Abstract
Duchenne muscular dystrophy is associated with an increased risk of bone fragility due to the adverse effects of prolonged glucocorticoid therapy and progressive muscle weakness on bone strength. Osteoporosis manifests clinically as low-trauma long-bone and vertebral fractures (VFs), with VFs frequent, particularly in those treated with glucocorticoid therapy. It is increasingly recognized that bone pain, medical complications of osteoporosis (such as fat embolism syndrome), and the potential for permanent, fracture-induced loss of ambulation can be mitigated with timely bone health surveillance and management. This includes periodic spine radiographs for VF detection because VFs can be asymptomatic in their early phases and thereby go undetected in the absence of monitoring. With this article, we provide a comprehensive review of the following 4 phases of bone health management: (1) bone health monitoring, which is used to identify early signs of compromised bone health; (2) osteoporosis stabilization, which is aimed to mitigate back pain and interrupt the fracture–refracture cycle through bone-targeted therapy; (3) bone health maintenance, which has the goal to preserve the clinical gains realized during the stabilization phase through ongoing bone-targeted therapy; and (4) osteoporosis therapy discontinuation, which places those who are eligible for discontinuation of osteoporosis treatment back on a health monitoring program. In the course of reviewing these 4 phases of management, we will discuss the criteria for diagnosing osteoporosis, along with detailed recommendations for osteoporosis intervention including specific drugs, dose, length of therapy, contraindications, and monitoring of treatment efficacy and safety.
Awareness is increasing that bone morbidity due to osteoporosis is a major complication of Duchenne muscular dystrophy (DMD) and its treatment and that it requires monitoring for early diagnosis and intervention to prevent clinically important sequelae. The 2 main risk factors for osteoporosis in this context are the progressive muscle weakness with loss of weight-bearing activity and osteotoxicity from glucocorticoid therapy. Short stature, delayed puberty, and frequent falls augment the already high risk of fractures. Vertebral fractures (VFs) can cause chronic pain and spine deformity, whereas long-bone fractures have been linked to permanent, premature loss of ambulation.1 As such, optimal management of osteoporosis is a major contributor to quality of life in patients living with DMD. Effective management of bone health in DMD is possible and may even influence survival.2–4 Authors of case series have described acute respiratory distress leading to death as a result of fat embolism syndrome occurring after long-bone fractures or injuries in patients with DMD2,3; authors of another study suggested that bisphosphonate therapy for osteoporosis may be linked to longevity.4
This review is targeted for primary care providers, neurologists, endocrinologists, and bone health specialists involved in the care of patients with DMD by providing specific recommendations to guide clinical practice. With appropriate prevention and treatment of glucocorticoid-related bone morbidity, it is anticipated that serious sequelae of osteoporosis and the need to withdraw glucocorticoid therapy because of bone health complications will be mitigated. The goals of optimal bone health management, therefore, are twofold. The first is to improve quality of life by reducing bone pain and preventing loss of ambulation due to fractures. The second goal is to provide skeletal protection in a timely manner so as to allow the patient to remain on glucocorticoid therapy for as long as desired and indeed necessary.
OSTEOPOROSIS IN DMD
Fractures due to osteoporosis are frequent in DMD,5 arising from the toxic effects of glucocorticoid therapy on bone metabolism along with the progressive dystrophinopathy, both of which are negative regulators of bone strength. Up to 60% of individuals with DMD present with low-trauma extremity fractures, often at the distal femur or tibia and fibula. Low-trauma VFs are also frequent but often go unrecognized because of their potential to be asymptomatic (particularly in the early stages).1,5–8 If left untreated, VFs are associated with progressive back pain, spine deformity, and heightened risk of sustaining a future fracture, whereas femur fractures have been linked to permanent, premature loss of ambulation.5 That osteoporosis treatment with bisphosphonates has been linked to survival provides further rationale for effective osteoporosis diagnosis, surveillance, and prevention strategies.4
Although the frequency of fractures is high in DMD, no published studies in this setting or in any other at-risk pediatric condition have been used to evaluate the safety and efficacy of drug therapy to prevent the first fracture. The current approach is to diagnose and treat the earliest signs of fractures, including VFs, in those with limited potential for spontaneous (drug-unassisted) recovery. This is in line with a secondary prevention strategy, which is to interrupt the progression of osteoporosis and facilitate recovery in patients with not only early evidence of bone fragility but also less potential for medication-unassisted recovery because of persistent risk factors.
An overview of the rationale for the recommended approach to bone health management is provided in the 2018 Updated DMD Care Considerations, sponsored by the Centers for Disease Control and Prevention.9 In the present article, we delve more deeply into the 4 phases of bone health care, as follows: (1) the bone health monitoring phase, which is used to identify early signs of compromised bone health in this high-risk group; (2) the osteoporosis stabilization phase, which is aimed to mitigate back pain and interrupt the fracture–refracture cycle through the administration of bone-targeted therapy; (3) the bone health maintenance phase, which has the goal to preserve the clinical gains realized during the stabilization phase; and (4) the osteoporosis therapy discontinuation phase, which places those who are eligible for discontinuation of osteoporosis treatment back on a skeletal health monitoring program. In the course of reviewing these 4 phases, we will discuss the criteria for diagnosing osteoporosis, along with detailed recommendations for osteoporosis intervention including specific drugs, dose, length of therapy, contraindications, and monitoring.
Skeletal Health Monitoring Phase
The extent of bone morbidity in pediatric DMD, including the potential for fractures before and in the years immediately after diagnosis, has prompted the recommendation to initiate monitoring at the time of diagnosis or no later than the time at which glucocorticoid therapy is initiated. Because VFs are more common in boys on glucocorticoid therapy,5 lateral thoracolumbar spine radiographs should be conducted at least every 2 years, compared with radiographs every few years in those who are not receiving glucocorticoid therapy. Radiographs for VF detection should be conducted sooner in the presence of back pain or a ≥0.5 decline in spine bone mineral density (BMD) z score on serial BMD measurements over a 12-month period or more. A baseline lateral spine radiograph around the time of diagnosis is recommended to facilitate the detection of the earliest signs of collapse on subsequent films.
A lumbar spine BMD by dual-energy x-ray absorptiometry is recommended annually in all patients to determine the overall bone health trajectory on serial measurements. In the event that dual-energy x-ray absorptiometry is challenging for cost or logistical reasons, a lateral thoracolumbar spine radiograph should be prioritized for VF detection. Although the lumbar spine is a frequent site for ascertaining BMD in children,10 lateral distal femur, hip,5 and total-body BMD z scores are also useful in children with neuromuscular disorders,11,12 including those with declining muscle function.8 BMD raw values are converted to age- and sex-specific z scores and require additional interpretation in view of body size, ethnicity, and pubertal staging or skeletal maturity (the latter, by bone age).13 Because BMD can be underestimated in patients with DMD because of their short stature, bone size should be adjusted by using a technique such as bone mineral apparent density (an estimation of volumetric BMD, in gram per cubic centimeter)14 or height z score–corrected BMD z score.15 A ≥0.5 decline in spine BMD z score is considered clinically significant on the basis of recent observations16; such a decline on serial BMD measurements over a 12-month period provides the rationale in a given patient to conduct spine radiographs sooner rather than later, as outlined in the 2018 Updated Care Considerations algorithm.9
During the monitoring phase, conservative steps can be taken to maintain overall bone health, including discussion around strategies to prevent falls and other accidents. Calcium intake should be assessed at least annually, with recommendations to achieve the Institute of Medicine’s updated age-related intake17 through diet and/or supplementation. Calcium supplementation is recommended only if daily intake is inadequate, out of concern for exacerbating the hypercalciuria that is a known feature of DMD.
In addition to at least an annual assessment of calcium intake, serum 25-hydroxyvitamin D (25OHD) should be verified annually (ideally at the end of winter in seasonal countries, recognizing that this is not always feasible). In keeping with the Institute of Medicine’s guidelines,17 the lowest acceptable vitamin D level is 20 ng/mL (50 nmol/L), with the ideal target being ≥30 ng/mL (75 nmol/L).18 Intakes beyond the Institute of Medicine’s recommended 600 IU per day are often required to achieve these target levels, given the paucity of vitamin D in the most commonly consumed foods, compounded by the lack of sunlight or sun exposure in many countries. As a fat-soluble vitamin, vitamin D can be given daily or intermittently at higher doses (ie, weekly, monthly). In the absence of rickets, typical vitamin D doses used to achieve these levels are as follows: 25OHD = 20 to 30 ng/mL → 1000 IU per day; 25OHD <20 ng/mL → 2000 IU per day; and 25OHD <10 ng/mL → 4000 IU per day. Higher doses may be required in some patients (those overweight or obese, with darker skin, less sun exposure, diets low in vitamin D, malabsorption, or medical therapy that interferes with vitamin D metabolism including glucocorticoids). After vitamin D supplementation for a low 25OHD level has been initiated, the measurement should be repeated 3 months later to document the adequacy of dosing and compliance. Although vitamin D2 and D3 have similar efficacy with daily dosing,19 vitamin D2 has rapid decay with intermittent therapy, whereas the decay is less rapid with vitamin D3.20 Thus, vitamin D3 is recommended in any patient undergoing intermittent therapy.
At each monitoring visit, the practitioner should take a fracture history and advise patients to report to their health care provider any fractures that occur in between visits. Bone and back pain assessments are also part of the annual monitoring approach, with pain assessed either according to a standardized tool such as the Faces of Pain Scale–Revised21 or by routine history taking. Back or bone pain that is reported between clinic visits should be assessed by plain radiographs to assess the possibility of fracture.
The Genant semiquantitative method22 for VF assessment is now accepted as a valid tool in children, given observations that Genant-defined fractures are associated with biologically logical predictors including back pain,23 low and/or declining BMD z scores,16,23 glucocorticoid exposure,16,23 and an increased risk of future VF.16,23 The Genant method defines VF according to the following reduction in height ratios: grade 0 (normal) ≤20%; grade 1 fracture (mild) >20% to 25%; grade 2 fracture (moderate) >25% to 40%; grade 3 fracture (severe) >40%. The scoring should be done by a radiologist, because it requires expertise in distinguishing VF from normal pediatric variants.24
Treatment: Osteoporosis Stabilization Phase
Osteoporosis is present once a child with risk factors for low-trauma bone fragility demonstrates at least 1 clinically significant fracture (ie, a long-bone fracture or VF; Fig 1).25 The patient should be referred at the time of a low-trauma fracture to a clinician with specific expertise in managing pediatric osteoporosis if this has not already been done. As shown in the algorithm (Fig 2), in the presence of a mild (grade 1) VF, treatment is recommended at the latest once the mild VF is associated with symptomatology, with back pain relief providing an important index of treatment efficacy in this setting. When an asymptomatic or minimally symptomatic grade 1 VF is identified, the patient should have a follow-up lateral spine radiograph 6 to 12 months later, or sooner if back pain emerges in the interim, to evaluate the status of the VF.
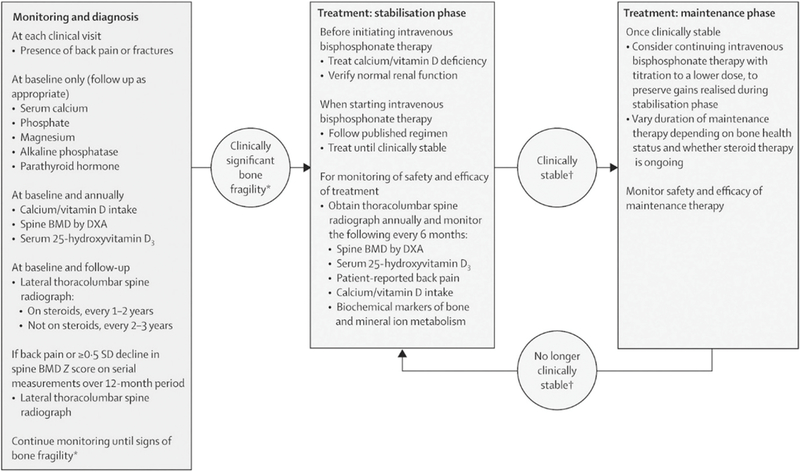
FIGURE 1.
Examples of VFs on a lateral thoracolumbar spine radiograph in a patient with DMD. This figure reveals the spine of a patient, age 10 years, with DMD who presented with back pain after 18 months of glucocorticoid therapy, in the absence of a previous history of routine spine health monitoring. Multiple VFs were identified on a lateral thoracolumbar spine radiograph, many in advanced stages of collapse. T10, thoracic vertebra 10; L5, lumbar vertebra 5.
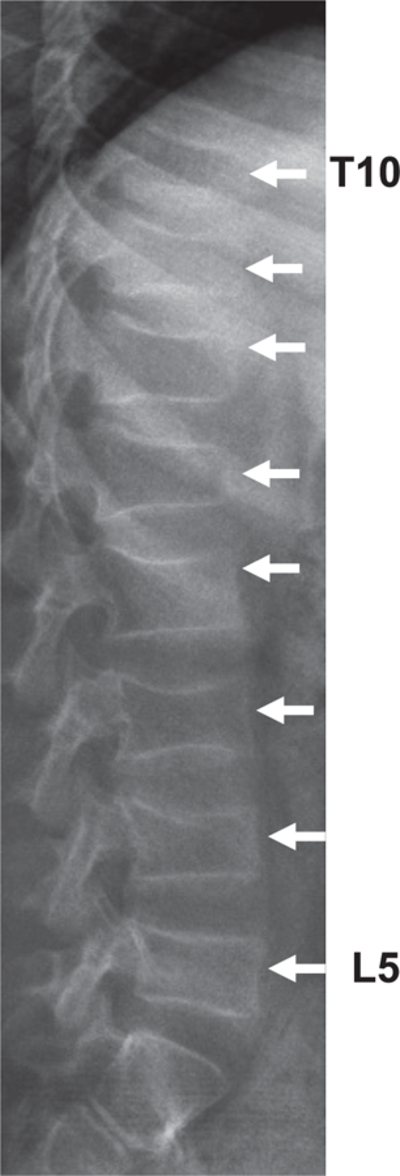
FIGURE 2.
Osteoporosis monitoring, diagnosis, and treatment algorithm for patients with DMD. DXA, dual-energy x-ray absorptiometry. *Signs of clinically significant bone fragility are low-trauma fractures of long bones or vertebra. †Clinical stability refers to the absence of nonvertebal fractures, stable healed VFs, absence of new VFs in previously normal vertebral bodies, absence of bone and back pain, and a BMD z score appropriate for height z score or >−2 SDs. (Reproduced with permission from Birnkrant DJ, Bushby K, Bann CM, et al; DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol. 2018;17[4]:353.)
The current standard of care for treating osteoporosis in childhood is intravenous (IV) bisphosphonate therapy (pamidronate, zoledronic acid, or neridronate).25,26 Using oral bisphosphonate therapy during the pediatric years is not advised because of data arising from controlled trials in osteogenesis imperfecta; the published controlled trials in which authors quantified vertebral body height clearly revealed increased vertebral heights in youth with osteogenesis imperfecta who were treated with IV bisphosphonate therapy.27–29 In contrast, none of the controlled studies of oral bisphosphonate studies revealed a positive effect on vertebral height.30–32 In addition, it is well known that the oral bioavailability of oral bisphosphonates is low.33,34 These data are particularly relevant to DMD in which the frequency of VF is high1 and support the use of IV instead of oral bisphosphonates as first-line therapy wherever possible in children despite its less convenient mode of administration.
IV therapy should be given at standard, published doses, as outlined in Fig 2.25,27,35,36 A clinician with relevant expertise should administer these agents to ensure the appropriate side effect management and that contraindications, such as renal disease, are respected. In some centers, bisphosphonate therapy is administered on an in-patient basis. However, the treatment can also be safely delivered in outpatient settings provided an on-call physician is available to the patient in the week after each infusion. Given the possibility of fever and vomiting with the first infusion, glucocorticoid stress-dosing recommendations must be provided (as discussed in the article on obesity and endocrine management in this supplement).37 In centers where access to a clinician with expertise in osteoporosis medical management is not available yet, and a patient is in need of treatment, liaison with an osteoporosis expert (usually an endocrinologist) through telehealth or other means of communication is recommended.
Bisphosphonates are contraindicated in patients with poor renal function (estimated glomerular filtration rate <35 mL per minute). Recently, the US Food and Drug Administration updated the label for zoledronic acid, stating it is also contraindicated in patients with acute renal impairment and that patients should be screened for renal insufficiency before initiating treatment. To this end, serum creatinine is not a reliable marker of renal function in patients with DMD, creating the need for other measures such as cystatin C to ensure adequate renal function before each bisphosphonate infusion. Monitoring for other side effects reported in adults on long-term bisphosphonate therapy (including osteonecrosis of the jaw and atypical femur fractures) is also necessary and underscores the importance of bisphosphonate therapy in the hands of an osteoporosis treatment expert. A full discussion of appropriate doses, potential side effects, and steps to ensure patient safety on bisphosphonate therapy is beyond the scope of these core recommendations, but these issues are comprehensively discussed in recent reviews.9,26,38
Treatment: Osteoporosis Maintenance Phase and Discontinuation of Osteoporosis Therapy
Risk factors for ongoing bone fragility are inherently persistent in DMD (ie, the myopathy ± glucocorticoid therapy). Therefore, once the patient is clinically stable (see Fig 2 for the definition of clinically stable in the osteoporosis setting), consideration should be given to continuing IV therapy but at a lower dose.39 The goal of this approach is to preserve the clinical gains achieved during the stabilization phase while avoiding overtreatment. Vertebral body reshaping after VF is a frequently overlooked treatment goal, one that occurs only when bisphosphonate therapy is administered to patients during the growth phase (Fig 3). This phenomenon underscores the critical importance of treating signs of vertebral collapse earlier rather than later, so that treatment can be administered as far in advance of epiphyseal closure as possible. On the other hand, patients with DMD often manifest growth deceleration and even growth arrest because of the toxic effects of glucocorticoids on the growth plate. In such cases, the potential for vertebral body reshaping is limited, and the goals of therapy then become prevention of new VF and associated back pain, because reshaping of existing VF may not be realistic depending on the magnitude of the growth failure. In our experience, new VFs are more likely in those who start bisphosphonates following severe vertebral collapse after years of glucocorticoid therapy; highlighted in this observation is the importance of early rather than late identification and treatment of VF.
FIGURE 3.
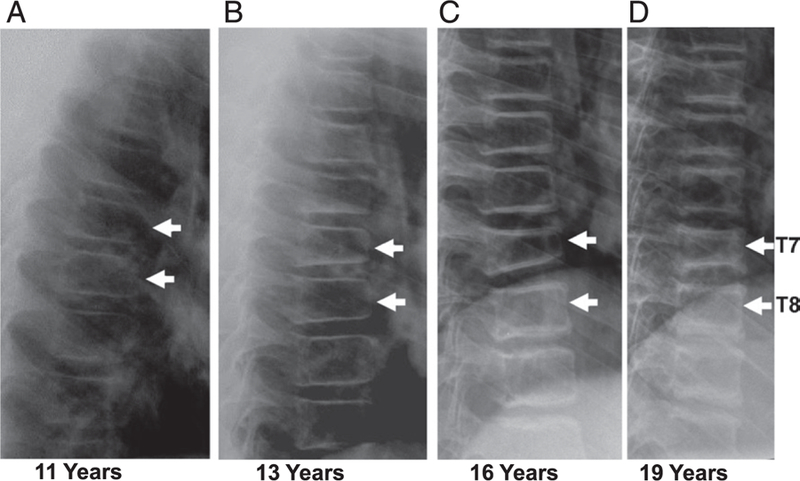
The evolution of spine morphology in a patient with DMD treated with glucocorticoid followed by IV bisphosphosphonate therapy for painful VFs. This figure is used to illustrate changes in vertebral morphology during glucocorticoid and IV bisphosphonate therapy. A, Early asymptomatic signs of T7 and T8 VFs on glucocorticoid therapy. B, Progressive vertebral collapse with an emergence of back pain triggering IV pamidronate therapy. C and D, Vertebral body reshaping on IV pamidronate therapy. Vertebral body reshaping is a growth-dependent process that is facilitated by bone strengthening therapy. The extent to which vertebral bodies can undergo reshaping on bisphosphonate therapy is determined by a number of clinical factors, including the degree of collapse, growth velocity, severity of ongoing risk factors for osteoporosis, and the magnitude of residual growth potential (before epiphyseal fusion). Patients with poor growth velocity have less potential for reshaping, as do patients who start therapy with more severe collapse and who are closer to attaining their final adult height. T7, Thoracic vertebra 7; T8, Thoracic vertebra 8.
The duration of maintenance therapy depends on the patient’s bone health status (whether clinically stable or not) and whether glucocorticoid therapy is ongoing. When bisphosphonate therapy is discontinued during the growth phase, the newly formed bone adjacent to the growth plate (ie, the treatment-naive bone) is once again low density, creating a stress riser between the treated and treatment-naive bone. Metaphyseal fractures have been observed at the interface between the treated and untreated bone in children after treatment is discontinued.40 This observation has led to the general recommendation in children that bisphosphonate therapy should be continued at least until the end of final height in those with persistent or permanent risk factors for osteoporosis41 (including glucocorticoid therapy and myopathy as in DMD) and, as a minimum, even beyond final adult height if the patient is not yet clinically stable. With Fig 2, we outline the definition of clinically stable in patients undergoing osteoporosis treatment.
No studies have been used to address which BMD increment or cutoff is associated with a clinically acceptable decrease in fracture rates that would categorize the patient as stable once achieving final adult height. In the absence of such data, it is recommended that the areal BMD z score should stabilize (if previously on the decline) or increase beyond the precision of the measurement, and furthermore, the areal BMD z score should approximate the patient’s height z score.25 Another approach is to aim for a BMD z score >−2.0.42
If a patient deteriorates after treatment is discontinued (ie, presents with a new VF, worsening of existing VF, or a low-trauma extremity fracture after adult height attainment and after bisphosphonate cessation), then reinitiation of treatment is indicated. At present, the benefits and risks of drug holidays (periods of bisphosphonate discontinuation) in pediatric or adult patients with DMD (all of whom have permanent bone heath threats and thereby at least the theoretical need for ongoing bone protection) remain uncertain. Although rare, atypical femur fractures on bisphosphonate therapy have led care providers for adult postmenopausal osteoporosis to consider drug holidays for those with a low risk of first-ever fractures and for those with a moderate risk who are clinically well after 3 to 5 years of therapy.43 High-risk adult patients (those with a history of bone fragility or a T score ≤−2) are not considered candidates for drug holidays.43 In practical terms, our current recommendations are to treat the pediatric patient with DMD according to the IV bisphosphonate initiation guidelines outlined here and then continue until final adult height is attained. After final adult height is attained, the course of action is less clear. One approach is to discontinue therapy if the patient is clinically stable (as defined in Fig 2). Monitoring should then be continued, and if fractures recur, treatment can be reinitiated. The other approach is to adopt the adult criteria for deciding to institute drug holidays. In this case, patients should not take drug holidays based on current adult guidelines because the risk of VF in DMD patients increases with age.44 Further research is required to determine the optimal efficacy and safety with these long-term bisphosphonate approaches in DMD.
FUTURE DIRECTIONS IN OSTEOPOROSIS MANAGEMENT FOR DMD
The most pressing need is for a large-scale, well-designed osteoporosis prevention trial in which medical therapy is started around the time of diagnosis or glucocorticoid initiation to prevent the first fracture. The challenge with such a trial is achieving an adequate sample size to assess differences between the treated and control groups for VF and non-VF outcomes; assessing only surrogates for bone strength (bone biomarkers and BMD) does not address the clinical end points that are most relevant to the patient. In the context of such a trial, patients will receive therapy before a fracture would have occurred naturally, so the safety of such an approach warrants rigorous scrutiny. Secondly, more convenient antiresorptive agents (such as denosumab) merit further study. Because patients may experience some degree of progressive vertebral height loss even on IV bisphosphonate therapy if therapy is started once VFs are in more advanced stages of collapse,45 the question is whether treatment before the first-ever VF will be even more successful in maintaining the height of vertebral bodies rather than starting treatment once collapse is evident and the VF cascade is in motion. Thirdly, it remains unanswered whether bone anabolic agents will improve efficacy given the low bone turnover in DMD patients.45 Antisclerostin antibody is one such promising agent. Another anabolic agent, teriparatide, has an FDA “black box” label for patients with open epiphyses but is a logical agent for study in DMD once final adult height is attained.
ACKNOWLEDGMENTS
We thank Victor Konji for his assistance in the preparation of references and figures for the manuscript. Dr Leanne M. Ward was supported by the Canadian Institutions for Health Research Operating Grants Program, the Canadian Child Health Clinician Scientist Program, the Children’s Hospital of Eastern Ontario Research Institute, the University of Ottawa Research Chair Program, and the Children’s Hospital of Eastern Ontario Departments of Pediatrics and Surgery.
FUNDING: Dr Ward is supported by a research chair from the University of Ottawa. This publication was supported in part by the cooperative agreement, NU38OT000167, funded by the Centers for Disease Control and Prevention.
ABBREVIATIONS
- 25OHD
25-hydroxyvitamin D
- BMD
bone mineral density
- DMD
Duchenne muscular dystrophy
- IV
intravenous
- VF
vertebral fracture
Footnotes
FINANCIAL DISCLOSURE: Other than those listed under Potential Conflict of Interest, the other authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: Dr Ward was a consultant to and participated in clinical trials with Novartis; Dr Weber was a paid consultant for Marathon Pharmaceuticals; and Drs Hadjiyannakis, McMillan, and Noritz have indicated they have no potential conflicts of interest to disclose.
The guidelines or recommendations in this article are not American Academy of Pediatrics policy and publication herein does not imply endorsement.
REFERENCES
- 1.Ma J, McMillan HJ, Karagüzel G, et al. The time to and determinants of first fractures in boys with Duchenne muscular dystrophy. Osteoporos Int 2017;28(2):597–608 [DOI] [PubMed] [Google Scholar]
- 2.McAdam LC, Rastogi A, Macleod K, Douglas Biggar W. Fat Embolism Syndrome following minor trauma in Duchenne muscular dystrophy. Neuromuscul Disord 2012;22(12):1035–1039 [DOI] [PubMed] [Google Scholar]
- 3.Medeiros MO, Behrend C, King W, Sanders J, Kissel J, Ciafaloni E. Fat embolism syndrome in patients with Duchenne muscular dystrophy. Neurology 2013;80(14):1350–1352 [DOI] [PubMed] [Google Scholar]
- 4.Gordon KE, Dooley JM, Sheppard KM, MacSween J, Esser MJ. Impact of bisphosphonates on survival for patients with Duchenne muscular dystrophy. Pediatrics 2011;127(2). Available at: www.pediatrics.org/cgi/content/full/127/2/e353 [DOI] [PubMed] [Google Scholar]
- 5.Larson CM, Henderson RC. Bone mineral density and fractures in boys with Duchenne muscular dystrophy. J Pediatr Orthop 2000;20(1):71–74 [PubMed] [Google Scholar]
- 6.McDonald DG, Kinali M, Gallagher AC, et al. Fracture prevalence in Duchenne muscular dystrophy. Dev Med Child Neurol 2002;44(10):695–698 [DOI] [PubMed] [Google Scholar]
- 7.King WM, Ruttencutter R, Nagaraja HN, et al. Orthopedic outcomes of long-term daily corticosteroid treatment in Duchenne muscular dystrophy. Neurology 2007;68(19):1607–1613 [DOI] [PubMed] [Google Scholar]
- 8.Tian C, Wong BL, Hornung L, et al. Bone health measures in glucocorticoid-treated ambulatory boys with Duchenne muscular dystrophy. Neuromuscul Disord 2016;26(11):760–767 [DOI] [PubMed] [Google Scholar]
- 9.Birnkrant DJ, Bushby K, Bann CM, et al. ; DMD Care Considerations Working Group. Diagnosis and management of Duchenne muscular dystrophy, part 2: respiratory, cardiac, bone health, and orthopaedic management. Lancet Neurol 2018;17(4):347–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crabtree NJ, Arabi A, Bachrach LK, et al. ; International Society for Clinical Densitometry. Dual-energy x-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD Pediatric Official Positions. J Clin Densitom 2014;17(2): 225–242 [DOI] [PubMed] [Google Scholar]
- 11.Henderson RC, Berglund LM, May R, et al. The relationship between fractures and DXA measures of BMD in the distal femur of children and adolescents with cerebral palsy or muscular dystrophy. J Bone Miner Res 2010;25(3): 520–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zemel BS, Stallings VA, Leonard MB, et al. Revised pediatric reference data for the lateral distal femur measured by Hologic Discovery/Delphi dual-energy x-ray absorptiometry. J Clin Densitom 2009;12(2):207–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greulich WW, Pyle SI. Radiographic Atlas of Skeletal Development of the Hand and Wrist 2nd ed. Stanford, CA: Stanford University Press; 1959 [Google Scholar]
- 14.Kröger H, Kotaniemi A, Vainio P, Alhava E. Bone densitometry of the spine and femur in children by dual-energy x-ray absorptiometry. Bone Miner 1992;17(1):75–85 [DOI] [PubMed] [Google Scholar]
- 15.Zemel BS, Kalkwarf HJ, Gilsanz V, et al. Revised reference curves for bone mineral content and areal bone mineral density according to age and sex for black and non-black children: results of the bone mineral density in childhood study. J Clin Endocrinol Metab 2011;96(10):3160–3169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LeBlanc CM, Ma J, Taljaard M; Canadian STeroid-Associated Osteoporosis in Pediatric Population (STOPP) Consortium, et al. Incident Vertebral Fractures and Risk Factors in the First Three Years Following Glucocorticoid Initiation Among Pediatric Patients With Rheumatic Disorders. J Bone Miner Res 2015;30(9):1667–1675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D Washington, DC: The National Academies Press; 2011 [PubMed] [Google Scholar]
- 18.Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. ; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96(7):1911–1930 [DOI] [PubMed] [Google Scholar]
- 19.Holick MF, Biancuzzo RM, Chen TC, et al. Vitamin D2 is as effective as vitamin D3 in maintaining circulating concentrations of 25-hydroxyvitamin D. J Clin Endocrinol Metab 2008;93(3):677–681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Armas LA, Hollis BW, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab 2004;89(11):5387–5391 [DOI] [PubMed] [Google Scholar]
- 21.Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B. The Faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain 2001;93(2):173–183 [DOI] [PubMed] [Google Scholar]
- 22.Genant HK, Wu CY, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8(9):1137–1148 [DOI] [PubMed] [Google Scholar]
- 23.Halton J, Gaboury I, Grant R, et al. ; Canadian STOPP Consortium. Advanced vertebral fracture among newly diagnosed children with acute lymphoblastic leukemia: results of the Canadian Steroid-Associated Osteoporosis in the Pediatric Population (STOPP) research program. J Bone Miner Res 2009;24(7):1326–1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaremko JL, Siminoski K, Firth GB, et al. ; Canadian STOPP Consortium National Pediatric Bone Health Working Group. Common normal variants of pediatric vertebral development that mimic fractures: a pictorial review from a national longitudinal bone health study. Pediatr Radiol 2015;45(4):593–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ward LM, Konji VN, Ma J. The management of osteoporosis in children. Osteoporos Int 2016;27(7):2147–2179 [DOI] [PubMed] [Google Scholar]
- 26.Bachrach LK. Diagnosis and treatment of pediatric osteoporosis. Curr Opin Endocrinol Diabetes Obes 2014;21(6): 454–460 [DOI] [PubMed] [Google Scholar]
- 27.Gatti D, Antoniazzi F, Prizzi R, et al. Intravenous neridronate in children with osteogenesis imperfecta: a randomized controlled study. J Bone Miner Res 2005;20(5):758–763 [DOI] [PubMed] [Google Scholar]
- 28.Antoniazzi F, Zamboni G, Lauriola S, Donadi L, Adami S, Tatò L. Early bisphosphonate treatment in infants with severe osteogenesis imperfecta. J Pediatr 2006;149(2):174–179 [DOI] [PubMed] [Google Scholar]
- 29.Aström E, Jorulf H, Söderhäll S. Intravenous pamidronate treatment of infants with severe osteogenesis imperfecta. Arch Dis Child 2007;92(4):332–338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ward LM, Glorieux FH, Rauch F, Verbruggen N, Heyden N, Lombardi A. A randomized, placebo-controlled trial of oral alendronate in children and adolescents with osteogenesis imperfecta. Bone 2005;36(S1):0–18 [Google Scholar]
- 31.Rauch F, Munns CF, Land C, Cheung M, Glorieux FH. Risedronate in the treatment of mild pediatric osteogenesis imperfecta: a randomized placebo-controlled study. J Bone Miner Res 2009;24(7):1282–1289 [DOI] [PubMed] [Google Scholar]
- 32.Sakkers R, Kok D, Engelbert R, et al. Skeletal effects and functional outcome with olpadronate in children with osteogenesis imperfecta: a 2-year randomised placebo-controlled study. Lancet 2004;363(9419):1427–1431 [DOI] [PubMed] [Google Scholar]
- 33.Ward LM, Denker AE, Porras A, et al. Single-dose pharmacokinetics and tolerability of alendronate 35- and 70-milligram tablets in children and adolescents with osteogenesis imperfecta type I. J Clin Endocrinol Metab 2005;90(7):4051–4056 [DOI] [PubMed] [Google Scholar]
- 34.Ward LM, Rauch F. Oral bisphosphonates for paediatric osteogenesis imperfecta? Lancet 2013;382(9902):1388–1389 [DOI] [PubMed] [Google Scholar]
- 35.Vuorimies I, Toiviainen-Salo S, Hero M, Mäkitie O. Zoledronic acid treatment in children with osteogenesis imperfecta. Horm Res Paediatr 2011;75(5): 346–353 [DOI] [PubMed] [Google Scholar]
- 36.Glorieux FH, Bishop NJ, Plotkin H, Chabot G, Lanoue G, Travers R. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med 1998;339(14):947–952 [DOI] [PubMed] [Google Scholar]
- 37.Weber DR, Hadjiyannakis S, McMillan HJ, Nortiz G, Ward LM. Obesity and endocrine management of the patient with Duchenne muscular dystrophy. Pediatrics 2018;142(suppl 2):e20180333F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mäkitie O. Causes, mechanisms and management of paediatric osteoporosis. Nat Rev Rheumatol 2013;9(8):465–475 [DOI] [PubMed] [Google Scholar]
- 39.Biggin A, Zheng L, Briody JN, Coorey CP, Munns CF. The long-term effects of switching from active intravenous bisphosphonate treatment to low-dose maintenance therapy in children with osteogenesis imperfecta. Horm Res Paediatr 2015;83(3): 183–189 [DOI] [PubMed] [Google Scholar]
- 40.Rauch F, Cornibert S, Cheung M, Glorieux FH. Long-bone changes after pamidronate discontinuation in children and adolescents with osteogenesis imperfecta. Bone 2007;40(4):821–827 [DOI] [PubMed] [Google Scholar]
- 41.Rauch F, Glorieux FH. Bisphosphonate treatment in osteogenesis imperfecta: which drug, for whom, for how long? Ann Med 2005;37(4):295–302 [DOI] [PubMed] [Google Scholar]
- 42.Palomo T, Fassier F, Ouellet J, et al. Intravenous bisphosphonate therapy of young children with osteogenesis imperfecta: skeletal findings during follow up throughout the growing years. J Bone Miner Res 2015;30(12):2150–2157 [DOI] [PubMed] [Google Scholar]
- 43.Brown JP, Morin S, Leslie W, et al. Bisphosphonates for treatment of osteoporosis: expected benefits, potential harms, and drug holidays. Can Fam Physician 2014;60(4): 324–333 [PMC free article] [PubMed] [Google Scholar]
- 44.Buckner JL, Bowden SA, Mahan JD. Optimizing bone health in Duchenne muscular dystrophy. Int J Endocrinol 2015;2015:928385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sbrocchi AM, Rauch F, Jacob P, et al. The use of intravenous bisphosphonate therapy to treat vertebral fractures due to osteoporosis among boys with Duchenne muscular dystrophy. Osteoporos Int 2012;23(11): 2703–2711 [DOI] [PubMed] [Google Scholar]