Significance
The United States is increasingly diverse, especially among youth. At the same time, racial and ethnic gaps persist in many domains, including risk for cardiovascular disease. Here, we use a diverse sample of adolescents in a mostly urban setting to show that when schools emphasize the value of diversity, students of color are healthier. Thus, schools’ climates around diversity may have a role to play in reducing health disparities.
Keywords: race, ethnicity, school, health, inequality
Abstract
As the United States becomes more diverse, the ways in which mainstream institutions recognize and address race and ethnicity will be increasingly important. Here, we show that one novel and salient characteristic of an institutional environment, that is, whether a school emphasizes the value of racial and ethnic diversity, predicts better cardiometabolic health among adolescents of color. Using a diverse sample of adolescents who attend more than 100 different schools in predominantly urban locations, we find that when schools emphasize the value of diversity (operationalized as mentioning diversity in their mission statements), students of color, but not white students, have lower values on a composite of five biomarkers of inflammation, have less insulin resistance and compensatory β-cell activity, and have fewer metabolic syndrome signs and score lower on a continuous metabolic syndrome composite. These results suggest that institutions that emphasize diversity may play an unacknowledged role in protecting the health of people of color and, thus, may be a site for future interventions to reduce health disparities.
The United States is increasingly diverse, especially among youth. As a consequence, the ways in which a community’s institutions, including its schools, medical centers, government offices, and courts, recognize and respond to diversity are increasingly important. Here, we show that one facet of how institutions handle diversity is linked to an important life outcome among children of color; namely, their physical health. Specifically, looking at multiple indicators of cardiometabolic risk, we test whether the health of adolescents of color varies with a novel and salient characteristic of their school environment: whether the school emphasizes the value of diversity. This emphasis is communicated in multiple ways that include schools acknowledging the diversity of students; teaching about different cultures, languages, and perspectives; and preparing students for a multicultural world.
The experiences of both youth and adults of color living in the United States differ qualitatively from those of whites. In addition to experiencing more racial discrimination, people of color are also less likely than whites to feel welcome and included in schools and workplaces, and less likely to see members of their group represented in positions of power in society (1, 2). Further, they are more likely than whites to feel that not enough is being done to acknowledge and address these and other issues related to race in this country (3). As a result, from a young age, people of color are especially attuned to, and affected by, experiences, ideas, and messages related to race and ethnicity in their immediate environments (4). In settings in which people of color encounter discrimination, exclusion, and underrepresentation, and, further, in which others fail to understand and acknowledge the role that race plays in shaping people’s experiences and life outcomes, people of color are more alienated, less motivated, less successful, and lower in psychological well-being (5–7).
In contrast, in settings in which people of color are welcomed and their identities and perspectives are explicitly valued, they experience more positive outcomes, such as greater motivation and belonging and improved academic performance (5, 8). One way to create such inclusive environments is to recognize and appreciate race and ethnicity and to signal that diversity and diverse perspectives are valued and included. When institutions send these types of prodiversity messages, people of color are more engaged, trust they will be treated fairly, and persist longer in that setting (9, 10). Merely setting a norm that it is acceptable to talk about race, where relevant, decreases the anxiety and concerns about prejudice that people of color experience in interracial interactions, and increases the opportunities for youth of color to develop positive racial identities (11–13). Moreover, incorporating culturally diverse perspectives into school activities and presenting students with racially diverse examples of successful students improves the sense of belonging and academic performance of students of color (14–17).
In the present work, we consider whether the protective nature of environments that emphasize diversity might also be relevant to another pervasive type of inequality in American society: physical health. Racial disparities in health, which have been documented across a wide range of outcomes, begin to emerge as early as adolescence (18–20). For example, relative to whites, African American and Latino adolescents are more likely to be overweight (21), which predicts greater risk for cardiovascular disease and other chronic diseases of aging later in life (22). Relative to white adolescents, African American adolescents also show more insulin resistance, which increases risk for subsequent diabetes, and more carotid artery intima-media thickness, a marker of preclinical atherosclerosis that portends higher risk for subsequent cardiovascular disease (23, 24). By adulthood, there are notable racial disparities in cardiovascular disease prevalence and mortality, as well as in diabetes prevalence (19).
These racial disparities in health hold even when controlling for socioeconomic status (20, 21, 23, 24), indicating that adolescents of color have unique experiences related to race and ethnicity that have implications for their health (18, 25). Consistent with this idea, a large body of research links perceived racial discrimination to a range of poor health outcomes in youth and adults (26, 27). Moreover, more recent research has extended this literature to show that, even in the absence of explicit unfair treatment, subtler characteristics of the environment that convey messages related to race and ethnicity are also linked to health outcomes. For example, African Americans, but not whites, have worse cardiometabolic health (i.e., higher rates of hypertension, metabolic syndrome, and dyslipidemia) when they live in neighborhoods in which a higher proportion of the residents are incarcerated (28). This is presumably because the threat of arrest is especially salient to African Americans, who tend to be more concerned than whites about unfair treatment from the police (29). In contrast, environments with more positive messages about one’s racial or ethnic group are linked to better health outcomes. For example, Latino students have lower levels of interleukin 6, an inflammatory biomarker that contributes to cardiometabolic disease, when they live in ethnically themed dorms and are, thus, presumably exposed to positive representations of their group (30).
We propose that a willingness to emphasize diversity is a meaningful, yet relatively unexamined, characteristic of the environment that will also relate to health outcomes among people of color. When mainstream contexts, such as schools or workplaces, acknowledge and value diversity, people of color experience a greater sense of trust, comfort, and belonging, all of which are psychological experiences that, in the broader population, have been linked to better health outcomes. For example, trusting that one will be treated fairly is linked to lower blood pressure and inflammatory biomarker levels (30, 31), indicating lower risk of developing multiple health problems associated with aging, including diabetes, heart disease, stroke, and some cancers (32–34). In addition, people who experience a greater sense of belonging and social integration report fewer visits to the doctor and have lower concentrations of inflammatory biomarkers (1, 35).
Drawing on these links among the acknowledgment of diversity, trust, belonging, and health, we tested the hypothesis that adolescents of color would have better health when they attended schools that emphasized diversity. We recruited a large and diverse sample of healthy eighth graders who attended more than 100 different schools, the majority of which were in urban settings and served primarily nonwhite students. We conceptualized an emphasis on diversity as a feature of the school’s culture that encompassed a number of interrelated ideas and values that have been shown to benefit students of color, including acknowledging race, valuing diversity, and including diverse perspectives in the classroom. To capture this feature of schools’ cultures, we obtained each school’s mission statement. Such statements have been shown to reflect an organization’s policies and the attitudes, values, and behaviors of its people within the organization (36–38). We then coded the mission statements for their emphasis on the value of diversity (e.g., serving “a diverse student body,” “promoting life-long learning and respect for diversity”). Given the racial and ethnic disparities in cardiovascular disease and the burdens they pose for communities of color, our health assessment focused on multiple indicators of cardiometabolic risk: inflammatory biomarkers, insulin resistance and β-cell function, and metabolic syndrome. These indices have been prospectively shown to forecast risk for diabetes, heart disease, and stroke in adulthood (32, 33, 39, 40).
Among students of color, we expected that attending a school that emphasized diversity would be associated with lower cardiometabolic risk. Given that students of color are more likely than whites to experience a lack of belonging in school and to be attuned to diversity-related cues (1, 6), we further hypothesized that this pattern would not emerge among white students. We hypothesized that among white students, who often see attention to diversity as less self-relevant or important, or even as threatening (41), attending schools that emphasized diversity would either be unrelated to cardiometabolic risk or related to higher risk. Finally, building on research that people of color feel a sense of belonging in environments in which diversity is acknowledged, and that race-relevant messages in the environment other than explicit discrimination matter for the health of people of color (6, 8, 28, 30), we predicted that these relationships would emerge above and beyond students’ perceptions of discrimination.
Results
Participants.
Participants were healthy eighth graders who were part of a larger study on cardiovascular disease risk. Of the 277 participants in the full sample, the relevant school data were available for 270 participants (Mage = 13.91; SDage = 0.54; 36.67% boys; 3.33% Asian, 24.07% Hispanic, 29.63% African American, 27.41% white, and 15.56% more than one race/ethnicity). See Table 1 for details. Participants in the analytic sample attended 120 different schools in the greater Chicago, Illinois, area (84.17% public; mean percentage of student body that is white, 29.26%).
Table 1.
Sample descriptive statistics
| Variables | White students | Students of color | |||
| N | M (SD) or % | N | M (SD) or % | P | |
| Age | 74 | 13.79 (0.53) | 196 | 13.96 (0.54) | 0.025 |
| Sex, % male | 74 | 37.84 | 196 | 36.22 | 0.806 |
| Savings, 9-point scale | 73 | 6.00 (2.20) | 189 | 2.99 (2.16) | <0.001 |
| Pubertal stage | 74 | 3.58 (0.70) | 195 | 3.78 (0.77) | 0.048 |
| Inflammation composite | 73 | −0.10 (2.27) | 195 | 0.03 (3.25) | 0.759 |
| HOMA-IR | 73 | 2.60 (1.67) | 195 | 3.30 (2.59) | 0.032 |
| Β-cell function | 72 | 138.62 (43.91) | 192 | 161.96 (60.32) | 0.003 |
| Metabolic syndrome, Count | 74 | 0.42 (0.70) | 196 | 0.54 (0.83) | 0.285 |
| Metabolic syndrome, Continuous | 74 | −0.23 (2.34) | 196 | 0.05 (2.93) | 0.453 |
| Discrimination | 74 | 16.53 (4.87) | 195 | 18.22 (5.36) | 0.018 |
School Diversity Climate.
To assess whether schools emphasized the value of diversity, we coded the content of their mission statements, which reflect organizations’ policies and the attitudes, values, and behaviors of organizations’ members (36–38). Although the process of creating mission statements varies by district, they are often written by committees of administrators, teachers, parents, and other stakeholders. In the Chicago Public School system, mission statements are written as part of the process of opening a new school, and schools complete regular reports in which they set goals for the coming years based on the priorities that are articulated in their mission statements.
We obtained schools’ mission statements by asking participants to report what school they attended and then searching each school’s website for its mission statement. Mission statements were nearly always printed on the website’s main homepage or accessible from a drop-down menu. Mission statements for each school within the Chicago Public School district were also available on the district site. In the few cases in which the mission statement was not clearly displayed on the school or district website, we located it by searching the school website for the term “mission statement.” Mission statements were available for 120 of the 124 schools attended by our participants.
Schools’ mission statements were typically two to three sentences long (Mwords = 81.42; SDwords = 59.56). They mentioned a range of ideas, including fostering curiosity and a desire to learn, providing a high-quality education, encouraging collaboration among students, supporting students’ social-emotional well-being, using technology in the classroom, and teaching students to contribute to the community or world. The focus of our analyses was whether the mission statements indicated that the school emphasized diversity. We coded mission statements as emphasizing diversity if they mentioned preparing students to live in a multicultural or global world (e.g., “thrive in a global society”); respecting or valuing diversity (e.g., “embraces cultural diversity”); serving a diverse student body (“our diverse community”); offering bilingual instruction (e.g., “students develop fluency...in both Spanish and English”); including racially or culturally diverse perspectives in the curriculum (e.g., teaching “literary works from diverse social, cultural, and historical contexts”); teaching an awareness of or responsiveness to other racial, ethnic, or cultural groups (e.g., “promoting an understanding of other racial and cultural groups”); and meeting students’ cultural needs (e.g., “meet[ing] the...cultural needs of all students”). Schools were coded as either not mentioning any of these points (not emphasizing diversity) or mentioning at least one of these points (emphasizing diversity), a dichotomous variable.
We conceptualized these mission statements as encapsulations of the schools’ cultures, including their values, policies, and practices. To determine whether our coding scheme captured meaningful, observable differences in the school environment for students of color, as opposed to just rhetoric, we conducted a separate validation study. This study used a separate sample of all K–8 public schools in Chicago that were not attended by our participants (i.e., all other K–8 schools in the city; n = 315). We located these schools’ mission statements, coded them as described above, and integrated those results with publicly available data on the schools’ academic outcomes and disciplinary rates, available from the US Department of Education (https://ocrdata.ed.gov). We tested whether students of color were more academically successful and disciplined less often in schools that our mission statement coding scheme classified as emphasizing diversity. Consistent with the validity of the coding scheme, we found that in schools that emphasized (vs. did not emphasize) diversity, students of color progressed onto the next grade (i.e., because of passing courses) at higher rates and were less likely to receive out-of-school suspensions (Ps < 0.013). They were also marginally less likely to receive in-school suspensions (P = 0.109). No such differences emerged among white students (Ps > 0.370). See SI Appendix for more details.
Having established that our coding scheme captured meaningful differences in the school environment for students of color, we returned to analyses of the schools attended by participants in our study and considered whether the emphasis on diversity was associated with other school-level characteristics that could provide alternative explanations for any linkage to health. These comparisons, which are reported in detail in the SI Appendix, Table S1, revealed no differences between schools that did and did not emphasize diversity in their likelihood of being public, their mean student–teacher ratios, the demographics (i.e., race/ethnicity, socioeconomic status, English language learner status) of their student bodies, or the overall standardized test performance of eighth grade students, although schools that emphasized diversity did have longer mission statements.
Cardiometabolic Risk.
Three dimensions of cardiometabolic risk were assessed: low-grade inflammation, insulin resistance and β-cell function, and metabolic syndrome. To assess low-grade inflammation, antecubital blood was collected from participants after an overnight fast. Five inflammatory biomarkers were quantified: interleukins 6, 8, and 10; tumor necrosis factor alpha; and C-reactive protein. In long-term prospective studies, higher levels of these biomarkers forecast greater odds of diabetes, myocardial infarction, coronary heart disease, stroke, and some cancers (32–34). Values were log-10 transformed to correct for skew, standardized into z-scores, and summed to create a composite.
From the same fasting blood samples, we also measured serum levels of glucose and insulin to estimate insulin resistance and β-cell function. Increased levels of both these markers reflect dysregulation in the body’s ability to use insulin to keep glucose levels within a narrow physiologic range and indicate greater risk for diabetes (42, 43). We estimated insulin resistance using the homeostasis model assessment (HOMA-IR) (42, 43), with the equation ([fasting glucose (mmol/L) × fasting insulin (mIU/L)]/22.5) and pancreatic β-cell function with the Oxford Centre for Diabetes, Endocrinology, and Metabolism software (https://www.dtu.ox.ac.uk/homacalculator).
Finally, we measured metabolic syndrome, a cluster of signs linked to the development of cardiovascular disease and type 2 diabetes (40, 44). According to the International Diabetes Federation’s guidelines, 11–16-y-olds are diagnosed with metabolic syndrome if they have central adiposity (waist circumference ≥90th percentile for their age, sex, and race/ethnicity, or the adult cutoff if lower) and at least two of the following: high-density lipoprotein cholesterol <40 mg/dL, triglycerides ≥150 mg/dL, fasting glucose ≥100 mg/dL, and systolic blood pressure ≥130 mm Hg and/or diastolic blood pressure ≥85 mm Hg (44). In our relatively young and healthy sample, only eight participants met the criteria for diagnosis. Therefore, we also calculated two continuous indices, which were the outcomes of interest in our analyses. The first was a sum of the number of components on which participants met the clinical cutoffs, which ranged from 0 to 5. Second, in acknowledgment of concerns about the validity of dichotomizing children into risk categories when variables are continuous (45), we also created a composite that was the sum of the z-scores of each component.
Analyses.
Students of color were slightly older, had families with fewer savings, were at a higher pubertal stage, and had higher insulin resistance levels than whites. See Table 1 for details.
To account for the nested structure of our dataset (i.e., students within schools), we tested the study hypotheses using generalized estimating equations. School was treated as a nesting variable, and an exchangeable covariate structure was specified. The primary independent variables, students’ race (0 = students of color, including all multiracial participants; 1 = white students) and whether schools emphasized diversity (0 = yes; 1 = no), were both dummy coded. Covariates in all models were sex, age, family’s savings, pubertal stage, mission statement word count, whether the school was public, the school’s student–teacher ratio, and the student body racial demographics (% white and % African American). Continuous covariates were standardized.
Inflammation.
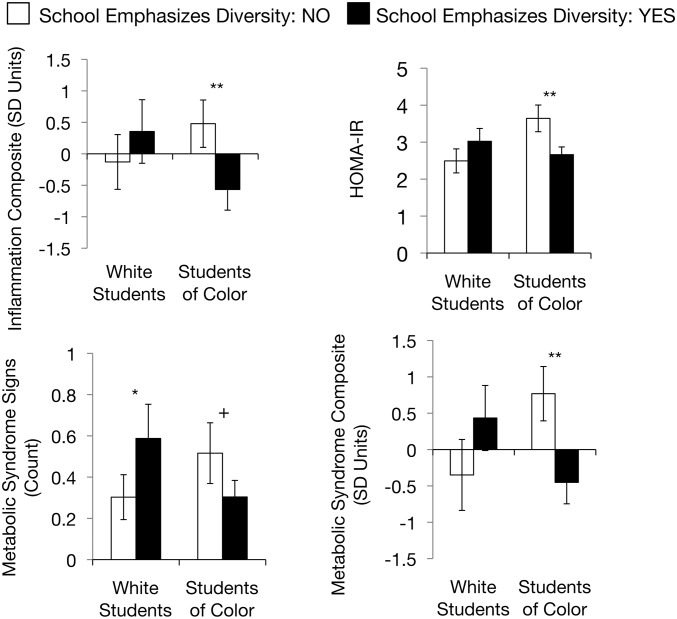
We first tested the effect of child race, whether the school emphasized diversity, and their interaction on the inflammation composite. Neither main effect was significant (Ps > 0.16), but the expected interaction emerged (b = −1.53; 95% confidence interval [CI], −2.80 to −0.27; P = 0.018). The school’s emphasis on diversity was not related to inflammation among white students (b = 0.48; 95% CI, −0.60 to 1.57; P = 0.381; d = 0.24; diversity not emphasized: M = −0.13, SD = 2.75; diversity emphasized: M = 0.35, SD = 2.90). However, students of color had lower inflammation levels when they attended schools that emphasized diversity (M = −0.57, SD = 3.28) compared with schools that did not (M = 0.48; SD = 3.67; b = −1.05; 95% CI, −1.81 to −0.28; P = 0.007; d = 0.43). See Fig. 1.
Fig. 1.
Estimated marginal means of inflammation composite, insulin resistance, and metabolic syndrome outcomes among white students and students of color as a function of whether the school emphasizes diversity. Error bars represent ± 1 SE. **P ≤ 0.01; *P ≤ 0.05; +P ≤ 0.10.
Insulin Resistance and β-Cell Function.
We repeated the analyses with insulin resistance (HOMA-IR) as the outcome. There was a main effect of child race (b = 0.38; 95% CI, 0.10 to 0.66; P = 0.009), but not of whether the school emphasized diversity (b = 0.19; 95% CI, −0.14 to 0.52; P = 0.251). The expected interaction also emerged (b = −0.51; 95% CI, −0.89 to −0.12; P = 0.010). Whether the school emphasized diversity was not related to insulin resistance among white students (b = 0.19; 95% CI, −0.14 to 0.52; P = 0.251; d = 0.37; diversity not emphasized: M = 2.49, SD = 2.06; diversity emphasized: M = 3.02, SD = 1.99). However, students of color had lower insulin resistance when they attended schools that emphasized diversity (M = 2.66; SD = 2.09) compared with schools that did not (M = 3.64; SD = 3.52; b = −0.31; 95% CI, −0.50 to −0.13; P = 0.001; d = 0.48; Fig. 1).
Next, we repeated the analyses with β-cell function as the outcome. There was a main effect of child race (b = 26.12; 95% CI, 6.75 to 45.50; P = 0.008), but not of whether the school emphasized diversity (b = 13.24; 95% CI, −10.77 to 37.25; P = 0.280). Again, the expected interaction emerged (b = −25.13; 95% CI, −50.62 to 0.35; P = 0.053). Although whether the school emphasized diversity did not significantly predict β-cell function among students in either racial group (Ps > 0.15), the pattern of the means among students of color was in the expected direction (diversity not emphasized: M = 168.42, SD = 91.11; diversity emphasized: M = 156.52, SD = 78.57).
Metabolic Syndrome.
Next, we repeated the analyses with the number of clinically elevated metabolic syndrome signs as the outcome. There was a significant main effect of child race (b = 0.53; 95% CI, 0.01 to 1.06; P = 0.047) and a main effect of whether the school emphasized diversity (b = 0.66, 95% CI, 0.09 to 1.41; P = 0.045). The expected interaction also emerged (b = −1.19, 95% CI, −1.97 to −0.41; P = 0.003). White students had more metabolic syndrome signs when they attended schools that emphasized diversity (M = 0.59; SD = 0.95) compared with schools that did not (M = 0.30; SD = 0.70; b = 0.66, 95% CI, 0.09 to 1.41; P = 0.045; d = 0.48). In contrast, students of color had marginally fewer metabolic syndrome signs when they attended schools that emphasized diversity (M = 0.30; SD = 0.80) compared with schools that did not (M = 0.52; SD = 1.44; b = −0.53, 95% CI, −1.03 to 0.03; P = 0.079; d = 0.26; Fig. 1).
Finally, we tested the effect of child race, whether the school valued diversity, and their interaction on the continuous metabolic syndrome composite. There was a main effect of child race (b = 1.12; 95% CI, 0.14 to 2.09; P = 0.025), but not of whether the school emphasized diversity (b = 0.78; 95% CI, −0.37 to 1.93; P = 0.182). In addition, the expected interaction emerged (b = −2.00; 95% CI, −3.26 to −0.75; P = 0.002). Whether the school emphasized diversity was not related to the continuous metabolic syndrome composite among white students (b = 0.78; 95% CI, −0.37 to 1.93; P = 0.182; d = 0.39; diversity not emphasized: M = −0.35, SD = 3.12; diversity emphasized: M = 0.43, SD = 2.57), but students of color had lower scores on this composite when they attended schools that emphasized diversity (M = −0.45; SD = 2.95) compared with schools that did not (M = 0.77; SD = 3.66; b = −1.22, 95% CI, −1.99 to −0.46; P = 0.002; d = 0.52; Fig. 1).
Additional Analyses: Discrimination.
As noted earlier, we built on research showing that people of color feel a sense of belonging in environments in which diversity is acknowledged, and that race-relevant messages in the environment other than explicit discrimination matter for the health of people of color (6, 8, 28, 30), to predict that our observed relationships would emerge above and beyond perceived discrimination. To test this, we repeated the analyses controlling for participants’ self-reported experiences of discrimination, using Williams and colleagues’ scale, which asks participants to respond to 10 items that assess frequency of discriminatory treatment (e.g., treated with less respect or seen as less smart than others) (25). Although this scale is not specific to discrimination in schools, it is commonly used to assess how discriminatory experiences relate to health. Thus, the persistence of our observed effects controlling for this scale would indicate that an institutional environment that emphasizes diversity is related to health above and beyond discrimination, as often measured. All the interactions and contrasts that had been significant remained so (Ps ≤ 0.040), and the one interaction that had been marginal (i.e., for β-cell function) remained marginal as well (P = 0.051). See SI Appendix for details.
Discussion
Using a diverse sample of adolescents, we show that students of color have better cardiometabolic health when their school emphasizes diversity. This pattern is apparent across multiple dimensions of cardiometabolic health, including biomarkers of inflammation, insulin resistance and β-cell activity, and two definitions of metabolic syndrome. Furthermore, these associations exist controlling for a range of other factors, including participants’ socioeconomic status and school characteristics, such as the student body demographics and the student–teacher ratios.
A growing body of work recognizes that, even after accounting for socioeconomic resources and opportunities, people of color have unique experiences related to race and ethnicity that are associated with worse health (18, 25). However, a great deal of the empirical work in this area has focused on concrete examples of racially biased treatment, often reported by participants. Our work helps to broaden the scope of this literature in two ways. First, our effects emerge controlling for students’ self-reported experiences of discrimination. This suggests that fully understanding the relationship between the social environment and health among people of color requires attending to more than just explicit discrimination. Institutions, norms, policies, and practices that convey subtle, yet powerful, messages about diversity may play an additional role. Second, we extend the race-health literature by shifting the focus from the negative race-related experiences that have been prominent in past work to more positive race-related experiences. An implicit assumption of past research is that if enough negative experiences (e.g., discrimination) were eliminated, people of color would be as healthy as whites. However, the schools in our sample whose mission statements did not mention diversity were not directly communicating anything negative about race and ethnicity to their students. Instead, we find that the presence of an additional positive factor relevant to race, emphasizing diversity, predicts better health.
This is not to say that previous health research has left the role of supportive schools unexamined. The link between school belonging and health is well documented (46). However, very little of this research has explicitly recognized that schools are often set up in ways that make it harder for students of color than for white students to feel that they belong there (see ref. 2 for an exception). Furthermore, many of these studies ask students to report on their feelings of belonging and connection at school. Instead, we built on past research showing that people of color feel a greater sense of belonging in organizations that acknowledge and value diversity (8, 10) to code an objective feature of the school context (i.e., mission statements) that relates to better health. This approach is consistent with other work showing that academic outcomes such as engagement, persistence, self-efficacy, and performance are improved among people from underrepresented groups when objective features of the environment are altered to improve their sense of belonging (47–50).
Mechanisms Among Students of Color.
To understand these findings, it is useful to consider what is happening in schools at multiple levels, ranging from institutional policies and practices to individual students’ psychological, behavioral, and physiological processes. In schools that do not emphasize diversity, students of color may encounter negative or threatening psychosocial experiences, including low expectations from teachers, underrepresentation in the curriculum, and as our coding scheme validation analyses show, more frequent, harsh discipline (5, 8, 51). Daily exposure to this type of context could prompt a sense of exclusion, mistrust, or anxiety and vigilance, which are all psychological states that previous research has linked to unhealthier behaviors, autonomic and/or adrenocortical dysregulation, and higher inflammatory biomarker levels (52–54).
In contrast, students of color attending schools that emphasize diversity likely face a more welcoming environment. They may recognize that others see their racial group positively, which is associated with lower levels of inflammation (55). In addition, schools that emphasize diversity may have more teachers of color, include the perspectives of people of color in the curriculum to a greater degree, or have fewer racial disparities in academic success or disciplinary rates. This, in turn, could mean that students of color feel better understood, valued, and supported, which is associated with better health (56). Finally, when questions related to race and ethnicity arise, teachers might be more likely to acknowledge and discuss them, which can reduce stress levels among people of color (11), with downstream consequences for cardiometabolic health (57). These and other mechanisms could be tested in follow-up research.
White Students’ Experiences.
White students’ cardiometabolic outcomes showed a different pattern than those of students of color. Among white students, analyses with most outcome variables revealed no significant differences as a function of their school context. This effect could be explained by whites’ tendency to see diversity as less self-relevant (41), which could result in their being less attuned to or affected by this aspect of their school environment. At the same time, the pattern of results was such that whites’ cardiometabolic outcomes were in the direction of being less healthy (significantly so for the count of clinically elevated metabolic syndrome signs) when they attended schools that emphasized diversity. This pattern is consistent with research showing that white men exhibit a cardiovascular threat response (i.e., lower cardiac activation, increased peripheral resistance) when applying to work at a company that values diversity (58) and raises the possibility that prodiversity climates harm whites’ health. Given our interest in the health of adolescents of color, our sample of whites was relatively small. However, if future research with larger samples of white students also supports this conclusion, follow-up work could explore how schools could handle diversity in ways that simultaneously promote health among both white students and students of color. This might involve ensuring that white students feel included in conversations about diversity and feel a sense of belonging in school (41).
Experiments and Interventions.
A notable limitation of the current work is its correlational design. We have suggested that schools that emphasize diversity foster better health among students of color. However, an alternative explanation is that when students of color are healthier, they are more successful in school, leading school staff to see diversity as beneficial. It is also possible that parents who value diversity send their children to schools in which diversity is celebrated and simultaneously adopt healthier routines at home. Longitudinal research could rule out some of these possibilities by exploring how students’ health changes over time; for example (e.g., as they move from a junior high school that does not emphasize diversity to a high school that does).
In addition, experiments could test the causal relationships between schools’ emphasis on diversity and students’ health. In the laboratory, researchers might ask students to think about ways in which their schools do or do not emphasize diversity and then measure students’ cortisol levels or blood pressure. Outside of the laboratory, interventions that manipulate the extent to which schools emphasize diversity might also reduce cardiometabolic risk among students of color. Importantly, we suggest that effective interventions will manipulate not only messages in mission statements and other materials but also on-the-ground policies and practices related to diversity. We showed that mission statement content reflected concrete differences in the experiences of students of color in these schools (i.e., in academic success and discipline). Rhetorical changes alone are unlikely to have positive effects on health, and might even backfire.
Approaches to Emphasizing Diversity.
Future research could also explore what particular approaches to emphasizing diversity are associated with the healthiest outcomes for students of color. Our sample was too small to explore variation within the group of schools that emphasized diversity. However, within this group, some schools might have merely acknowledged that their student bodies were diverse, whereas others had a deeper commitment to diversity and actively worked to include diverse perspectives and dismantle inequality in the classroom. We would predict that students of color would have the best health in the latter environment.
Public Health and Policy Implications.
Our results emerged consistently across multiple biomarkers that have been prospectively linked to cardiovascular disease (32, 33, 39, 40), which is a major cause of disability and death in the United States, with stark racial disparities in prevalence and mortality rates (19, 59). For instance, African Americans are ∼50% more likely than whites to die early (i.e., before age 75 years) from cardiovascular disease (19). Cardiovascular disease thus disproportionately takes African Americans away from their families, communities, and workplaces, thereby maintaining and worsening existing social and economic inequalities. Efforts to address these health disparities often focus on traditional risk factors, such as access to healthy food or quality healthcare (19). Our work suggests that it is also important to consider ideas about diversity embedded in social structures and institutions, including schools, as we show here, but also workplaces, government offices, and other institutions (see also ref. 18). Helping people of color to feel fully valued and included by addressing issues related to diversity and instituting policies and practices that acknowledge and even celebrate diversity thus has the potential to improve the health of people of color and reduce health disparities.
Methods
Participants visited the laboratory, reported the name of their school and demographic characteristics, and underwent a blood draw. Youths and their parents gave written informed assent and consent, respectively. Northwestern University’s institutional review board approved the protocol. See SI Appendix for details.
Supplementary Material
Acknowledgments
We thank Thalia Perez for her help with coding. This research was funded by grants from the National Institutes of Health, National Heart Lung and Blood Institute (HL122328 and F32HL119021), and a Russell Sage Foundation Grant 96-18-01.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1812068116/-/DCSupplemental.
References
- 1.Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science. 2011;331:1447–1451. doi: 10.1126/science.1198364. [DOI] [PubMed] [Google Scholar]
- 2.Park H, Keller J, Williams J. 2016 The face of American power, nearly as White as the Oscar nominations. New York Times. Available at https://www.nytimes.com/interactive/2016/02/26/us/race-of-american-power.html. Accessed February 20, 2019.
- 3.Pew Research Center 2016 On views of race and inequality, blacks and whites are worlds apart. Available at assets.pewresearch.org/wp-content/uploads/sites/3/2016/06/ST_2016.06.27_Race-Inequality-Final.pdf. Accessed February 20, 2019.
- 4.Brown CS, Alabi BO, Huynh VW, Masten CL. Ethnicity and gender in late childhood and early adolescence: Group identity and awareness of bias. Dev Psychol. 2011;47:463–471. doi: 10.1037/a0021819. [DOI] [PubMed] [Google Scholar]
- 5.Steele C. Whistling Vivaldi and Other Clues to How Stereotypes Affect Us and What We Can Do. Norton; New York: 2011. [Google Scholar]
- 6.Plaut VC. Diversity science: Why and how difference makes a difference. Psychol Inq. 2010;21:77–99. [Google Scholar]
- 7.Holoien DS, Bergsieker HB, Shelton JN, Alegre JM. Do you really understand? Achieving accuracy in interracial relationships. J Pers Soc Psychol. 2015;108:76–92. doi: 10.1037/pspi0000003. [DOI] [PubMed] [Google Scholar]
- 8.Steele DM, Cohn-Vargas B. Identity Safe Classrooms: Places to Belong and Learn. Corwin, a Sage Company; Thousand Oaks, CA: 2013. [Google Scholar]
- 9.McKay PF, et al. Racial differences in employee retention: Are diversity climate perceptions the key? Person Psychol. 2007;60:35–62. [Google Scholar]
- 10.Plaut VC, Thomas KM, Goren MJ. Is multiculturalism or color blindness better for minorities? Psychol Sci. 2009;20:444–446. doi: 10.1111/j.1467-9280.2009.02318.x. [DOI] [PubMed] [Google Scholar]
- 11.Trawalter S, Richeson JA. Let’s talk about race, baby! When whites’ and blacks’ interracial contact experiences diverge. J Exp Soc Psychol. 2008;44:1214–1217. doi: 10.1016/j.jesp.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Apfelbaum EP, Sommers SR, Norton MI. Seeing race and seeming racist? Evaluating strategic colorblindness in social interaction. J Pers Soc Psychol. 2008;95:918–932. doi: 10.1037/a0011990. [DOI] [PubMed] [Google Scholar]
- 13.Pauker K, Apfelbaum EP, Spitzer B. When societal norms and social identity collide: The race talk dilemma for racial minority children. Soc Psychol Personal Sci. 2015;6:887–895. doi: 10.1177/1948550615598379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dee TS, Penner EK. The causal effects of cultural relevance: Evidence from an ethnic studies curriculum. Am Educ Res J. 2017;54:127–166. [Google Scholar]
- 15.Brannon TN, Markus HR, Taylor VJ. “Two souls, two thoughts,” two self-schemas: Double consciousness can have positive academic consequences for African Americans. J Pers Soc Psychol. 2015;108:586–609. doi: 10.1037/a0038992. [DOI] [PubMed] [Google Scholar]
- 16.Covarrubias R, Fryberg SA. The impact of self-relevant representations on school belonging for native American students. Cultur Divers Ethnic Minor Psychol. 2015;21:10–18. doi: 10.1037/a0037819. [DOI] [PubMed] [Google Scholar]
- 17.Salter PS, Adams G, Perez MJ. Racism in the structure of everyday worlds: A cultural-psychological perspective. Curr Dir Psychol Sci. 2018;27:150–155. [Google Scholar]
- 18.Priest N, Williams DR. In: Racial Discrimination and Racial Disparities in Health the Oxford Handbook of Stigma, Discrimination, and Health. Major B, Dovidio JF, Link BG, editors. Oxford Univ Press; New York: 2018. [Google Scholar]
- 19.Centers for Disease Control and Prevention 2013 CDC health disparities and inequalities report–United States, 2013. Available at https://www.cdc.gov/mmwr/pdf/other/su6203.pdf. Accessed February 20, 2019.
- 20.Flores G. Committee On Pediatric Research Technical report–Racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125:e979–e1020. doi: 10.1542/peds.2010-0188. [DOI] [PubMed] [Google Scholar]
- 21.Lee NE, De AK, Simon PA. School-based physical fitness testing identifies large disparities in childhood overweight in Los Angeles. J Am Diet Assoc. 2006;106:118–121. doi: 10.1016/j.jada.2005.09.053. [DOI] [PubMed] [Google Scholar]
- 22.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23:S2–S11. doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 23.Goodman E, Daniels SR, Dolan LM. Socioeconomic disparities in insulin resistance: Results from the Princeton school district study. Psychosom Med. 2007;69:61–67. doi: 10.1097/01.psy.0000249732.96753.8f. [DOI] [PubMed] [Google Scholar]
- 24.Lefferts WK, et al. Racial differences in aortic stiffness in children. J Pediatr. 2017;180:62–67. doi: 10.1016/j.jpeds.2016.09.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams DR, Yan Yu, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 26.Lewis TT, Williams DR, Tamene M, Clark CR. Self-reported experiences of discrimination and cardiovascular disease. Curr Cardiovasc Risk Rep. 2014;8:365. doi: 10.1007/s12170-013-0365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huynh VW, Fuligni AJ. Discrimination hurts: The academic, psychological, and physical well-being of adolescents: Discrimination hurts. J Res Adolesc. 2010;20:916–941. [Google Scholar]
- 28.Topel ML, et al. High neighborhood incarceration rate is associated with cardiometabolic disease in nonincarcerated black individuals. Ann Epidemiol. 2018;28:489–492. doi: 10.1016/j.annepidem.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tyler TR. Policing in black and white: Ethnic group differences in trust and confidence in the police. Police Q. 2005;8:322–342. [Google Scholar]
- 30.Rheinschmidt-Same M, John-Henderson NA, Mendoza-Denton R. Ethnically-based theme house residency and expected discrimination predict downstream markers of inflammation among college students. Soc Psychol Personal Sci. 2017;8:102–111. [Google Scholar]
- 31.Blascovich J, Spencer SJ, Quinn D, Steele C. African Americans and high blood pressure: The role of stereotype threat. Psychol Sci. 2001;12:225–229. doi: 10.1111/1467-9280.00340. [DOI] [PubMed] [Google Scholar]
- 32.Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 33.Kaptoge S, et al. The Emerging Risk Factors Collaboration C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: An individual participant meta-analysis. Lancet. 2010;375:132–140. doi: 10.1016/S0140-6736(09)61717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crusz SM, Balkwill FR. Inflammation and cancer: Advances and new agents. Nat Rev Clin Oncol. 2015;12:584–596. doi: 10.1038/nrclinonc.2015.105. [DOI] [PubMed] [Google Scholar]
- 35.Ford ES, Loucks EB, Berkman LF. Social integration and concentrations of C-reactive protein among US adults. Ann Epidemiol. 2006;16:78–84. doi: 10.1016/j.annepidem.2005.08.005. [DOI] [PubMed] [Google Scholar]
- 36.Davis JH, Ruhe JA, Lee M, Rajadhyaksha U. Mission possible: Do school mission statements work? J Bus Ethics. 2006;70:99–110. [Google Scholar]
- 37.Morley CP, et al. The social mission in medical school mission statements: Associations with graduate outcomes. Fam Med. 2015;47:427–434. [PubMed] [Google Scholar]
- 38.Blair-Loy M, Wharton AS, Goodstein J. Exploring the relationship between mission statements and work-life practices in organizations. Organ Stud. 2011;32:427–450. [Google Scholar]
- 39.Berenson GS, Srnivasan SR. Bogalusa Heart Study Group Cardiovascular risk factors in youth with implications for aging: The Bogalusa heart study. Neurobiol Aging. 2005;26:303–307. doi: 10.1016/j.neurobiolaging.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 40.Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: The Princeton lipid research clinics follow-up study. Pediatrics. 2007;120:340–345. doi: 10.1542/peds.2006-1699. [DOI] [PubMed] [Google Scholar]
- 41.Plaut VC, Garnett FG, Buffardi LE, Sanchez-Burks J. “What about me?” Perceptions of exclusion and whites’ reactions to multiculturalism. J Pers Soc Psychol. 2011;101:337–353. doi: 10.1037/a0022832. [DOI] [PubMed] [Google Scholar]
- 42.Matthews DR, et al. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 43.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 44.International Diabetes Federation 2007 The IDF consensus definition of the metabolic syndrome in children and adolescents. Available at https://www.idf.org/e-library/consensus-statements/. Accessed February 20, 2019.
- 45.Goodman E. Metabolic syndrome and the mismeasure of risk. J Adolesc Health. 2008;42:538–540. doi: 10.1016/j.jadohealth.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 46.Resnick MD, et al. Protecting adolescents from harm. Findings from the national longitudinal study on adolescent health. JAMA. 1997;278:823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 47.Browman AS, Destin M. The effects of a warm or chilly climate toward socioeconomic diversity on academic motivation and self-concept. Pers Soc Psychol Bull. 2016;42:172–187. doi: 10.1177/0146167215619379. [DOI] [PubMed] [Google Scholar]
- 48.Cheryan S, Plaut VC, Davies PG, Steele CM. Ambient belonging: How stereotypical cues impact gender participation in computer science. J Pers Soc Psychol. 2009;97:1045–1060. doi: 10.1037/a0016239. [DOI] [PubMed] [Google Scholar]
- 49.Murphy MC, Steele CM, Gross JJ. Signaling threat: How situational cues affect women in math, science, and engineering settings. Psychol Sci. 2007;18:879–885. doi: 10.1111/j.1467-9280.2007.01995.x. [DOI] [PubMed] [Google Scholar]
- 50.Stephens NM, Fryberg SA, Markus HR, Johnson CS, Covarrubias R. Unseen disadvantage: How American universities’ focus on independence undermines the academic performance of first-generation college students. J Pers Soc Psychol. 2012;102:1178–1197. doi: 10.1037/a0027143. [DOI] [PubMed] [Google Scholar]
- 51.Okonofua JA, Eberhardt JL. Two strikes: Race and the disciplining of young students. Psychol Sci. 2015;26:617–624. doi: 10.1177/0956797615570365. [DOI] [PubMed] [Google Scholar]
- 52.Ranjit N, et al. Psychosocial factors and inflammation in the multi-ethnic study of atherosclerosis. Arch Intern Med. 2007;167:174–181. doi: 10.1001/archinte.167.2.174. [DOI] [PubMed] [Google Scholar]
- 53.Cartwright M, et al. Stress and dietary practices in adolescents. Health Psychol. 2003;22:362–369. doi: 10.1037/0278-6133.22.4.362. [DOI] [PubMed] [Google Scholar]
- 54.Townsend SSM, Major B, Gangi CE, Mendes WB. From “in the air” to “under the skin”: Cortisol responses to social identity threat. Pers Soc Psychol Bull. 2011;37:151–164. doi: 10.1177/0146167210392384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ratner KG, Halim ML, Amodio DM. Perceived stigmatization, ingroup pride, and immune and endocrine activity: Evidence from a community sample of black and Latina women. Soc Psychol Personal Sci. 2013;4:82–91. [Google Scholar]
- 56.Pietromonaco PR, Collins NL. Interpersonal mechanisms linking close relationships to health. Am Psychol. 2017;72:531–542. doi: 10.1037/amp0000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cohen S, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci USA. 2012;109:5995–5999. doi: 10.1073/pnas.1118355109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dover TL, Major B, Kaiser CR. Members of high-status groups are threatened by pro-diversity organizational messages. J Exp Soc Psychol. 2016;62:58–67. [Google Scholar]
- 59.Murray CJL, et al. U.S. Burden of Disease Collaborators The state of US health, 1990-2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.