ≤ .001.
Psychological functioning.
Regarding depressive symptoms, at age 71 parents of adults with disabilities had significantly higher rates of depressive symptoms than parents in the comparison group, controlling for gender, education, and whether the parent had experienced the death of a child. This was a modest difference; parents of adults with developmental disabilities experienced 1.34 more depressive symptoms than parents in the comparison group when they were 71 years old, on average. The parental group by age interaction was not significant, indicating that depressive symptoms changed at a similar rate over time for both groups.
For all parents, depressive symptoms displayed a curvilinear relationship over time. Depressive symptoms decreased between 1992–1994 and 2004–2006 (with a negative linear slope when the intercept was set at the mean age of 53 years in 1992, β = —0.19, p < .001), but increased again by 2011 (with a positive quadratic slope coefficient, β = 0.01, p < .001). Women, those with less education, and those who had experienced the death of a child reported, on average, higher levels of depressive symptoms.
Regarding psychological well-being, the main effect of parental group status was significant, indicating that parents of an adult child with developmental disabilities had poorer well-being than comparison group parents when they were 71 years old, on average. Also, the parental group x age interaction was a trend level effect. As shown in Figure 1, although the two groups were quite similar in their levels of psychological well-being when they were in their early 50s, parents of children with developmental disabilities experienced a steeper decline over time and had lower levels of psychological well-being by age 71 than parents in the comparison group. Women and those with more education reported higher levels of psychological well-being.
Figure 1.
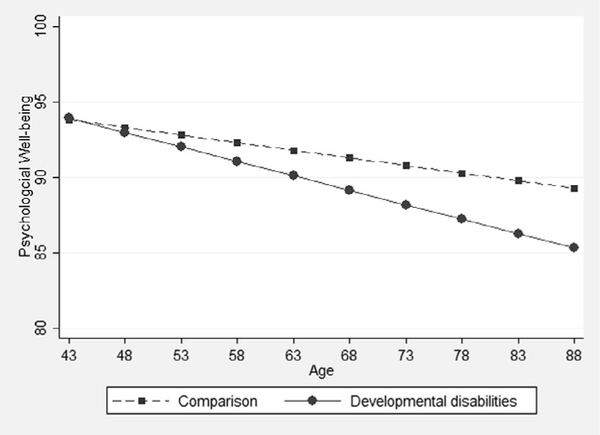
Changes in psychological well-being over time by parental group.
Physical health.
At age 71, parents of adults with developmental disabilities rated their health as being significantly poorer and reported significantly more physical health symptoms than parents in the comparison group. There was no difference in BMI between parents of adults with developmental disabilities and their age peers at age 71. The interaction effect of parental group by age on the number of physical symptoms was significant (β = 0.04, p < .01), indicating that parents of adults with developmental disabilities showed a steeper increase in physical symptoms over the 20-year study period than parents in the comparison group (See Figure 2). The interaction of parental group by age was not significant for self-rated health or BMI, indicating that the rate of change over time was similar across the two groups. Women perceived their health as better and had a lower BMI, but reported more physical health symptoms than men. Those with more education perceived their health as better, reported fewer physical health symptoms, and had a lower BMI than those with less education. The experience of child death was not related to physical health.
Figure 2.
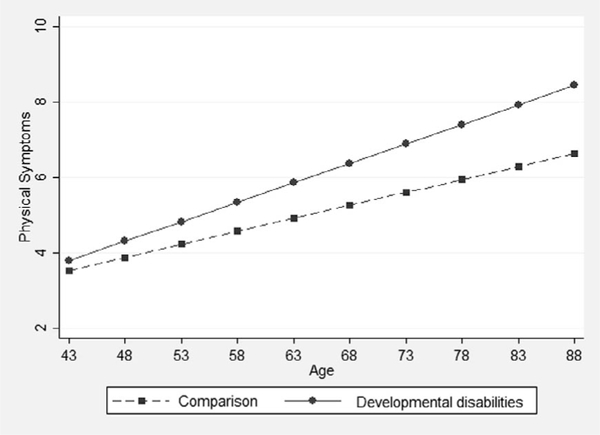
Changes in number of physical symptoms over time by parental group.
Social integration.
At age 71, parents of adults with developmental disabilities had fewer visits with friends or relatives than parents in the comparison group, but the two parental groups did not differ with respect to having a confidant. The interaction of parental group by age was not significant. Women and those with higher levels of education were more likely to visit with friends or relatives and have a confidant, but the experience of losing a child was unrelated to these outcomes.
Within-group analysis of co-residence.
Parents whose adult child with developmental disabilities lived with them reported significantly lower levels of psychological well-being, fewer visits with friends or relatives, more health symptoms, and a greater BMI (at a trend level) at age 71 than parents whose adult child with developmental disabilities lived outside the house-hold (see Table 3).
Table 3.
Trajectories of Co-residing and Non-co-residing Parents of an Adult Child With Developmental Disabilities (Pooled Results From Multiple Imputed Data)
| Depressive Symptoms |
Psychological Well-being |
Self-rated Health |
Physical Symptoms |
Body Mass Index |
Friend/ Relative Visits |
Having a Confidant | |
|---|---|---|---|---|---|---|---|
| Fixed Part | |||||||
| Intercept | 11.45*** (2.57) | 78.01*** (4.51) | 3.44*** (0.24) | 5.34*** (1.10) | 31.23*** (2.25) | 3.40*** (0.86) | 1 27*** (0.23) |
| Co-residence | 1.59 (1.00) | −2.67* (1.33) | −0.07 (0.09) | 0.88† (0.46) | 0.99† (0.57) | −0.91** (0.34) | −0.01 (0.09) |
| Linear slope (age) | 0.05 (0.06) | −0.19** (0.07) | −0.02*** (0.00) | 0.09*** (0.02) | 0.08*** (0.02) | −0.01 (0.02) | −0.01** (0.00) |
| Quadratic slope (age2) | 0.01† (0.00) | ||||||
| Female | 1.71† (0.95) | 0.74 (1.62) | −0.04 (0.07) | 0.58 (0.39) | 0.23 (0.74) | 0.47 (0.30) | 0.25*** (0.07) |
| Education | −0.28† (0.16) | 0.87*** (0.27) | 0.04* (0.02) | 0.02 (0.07) | −0.22 (0.14) | −0.03 (0.05) | 0.01 (0.01) |
| Have a deceased child | 1.15 (0.92) | −2.80† (1.54) | −0.03 (0.08) | 0.39 (0.41) | 0.36 (0.68) | −0.15 (0.36) | 0.01 (0.09) |
| Daughter | −0.34 (1.01) | −0.55 (1.53) | −0.08 (0.08) | 0.31 (0.37) | 1.01 (0.72) | 0.06 (0.29) | −0.02 (0.07) |
| Co-residence x age | 0.13* (0.06) | −0.02 (0.10) | −0.00 (0.01) | 0.03 (0.03) | 0.06† (0.03) | −0.03 (0.03) | 0.01 (0.01) |
| Random Part | |||||||
| Level 1 residual | 4.98 (0.37) | 6.74 (0.37) | 0.43 (0.02) | 2.26 (0.09) | 2.09 (0.17) | 2.16 (0.13) | 0.50 (0.03) |
| Level 2 age | 0.00 (0.00) | 0.28 (0.08) | 0.00 (0.01) | 0.00 (0.00) | 0.09 (0.06) | 0.00 (0.00) | 0.00 (0.00) |
| Level 2 intercept | 5.88 (0.56) | 10.40 (0.61) | 0.46 (0.03) | 2.38 (0.13) | 5.15 (0.46) | 1.55 (0.21) | 0.39 (0.03) |
p ≤ .10
p ≤ .05
p ≤ .01
p ≤ .001.
We found modest support for our hypothesis that as parents of adults with developmental disabilities aged, the well-being gap between coresiding and non-co-residing parents would become greater over time. As shown in Table 3, there was a significant interaction between co-residence and age for depressive symptoms. Specifically, parents whose adult child continued to co-reside showed increases in levels of depression over time, but levels of depression tended to be stable among parents who lived apart from their children (see Figure 3). The interaction between age and coresidence for BMI showed a trend level effect (p =.06). As shown in Figure 4, BMI increased at a greater rate over time among parents living with their son or daughter with developmental disabilities, than those living apart from their affected child. There were no significant interactions in psychological well-being, self-rated health, physical symptoms, the frequency of visits with friends or relatives, or the presence of a confidant.
Figure 3.
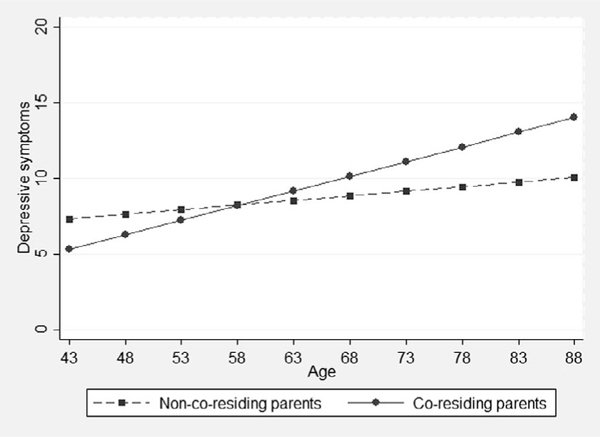
Changes in depressive symptoms over time by co-residence status of parents of adults with developmental disabilities.
Figure 4.
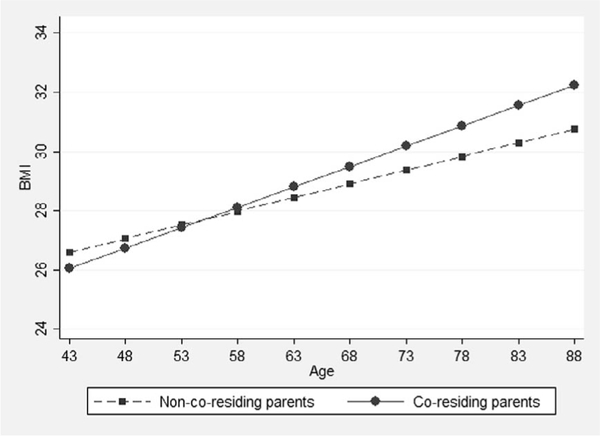
Changes in body mass index (BMI) over time by co-residence status of parents of adults with developmental disabilities.
Discussion
Using a probability sample, we examined the longitudinal effects of having an adult child with developmental disabilities on parental well-being over a 20-year period spanning midlife to early old age. The present study extends our prior analysis (Seltzer et al., 2011) in which we compared well-being of parents of adults with developmental disabilities to their age peers of adults without disabilities from their early 50s to their mid-60s. In this study, we examined whether the patterns of decline observed when parents were in their mid-60s persist into the next decade of life and whether these parents experienced a sharper decline in their health and well-being over time than their age peers without caregiving responsibilities.
We found that the effects of lifelong caregiv- ing that were evident when parents were in their 60s persisted into their 70s and that some effects not detected in early old age became significant as these parents entered their 70s. Specifically, parents of adults with developmental disabilities continued to experience poorer health and well-being in old age (i.e., at age 71) than their age peers whose children had no disabilities, as indicated by a greater number of health symptoms and fewer visits with friends or relatives, which are patterns that were detected when these parents were in their mid-60s (Seltzer et al, 2011). These parents also had higher levels of depression and lower levels of psychological well-being and poorer self-rated health than their age peers in their early 70s, a pattern not evident when they were in their mid-60s. Thus, the findings of the present study provide additional support for the importance of a life course approach to capture a more nuanced understanding of the long-term impact of caregiv- ing on parents of children with disabilities.
Overall, we found only modest support that parents of adults with disabilities experience a steeper decline in their well-being in later years than parents in the comparison group. It was only with respect to physical health symptoms and psychological well-being (at a trend-level) that we found evidence that aging parents of adults with developmental disabilities experienced a steeper decline in their well-being than their age peers without these caregiving responsibilities. This finding is in line with our prior study in which the most prominent profile of life course divergence from the normative pattern was reported in the domain of physical health (Seltzer et al., 2011).
The fact that parents of adults with developmental disabilities had poorer health in their early 70s and showed a steeper increase in health problems over time has important implications for policy and service delivery. There have been many efforts to develop programs and services to improve the health of adults with developmental disabilities (Heller, Fisher, Marks, & Hsieh, 2014). However, there has been virtually no research on the development of health promotion programs for aging parents of adults with developmental disabilities. An exception is the health promotion intervention, known as Caring for Myself, developed for Latina mothers of youth and adults with intellectual and developmental disabilities (Magana, Li, Miranda, & Paradiso de Sayu, 2015). This intervention consists of eight weekly sessions to encourage caregivers to engage in healthy behaviors, such as accessing health care services or relevant medical tests, nutrition, and exercise. The initial results for this intervention have been promising, reporting that in post-treatment assessment the caregivers felt an increased sense of health-related self-efficacy and reported an increase in preventative health behaviors (Magana et al., 2015). Studies are needed to extend this health promotion intervention to the general population of aging parental caregivers of adults with developmental disabilities.
Our findings suggest that aging parents who co-reside with their adult child with developmental disabilities are a particularly vulnerable group. At age 71, these parents had poorer psychological well-being, more physical health symptoms, greater obesity, and fewer visits with friends or relatives. Also, these parents experienced a significantly more rapid increase over time in depressive symptoms, and, at a trend level, a steeper increase in BMI. As nearly one-third of the parents of adults with developmental disabilities during this stage of life continued to have their adult children live at home, their increased vulnerability is a significant public health concern.
The present study has limitations that should be considered when interpreting the results. First, since the respondents of the study were identified during the 2004—2006 interviews when they were in their mid-60s on average, parents who died or dropped out of the longitudinal study prior to this time point were not identified. Second, the findings reflect the experience of one cohort of the adult population representative of Wisconsin high school graduates in 1957. The lack of racial and ethnic diversity within the sample places limitations on the generalizability of the findings to other cultural contexts. Finally, longitudinal data measuring the caregiving context, such as the child’s behavior problems were not collected and might have provided greater insight into the mechanisms underlying the parental declines.
Juxtaposed against these limitations are several strengths of the current study, including the availability of data on a random sample of parents of children with developmental disabilities over a 20-year period, measures of multiple domains of well-being of the parents, and the use of longitudinal analytic methods to capture both within-individual and between-individual change over time. The findings from this study extend our earlier work suggesting that the effects of parenting an adult child with developmental disabilities are more pronounced in the later years as compared with midlife. These effects, which were first detected when parents were in their mid-60s, persisted as parents entered their eighth decade of life. The findings point to the need for supports to meet the needs of older parents and families of adults with developmental disabilities. Considering the sharper declines in the physical health of aging parents of adults with developmental disabilities, respite care for individuals with disabilities, and health care services for their aging parents may be particularly needed. Intervention research is needed to determine how best to serve these families in the later phase of the life course.
Acknowledgments
Support for this research was provided by the National Institute on Aging for Project 3 of P01AG21079 (Pamela Herd, PI; Marsha R. Mailick, PI of Project 3). Support for this research was also provided by grant U54 HD090256 to the Waisman Center (Albee Messing, PI) and the Office of the Vice Chancellor for Research and Graduate Education at the University of Wisconsin - Madison with funding from the Wisconsin Alumni Research Foundation.
Contributor Information
Eun Ha Namkung, School of Social Work, University of Wisconsin-Madison; The Lurie Institute for Disability Policy, Brandeis University.
Jan S. Greenberg, School of Social Work and Waisman Center, University of Wisconsin-Madison
Marsha R. Mailick, School of Social Work and Waisman Center, University of Wisconsin-Madison
Frank J. Floyd, Psychology Department, University of Hawaii at Manoa.
References
- Anderson C (2010). Applied Missing Data Analysis. New York: Guilford Press. [Google Scholar]
- Baker BL, Blacher J, & Olsson MB (2005). Preschool children with and without developmental delay: Behaviour problems, parents’ optimism and well-being. Journal of Intellectual Disability Research, 49, 575–590. 10.1111/j.1365-2788.2005.00691.x [DOI] [PubMed] [Google Scholar]
- Barker ET, Hartley SL, Seltzer MM, Floyd FJ, Greenberg JS, & Orsmond GI (2011). Trajectories of emotional well-being in mothers of adolescents and adults with autism. Developmental Psychology, 47(2), 551–561. 10.1037/a0021268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell J (2008). Health and access to health care of female family caregivers of adults with developmental disabilities. Journal of Disability Policy Studies, 19(2), 68–79. 10.1177/1044207308316093 [DOI] [Google Scholar]
- Curran PJ, Obeidat K, & Losardo D (2010). Twelve frequently asked questions about growth curve modeling. Journal of Cognition and Development, 11(2), 121–136. 10.1080/15248371003699969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha JH, Hong J, Seltzer MM, & Greenberg JS (2008). Age and gender differences in the well-being of midlife and aging parents with children with mental health problems or development disorders: Report of a national study. Journal of Health & Social Behavior, 49(3), 301–316. 10.1177/002214650804900305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller T, Fisher D, Marks B, & Hsieh K (2014). Interventions to promote health: Crossing networks of intellectual and developmental disabilities and aging. Disability and Health Journal, 7(1), S24–S32. 10.1016/j.dhjo.2013.06.001 [DOI] [PubMed] [Google Scholar]
- Herd P, Carr D, & Roan C (2014). Cohort Profile: Wisconsin longitudinal study (WLS). InternationalJournal of Epidemiology, 43(1), 34–41. 10.1093/ije/dys194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R, & Folkman S (1984). Stress, Appraisal, and Coping. New York: Springer Publishing Company. [Google Scholar]
- Magaña S, Li H, Miranda E, & Paradiso de Sayu R (2015). Improving health behaviours of Latina mothers of youths and adults with intellectual and developmental disabilities. Journal of Intellectual Disability Research, 59(5), 397–410. 10.1111/jir.12139 [DOI] [PubMed] [Google Scholar]
- Magaña S, & Smith MJ (2006). Health outcomes of mid-life and aging Latina and Black American mothers of children with developmental disabilities. Mental Retardation, 44, 224–234. 10.1352/00476765(2006)44[224:HOOMAO]2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Menard S, (Ed.). (2008). Handbook of Longitudinal Research: Design, Measurement, and Analysis. Amsterdam: Elsevier. [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, & Meersman SC (2005). Stress, health, and the life course: Some conceptual perspectives. Journal of Health and Social Behavior, 46(2), 205–219. 10.1177/002214650504600206 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A selfreport depression scale for researching the general population. Applied Psychological Measurement, 1, 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rogers CH, Floyd FJ, Seltzer MM, Greenberg J, & Hong J (2008). Long-term effects of the death of a child on parents’ adjustment in midlife. Journal of Family Psychology, 22(2), 203–211. 10.1037/0893-3200.22.2.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology, 57(6), 1069–1081. 10.1037/0022-3514.57.6.1069 [DOI] [Google Scholar]
- Seltzer MM, Floyd FJ, Song J, Greenberg JS, & Hong J (2011). Midlife and aging parents of adults with intellectual and developmental disabilities: Impacts of lifelong parenting. American Journal on Intellectual and Developmental Disabilities, 116(6), 479–499. 10.1352/1944-7558-116.6.479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer MM, Greenberg JS, Floyd FJ, Pettee Y, & Hong J (2001). Life course impacts of parenting a child with a disability. American Journal on Mental Retardation, 106(3), 265–286. [DOI] [PubMed] [Google Scholar]
- Smith LE, Seltzer MM, Tager-Flusberg H, Greenberg JS, & Carter AS (2008). A comparative analysis of well-being and coping among mothers of toddlers and mothers of adolescents with ASD. Journal of Autism and Developmental Disorders, 38(5), 876–889. 10.1007/s10803-007-0461-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaki K, Hsieh K, & Heller T (2009). Health profile of aging family caregivers supporting adults with intellectual and developmental disabilities at home. Intellectual and Developmental Disabilities 47(6), 425–435. 10.1352/1934-9556-47.6.425 [DOI] [PubMed] [Google Scholar]
- Yoong A, & Koritsas S (2012). The impact of caring for adults with intellectual disability on the quality of life of parents. Journal of Intellectual Disability Research, 56(6), 609–619. 10.1111/j.1365-2788.2011.01501.x [DOI] [PubMed] [Google Scholar]


