Abstract
Background
A thorough review of the available orthopaedic literature shows significant controversies, inconsistencies and sparse data regarding the terminology used to describe foot deformities. This lack of consensus on terminology creates confusion in professional discussions of foot anatomy, pathoanatomy and treatment of deformities. The controversies apply to joint movements as well as static relationships between the bones.
Description
The calcaneopedal unit (CPU) is a specific anatomical and physiological entity, represented by the entire foot excepted the talus. The calcaneus, midfoot and forefoot are solidly bound by three strong ligaments that create a unit that articulates with the talus. The movement of the CPU is complex, as it rotates under the talus, around the axis of Henke that coincides with the talo-calcaneal ligament of Farabeuf.
This calcaneopedal unit is deformable. It is compared with a twisted plate, able to adapt to many physiological situations in standing position, in order to acheive a plantigrade position.
Moreover, the calcaneopedal unit and the talo-tibiofibular complex are interdependent; rotation of the latter produces morphologic modifications inside the former and vice versa.
Purpose
This paper is a review article of this concept and of its physiopathological applications.
Keywords: calcaneopedal unit, foot biomechanics, talocalcaneonavicular joint
Introduction
A thorough review of the available orthopaedic literature shows significant controversies, inconsistencies and sparse data regarding the terminology used to describe foot deformities. This lack of consensus on terminology creates confusion in professional discussions of foot anatomy, pathoanatomy and treatment of deformities. The controversies apply to joint movements as well as static relationships between the bones.
The terms varus and valgus are often used to describe deformities in the forefoot and the hindfoot. They are frequently used interchangeably with the terms supination and pronation, inversion and eversion, and adduction and abduction. This is mostly due to the multiple biomechanical theories and concepts that have been applied to the foot.1-5
Before attempting to bring consistency and reason to the terminology, a good understanding of foot mechanics is mandatory.
In 1803, Scarpa6 proposed an analogy between movements in the hindfoot and those in the hip joint, thereby developing the concept of the ‘acetabulum pedis’. He saw similarities in the way the femoral head rotated within the acetabulum of the pelvis and the talar head/talus rotated within the ‘acetabulum’ of the subtalar joint, which he defined as the articular surfaces of the navicular and the calcaneus as well as the spring ligament.6-10 Around 25 years later, Delpeche11 reported on the movement of the calcaneus under the talus when the foot is adducted: “...when the foot moves inward, the calcaneus rolls as a cylinder and swings at the same time, almost horizontally under the posterior part of the astragalus (talus); in such a way that the inferior aspect of the first one of these two bones (i.e. the calcaneus) rotates inward, and its anterior part slides in the same direction, under the head of the second (i.e. the astragalus)...”. In Duchenne de Boulogne’s book, Physiologie des Mouvements,12 published in 1867, he devoted a chapter of 200 pages to ‘the foot’. In it he describes, in a very clear manner, the different muscular activities in the foot with the corresponding joint movements. He described a certain rotation of the foot under the ‘astragalus (talus) and the leg’.12 These early great thinkers and authors laid the foundation for the second wave of pioneering work on foot biomechanics lead by Méary in 1967 and Queneau in 1977.13 Their research and writings led to the concept of and the terminology for, the calcaneopedal unit (CPU).
The CPU is a specific anatomical and physiological entity, represented by the entire foot excepted the talus. The calcaneus, midfoot and forefoot are solidly bound by strong ligaments that create a unit that articulates with the talus. The movement of the CPU is complex, as it rotates under the talus around the axis constituted by the talo-calcaneal ligament of Farabeuf. Additionally, CPU is deformable. The bones that constitute it move to small degrees in relation to each other in order to maintain a plantigrade foot in stance. Moreover, it seems to have a close interdependence with the talo-tibiofibular unit, so that any movement of the latter produces an adaptive or compensatory movement and/or deformity of the former. Although this concept is old and very useful for the understanding of the foot mechanics, we did not find any detailed description about it in the orthopaedic literature of the last 60 years, with exception of an article written by Seringe and Wicart in 2013.9
The purpose of this paper is to review the anatomical and biomechanical aspects of the CPU concept, to use them in the analysis of some foot deformities, and to explore them in the planning of treatment, taking into consideration the ultimate functional position of the foot, i.e. standing.
Functional anatomy of the normal foot
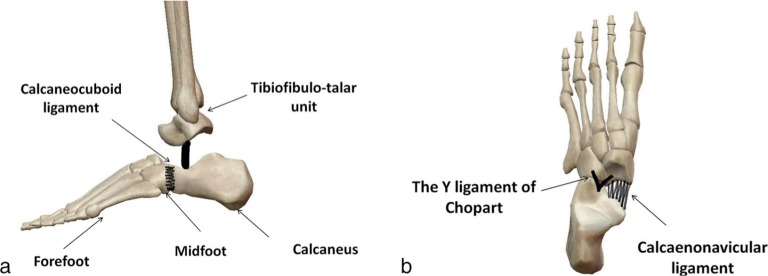
The CPU is made up of the calcaneus, the midfoot and the forefoot (Fig. 1a), solidly bound by the calcaneocuboid ligament, the bifurcate ligament (Y ligament of Chopart) and the inferior calcaneonavicular ligament (glenoid or spring ligament) (Figs 1a and 1b). It represents a functional unit that articulates with the talus through four articular components: the posterior, middle and anterior subtalar, and the talonavicular joints.14 The talus does not belong to the foot CPU; it rather belongs to the same functional unit as the tibia and fibula, with which it forms the talo-tibiofibular complex4,5,12,15 (Fig. 1a).
Fig. 1.
The calcaneopedal block is formed by the calcaneus, the midfoot and the forefoot; it articulates with the talus (talo-tibiofibular unit) and is bounded by the calcaneocuboid ligament (a), the Y ligament of Chopart and the calcaneonavicular ligament (b).
This concept, in addition to an oblique division of the foot, is complementary to the traditional and commonly used separations of the foot: 1) the transverse division between hindfoot, midfoot and forefoot; and 2) the longitudinal division between the medial arch (three medial rays) and the lateral arch (two lateral rays). This concept goes along with the ‘acetabulum pedis’ concept of Scarpa6,9 where the articular surface of the navicular, the anterior and middle articular facets of the calcaneus and the dorsal part of the spring ligament form a socket (or acetabulum) in which the talar head articulates. In this ball and socket concept, it is the socket (acetabulum pedis) that rotates three-dimensionally around the ball (talar head).6,7,9,10
The CPU has 3D mobility around an oblique axis (the Henke axis) that is, on average, 41° dorsiflexed and 23° internally rotated.14-16 This imaginary axis enters the talus at the upper medial aspect of its neck, passes through the deep part of the talocalcaneal interosseous ligament and emerges at the posterior lateral aspect of the calcaneus15-19 (Fig. 2).
Fig. 2.
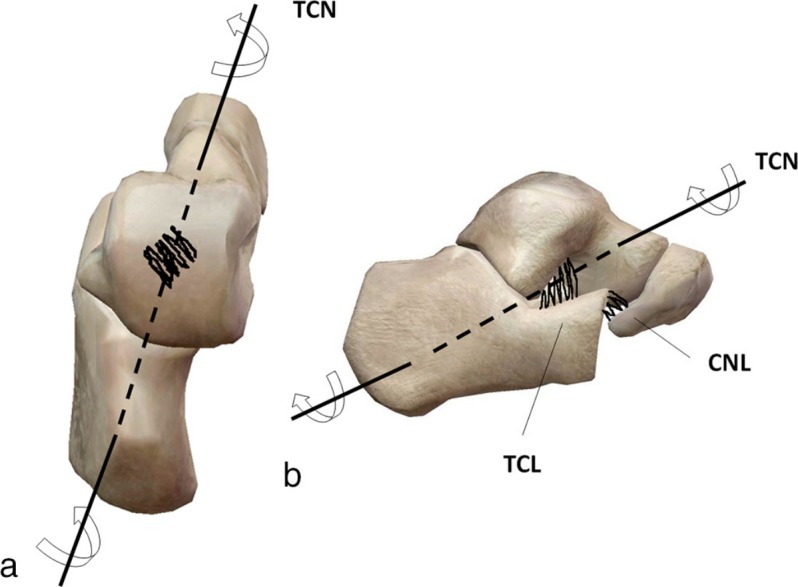
(a) Transverse view of the talocalcaneonavicular joint (TCN, talocalcaneonavicular axis); (b) sagittal view of the talocalcaneonavicular joint. The TCN passes through the interosseous talocalcaneal ligament (TCL) (CNL, calcaneonavicular ligament).
The combination of the four joints mentioned above rotating three-dimensionally around the non-orthogonal Henke axis creates movements that give the subtalar joint complex the appearance of an enarthrosis, or ball and socket joint, although it is not truly a ball and socket joint like the hip or shoulder. Its proximity and coordinated movements with the pure dorsiflexion-plantar flexion ankle joint further create the false appearance of a true enarthrosis in the hindfoot. The subtalar joint complex would best be described as a constrained ball and socket joint that rotates three-dimensionally and simultaneously around a fixed oblique axis.10,15,20 All movements are combinations of rotations rather than pure linear angular movements because the axis of movement is not in any of the the three orthogonal planes, i.e. sagittal, coronal or transverse. Inward movement, that would be termed adduction at other joints, is actually a combination of internal rotation, plantar flexion and supination of the CPU. Outward movement, that would be termed abduction at other joints, is actually a combination of external rotation, dorsiflexion and pronation of the CPU. For that reason, the movements of the CPU should have their own unique terms, the most descriptive being inversion and eversion.
The CPU itself is intrinsically deformable, due to the reciprocal rotations of the multiple bony elements that constitute it. The following characteristics describe this deformability clearly and are outlined below.
The dual anatomy and function of the talonavicular joint
The talonavicular joint is the medial component of Chopart’s transverse joints as well as the anterior-most aspect of the acetabulum pedis in the CPU. Unlike the essentially immobile calcaneo-cuboid joint, which is the lateral component of Chopart’s joints, the talonavicular joint is a proxy for the entire subtalar joint complex as it moves three-dimensionally with inversion and eversion. That said, there is some subtle movement and adaptive flexibility at the calcaneo-cuboid joint that is shared by the talonavicular joint.
Medial and lateral arches interdependence law
The medial and lateral arches interdependence law stipulates that every time the fifth metatarsal is displaced superiorly, the first metatarsal is displaced inferiorly, and vice versa.2,15 This is due to a particular anatomical disposition through which a synchronism between both arches is always present. This synchronism is mostly represented by the combined and reciprocal pronation and supination between the forefoot and the hindfoot, which take place in the Chopart, the midtarsal and the tarsometatarsal joints. These joints are intrinsically mobile, and move initially in the same direction, in pronation or in supination. Each bone acts as a lever with regards to the other; their movement begins when one of these bones uses the adjacent bone as a fulcrum, and pushes the next one, which in its turn displaces another adjacent bone.
However, this interdependence between the medial and lateral arches of the foot is also related to the complex movement that takes place in the talocalcaneonavicular joint.
Load transmission
The CPU is excavated both in the frontal and the sagittal planes.3,15,18 When an axial load is applied to the dorsum of the foot, the lateral and medial arches act mechanically as a unique longitudinal arch. When axial load is applied, arch deformation in the coronal plane is similar to that found in the sagittal plane, but of less magnitude.
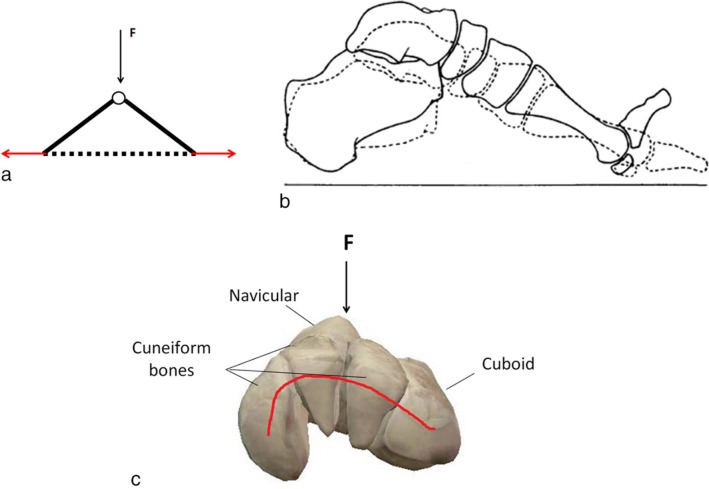
The longitudinal arch is a multisegmental arcuate structure that may behave as an arch, a truss or a curved beam.15 A truss is triangular in arrangement, with the sides formed by two articulated struts, and the base by a tie-rod, representing the plantar fascia. When an external vertical descending load is applied at the apex of the triangle, the struts are under compression and the tie-rod under tension. The strain transmission works through an imbalance between the different segments of the triangle (Fig. 3a). The longitudinal arch was also previously described by Hicks in 195421. He extended the tied arch model to a windlass defined by two rigid segments joined by a pin. He noted that arch raising movements and ray plantar flexion are synchronous (Fig. 3b). On another side, in tip toe standing, when the toes are hyperextended the arch rises and the distance between the calcaneus and the metatarsal heads is decreased. This mechanism is passive and independent of muscle action.
Fig. 3.
(a) The longitudinal arch of the foot represented by a truss (F, vertical descending load). The arrows represent the interior reaction forces; (b) the windlass mechanism described by Hicks in 1954:21 the arch raising movement and ray plantarflexion are synchronous; (c) the coronal arch of the foot may be represented by a uni- or a multisegmental arcuate structure: the load produces a compression force at the convexity, and a traction force at the concavity.
The coronal arch can be schematized by an arcuate unisegmental or multisegmental structure.15,18 A vertical descending load applied to its apex produces compression forces on the convex side and elongation forces on the concave side, i.e. on the plantar ligaments and fascia (Fig. 3c).
The lamina pedis and foot adaptability
MacConnaill and Basmajian22 compared the foot without the toes to a twisted plate, that he called lamina pedis. Structurally, the lamina pedis is formed by the calcaneopedal skeleton and the supportive ligaments. It is made up of two non-coplanar segments linked at the level of the tarsal joints (Fig. 4): the distal one is represented by the metatarsals, almost horizontal with minimal pronation; the proximal one is almost sagittal and represented by the hindfoot (the calcaneus). This twisted plate is flexible and allows the forefoot to adapt to any hindfoot rotation, and vice versa, with the main objective being to keep the foot in a well balanced plantigrade position. The supination of the forefoot in the standing position produces detorsion or untwisting of the lamina pedis with subsequent valgus of the hindfoot, in order to maintain a plantigrade position flat foot. The pronation of the forefoot produces the opposite phenomenon, with hindfoot varus and increased twisting of the lamina pedis (Fig. 4) resulting in cavovarus foot.9,15,23,24
Fig. 4.
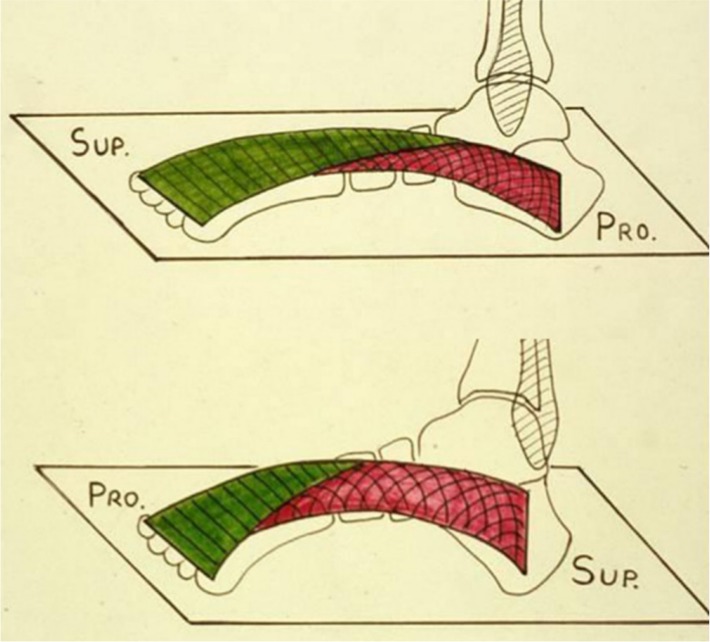
Lamina pedis (calcaneopedal unit) according to MacConnail and Basmajian22. An example of the adaptability of the twisted lamina pedis illustrated by Seringe and Wicart (2013):9 supination (Sup) of the forefoot is compensated by an untwisting of the lamina pedis with subsequent valgus of the hindfoot. In order to maintain a plantigrade position of the foot and vice versa, pronation (Pro) of the forefoot is compensated by a varus of the hindfoot. This figure has been reproduced with permission.
Conversely, a pronation twist of the lamina pedis relaxes the plantar fascia and is followed by a push and pull intersegmental movement at the tarsal and tarsometatarsal joints, as if playing the accordion. In mechanical terms, this is called a loose pack situation, and leads to an increase in medial arch height. The opposite phenomenon is noted during a supination twist of the forefoot, with a subsequent decrease in the height of both longitudinal and coronal arches of the foot.
Functional relationship between the CPU and the leg in the standing position
Rotation of the leg produces an identical axial rotation of the tibiofibulo-talar unit, with its three components rotating in the same direction. In the standing plantigrade position, external rotation of the leg is a rotation of the talo-tibiofibular unit above the CPU. The foot and, therefore, the CPU is fixed to the ground. For the talus to externally rotate, the CPU must internally rotate by means of inversion, i.e. internal rotation, plantar flexion and supination. The plantar flexion can be manifest through the subtalar joint with simultaneous plantar flexion of the ankle or the ankle can dorsiflex in compensation thereby maintaining vertical alignment of the leg. In other words, the CPU is now in varus with regard to the talo-tibiofibular unit. If the movement continues, it induces a deformation in torsion of the CPU with pronation of the forefoot. The hindfoot varus, in association with the forefoot pronation, produces a cavovarus deformity, through an increase in the height of the medial arch of the foot (the above-mentioned loose pack situation). The external rotation of the tibia thus produces a classic cavovarus deformity of the foot (Fig. 5).
Fig. 5.
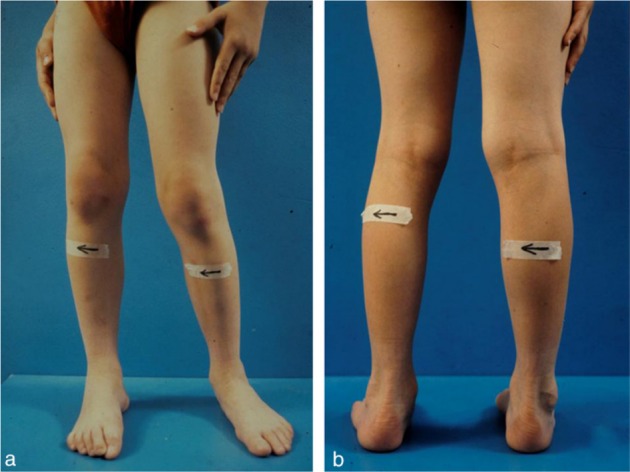
(a) Front view and (b) posterior view in the same standing position. When the patient is asked to turn the trunk and pelvis to the right, the right lower limb is subsequently externally rotated while the left lower limb is internally rotated, leading to a pes cavo-varus of the right foot and a pes plano-valgus of the left foot (from Seringe and Wicart 2013).9 This figure has been reproduced with permission.
Internal tibial rotation produces the opposite phenomenon, with subsequent hindfoot valgus, forefoot supination and flattening of the medial arch of the CPU. This internal rotation thus produces a classic planovalgus deformity of the foot (Fig. 5).
Terminology
Based on better knowledge of foot biomechanics, and especially what was presented above concerning the CPU concept, we recommend the following terminology for universal usage.
Varus and valgus describe fixed hindfoot angular deformities, regardless of the forefoot position. These terms apply to the frontal/coronal plane alignment of all bones and joints in the musculoskeletal system in which the distal part is angled medially or laterally in relation to the immediately more proximal part. Examples include genu varus/valgus, cubitus varus/valgus, hallux varus/valgus and varus/valgus malunion of a long bone fracture. In the subtalar joint complex, varus and valgus are the static alignment positions resulting from inversion and eversion deformities. Varus and valgus start by being adaptive and are thus flexible early in any foot pathology where they are observed, but end by becoming static and rigid with advancement and maintenance of the underlying pathology. In most cases, varus and inverted, as well as valgus and everted, are synonymous terms. In some cases, however, there is isolated varus or valgus deformity of the hindfoot without inversion or eversion. These are seen in some malformations and post-traumatic situations.
Inversion, which is a combination of internal rotation, plantar flexion and supination movements of the CPU, results in the static position synonymously termed varus or inverted. And eversion, which is a combination of external rotation, dorsiflexion and pronation movements of the CPU, results in the static position synonymously termed valgus or everted. Among all joints in the body, these movements are unique to the subtalar joint complex.
The terms pronation and supination should be used to describe the movements of the forefoot in relation to the hindfoot that result in the static deformities that are labelled pronated and supinated. Pronation refers to plantar flexion and internal rotation of the first metatarsal in realtion to the fifth metatarsal and the hindfoot. It is associated with an increased medial arch height. Supination is the opposite movement. It is associated with a decrease in the medial longitudinal arch. This simplistic description is used to describe the rotationally opposite relationships between the forefoot and the hindfoot.
Abduction and adduction are pure frontal/coronal plane angular movements (not deformities) of true ball and socket joints in the musculoskeletal system. The distal part rotates medially or laterally in relation to the more proximal part in the frontal/coronal plane. Fixed malpositions, termed abducted and adducted, can result. Examples include shoulder adduction contractures with rotator cuff tears and hip abduction contractures with poliomyelitis. In these examples, the shoulder is adducted and the hip is abducted. The CPU cannot purely abduct or adduct in the frontal/coronal plane because of the oblique axis of Henke that requires concurrent plantar flexion/internal rotation or dorsiflexion/external rotation. When the forefoot alone moves into abduction or adduction, an intrinsic deformation of the CPU takes place, with modification of the shape of the medial and lateral borders of the foot as in metatarsus adduction/adductus, however, when the CPU moves as a whole, there is no intrinsic deformation.
Flexion and extension are confusing terms when applied to the hindfoot. Plantar flexion and dorsiflexion are more clearly descriptive terms. Both movements occur in the ankle joint and the subtalar joint complex. The entire role of the ankle joint is plantar flexion and dorsiflexion. Plantar flexion of the CPU is a component of inversion that also includes internal rotation and supination, whereas dorsiflexion of the CPU is a component of eversion that also includes external rotation and pronation.
Biomechanical models
Biomechanical models of the foot were described to better understand foot kinematics in a dynamic situation. While deformations under load are routinely evaluated in a static position using radiographs or footprints,25-27 the assessment of these deformations in dynamic phases is possible using 3D motion capture systems. The optoelectronic system is mainly used to track markers placed on the foot. To date, and based on several reviews,28-31 there are no standard models to define foot mechanics. The single segment foot model is used in clinical gait analysis based on the model proposed by Davis in 1991.32 This model does not allow the appreciation of the foot kinematics including all its joints during gait. Many researchers introduced new modelling of the foot as a multi-segmented structure.33-36
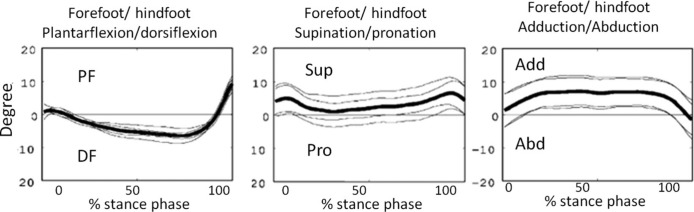
The Oxford model35 defines the hindfoot (calcaneus and talus), the forefoot (five metatarsals) and the hallux plus a tibia segment to study the ankle movement. Subsequently, the angular movement of the hindfoot with respect to the forefoot and the rotation of the hindfoot with respect to the tibia were described during the gait cycle in three anatomical planes. Quantifying the movement of the different segments of the foot with respect to the others permits a better understanding of the foot adaptability in dynamic phases. For instance, in the sagittal plane, the Oxford model shows a dorsiflexion of the forefoot during the mid-stance with respect to the hindfoot as the longitudinal arch of the foot flattens. In the coronal and transverse planes, supination and abduction of the forefoot are noticed and, subsequently, a restoration of the arch takes place (Fig. 6). Although this model is simplistic, it meets basic principles of CPU concepts where the leg is mechanically and intimately in relation with the hindfoot, which in turn shows mechanical interdependence with the forefoot.
Fig. 6.
The kinematics of the forefoot according to the hindfoot; example of a median trial of one subject with between-day 95% confidence interval of two testers (from Carson et al 2001)35 (PF, plantar flexion; DF, dorsiflexion; Sup, supination; Pro, pronation; Add, adduction; Abd, abduction). This figure has been reproduced with permission.
The Milwaukee foot model likewise describes three rigid body segments of the foot:34 hindfoot (calcaneus, talus and navicular), forefoot (cuneiforms, cuboid and metatarsals) and the hallux plus the tibia and fibula segments. The comparison of the kinematics between the two models is inappropriate because of the different definitions in the joint coordinate system of the foot segments.
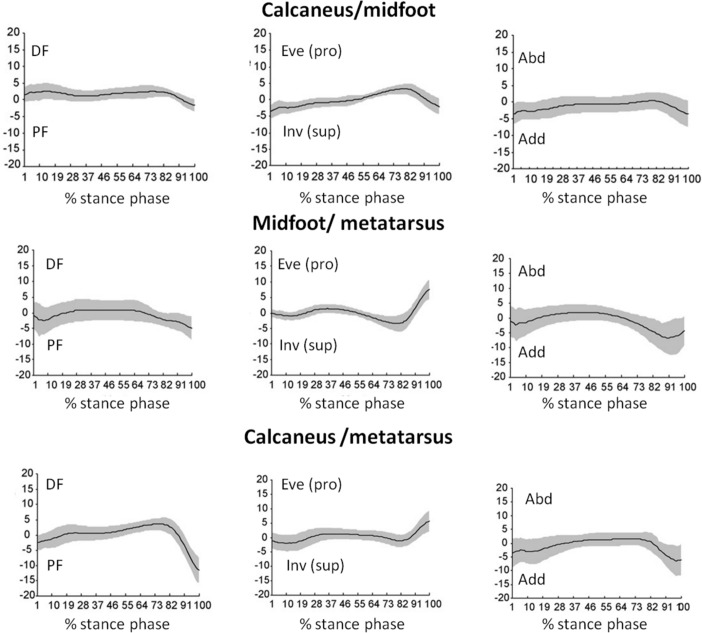
In order to track the movement of the midfoot during the stance phase, Leardini et al33 modelled five segments in the foot including the calcaneus, the mid-foot (lateral, middle and medial cuneiform and cuboid) and the metatarsus. Joint rotations were calculated according to the International Society of Biomechanics recommendations.37,38 For example, dorsi/plantar flexion is the rotation around the medio-lateral axis of the proximal segment, adduction/abduction is the rotation around the vertical axis of the distal segment, and eversion/inversion is the rotation around the axis orthogonal to the previous two axes. Eversion and inversion in this biomechanical model are equivalent to the pronation and supination according to the clinical terminology. Kinematics results showed a small range of movement of the calcaneus with respect to the midfoot in the three planes. However, synchronized movements are noticed at the late stance phase where the midfoot is dorsiflexed, everted (which is the equivalent of the pronation movement according to the clinical terminology) and abducted with respect to the calcaneus (Fig. 7). These rotations are reversed at the end of the stance phase where the midfoot becomes plantarflexed, inverted (which is the equivalent of the supination movement according to the clinical terminology) and adducted with respect to the calcaneus. Concerning the midfoot-metatarsal range of movement, it was limited as well in the three planes. At this level, a transition from supination at the late stance to 10° of pronation at the end of the stance is noticed. This could be related to the transition from lateral to medial forefoot contact with the floor necessary to stabilize the first metatarsus and to push off. The movement of the calcaneus with respect to the metatarsus could describe the windlass mechanism21 between the hindfoot and the forefoot. When the effect of the body weight tends to flatten the arch, an alignment of the calcaneus-metatarsus in the mid-stance is observed in the three planes (Fig. 7).33 Furthermore, the twist of the lamina pedis could be objectively quantified by the degrees of inversion and eversion, the equivalent of supination and pronation respectively, of the calcaneus with respect to the metatarsus (Fig. 7). At the end of the stance phase the large plantarflexion of the metatarsus is combined to a large dorsiflexion of the foot during this same phase provided by the windlass mechanism. The kinematics of the forefoot with regard to the hindfoot are in accordance with the arch raising mechanism seen during toe dorsiflexion as described by Hicks (1954),21 allowing a better understanding of foot adaptability during gait.
Fig. 7.
Mean value (black line) and sd (grey) of the movement of the calcaneus (cal) with respect to the midfoot (mid), the midfoot with respect to the metatarsus (Met) and the calcaneus with respect to the metatarsus of ten asymptomatic subjects. Dorsiflexion (DF), plantar flexion (PF), inversion (Inv), eversion (Eve), pronation (pro), supination (sup), abduction (Abd) and adduction (Add) are labelled (from Leardini et al 2007)33. This figure has been reproduced with permission.
The skin-mounted markers have their limits in the study of foot kinematics. These limits are related to skin movement artifacts, the multitude of small and adjacent foot segments, as well as uncertainties in the calculated angles.39
Therefore, the use of foot kinematic models in daily practice remains uncommon. The lack of uniformity and consensus concerning the marker placement, angular calculation and the definition of the neutral position of the foot has limited the application of multi-segmental foot modelling in clinical practice.31
Plantar pressure distribution measurements using pressure mapping techniques are also useful in understanding foot biomechanics. A relationship between foot structure and plantar pressure has already been reported in previous studies.40,41 The Arch Index has been shown to be the most important parameter to study the structure of the foot and is defined as the ratio of the midfoot area relative to the total area of the foot, excluding the toes.42 An increased or decreased arch index could indicate a pes planovalgus or cavovarus respectively. Another parameter, the Arch Index Contact Force Ratio, has also been described.43 It is calculated by dividing the contact force on the midfoot area by the contact force on the total foot area, excluding the toes. This index is also used to study foot deformities in children and has shown significant correlation with radiographic abnormalities.44
Physiopathological considerations
Congenital clubfoot or talipes equinovarus
The application of two general principles commonly used in biomechanics to foot physiology allows a better understanding of the mechanisms of foot deformation in congenital clubfoot:
The diadochal movements law (successive movements):45 in joints with three degrees of freedom (enarthrosis), two successive movements that take place in two different directions automatically produce a third movement in a third direction.
The convergent forces law:1,19,46 two convergent forces produce a movement corresponding to that obtained by their resultant force (Fig. 8a).
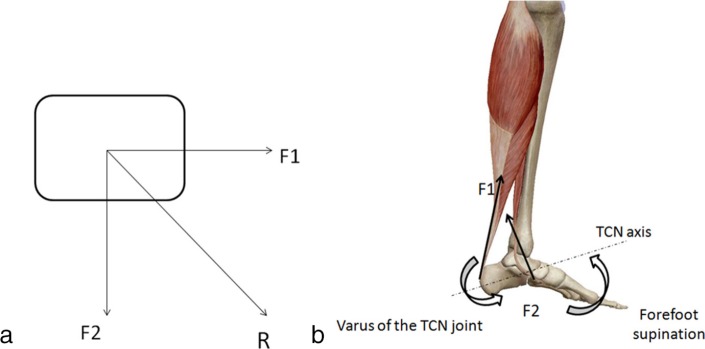
Fig. 8.
(a) A simplified schematic of two convergent forces (F1 and F2) applied on the same solid will produce a movement in the direction of their resultant (R); (b) schematic representation of the diadochal movements where the action of the triceps surae (F1) and posterior tibialis (F2) will produce a varus position of the talocalcaneonavicular (TCN) joint with regard to the forefoot. Subsequently an intrinsic deformity of the calcanealpedal unit is noted with an adduction-supination of the forefoot.
Based on the first law, equinus and adduction of the CPU produce an automatic varus of the hindfoot.14,47 Adduction of the forefoot with regards to the hindfoot in association with equinus48-50 produces an automatic pronation of the forefoot in relation to the hindfoot (Fig. 8b). Based on the second law, the equinus of the CPU produced by the triceps surae creates, in combination with the tibialis posterior (adductor and plantar flexor of the CPU and adductor-pronator of the forefoot with regards to the hindfoot), a force couple, which, unopposed by the weak peroneals, leads to medial and downward rotation of the CPU around the talocalcaneonavicular axis (inversion) and an adduction-pronation of the forefoot (Fig. 8b). In fact, the projection of the vectors of the forces produced by both muscles (triceps surae and tibialis posterior) or their equivalent representatives at the talocalcaneonavicular joint, produces two convergent forces, the resultant of which creates a global varus deformation of the CPU. The same reasoning could be applied to the forefoot position with regards to the hindfoot, with a subsequent adduction-pronation deformity of the former (intrinsic deformity of the CPU) (Fig. 8a). Retracted soft tissues, especially the medial tight capsules and ligaments between the medial malleolus and the calcaneus lock the diseased foot in adduction of the CPU and maintain the adduction of the forefoot with respect to the hindfoot.14 The fixed deformity, even if not severe, is aggravated by another deforming force. This additional deforming force comes from the tibialis anterior, the action of which is changed from a dorsiflexor, when the foot is plantigrade, to a supinator-elevator of the first ray when the foot is in varus-adduction-forefoot pronation. This is confirmed in some patients with or without residual congenital talipes equino varus (CTEV) deformity after conservative treatment who have dynamic foot supination. The increased functional supination is due to a strong, active tibialis anterior and relatively weaker peroneal musculature.51,52 In these cases, it is recommended to transfer the tibialis anterior laterally to treat the functional supination and to amplify foot eversion.51,52
Metatarsus adductus (erroneously called metatarsus varus)
There is an intrinsic deformity of the CPU, with the forefoot being in adduction and sometimes slight supination with regards to the hindfoot, which is not deformed. There is no global rotation of the CPU.
Pes convex or congenital vertical talus
The combined contracture of the triceps surae, the dorsiflexors of the midfoot/forefoot/toes (tibialis anterior, extensor hallucis longus, extensor digitorum communis, extensor hallucis brevis and peroneus tertius) and the dorsal aspect of the talonavicular joint capsule creates extrinsic and intrinsic deformities of the CPU that are located at Chopart’s midtarsal joints.53 There is ankle equinus in association with extreme eversion of the subtalar joint complex and a dorsal-lateral dislocation of the navicular on the head of the talus. The calcaneocuboid joint is either dorsally maloriented or the cuboid is dorsally subluxated on the calcaneus, depending on the severity of the deformity.53,54 The lamina pedis may be over or undertwisted, with a subsequent pronation or supination of the forefoot with regards to the calcaneus.
Pes cavovarus
This deformity is characterized by a primary increase in the pronation of the distal part of the lamina pedis, i.e. the forefoot, which is evident when the heel is kept in a neutral position.9,55,56 In this case, the height of the medial arch is increased. In the standing position, the posterior part of the lamina pedis, represented by the calcaneus, moves into varus in the talocalcaneonavicular joint, in order to compensate and recreate a plantigrade position of the foot. This constitutes an intrinsic deformity of the CPU. A subsequent external tibial rotation takes place (see above). If not treated, this deformity will become fixed with time.
Pes planovalgus
The deformation of the CPU is opposite to the one described for the pes cavovarus.9 When the heel is held in a neutral position, the forefoot is primarily in supination. In stance, the calcaneus moves into valgus in the talocalcaneonavicular joint, thus compensating for the forefoot deformity, and recreating a plantigrade position. This is an intrinsic deformity of the CPU.
Although it would have been interesting to discuss data for normal age-related values and pathological cut-offs, we believe that this topic is not in the aim of the current paper and would be interesting to address in a future work.
Therapeutic considerations
A better understanding of the pathomechanical function of foot deformities leads to a better planning of treatment. In cases where an intrinsic deformity of the CPU is also present (very frequently), we recommend to start with the correction of the forefoot deformity in order to restore a CPU of ‘normal morphology’. This is true in all cases except for fixed pes planovalgus where surgical correction should start at the hindfoot.10
In talipes equinovarus, treatment is directed towards the correction of the three components of the deformity.9 The three major therapeutic steps (regardless of the type of treatment, surgical or non surgical) are: 1) correction of forefoot adduction and pronation; 2) external derotation/eversion of the CPU; and 3) correction of the CPU and ankle equinus. Although not presented as such by its promotor, Ponseti’s gradual correction of clubfoot is based on the CPU concept. This is also true for the French functional method for clubfoot treatment. The thumb of one hand pushes against the talar head while the second hand manipulates the CPU in the opposite direction. This represents one of the best illustrations of how the CPU concept is applied in the most accepted methods of clubfoot treatment around the globe. This is also the reason why Kite casting is not very helpful in clubfoot and achieves only partial correction. In fact, in Kite casting, the fulcrum of rotation is not the talar head but rather the lateral aspect of the midtarsal or tarsometatarsal joints, which produces correction of forefoot pronation and adduction, but not of the CPU deformity. The Turco surgical treatment for clubfoot has been abandoned because it follows the same incorrect understanding of the deformities. The McKay surgical treatment for clubfoot is based on the true understanding of the CPU, as described herein, though it was developed before the present terminology was described. Release of the anteromedial knot of Henry and the retracted tight capsules and ligaments located between medial malleolus and the navicular,9 along with the lengthening of the tibialis posterior tendon, allow for total correction of the intrinsic deformity of the CPU, i.e. forefoot adduction and pronation, and part of the hindfoot varus-inversion. Posterolateral release improves rotation of the entire CPU underneath the talus, by freeing any attachments of the calcaneus to the peroneals and lateral malleolus. This improves global foot eversion by allowing the posterior calcaneus to move medially and the acetabulum pedis-anterior CPU to move laterally.
In metatarsus adductus, the correction of only the adducted forefoot is undertaken,57 the fulcrum of rotation being at the mid aspect of the lateral foot border.
In pes convex, the treatment (surgical or not) begins with correction of the dorsal subluxation/dislocation of the forefoot. Correction of CPU equinus is then undertaken.
In fixed pes cavovarus, the treatment (surgical or not) begins with correction of the pronation (and the cavus) of the forefoot. Correction of the hindfoot varus follows58 (Fig. 9).
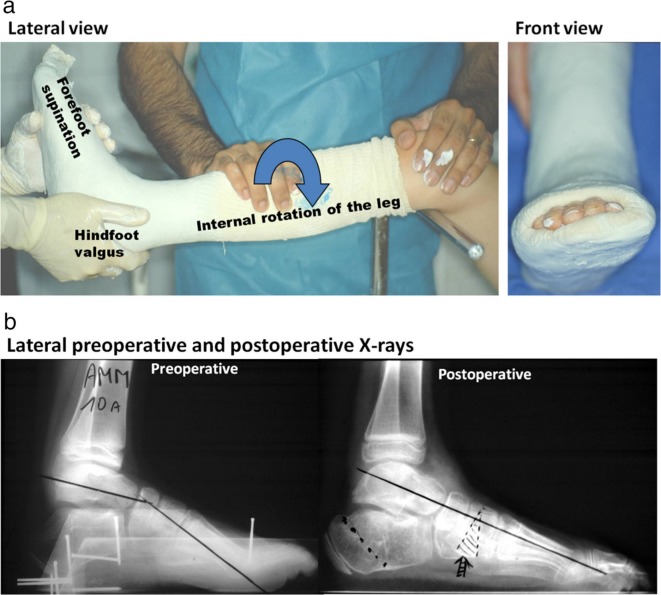
Fig. 9.
Treatment of the fixed pes cavo-varus: (a) nonoperative treatment where the leg is rotated internally and a force couple displaces the hindfoot into valgus and the forefoot into supination (from d’Astorg et al 2016;58 Wicart 201255); (b) operative treatment where a cuneiform plantar open wedge osteotomy and a selective plantar release are performed with a Dwyer lateral closed osteotomy of the calcaneus (from Wicart and Seringe 2006).56 These figures are reproduced with permission.
The most logical currently accepted surgical method of treatment in severe and symptomatic flexible pes planovalgus, the calcaneal lengthening osteotomy (CLO)10,59,60 (Fig. 10), is based on the CPU concept. Evans,59 the originator of the calcaneal lengthening concept, did not present it as such and perhaps did not truly understand it. Mosca,10,60 the developer of the most commonly used expanded method, based his technique on the CPU concept. The CLO inverts the acetabulum pedis along the axis of Henke, thereby directly correcting the anterior CPU with resultant indirect correction of the posterior CPU. The hindfoot valgus spontaneously corrects as the acetabulum pedis and talonavicular joint realign.
Fig. 10.
Operative treatment of the pes planovalgus according to the Evans calcaneal lengthening.
As discussed earlier, the forefoot in a flatfoot is supinated in relation to the hindfoot. It may be flexible or rigid. Realignment of the CPU with a CLO may uncover rigid intrinsic forefoot supination deformity. It doesn’t create it. In the majority of cases, this intrinsic forefoot supination deformity is flexible and corrects spontaneously following CLO, probably due to the relatively tight, acutely inextensible plantar fascia that forces the CPU bones to realign in the direction of cavovarus without any need for additional osteotomies.10,61-63
In severe and long-standing cases, the forefoot supination deformity is rigid and will require a medial column deformity correcting osteotomy.10,60,64 If the forefoot is supinated and adducted, a dorso-medially based opening wedge osteotomy of the medial cuneiform will simultaneously correct both deformities.10 If the forefoot is supinated and abducted or in neutral ab/adduction, a plantar based closing wedge osteotomy of the medial cuneiform is indicated.10
One other alternative for the treatment of symptomatic flat foot is the ‘triple C osteotomy’.65 This technique, modified by Rathjen and Mubarak66, includes a sliding-closing medial wedge calcaneal osteotomy, a plantar-closing wedge osteotomy of the medial cuneiform and an opening wedge osteotomy of the cuboid. A comparison study of the CLO and the triple-C led to comparable radiological and clinical outcomes.67 The CLO achieved better anatomical alignment of the navicular on the head of the talus than the triple C.65 The authors, who developed the triple C procedure, reported more technique related problems with the CLO, perhaps because of their unfamiliarity with the procedure.65
In conclusion, although the CPU concept is old, it seems very useful for the understanding of the foot’s normal and pathologic mechanics, and for the clarification and the unification of our language in the analysis of foot deformities. A logical and accurate functional terminology ensues and helps in planning the treatment of the most frequently encountered deformities.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: This article does not contain any studies with human participants performed by any of the authors.
Informed consent: Informed consent was not required.
ICMJE Conflict of interest statement
None of the authors have any conflict of interest to declare.
Author Contributions
IG: Writing the manuscript and literature review.
AM: Writing the manuscript and literature review.
AA: Writing the manuscript and literature review.
MR: Editing the manuscript and literature review.
AJB: Editing the manuscript and literature review.
REA: Editing the manuscript and literature revirew.
RS: Reviewing and editing the manuscript.
VM: Reviewing and editing the manuscript.
PW: Reviewing and editing the manuscript.
Acknowledgement
The authors would like to thank Mohamad Karam for help with the production of figures 1, 2 and 3c.
References
- 1.Hainault K. Introduction à la biomécanique. Paris: Presses Un. Maloine, 1971. [Google Scholar]
- 2.Hendrix G. The law of interdependence of the longitudinal arches of the foot applied to the surgery of inveterate clubfoot in the young child. Acta Orthop Belg 1962;28:8-14. [PubMed] [Google Scholar]
- 3.Lapidus PW. Kinesiology and mechanical anatomy of the tarsal joints. Clin Orthop Relat Res 1963;30:20-36. [PubMed] [Google Scholar]
- 4.Le Coeur P-F. La pince malléolaire. Physiologie normale et pathologique du péroné. Paris: L. Arnette, 1938. [Google Scholar]
- 5.Morris JM. Biomechanics of the foot and ankle. Clin Orthop Relat Res 1977;122:10-17. [PubMed] [Google Scholar]
- 6.Scarpa A. Memoria chirurgica sui piedi torti congeniti dei fanciulli : e sulla maniera di correggere questa deformita. Pavia: Presso Baldassare Comino, 1806. [Google Scholar]
- 7.Epeldegui T, Delgado E. Acetabulum pedis. Part I: Talocalcaneonavicular joint socket in normal foot. J Pediatr Orthop B 1995;4:1-10. [PubMed] [Google Scholar]
- 8.Epeldegui T, Delgado E. Acetabulum pedis. Part II: Talocalcaneonavicular joint socket in clubfoot. J Pediatr Orthop B 1995;4:11-16. [DOI] [PubMed] [Google Scholar]
- 9.Seringe R, Wicart P, French Society of Pediatric Orthopaedics . The talonavicular and subtalar joints: the “calcaneopedal unit” concept. Orthop Traumatol Surg Res 2013;99:S345-S355. [DOI] [PubMed] [Google Scholar]
- 10.Mosca VS. Principles and management of pediatric foot and ankle deformities and malformations. 1st ed. Philadelphia: Lippincott Williams & Wilkins, 2014. [Google Scholar]
- 11.Delpech JM. De l’orthomorphie. Paris: Gabon, 1828. [Google Scholar]
- 12.Duchenne de Boulogne GB. Physiologie des mouvements. Paris: J.-B. Baillière et fils, 1867. [Google Scholar]
- 13.Meary R. Le pied creux essentiel, 19ième réunion annuelle de la SOFCOT. Rev Chir Orthop Repar Appar Mot 1967;53:389-467. [PubMed] [Google Scholar]
- 14.Seringe R. Morbid anatomy of congenital equino-varus club foot. I - The osteo-articular defects at birth (author’s transl). Ann Chir 1977;31:107-111. [PubMed] [Google Scholar]
- 15.Kelikian AS, Sarrafian SK. Sarrafian’s anatomy of the foot and ankle: descriptive, topographic, functional. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2011. [Google Scholar]
- 16.Close JR, Inman VT, Poor PM, Todd FN. The function of the subtalar joint. Clin Orthop Relat Res 1967;50:159-179. [PubMed] [Google Scholar]
- 17.Delagoutte J, Bonnel F. Le pied: Pathologie et technique chirurgicale Paris: Masson & Cie, 1989. [Google Scholar]
- 18.Lelièvre J. Pathologie du pied. Paris: Masson & Cie, 1971. [Google Scholar]
- 19.Levangie PK, Norkin CC. Joint structure and function: a comprehensive analysis. 5th Ed. Philadelphia: F.A. Davis, 2011. [Google Scholar]
- 20.Hicks JH. The mechanics of the foot. I. The joints. J Anat 1953;87:345-357. [PMC free article] [PubMed] [Google Scholar]
- 21.Hicks JH. The mechanics of the foot. II. The plantar aponeurosis and the arch. J Anat 1954;88:25-30. [PMC free article] [PubMed] [Google Scholar]
- 22.MacConnail MA, Basmajian JV. Muscles and movements. A base for human kinesiology. Baltimore: Williams & Wilkins, 1969. [Google Scholar]
- 23.Rocher C, Rigaud A. Fonctions et bilans articulaires. Kinésithérapie et rééducation. Paris: Masson & Cie, 1964. [Google Scholar]
- 24.Rohan PY, Perrier A, Ramanoudjame M, et al. . Three-dimensional reconstruction of foot in the weightbearing position from biplanar radiographs: evaluation of accuracy and reliability. J Foot Ankle Surg 2018;57(5):931-937. [DOI] [PubMed] [Google Scholar]
- 25.Menz HB, Munteanu SE. Validity of 3 clinical techniques for the measurement of static foot posture in older people. J Orthop Sports Phys Ther 2005;35:479-486. [DOI] [PubMed] [Google Scholar]
- 26.Lamm BM, Mendicino RW, Catanzariti AR, Hillstrom HJ. Static rearfoot alignment: a comparison of clinical and radiographic measures. J Am Podiatr Med Assoc 2005;95:26-33. [DOI] [PubMed] [Google Scholar]
- 27.Gilmour JC, Burns Y. The measurement of the medial longitudinal arch in children. Foot Ankle Int 2001;22:493-498. [DOI] [PubMed] [Google Scholar]
- 28.Bishop C, Paul G, Thewlis D. Recommendations for the reporting of foot and ankle models. J Biomech 2012;45:2185-2194. [DOI] [PubMed] [Google Scholar]
- 29.Deschamps K, Staes F, Roosen P, et al. . Body of evidence supporting the clinical use of 3D multisegment foot models: a systematic review. Gait Posture 2011;33:338-349. [DOI] [PubMed] [Google Scholar]
- 30.Novak AC, Mayich DJ, Perry SD, Daniels TR, Brodsky JW. Gait analysis for foot and ankle surgeons - topical review, part 2: approaches to multisegment modeling of the foot. Foot Ankle Int 2014;35:178-191. [DOI] [PubMed] [Google Scholar]
- 31.Rankine L, Long J, Canseco K, Harris GF. Multisegmental foot modeling: a review. Crit Rev Biomed Eng 2008;36:127-181. [DOI] [PubMed] [Google Scholar]
- 32.Davis RB III, Õunpuu S, Tyburski D, Gage JR. A gait analysis data collection and reduction technique. Hum Mov Sci 1991;10:575-587. [Google Scholar]
- 33.Leardini A, Benedetti MG, Berti L, et al. . Rear-foot, mid-foot and fore-foot motion during the stance phase of gait. Gait Posture 2007;25:453-462. [DOI] [PubMed] [Google Scholar]
- 34.Kidder SM, Abuzzahab FS Jr, Harris GF, Johnson JE. A system for the analysis of foot and ankle kinematics during gait. IEEE Trans Rehabil Eng 1996;4:25-32. [DOI] [PubMed] [Google Scholar]
- 35.Carson MC, Harrington ME, Thompson N, O’Connor JJ, Theologis TN. Kinematic analysis of a multi-segment foot model for research and clinical applications: a repeatability analysis. J Biomech 2001;34:1299-1307. [DOI] [PubMed] [Google Scholar]
- 36.MacWilliams BA, Cowley M, Nicholson DE. Foot kinematics and kinetics during adolescent gait. Gait Posture 2003;17:214-224. [DOI] [PubMed] [Google Scholar]
- 37.Wu G, Siegler S, Allard P, et al. . ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, and spine. J Biomech 2002;35:543-548. [DOI] [PubMed] [Google Scholar]
- 38.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 1983;105:136-144. [DOI] [PubMed] [Google Scholar]
- 39.Okita N, Meyers SA, Challis JH, Sharkey NA. An objective evaluation of a segmented foot model. Gait Posture 2009;30:27-34. [DOI] [PubMed] [Google Scholar]
- 40.Morag E, Cavanagh PR. Structural and functional predictors of regional peak pressures under the foot during walking. J Biomech 1999;32:359-370. [DOI] [PubMed] [Google Scholar]
- 41.Teyhen DS, Stoltenberg BE, Collinsworth KM, et al. . Dynamic plantar pressure parameters associated with static arch height index during gait. Clin Biomech (Bristol, Avon) 2009;24:391-396. [DOI] [PubMed] [Google Scholar]
- 42.Cavanagh PR, Rodgers MM. The arch index: a useful measure from footprints. J Biomech 1987;20:547-551. [DOI] [PubMed] [Google Scholar]
- 43.Leung AKL, Cheng JCY, Zhang M, Fan Y, Dong X. Contact force ratio: a new parameter to assess foot arch function. Prosthet Orthot Int 2004;28:167-174. [DOI] [PubMed] [Google Scholar]
- 44.Elmoatasem EM, Eid MA. Assessment of the medial longitudinal arch in children with flexible pes planus by plantar pressure mapping. Acta Orthop Belg 2016;82:737-744. [PubMed] [Google Scholar]
- 45.MacConaill MA. Studies in the mechanics of synovial joints; fundamental principles and diadochal movements. Ir J Med Sci. 1946;21:190-199. [DOI] [PubMed] [Google Scholar]
- 46.Mow VC, Hayes WC. Basic orthopaedic biomechanics. New York: Raven Press, 1991. [Google Scholar]
- 47.Seringe R. Congenital equinovarus clubfoot. Acta Orthop Belg 1999;65:127-153. [PubMed] [Google Scholar]
- 48.Heywood AW. The mechanics of the hind foot in club foot as demonstrated radiographically. J Bone Joint Surg [Br] 1964;46-B:102-107. [PubMed] [Google Scholar]
- 49.Kaplan EB. Comparative anatomy of the talus in relation to idiopathic clubfoot. Clin Orthop Relat Res 1972;85:32-37. [DOI] [PubMed] [Google Scholar]
- 50.Settle GW. The anatomy of congenital talipes equinovarus: sixteen dissected specimens. J Bone Joint Surg [Am] 1963;45-A:1341-1354. [PubMed] [Google Scholar]
- 51.Thompson GH, Hoyen HA, Barthel T. Tibialis anterior tendon transfer after clubfoot surgery. Clin Orthop Relat Res 2009;467:1306-1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mulhern JL, Protzman NM, Brigido SA. Tibialis Anterior Tendon Transfer. Clin Podiatr Med Surg 2016;33:41-53. [DOI] [PubMed] [Google Scholar]
- 53.Miller M, Dobbs MB. Congenital vertical talus: etiology and management. J Am Acad Orthop Surg 2015;23:604-611. [DOI] [PubMed] [Google Scholar]
- 54.Seringe R, Martin G, Katti E, Vaquier J. Congenital convexity of the feet. Anatomical study and practical conclusions. Rev Chir Orthop Reparatrice Appar Mot 1990;76:234-244. [PubMed] [Google Scholar]
- 55.Wicart P. Cavus foot, from neonates to adolescents. Orthop Traumatol Surg Res 2012;98:813-828. [DOI] [PubMed] [Google Scholar]
- 56.Wicart P, Seringe R. Plantar opening-wedge osteotomy of cuneiform bones combined with selective plantar release and dwyer osteotomy for pes cavovarus in children. J Pediatr Orthop 2006;26:100-108. [DOI] [PubMed] [Google Scholar]
- 57.Kite JH. Congenital metatarsus varus; report of 300 cases. J Bone Joint Surg [Am] 1950;32-A:500-506. [PubMed] [Google Scholar]
- 58.d’Astorg H, Rampal V, Seringe R, Glorion C, Wicart P. Is non-operative management of childhood neurologic cavovarus foot effective? Orthop Traumatol Surg Res 2016;102:1087-1091. [DOI] [PubMed] [Google Scholar]
- 59.Evans D. Calcaneo-valgus deformity. J Bone Joint Surg [Br] 1975;57-B:270-278. [PubMed] [Google Scholar]
- 60.Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Boint Joint Surg [Am] 1995;77-A:500-512. [DOI] [PubMed] [Google Scholar]
- 61.Sung KH, Chung CY, Lee KM, Lee SY, Park MS. Calcaneal lengthening for planovalgus foot deformity in patients with cerebral palsy. Clin Orthop Relat Res 2013;471:1682-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yoo WJ, Chung CY, Choi IH, Cho TJ, Kim DH. Calcaneal lengthening for the planovalgus foot deformity in children with cerebral palsy. J Pediatr Orthop 2005;25:781-785. [DOI] [PubMed] [Google Scholar]
- 63.Luo CA, Kao HK, Lee WC, Yang WE, Chang CH. Limits of calcaneal lengthening for treating planovalgus foot deformity in children with cerebral palsy. Foot Ankle Int 2017;38:863-869. [DOI] [PubMed] [Google Scholar]
- 64.Bourdet C, Seringe R, Adamsbaum C, Glorion C, Wicart P. Flatfoot in children and adolescents. Analysis of imaging findings and therapeutic implications. Orthop Traumatol Surg Res 2013;99:80-87. [DOI] [PubMed] [Google Scholar]
- 65.Moraleda L, Salcedo M, Bastrom TP, et al. . Comparison of the calcaneo-cuboid-cuneiform osteotomies and the calcaneal lengthening osteotomy in the surgical treatment of symptomatic flexible flatfoot. J Pediatr Orthop 2012;32:821-829. [DOI] [PubMed] [Google Scholar]
- 66.Rathjen KE, Mubarak SJ. Calcaneal-cuboid-cuneiform osteotomy for the correction of valgus foot deformities in children. J Pediatr Orthop 1998;18:775-782. [PubMed] [Google Scholar]
- 67.Kim JR, Park CI, Moon YJ, Wang SI, Kwon KS. Concomitant calcaneo-cuboid-cuneiform osteotomies and the modified Kidner procedure for severe flatfoot associated with symptomatic accessory navicular in children and adolescents. J Orthop Surg Res 2014;9:131. [DOI] [PMC free article] [PubMed] [Google Scholar]