Abstract
Objective:
Low-income urban children of color are at elevated risk for poor asthma control. This cross-sectional study examined associations among parents’ coping (primary control, secondary control, and disengagement), parental depressive symptoms, and children’s asthma outcomes (asthma control and school attendance) in a predominantly low-income, racially/ethnically diverse sample of families.
Methods:
Parents (N = 78; 90% female) of children (33% female; 46% Black; 38% Latino) ages 5 to 17 years old (M = 9.5 years) reported on their own coping and depressive symptoms, their child’s asthma control, and full and partial days of school missed due to asthma.
Results:
Parents’ secondary control coping (i.e., coping efforts to accommodate/adapt to asthma-related stressors) was negatively correlated, and disengagement coping (i.e. coping efforts to avoid/detach from stressors) was positively correlated, with their depressive symptoms. Secondary control coping was also correlated with fewer partial days of school missed. Primary control coping (i.e., coping efforts to change stressors) was not associated with depressive symptoms or asthma outcomes. Parents’ depressive symptoms were also positively correlated with poorer asthma control and partial days of school missed. Regression models showed direct and indirect effects of secondary control and disengagement coping on asthma outcomes via depressive symptoms, after controlling for demographic factors.
Conclusions:
Parents’ secondary control and disengagement coping are related to children’s asthma outcomes. Secondary control coping may support parents’ mental health and children’s asthma control in low-income urban families.
Keywords: asthma, coping, depression, parent, child, low-income
Introduction
Pediatric asthma results in significant school absenteeism for children and missed work and loss of income for parents [1,2]. Parents of children with asthma, especially those from lower socioeconomic backgrounds, are at increased risk for depressive symptoms [3–5], and parental depressive symptoms are associated with worse asthma morbidity [6]. Children’s asthma morbidity is also linked to parental stressors [6], suggesting the importance of effective parental coping strategies to support children’s asthma outcomes [7]. However, little research has examined the relations among parental coping, parental depressive symptoms, and child asthma outcomes, particularly in low-income, urban children of color who are at the greatest risk of disparities in asthma control and healthcare [8,9].
Parental Depressive Symptoms and Children’s Asthma
Parental depressive symptoms have been linked to more severe asthma [10] and poorer disease control, including increased asthma-related inflammatory markers in children [6,11]. Parents with more depressive symptoms report that their children have fewer symptom free days and nights [4], and children of parents with mental health diagnoses, including depression, are almost twice as likely to require hospitalization for their asthma [12] and miss more days of school [13]. The increased risk for poorer asthma outcomes may be due to greater difficulty with disease management for parents with depression [14], as well as psychobiologic disease pathways in which parental depression leads to increased child stress and asthma symptomatology [15]. Treating parental depression leads to improved asthma management and a reduction in asthma treatment costs [16], suggesting the importance of identification and intervention for depression in these parents. However, less is known about factors that could identify and mitigate risk for depression in parents of children with asthma, particularly for low-income urban families of children of color.
Parental Coping and Children’s Asthma
Research with pediatric populations suggests that how parents cope with a child’s illness is linked to parental emotional well-being [17–19]. Coping can be defined as conscious, volitional efforts to regulate oneself and/or the environment in response to stress [20]. The current study is grounded in an empirically validated theoretical model that has direct implications for intervention with pediatric chronic illness populations [21]. This model proposes that coping occurs across engagement and disengagement dimensions. Engagement strategies include primary control and secondary control coping. Primary control strategies involve active efforts to change a stressor or one’s emotional response to a stressor, such as problem solving, emotional expression, and emotion modulation. Secondary control coping involves efforts to accommodate/adapt to a stressor using strategies such as cognitive restructuring, acceptance, positive thinking, and distraction (i.e., engaging with a thought/activity that is not related to the stressor). In contrast, disengagement coping involves detaching from a stressor by denial, wishful thinking, and avoidance. In this framework, coping strategies may be more or less adaptive depending on the nature and context of the stressor (e.g., primary control may be adaptive in response to stressors that are more controllable or able to change, and secondary control in response to stressors with less controllability [21]). Evidence-based interventions such as cognitive behavioral therapy are consistent with this model of coping, and interventions that enhance secondary control coping in particular have been shown to improve parent and child depressive symptoms [22], suggesting the potential clinical import of this model for improving child asthma outcomes.
Research with families of children with asthma suggests that both primary and secondary control engagement strategies support parents’ mental health and children’s asthma outcomes, while disengagement coping strategies may be less adaptive. One study with mothers of children with asthma found that mothers’ active (i.e., engagement) coping predicted better child quality of life six months later, while avoidance (i.e., disengagement) coping predicted poorer child quality of life [7]. In addition, mothers’ avoidance coping predicted mothers’ own quality of life and anxiety, suggesting that coping may impact both maternal emotional health and children’s disease outcomes [7]. Coping (and its effects on well being) also appears to vary based on demographic factors. For example, higher levels of parental engagement coping strategies, including maintaining family integration, social support and self-esteem, and understanding the health care situation, are related to higher levels of emotional well-being in White but not Black parents [23], and mothers in single-parent families may use fewer of these strategies than mothers in two-parent families [24]. Further, in a sample of Portuguese families, the relation between higher caregiver burden and poorer parental quality of life was mediated by secondary control (e.g., acceptance) coping and disengagement (e.g., denial) coping strategies, and higher denial coping was correlated with lower socioeconomic status (SES) [25]. However, research in pediatric asthma has not typically utilized empirically validated models of coping, which distinguish between primary and secondary control coping strategies. Assessing primary and secondary control separately may yield more specific implications for risk identification and intervention. Nor has previous research examined the relation between parental coping with asthma and depressive symptoms, despite the detrimental impact of parents’ depressive symptoms on children’s asthma management, stress, and disease control.
The Current Study
The current study examines relations among parental coping, parental depressive symptoms, and children’s asthma outcomes (asthma control and partial and full days of school missed due to asthma) in a sample of primarily low-income, urban, racial/ethnic minority families. This study addresses several limitations of the previous literature. First, few studies have examined parental coping in relation to children’s disease outcomes, and the studies that do have used primarily white, middle-SES families [7], despite the evidence that coping with asthma may differ by socioeconomic status and across racial/ethnic groups [23–25]. Our sample, which is primarily low-income, urban, and Black and Latino, represents a population at elevated risk for poorer asthma morbidity and asthma-related functional impairment [26] but underrepresented in this area of research. We also consider the role of demographic factors, including child age, parental education, family income, and race/ethnicity in the relations between parental coping, depressive symptoms, and children’s asthma outcomes. Previous research suggests that parents are less involved in their child’s asthma management as children get older [27,28] which could suggest that parental coping has less of an impact on asthma control for older youth. However, biopsychosocial models of childhood asthma (e.g., the Biobehavioral Family Model [15]) suggest that poorer parental psychosocial functioning may increase child stress, which may lead to poorer asthma control through psychobiologic stress pathways that are independent from asthma management behaviors. Therefore, parental coping may have an impact on child asthma control even in older youth who have more responsibility for self-management. Finally, previous research has not examined how parental coping with asthma relates to parents’ depressive symptoms, despite the evidence implicating parental depressive symptoms in children’s asthma control. In this study, we examine the relation between each dimension of parents’ coping (i.e., primary control, secondary control, and disengagement) and parental depressive symptoms, and examine whether depressive symptoms explain the link between coping and asthma outcomes. By identifying coping strategies associated with lower levels of depressive symptoms, we can suggest intervention targets for parents whose depressive symptoms put their children at greater risk for worse asthma morbidity and for whom other interventions (focused on medication adherence or environmental triggers) may be less effective.
We hypothesized that higher levels of primary and secondary control coping, and lower levels of disengagement coping, would be correlated with fewer depressive symptoms, better asthma control, and fewer full and partial days of school missed due to asthma. We also hypothesized that the relation (i.e., either the direct or indirect effect) between parental coping and child asthma outcomes would be explained by parental depressive symptoms (see Figure 1). Although this study is cross-sectional and we could not test the directionality of the effects, we conceptualized coping as the independent variable and depressive symptoms as the mediator because previous research has suggested that coping is an antecedent of depressive symptoms, and has shown a longitudinal link between coping strategies and later depressive symptoms [29,30]. Finally, we expected that these hypothesized relations would be significant even after accounting for sociodemographic factors (parental education, family income, and child age, race/ethnicity, and gender) associated with children’s asthma outcomes.
Figure 1.
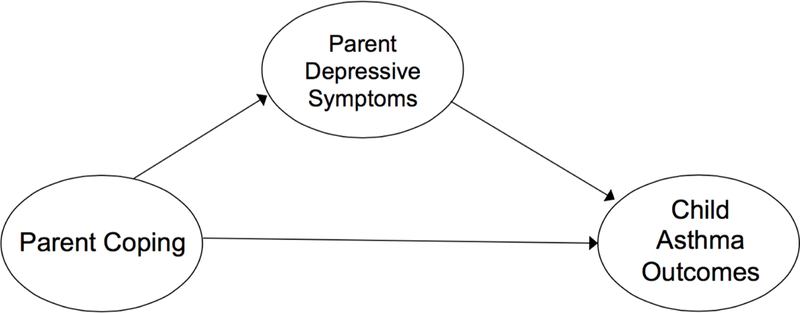
Model of hypothesized relations among parental coping, parental depressive symptoms, and child asthma outcomes.
Method
Participants
Participants were 78 parents/caregivers (hereafter referred to as parents) of children ages 5 to 17 years old with asthma (see Table 1 for demographic information).
Table 1.
Participant Characteristics
| Characteristics | Parent | Child |
|---|---|---|
| Age | M = 38.5 (SD = 8.6) | M = 9.5 (SD = 3.3) |
| Gender | ||
| Female | 90% (N = 70) | 33% (N = 26) |
| Male | 10% (N = 8) | 67% (N = 52) |
| Race/Ethnicity | ||
| Black | 45% (N = 35) | 46% (N = 36) |
| Latino | 37% (N = 29) | 38% (N = 30) |
| White | 12% (N = 9) | 9% (N = 7) |
| Asian | 3% (N = 2) | 3% (N = 2) |
| Other/More than one | 3% (N = 2) | 3% (N = 2) |
| Latino Ethnicity of Parent | ||
| Mexican/Mexican American | 91% (N = 22) | |
| Puerto Rican | 4% (N = 3) | |
| Salvadoran | 1% (N = 1) | |
| Honduran | 1% (N =1) | |
| Did not report | 3% (N = 2) | |
| Language of Parent Questionnaire | ||
| Spanish | 19% (N = 15) | |
| English | 81% (N = 63) | |
| Administration of Parent Questionnaire | ||
| Written | 76% (N=59) | |
| Oral Interview | 24% (N = 19) | |
| Parent Years of Education | M = 12.9 (SD = 3.0) | |
| Parent Marital Status | ||
| Single/Divorced/Separated/Widowed | 56% (N = 44) | |
| Married/Living with Someone | 43% (N = 32) | |
| Family Income | ||
| <$25,000 | 59% (N = 46) | |
| $25,000–50,000 | 30% (N=23) | |
| >$50,000 | 6% (N = 5) | |
Procedure
Participants were recruited from February to April 2014 from a university hospital outpatient clinic specializing in pediatric asthma and allergies, located in a large Midwestern city in the United States. Children are typically referred to this clinic by their primary care physician for uncontrolled moderate to severe persistent asthma. Eligibility requirements included: (a) parents of children ages 5–17 years of age, (b) diagnosis of asthma in the child (obtained via medical records, and confirmed by parent report), (c) child receiving treatment at the specialty clinic, and (d) parent spoke English or Spanish. The study was reviewed and approved by the university’s Institutional Review Board. Parents provided informed consent, and were compensated for participating. Participants completed the study at the clinic at the time of the child’s appointment and it took participants approximately 45 minutes to complete the study.
Measures1
Family demographics.
Parents reported the child’s age, race, and ethnicity and their own age, race, ethnicity, family income, marital status, and years of education.
Coping.
Parents completed the Responses to Stress Questionnaire-Pediatric Asthma version (RSQ [31]). This version of the RSQ was specifically tailored to assess coping in response to asthma-related stressors (e.g., “Not being able to help my child feel better;” “Missing work because of my child’s asthma”). The RSQ includes 57 items in which participants indicate on a 4-point scale how much they use various coping methods, from 0 (not at all) to 4 (a lot). Factor analyses of the RSQ have identified three coping factors [31]: primary control engagement coping (i.e., problem solving, emotional expression, emotional modulation), secondary control engagement coping (i.e., cognitive restructuring, positive thinking, acceptance, distraction), and disengagement coping (i.e., avoidance, denial, wishful thinking). Proportion scores were created by dividing the total score for each factor by the total score for the RSQ [31–33] and were used in the current analyses to control for varying patterns of responses related to the total number of items endorsed.
Depressive symptoms.
Parents completed the Beck Depression Inventory-II (BDI-II [34]), which is composed of 21 items that assess presence and severity of current depressive symptoms. Responses are on a 4-point scale from 0 (absence of symptom) to 3 (severe level of symptom) and yield an overall mean score.
Asthma symptom control.
Parents completed the Asthma Therapy Assessment Questionnaire (ATAQ [35]) about their child. The symptom control subscale was used to assess asthma control (e.g., “wheezing or difficulty breathing” in the last four weeks); higher scores indicate poorer asthma control.
Asthma-related school absenteeism.
Parents reported the number of full days and partial days (i.e., left early or arrived late) of school that their child missed in the past three months due to asthma.
Data Analyses and Statistical Power
We conducted t-tests and correlations (Pearson correlations for continuous data on child age and parent years of education; Spearman correlations for rank order data on family income) to examine if coping, depressive symptoms, and asthma outcomes differed across groups and were associated with child age, gender, and race/ethnicity (Black vs. non-Black children, and Latino vs. non-Latino children), as well as parental education, family income, and format of questionnaire administration. Next, we examined bivariate correlations among study variables (coping, depressive symptoms, and asthma outcomes). Third, we tested regression models for children’s asthma outcomes, controlling for demographic variables that were associated with coping or depressive symptoms, and examined direct and indirect effects of coping, based upon our hypothesis that there would be either direct or indirect effects of coping on asthma outcomes that would be explained by depressive symptoms. In each regression model, demographic variables were entered at Step 1, the coping variable was entered at Step 2, and depressive symptoms were entered at Step 3. Power analyses conducted with G*Power version 3.1 indicated that our sample of 78 participants yielded power of.77 to detect statistical significance for two-tailed correlations of.3 or greater with α =.05. Power was.76 to detect statistical significance for linear multiple regressions of f2 =.15 or greater with four predictors and α =.05. We tested direct and indirect associations using the SPSS macro PROCESS [36]. PROCESS uses bias-corrected bootstrapping confidence intervals to test significance. Bootstrapping is a procedure that involves random resampling to describe the accuracy of an estimate, such as a regression coefficient [37]. Bias-corrected bootstrapping confidence intervals can account for non-linear indirect effects unlike the traditional Sobel test, making them more able to identify that an indirect relationship is significant [38]. PROCESS yields unstandardized regression coefficients and bias corrected 95% confidence intervals (CIs) around the effect, using a resample procedure of 1,000 bootstrap samples. CIs that do not cross zero indicate significant effects (p < .05). Analyses were conducted with SPSS version 23.
Results
Descriptive Analyses and Correlations among Coping, Depressive Symptoms, and Asthma Outcomes
Means, standard deviations, and correlations among all study variables are reported in Table 2. Parents’ mean BDI-II scores indicated normative levels of depressive symptoms; 84% of the sample was below the cutoff score (14) for mild depression.
Table 2.
Correlations Among Parental Coping, Depressive Symptoms, Child Asthma Control, and School Missed Due to Asthma
| M (SD) | α | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1.RSQ Primary Control Coping | 0.19 (0.04) | 0.88 | -- | |||||
| 2.RSQ Secondary Control Coping | 0.27 (0.05) | 0.88 | .17 | -- | ||||
| 3.RSQ Disengagement Coping | 0.14 (0.03) | 0.88 | −.53** | −.44** | -- | |||
| 4.BDI-II | 6.26 (8.48) | 0.92 | −.21 | −.24* | .28* | -- | ||
| 5.ATAQ | 2.65 (2.52) | 0.83 | −.03 | −.07 | .06 | .24* | -- | |
| 6.Full Days of School Missed due to Asthma | 3.09 (6.40) | -- | .170 | .026 | −.10 | .12 | .42** | -- |
| 7.Partial Days of School Missed due to Asthma | 0.88 (1.59) | -- | −.096 | −.23* | .06 | .27* | .48** | .19 |
Note. RSQ = Response to Stress Questionnaire. BDI-II = Beck Depression Inventory-II. ATAQ = Asthma Therapy Assessment Questionnaire (parent report of asthma control). α = internal consistency.
p <.05;
p <.01.
Associations between Study Variables and Sociodemographic Variables
Girls had poorer parent-reported asthma control than boys, t(75) = −2.16, p <.05; no other differences were found between boys and girls on parents’ coping, depressive symptoms, or missed school due to asthma. No differences were found between Black and non-Black children on any study variables. Latino children were less likely to leave school early or arrive late due to asthma compared to non-Latino children, t(72.7) = 2.41, p <.05, but did not differ on parents’ coping, depressive symptoms, asthma control, or full days of school missed. Child age was not significantly correlated with any study variables. Parents’ years of education were positively correlated with secondary control coping (r =.25, p <.05) and negatively correlated with disengagement coping (r = −.41, p <.01), and family income was negatively correlated with disengagement coping (r = −.34, p < .01); neither income nor education were correlated with primary control coping, depressive symptoms, or asthma outcomes. Parents who completed the questionnaires as an oral interview had fewer years of education, t(20.5) = −2.60, p < .05, higher levels of disengagement coping, t(76) = 2.87, p < .01, and higher levels of depressive symptoms, t(24.3) = 2.25, p < .05.
Linear Multiple Regression Analyses Examining the Direct and Indirect Effects of Coping on Asthma Outcomes
Secondary control coping.
The results of the regression models with secondary control coping as the independent variable are presented in Table 3. The model predicting asthma control from secondary control coping was significant. At Step 2, child gender was a significant predictor; at Step 3, gender and depressive symptoms were significant predictors. While the direct effect of secondary control coping on asthma control was not significant, the indirect effect via depressive symptoms was significant. The model predicting partial days of school missed due to asthma from secondary control coping was also significant. At Step 2, Latino ethnicity and secondary control coping were significant predictors; at Step 3, Latino ethnicity and depressive symptoms were significant predictors but secondary control coping was no longer significant. The indirect association between secondary control coping and missed partial days of school via depressive symptoms was not significant.
Table 3.
Regressions Predicting Asthma Control and Partial Days of School Missed from Secondary CC and Depressive Symptoms
| Asthma Control | Partial Days of School Missed | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | t | 95% CI for indirect effect | B | SE | β | t | 95% CI for indirect effect | ||
| Step 1: | Step 1: | ||||||||||
| Parent Education | −.01 | 0.09 | −0.01 | −0.14 | Parent Education | −.05 | 0.06 | −0.09 | 0.78 | ||
| Child Gender | 1.37 | 0.60 | 0.26 | 2.28* | Ethnicity | −1.01 | 0.38 | −0.31 | −2.63* | ||
| Step 2: | Step 2: | ||||||||||
| Parent Education | −.01 | 0.10 | −0.01 | −.08 | Parent Education | −0.02 | 0.06 | −0.04 | −0.33 | ||
| Child Gender | 1.36 | 0.60 | 0.26 | 2.27* | Ethnicity | −1.03 | 0.38 | −0.32 | −2.74* | ||
| Secondary CC | −1.25 | 5.45 | −0.03 | −0.23 | Secondary CC | −6.78 | 3.33 | −0.23 | −2.04* | ||
| Step 3: | Step 3: | ||||||||||
| Parent Education | .00 | .10 | .00 | −.03 | Parent Education | −0.02 | 0.06 | −0.04 | −0.33 | ||
| Child Gender | 1.74 | 0.59 | .33 | 2.97** | Ethnicity | −1.03 | 0.36 | −0.32 | −2.83** | ||
| Secondary CC | 3.00 | 5.37 | .06 | 0.56 | Secondary CC | −5.01 | 3.31 | −0.17 | −1.51 | ||
| BDI-II | .10 | 0.03 | .34 | 2.97** | BDI-II | 0.05 | 0.02 | 0.26 | 2.37** | ||
| Indirect Effect | −4.25 | 2.44 | [−10.84, −0.73] | Indirect Effect | −1.77 | 1.70 | [−6.56, 0.07] | ||||
| Adjusted R2 = 0.13 | Adjusted R2 = 0.16 | ||||||||||
| F (4, 71) = 3.73** | F (4, 69) = 4.43** | ||||||||||
Note. Secondary CC = Secondary control coping. BDI-II = Beck Depression Inventory-II. Ethnicity was categorized as Latino or non-Latino.
p <.05;
p <.01.
Disengagement coping.
The results of the regression models with disengagement coping as the independent variable are presented in Table 4. The model predicting asthma control from disengagement coping was significant. At Step 3, child gender and depressive symptoms were significant predictors. While the direct effect of disengagement coping on asthma control was not significant at either Step 2 or Step 3, the indirect effect via depressive symptoms was significant. The model predicting partial days of school missed due to asthma from disengagement coping was also significant. At Step 3, Latino ethnicity and depressive symptoms were significant predictors. The direct effect of disengagement coping on missed partial days of school was not significant at either Step 2 or Step 3, and the indirect association between disengagement coping and missed partial days of school via depressive symptoms was not significant.
Table 4.
Regressions Predicting Asthma Control and Partial Days of School Missed from Disengagement Coping and Depressive Symptoms
| Asthma Control | Partial Days of School Missed | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Β | SE | β | t | 95% CI for indirect effect | Β | SE | β | t | 95% CI for indirect effect | ||
| Step 1: | Step 1: | ||||||||||
| Parent Education | 0.02 | 0.11 | 0.03 | 0.20 | Parent Education | −0.01 | 0.72 | −.02 | −0.13 | ||
| Child Gender | 1.25 | 0.62 | 0.24 | 2.00* | Ethnicity | −0.90 | 0.41 | −0.28 | −2.23* | ||
| Family Income | −0.25 | 0.41 | −0.08 | −0.61 | Family Income | −0.23 | 0.26 | −0.12 | −0.90 | ||
| Step 2: | Step 2: | ||||||||||
| Parent Education | 0.02 | 0.11 | 0.03 | 0.18 | Parent Education | 0.00 | 0.07 | 0.00 | −0.02 | ||
| Child Gender | 1.25 | 0.63 | 0.24 | 1.98 | Ethnicity | −0.96 | 0.42 | −0.30 | −2.29* | ||
| Family Income | −0.25 | 0.42 | −0.08 | −0.60 | Family Income | −0.20 | 0.27 | −0.10 | −0.73 | ||
| Disengagement | −0.49 | 12.9 | −0.01 | −0.04 | Disengagement | 4.67 | 8.43 | 0.07 | 0.55 | ||
| Step 3: | Step 3: | ||||||||||
| Parent Education | −0.01 | 0.11 | −0.01 | −0.07 | Parent Education | −0.01 | 0.07 | −0.02 | −0.14 | ||
| Child Gender | 1.70 | 0.62 | 0.33 | 2.75** | Ethnicity | −0.93 | 0.40 | 0.29 | −2.31* | ||
| Family Income | −0.14 | 0.40 | −0.04 | −0.35 | Family Income | −0.16 | 0.26 | −0.08 | −0.61 | ||
| Disengagement | −11.7 | 12.8 | −0.12 | −0.92 | Disengagement | 0.47 | 8.30 | 0.01 | 0.06 | ||
| BDI-II | 0.10 | 0.04 | 0.35 | 2.88** | BDI-II | 0.06 | 0.02 | 0.29 | 2.47* | ||
| Indirect Effect | 11.25 | 7.16 | [1.33, 29.27] | Indirect Effect | 4.21 | 3.93 | [−0.38, 16.02] | ||||
| Adjusted R2 = 0.17 | Adjusted R2 = 0.18 | ||||||||||
| F (5, 66) = 2.69* | F (5, 64) = 2.71* | ||||||||||
Note. BDI-II = Beck Depression Inventory-II. Ethnicity was categorized as Latino or non-Latino.
p <.05;
p <.01.
Exploratory analyses of interactions.
Given the significant main effects of child gender and Latino ethnicity, we explored interactions between these variables and depressive symptoms in predicting asthma outcomes. Additionally, given previous research suggesting that parent management of children’s asthma varies by child age, we also examined the interaction between child age and parental coping in predicting asthma outcomes. None of the interaction terms were significant and were dropped from the final analyses.
Discussion
The current study found significant associations among parental coping, depressive symptoms, and children’s asthma control and school attendance. Higher levels of secondary control coping were correlated with fewer depressive symptoms in parents, and fewer partial days of school missed in children with asthma. Disengagement coping was correlated with higher depressive symptoms, but not with asthma outcomes. Primary control coping was not correlated with depressive symptoms or asthma outcomes. Higher levels of depressive symptoms were correlated with poorer asthma control and more partial days of school missed. Further, we found indirect effects of parents’ secondary control coping and disengagement coping on children’s asthma control that occurred via parents’ depressive symptoms, and a direct effect of secondary control coping on partial days of school missed that was accounted for by depressive symptoms. Study variables were significantly associated with demographic variables. Higher levels of secondary control coping were correlated with higher parental education, and higher levels of disengagement coping were correlated with lower parental education and family income. Girls had poorer asthma control than boys, and Latino children had fewer partially missed days of school than non-Latino children. Notably, the direct and indirect effects of parent coping on child asthma outcomes remained significant after controlling for these demographic factors.
Our finding that parents’ secondary control and disengagement coping were linked to their depressive symptoms and their children’s asthma outcomes extends previous research on coping in parents of children with asthma. Our results regarding disengagement coping are consistent with previous research linking parents’ disengagement coping with poorer child quality of life [7], and extend prior findings by demonstrating the effect of disengagement coping on child asthma control occurs via parental depressive symptoms. Our findings on secondary control also extend previous studies that highlighted the importance of various engagement coping strategies for parents’ emotional functioning and children’s asthma outcomes [7,22,24], but were limited in their use of empirically validated models of coping, and did not distinguish between primary control and secondary control. Our findings suggest that secondary control coping is a uniquely adaptive response for low-income urban families, for whom contextual risks (e.g., environmental triggers, socioeconomic barriers to treatment) may be uncontrollable and unamenable to behavioral intervention without broader policy changes. Indeed, in low-income children with asthma, children’s own use of secondary control coping is linked to better mental health and disease-related outcomes [39,40]. Likewise, utilizing secondary control coping may be important for parents in low-income, urban environments. Intervention approaches for this population could involve screening by providers (e.g., nurses, physicians) to assess parents’ secondary control and disengagement coping at the child’s medical appointment, and providing at-risk parents with interventions in that setting. For example, family-based cognitive behavioral interventions for depressed parents and their children have been shown to enhance secondary control coping skills and reduce depression [21]. Future research should seek to adapt these interventions for low-income, urban families of children with asthma.
While both partial and full days of school missed due to asthma were associated with parents’ reports of asthma control, only partial days of school were associated with parents’ secondary control and disengagement coping and depressive symptoms. Previous research has not distinguished between partial and full days of school missed, but our results suggest that missing part of the school day is a distinct outcome that may be related to fewer parental resources (i.e., material and/or psychosocial resources). Future research should examine the functional impact of missing part of the school day due to asthma.
Child age was not associated with parental coping or depressive symptoms, or with asthma outcomes, and did not significantly interact with parental coping in our regression models predicting asthma outcomes. Although previous research indicates that parents’ role in their children’s asthma management shifts with age, our results suggest that parental coping may impact child asthma outcomes not through asthma management, but through other processes that affect asthma control independently from child age, such as the child’s stress levels and stress regulation [15].
We also found that girls had poorer asthma control, while Latino children had fewer partial school days missed due to asthma, independent of the effects of secondary control coping and depressive symptoms, suggesting that these gender and ethnic differences in asthma outcomes in our low-income, urban sample are not explained by parental coping or mental health processes. Our results showing poorer asthma control in girls is consistent with previous findings that asthma is more severe and undertreated in girls compared to boys as they enter adolescence [41]. Our findings on Latino compared to non-Latino children may reflect protective factors that support asthma management in low-income Latino families, such as high levels of family cohesion or parents born outside the U.S. [42]. Given the variability of these factors among Latinos, more research is needed to understand ethnic group differences in asthma control.
Study Strengths, Limitations, and Directions for Future Research
Study strengths such as the racially/ethnically diverse, predominantly low-income sample, use of an empirically validated measure of coping, and direct implications for prevention and intervention efforts with families, should be considered along with study limitations. The cross-sectional design limited our ability to test the directions of the effects. While we conceptualized coping as the predictor and asthma control and missed school as the outcomes, it is also possible that when children’s asthma is poorly controlled, the stressors of the disease limit parents’ ability to cope effectively and increase risk for depressive symptoms. Similarly, although we conceptualized coping as the independent variable and depressive symptoms as the mediator, it is also possible that depressive symptoms may precede and lead to less secondary control and more disengagement coping. Future research should use a multi-wave longitudinal design to examine the directions of these effects. Another limitation is our use of parent report of asthma control, rather than physiological measures of disease control, which could have increased error related to the monomethod design, although our outcomes (parent reported disease control and school missed due to asthma) likely reflect children’s actual functional impairment related to the disease. Future research would benefit from utilizing information from medical records, including physiological measures (e.g., pulmonary function test results) and school attendance data in addition to self-report data. Additionally, while we accounted for several demographic factors that have been linked to children’s asthma morbidity, our assessment of income was not sensitive enough to capture much variability in the predominantly low-income sample, which may have limited our ability to detect significant effects related to socioeconomic variables. Another limitation relates to our clinic-based recruitment strategy. While the clinic population consists predominantly of children referred for uncontrolled asthma, the families who are treated at the clinic may still manage their child’s asthma better than non-treatment seeking, community samples. Additional research with community-based samples is needed to generalize findings further. We also found that parents who completed the survey as an oral interview had higher levels of disengagement coping and depressive symptoms, as well as fewer years of education. Therefore, it is possible that the survey administration format affected how participants responded, although this limitation is balanced by the potential increase in feasibility and acceptability of the study for participants with lower education levels. Finally, while the sample represented a high-risk population that is typically underrepresented in pediatric coping research, the findings may not generalize to all families of children with asthma, including families of White children and those from middle- or higher-income backgrounds.
Conclusions
This study extends previous findings implicating parental depressive symptoms in children’s asthma control. Our results suggest that parents’ secondary control and disengagement coping are important factors in parental depressive symptoms, child disease outcomes, and school attendance in children with asthma. Pediatric asthma interventions may benefit from strengthening parental secondary control coping strategies, such as cognitive restructuring and acceptance, which could have a positive impact on both parental mental health and children’s asthma outcomes.
Acknowledgments
This work was supported by the National Institute of Mental Health (grant number T32 MH067631) and a grant from the Society of Pediatric Psychology.
Funding
National Institute of Mental Health (T32 MH067631)
Society of Pediatric Psychology (Diversity Research Grant)
Footnotes
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
All measures were translated into Spanish, and Spanish versions were pretested and refined based on feedback of bilingual research staff. The demographic questionnaire and the Response to Stress Questionnaire were adapted from similar versions translated and backtranslated by the first author and other bilingual researchers using the iterative process described by Brislin [43]. The Spanish version of the Asthma Therapy Assessment Questionnaire is distributed by Merck & Company, Inc., and the Spanish version of the Beck Depression Inventory-II was previously translated and validated with Spanish-speaking participants [44].
References
- 1.Diette G, Markson L, Skinner E, Nguyen T, Algatt-Bergstrom P, Wu A. Nocturnal asthma in children affects school attendance, school performance, and parents’ work attendance. Arch Pediatr Adolesc Med. 2000;154(9):923. [DOI] [PubMed] [Google Scholar]
- 2.Wang L, Zhong Y, Wheeler L. Direct and indirect costs of asthma in school-age children. Prev Chronic Dis. 2016;2(1):A11. [PMC free article] [PubMed] [Google Scholar]
- 3.Easter G, Sharpe L, J. Hunt C. Systematic review and meta-analysis of anxious and depressive symptoms in caregivers of children with asthma. J Pediatr Psychol. 2015;40(7):623–632. [DOI] [PubMed] [Google Scholar]
- 4.Martínez K The role of caregivers’ depressive symptoms and asthma beliefs on asthma outcomes among low-income puerto rican children. J Asthma. 2009;46(2):136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kub J, Jennings J, Donithan M, Walker J, Land C, Butz A. Life events, chronic stressors, and depressive symptoms in low-income urban mothers with asthmatic children. Public Health Nurs. 2009;26(4):297–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolf J, Miller G, Chen E. Parent psychological states predict changes in inflammatory markers in children with asthma and healthy children. Brain Behav Immun. 2008;22(4):433–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sales J, Fivush R, Teague G. The role of parental coping in children with asthma’s psychological well-being and asthma-related quality of life. J Pediatr Psychol. 2007;33(2):208–219. [DOI] [PubMed] [Google Scholar]
- 8.Clark N, Dodge J, Shah S, Thomas L, Andridge R, Awad D. A current picture of asthma diagnosis, severity, and control in a low-income minority preteen population. J Asthma. 2010;47(2):150–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gold D, Wright R. Population disparities in asthma. Annu Rev Public Health. 2005;26(1):89–113. [DOI] [PubMed] [Google Scholar]
- 10.Leão L High prevalence of depression amongst mothers of children with asthma. J Asthma. 2009;46(4):388–391. [DOI] [PubMed] [Google Scholar]
- 11.Shalowitz M, Berry C, Quinn K, Wolf R. The relationship of life stressors and maternal depression to pediatric asthma morbidity in a subspecialty practice. Ambul Pediatr. 2001;1(4):185–193. [DOI] [PubMed] [Google Scholar]
- 12.Weil C, Wade S, Bauman L, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104(6):1274–1280. [DOI] [PubMed] [Google Scholar]
- 13.Guevara J, Mandell D, Danagoulian S, Reyner J, Pati S. Parental depressive symptoms and children’s school attendance and emergency department use: A nationally representative study. Matern Child Health J. 2013;17(6):1130–1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bartlett S, Krishnan J, Riekert K, Butz A, Malveaux F, Rand C. Maternal depressive symptoms and adherence to therapy in inner-city children with asthma. Pediatrics. 2004;113(2):229–237. [DOI] [PubMed] [Google Scholar]
- 15.Wood B, Miller B, Lehman H. Review of family relational stress and pediatric asthma: The value of biopsychosocial systemic models. Family process. 2015:54(2):376–89. [DOI] [PubMed] [Google Scholar]
- 16.Perry C Does treating maternal depression improve child health management? The case of pediatric asthma. J Health Econ. 2008;27(1):157–173. [DOI] [PubMed] [Google Scholar]
- 17.Bachanas P, Kullgren K, Schwartz K, McDaniel J, Smith J, Nesheim S. Psychological adjustment in caregivers of school-age children infected with HIV: Stress, coping, and family factors. J Pediatr Psychol. 2001;26(6):331–342. [DOI] [PubMed] [Google Scholar]
- 18.Compas B, Bemis H, Gerhardt C, Dunn M, Rodriguez E, Desjardins L, Preacher K, Manring S, Vannatta K. Mothers and fathers coping with their children’s cancer: Individual and interpersonal processes. Health Psychol. 2015;34(8):783–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zelikovsky N, Schast A, Jean-Francois D. Parent stress and coping: waiting for a child to receive a kidney transplant. J Clin Psychol Med Settings. 2007;14(4):320–329. [Google Scholar]
- 20.Compas B, Connor-Smith J, Saltzman H, Thomsen A, Wadsworth M. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychol Bull. 2001;127(1):87–127. [PubMed] [Google Scholar]
- 21.Compas B, Jaser S, Dunn M, Rodriguez E. Coping with chronic illness in childhood and adolescence. Annu Rev Clin Psychol. 2012;8(1):455–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Compas B, Forehand R, Thigpen J, Keller G, Hardcastle E, Cole D, Potts J, Watson K, Rakow A, Colletti C, Reeslund K. Family group cognitive–behavioral preventive intervention for families of depressed parents: 18-and 24-month outcomes. J Consult Clin Psychol. 2011:79(4):488–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee E, Jackson B, Parker V, DuBose L, Botchway P. Influence of family resources and coping behaviors on well-being of African American and Caucasian parents of school-age children with asthma. ABNF Journal. 2009;20(1):5–11. [PubMed] [Google Scholar]
- 24.Brazil K, Krueger P. Patterns of family adaptation to childhood asthma. J Pediatr Nurs. 2002;17(3):167–173. [DOI] [PubMed] [Google Scholar]
- 25.Silva N, Crespo C, Carona C, Canavarro M. Mapping the caregiving process in paediatric asthma: Parental burden, acceptance and denial coping strategies and quality of life. Psychol & Health. 2015;30(8):949–968. [DOI] [PubMed] [Google Scholar]
- 26.Bryant-Stephens T Asthma disparities in urban environments. J Allergy Clin Immun. 2009;123(6):1199–1206. [DOI] [PubMed] [Google Scholar]
- 27.Orrell-Valente J, Jarlsberg L, Hill L, Cabana M. At what age do children start taking daily asthma medicines on their own? Pediatrics. 2008:122(6):e1186–e1192. [DOI] [PubMed] [Google Scholar]
- 28.Wade SL, Islam S, Holden G, Kruszon-Moran D, Mitchell H. Division of responsibility for asthma management tasks between caregivers and children in the inner city. J Dev Behav Pediatr. 1999:20(2):93–98. [DOI] [PubMed] [Google Scholar]
- 29.Berghuis JP, Stanton AL. Adjustment to a dyadic stressor: a longitudinal study of coping and depressive symptoms in infertile couples over an insemination attempt. J Consult Clin Psychol. 2002:70(2):433–438. [DOI] [PubMed] [Google Scholar]
- 30.Seiffge-Krenke I, Klessinger N. Long-term effects of avoidant coping on adolescents’ depressive symptoms. J Youth Adolesc. 2000:29(6):617–630. [Google Scholar]
- 31.Connor-Smith J, Compas B, Wadsworth M, Thomsen A, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. J Consult Clin Psychol. 2000;68(6):976–992. [PubMed] [Google Scholar]
- 32.Osowiecki D, Compas B. A prospective study of coping, perceived control, and psychological adaptation to breast cancer. Cognitive Ther Res. 1999;23(2):169–180. [Google Scholar]
- 33.Vitaliano P, DeWolfe D, Maiuro R, Russo J, Katon W. Appraised changeability of a stressor as a modifier of the relationship between coping and depression: A test of the hypothesis of fit. J Pers Soc Psychol. 1990;59(3):582–592. [DOI] [PubMed] [Google Scholar]
- 34.Beck A, Steer R, Brown G. BDI-II, Beck depression inventory. San Antonio, Tex.: Psychological Corp.; 1996. [Google Scholar]
- 35.Skinner E, Diette G, Algatt-Bergstrom P, Nguyen T, Clark R, Markson L, Wu A. The Asthma Therapy Assessment Questionnaire (ATAQ) for children and adolescents. Dis Manag. 2004;7(4):305–313. [DOI] [PubMed] [Google Scholar]
- 36.Hayes A Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-based Approach. New York: Guilford Press; 2013. [Google Scholar]
- 37.Efron B, Tibshirani R. An introduction to the bootstrap. Boca Roatan, FL: CRC Press; 1994. [Google Scholar]
- 38.Preacher K, Hayes A. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Beh Res Meth Ins C. 2004;36(4):717–731. [DOI] [PubMed] [Google Scholar]
- 39.Chen E, Strunk R, Trethewey A, Schreier H, Maharaj N, Miller G. Resilience in low-socioeconomic-status children with asthma: Adaptations to stress. J Allergy Clin Immun. 2011;128(5):970–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rodríguez E, Kumar H, Draeger A, Sánchez-Johnsen L. Coping with asthma in racially and ethnically diverse urban children: the role of emotional problems in disease control. Child Health Care. 2016; doi: 10.1080/02739615.2015.1124771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Almqvist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2008;63(1):47–57. [DOI] [PubMed] [Google Scholar]
- 42.Koinis-Mitchell D, Sato A, Kopel S, McQuaid E, Seifer R, Klein R, Esteban C, Lobato D, Ortega A, Canino G, Fritz G. Immigration and acculturation-related factors and asthma morbidity in Latino children. J Pediatr Psychol. 2011;36(10):1130–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brislin W Back-translation for cross-cultural research. J Cross Cult Psychol. 1970;1:185–216. [Google Scholar]
- 44.Penley J, Wiebe J, & Nwosu A . Psychometric properties of the Spanish Beck Depression Inventory-II in a medical sample. Psychol Assessment. 2003;15(4):569–577. [DOI] [PubMed] [Google Scholar]


