Abstract
Objective
To examine the feasibility, acceptability, and effects of a home-based morning bright light treatment on pain, mood, sleep, and circadian timing in US veterans with chronic low back pain.
Design
An open treatment trial with a seven-day baseline, followed by 13 days of a one-hour morning bright light treatment self-administered at home. Pain, pain sensitivity, mood, sleep, and circadian timing were assessed before, during, and after treatment.
Setting
Participants slept at home, with weekly study visits and home saliva collections.
Participants
Thirty-seven US veterans with medically verified chronic low back pain.
Methods
Pain, mood, and sleep quality were assessed with questionnaires. Pain sensitivity was assessed using two laboratory tasks: a heat stimulus and an ischemia stimulus that gave measures of threshold and tolerance. Sleep was objectively assessed with wrist actigraphy. Circadian timing was assessed with the dim light melatonin onset.
Results
Morning bright light treatment led to reduced pain intensity, pain behavior, thermal pain threshold sensitivity, post-traumatic stress disorder symptoms, and improved sleep quality (P < 0.05). Phase advances in circadian timing were associated with reductions in pain interference (r = 0.55, P < 0.05).
Conclusions
Morning bright light treatment is a feasible and acceptable treatment for US veterans with chronic low back pain. Those who undergo morning bright light treatment may show improvements in pain, pain sensitivity, and sleep. Advances in circadian timing may be one mechanism by which morning bright light reduces pain. Morning bright light treatment should be further explored as an innovative treatment for chronic pain conditions.
Keywords: Circadian, Bright Light, Chronic Low Back Pain
Introduction
Approximately 50% of US military veterans report that they experience pain on a regular basis [1,2], most commonly in the back and head [1]. One common approach to treating chronic pain is with opioid analgesic medications, which are not always effective, have negative side effects, and are widely misused [3,4]. Cognitive behavioral therapy (CBT) and exercise are available nonpharmacological treatments, but CBT requires access to specialized personnel and exercise requires high participant motivation. Thus, there is an urgent need to develop readily available, affordable, safe, and practical nonpharmacological approaches to managing chronic pain.
Results of meta-analyses indicate that exposure to bright light in the morning can improve sleep [5] and mood [6]. Therapies designed around bright light consist of having participants receive high-intensity ultraviolet-free light, most typically from a light box, during morning hours. In contrast to pharmacological treatments, morning bright light treatment is associated with few side effects, which often spontaneously remit [7,8], and patients rarely discontinue treatment due to side effects [8]. Bright light devices are considered safe, with participants showing no changes in ophthalmologic exams after six years of daily use in the fall and winter months [9]. The sleep and mood benefits of morning bright light treatment may in part be attributable to circadian phase advances (shifts earlier in the timing of the body clock) which often occur following morning bright light exposure [10].
Chronic pain is a multidimensional phenomenon, inter-related with many factors, including negative mood and poor sleep. Moreover, PTSD, depressive, and anxiety symptoms are all associated with elevated pain intensity [11,12]. Noting that people experiencing sleep disturbance are at greater risk of developing chronic pain [11,13–15] and that improving sleep reduces pain and pain sensitivity [16,17], we proposed that a treatment that improves sleep and mood—morning bright light treatment—may reduce pain intensity among people with chronic low back pain.
We recently reported results from a small sample of women with fibromyalgia who underwent bright light treatment. They received a daily one-hour morning bright light treatment, generated from light boxes, for six consecutive days. The women reported clinically meaningful improvements in pain and function [18]. The purpose of the current study was to examine the feasibility, acceptability, and effects of a similar home-based self-administered morning bright light treatment on pain, mood, sleep, and circadian timing in a new patient population, US veterans with chronic low back pain. To our knowledge, bright light treatment has never been tested as a potential treatment for chronic low back pain. Based on the literature and our previous findings, we hypothesized that the morning bright light treatment would reduce pain and pain sensitivity, improve function, mood, and sleep, and advance circadian timing (shift the timing of the body clock earlier). Further, if morning bright light treatment works partly via changes in circadian timing, then circadian timing changes should correlate with outcome changes. Alternatively, patient expectations of achieving benefits may also represent a mechanism, albeit not specific to bright light. To address this issue, we examine correlations among participant expectations and pre- to post-treatment changes in circadian timing and outcomes.
Methods
Participants
Thirty-seven US military veterans (10 females, 27 males) who reported chronic low back pain were enrolled in the study (Table 1). The veterans were required to provide proof of veteran status (e.g., DD Form 214, a certificate of release or discharge from active military duty). The presence of significant chronic low back pain was determined from a self-report of chronic low back pain for at least the previous six months, with an average intensity of at least 4/10 (1 = no pain to 10 = worst pain possible). Veterans also signed an authorization form to obtain their medical records regarding their back pain, which was used to verify a preexisting complaint of chronic low back pain to a medical provider.
Table 1.
Demographic characteristics of the sample of US veterans with chronic low back pain
| Characteristic | Total Sample (N = 37) |
|---|---|
| Sex, No. (%) | |
| Female | 10 (27) |
| Male | 27 (73) |
| Age, mean (SD), y | 48.4 (14.1) |
| Race, No. (%) | |
| African American | 22 (59) |
| White | 8 (22) |
| Hispanic | 5 (14) |
| More than 1 race | 2 (5) |
| Partner status, No. (%) | |
| Single | 18 (49) |
| Domestic partner | 19 (51) |
| Educational status, No. (%) | |
| Postgraduate degree | 1 (3) |
| College graduate | 17 (46) |
| Some college | 15 (41) |
| High school or less | 1 (3) |
| No answer | 3 (8) |
| Body mass index, mean (SD), kg/m² | 30.0 (5.8) |
Exclusion criteria were a) other significant chronic disease (apart from medication-controlled diabetes and hypertension); b) other condition associated with chronic pain (including chronic headaches, fibromyalgia, complex regional pain syndrome, rheumatoid arthritis); c) past or present psychosis or bipolar disorder; d) present alcohol or substance abuse problems; e) suicidal ideation; f) high risk for obstructive sleep apnea, restless leg syndrome, or seasonal affective disorder [19–21]; g) taking daily nonsteriodal anti-inflammatory medications (NSAIDs) and/or beta-blockers (these medications suppress melatonin) [22,23]. Accepted subjects reported no retinal pathology or eye surgery, and none were taking photosensitizing medications. No subjects were color blind as determined from the Ishihara test, and none had any prior experience with bright light treatment. Prescribed or over-the-counter sleep aids (apart from exogenous melatonin) and antidepressants were permitted, provided that medication use remained stable 30 days before and during the study. No subjects had worked any night shifts or traveled outside the Central Time Zone in the month preceding the study. The study was approved by the Rush University Medical Center Institutional Review Board, and all participants gave written informed consent before participation. This clinical trial was registered as NCT02373189 on clinicaltrials.gov.
Five veterans failed drug and alcohol screening on the first day of the study and did not participate further. An additional seven veterans dropped out before the start of the light treatment due to a variety of reasons, including jail time, job offers, and family crises. Therefore, a total of 25 veterans received the bright light treatment.
Protocol
This was a single-arm trial, in which all subjects received morning bright light treatment. The study consisted of a seven-day baseline during which subjects slept at home on their usual sleep schedule (ad lib). This baseline was followed by a daily one-hour morning bright light treatment for 13 consecutive days. Subjects underwent a baseline pretreatment assessment, a midtreatment assessment after six days of morning bright light treatment, and a final treatment assessment after a further seven days of morning bright light treatment. These assessments involved subjects visiting the Department of Behavioral Sciences at Rush University Medical Center at a set time in the morning. Upon arrival, they were breathalyzed for alcohol, underwent pain sensitivity testing, completed questionnaires, and then returned home for saliva sampling, used for later determination of circadian timing (details below). Research staff also visited the veterans in their homes to set up the light boxes for the one hour per day morning bright light treatment after baseline, midtreatment to confirm the light box setup was unchanged, and finally post-treatment to collect the light boxes.
Wrist Actigraphy
All subjects wore a wrist actigraphy monitor (30-second epochs, Actiwatch Spectrum, Respironics, Bend, OR, USA) on their nondominant wrist throughout the baseline and 13 days of bright light treatment and were instructed to complete sleep diaries and press the event marker on the actigraphy monitor before and after sleep during each of these days. The subjects were also instructed to ensure that the photosensor on the wrist monitor was not covered during the bright light treatment. The wrist actigraphy data were analyzed with the Actiware 6.0.9 program (Respironics, Bend, OR, USA). The setting of nightly rest intervals for analysis was guided by the event markers, sleep diaries, light data, and activity levels [24]. Objective actigraphic estimates of sleep onset time (clock time of the first epoch scored as sleep in each rest interval), wake time (clock time of the last epoch scored as sleep in each rest interval), total sleep time (number of minutes scored as sleep in each rest interval), and sleep efficiency (proportion of time from sleep onset to waking in each rest interval, scored as sleep, expressed as a percentage) were extracted for each study day. During the 13 days of bright light treatment, the subjects were advised to maintain their habitual sleep duration, and naps were discouraged to improve nighttime sleep efficiency. The sleep variables from the three nights of sleep immediately before the assessments were each averaged to estimate sleep just before the assessments.
Questionnaires
During the assessment visits, subjects completed questionnaires to assess pain, function, mood, and sleep. Pain and function were assessed with the PROMIS Pain Intensity, Pain Behavior, Pain Interference, and Physical Function domains. Depressive symptoms were assessed with the Center for Epidemiologic Studies Short Depression Scale (CES-D 10) [25], anxiety symptoms with the State Trait Anxiety Inventory (STAI) [26], and post-traumatic stress symptoms with the PTSD Checklist for DSM-5 (PCL-5) [27]. Subjective reports of sleep quality were collected with the Pittsburgh Sleep Quality Index (PSQI) [28] and the Insomnia Severity Index (ISI) [29].
Test of Pain Sensitivity
There were two pain sensitivity tests. First, participants underwent an ischemic pain task based on procedures described by Maurset et al. [30]. Participants first engaged in two minutes of dominant forearm muscle exercise using a hand dynamometer at 50% of his or her maximal grip strength, as determined before beginning the laboratory procedures. Then they were asked to raise their dominant forearm over their head for 15 seconds. A manual blood pressure cuff was then inflated on the participant’s dominant biceps to 200 mmHg SBP, the arm was lowered, and the cuff remained inflated until tolerance was reached, up to a maximum of eight minutes. Participants were instructed to indicate when they first experienced pain after the cuff was inflated, with this ischemic pain threshold defined as the time elapsed from task onset to when the sensation was first described as “painful.” Ischemic pain tolerance was defined as the time elapsed between onset of the pain task and participants’ expressed desire to terminate the task (set at a maximum of eight minutes).
The second laboratory pain task was a heat pain task using a Medoc TSAII NeuroSensory Analyzer (Medoc US, Minneapolis, MN, USA). This equipment was used to assess thermal pain threshold and tolerance using an ascending method of limits protocol, as in several previous studies [31–33]. Four trials each were conducted for thermal pain threshold and tolerance, with each trial conducted sequentially at one of four different nonoverlapping sites on the nondominant ventral forearm. An interval of 30 seconds between successive stimuli was employed. For pain threshold trials, the probe started at an adaptation temperature of 32°C, with the temperature increasing at a ramp rate of 0.5°C/sec until the participant indicated that the stimulus had begun to feel “painful” by depressing a button on a computer mouse. For each tolerance trial, the probe started at an adaptation temperature of 40°C, with the temperature increasing at a ramp rate of 0.5°C/sec until the participant indicated that maximum tolerance had been reached. Means of the four thermal pain threshold and tolerance trials were separately derived for use in analyses. Maximum possible tolerance temperature was 51°C due to an automatic hardware cutoff built into the TSAII device to ensure participant safety. Before beginning the first laboratory session, all participants underwent standardized training to familiarize themselves with the thermal stimulus device and the concepts of pain threshold and tolerance.
Circadian Phase Assessments
At the end of the assessment visits, subjects were trained in the use of a validated home saliva collection kit [34,35] to assess the dim light melatonin onset (DLMO). The DLMO is the most reliable circadian phase marker in humans [36,37]. Key features of the home saliva collection kit included 1) a track cap bottle (MEMS, Aardex, Switzerland), which provides objective markers of the sample times; 2) a photosensor (Actiwatch Spectrum, Philips, Bend, OR, USA) worn around the neck on top of clothing to objectively verify light <50 lux (to avoid melatonin suppression); and 3) a label dispenser to avoid incorrect sample labeling. A checklist and timer with alarms guided the subject to dim their home lighting and conduct the saliva collection. Neither toothpaste nor mouthwash was permitted. Small snacks and fluids were permitted, except in the 10 minutes before each sample, and subjects were required to rinse and brush their teeth with water while remaining seated 10 minutes before each sample if they had consumed food or drink. At the baseline assessment, subjects sampled their saliva with salivettes (Sarstedt, Newton, NC, USA) every 30 minutes starting six hours before and until their average bedtime. At the midtreatment and post-treatment assessments, subjects began to sample their saliva two hours earlier to optimally capture a phase advance (shift earlier) in the DLMO. The subjects were prompted by phone calls to refrain from consuming NSAIDs 72 hours before (replacement acetaminophen was provided) and alcohol/caffeine 24 hours before the saliva collections to avoid confounding the measurement of melatonin. The frozen saliva samples were collected by research staff during the home visits. Upon return to Rush University Medical Center, the samples were thawed, centrifuged, refrozen, and shipped in dry ice to Solidphase, Inc. (Portland, ME, USA). Technicians there performed the direct radioimmunoassay using standard Buhlmann kits with assay sensitivity of 0.5 pg/mL and intra- and interassay coefficient of variation <7.5% at 3 pg/mL. A DLMO was calculated for each phase assessment as the clock time (with linear interpolation) when the melatonin concentration exceeded the mean of three low consecutive daytime values plus twice the standard deviation of these points [38,39].
Bright Light Treatment at Home
The morning after the baseline assessment, research staff visited subjects in their homes to set up the light boxes. The research staff discussed with the subject their preferred activity during the light treatment (e.g., watching TV, working at a computer, reading, etc.). Two broad-spectrum white light boxes (33 × 18 × 55 cm, EnergyLight HF3318/60, Philips, Inc.) were set up to the left and right at a distance that allowed the subject to view a TV or computer in front of them (Figure 1). Each subject’s comfort was first maximized using comfortable chairs and/or cushions, as appropriate, and then the light boxes were positioned to maximize light intensity (Extech EA33 light meter, Nashua, NH, >3,000 lux). A 60-cm string was taped to the base of each light box to remind the subjects how close they needed to sit near the light boxes, and painter’s tape was placed around the base of each light box to show where the boxes should remain. The morning light treatment was for one hour per day for a total of 13 days and started each morning at the subject’s average wake time (derived from the baseline week of wrist actigraphy) or up to one hour earlier to accommodate morning social responsibilities (e.g., work, child care) [40]. A photosensor (Actiwatch Spectrum, Philips, Inc., Bend, OR, USA) was taped facing inwards to the outside of each light box to confirm adherence. An alarm clock was set to the start of the bright light treatment and was placed near the light boxes (subjects also set their home alarm clock). Subjects were given a list of written reminders: a) do not permit anyone to touch the light boxes; b) only turn on light boxes during the scheduled time; and c) turn on all ambient lighting during light treatment time. At the end of the light box set up, subjects completed a treatment expectation item of 1 = “expect to be completely pain free” to 7 = “expect no change.”
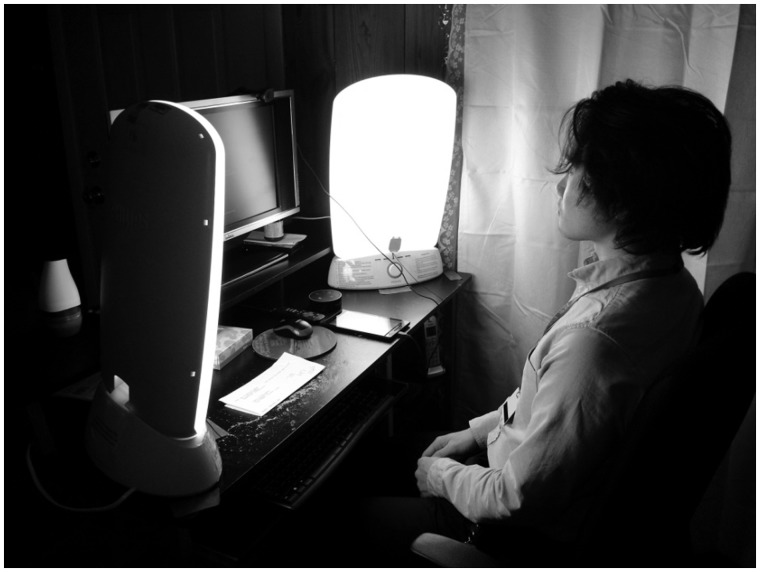
Figure 1.
A research staff member sitting at a participant’s desk after the light boxes were set up. Two light boxes were used: one light box was positioned slightly to the left, and one light box was positioned slightly to the right so that the participant could work on a computer or watch TV between them.
Research staff phoned each subject daily, shortly after the start of the light treatment, to confirm correct use of the light boxes, ensure that the photosenor on their wrist monitor was uncovered, and assess potential side effects. Research staff also visited the subjects at home at midtreatment (after six days of light treatment) to confirm that the light box set up was unchanged and at post-treatment (after 13 days of light treatment) to collect the light boxes. During this post-treatment home visit, subjects completed a treatment satisfaction item of 1 = “not satisfied at all” to 10 = “extremely satisfied.”
Statistical Analysis
To examine the change in the measures between baseline, after six days, and after 13 days of light treatment, we used a semiparametric generalized estimating equation regression model with an identity link function and an exchangeable working correlation matrix to account for correlations of the outcome measures over time. This nonparametric approach remains robust with smaller sample sizes and is less likely to lead to false-positive findings. Baseline served as the reference time frame, and two indicator variables for after six days and after 13 days of light treatment were created to examine the change in outcome measures at six days and 13 days relative to baseline measures. As only one veteran dropped out of the study after the start of light treatment, no additional missing data methods were performed. As this proof of concept study was focused primarily on acceptability and feasibility of treatment, and secondarily on treatment efficacy, all two-tailed statistical tests were based on a type I error rate of 5%. In addition, simple baseline to post-treatment change scores were computed for all measures. Correlations were generated among the participant treatment expectation measure and the baseline to post-treatment change scores.
Results
Acceptability and Feasibility
One veteran dropped out at the midtreatment assessment point in order to go on a vacation, and thereby only received six days of light treatment. The remaining 24 veterans completed the full 13 days of light treatment. The average expectation rating was 4.0 ± 1.9, suggesting that the veterans endorsed the possibility that the morning bright light treatment could reduce their pain. Light readings from the photosensors on the light boxes were checked against the light readings on each subject’s wrist monitor during the light treatment to gauge when subjects received the light treatment. Results indicated that on average subjects received bright light during 87.8% of the scheduled light treatment times (range = 18.5–99.4%). Likely due to ≥80% adherence in all participants but two, no significant associations were found between adherence and outcome measures. No participant reported any side effects or adverse events associated with the light treatment. The average treatment satisfaction rating was 8.0 ± 2.2, suggesting that, on average, the veterans were well satisfied with the treatment.
Pain Sensitivity from Laboratory Pain Tasks
No pain sensitivity data were lost. The light treatment did not lead to any significant changes in ischemia pain threshold or tolerance (Table 2). Thermal pain threshold significantly increased from baseline to after 13 days of light treatment, reflecting a decrease in pain sensitivity after the light treatment. Thermal tolerance, however, did not change significantly during light treatment.
Table 2.
Means and SDs of variables at baseline, after six days, and after 13 days of morning bright light treatment
| Variable | Baseline | 6 d | 13 d |
|---|---|---|---|
| Ischemic threshold, sec | 81.48 (119.80) | 67.56 (100.69) | 84.67 (129.23) |
| Ischemic tolerance, sec | 187.88 (160.13) | 217.04 (176.01) | 200.46 (162.40) |
| Thermal threshold, °C | 42.95 (3.68) | 43.27 (4.09) | 43.72 (3.11)* |
| Thermal tolerance, °C | 47.09 (1.64) | 47.16 (1.74) | 47.11 (1.97) |
| PROMIS Pain Intensity | 48.84 (6.30) | 49.59 (7.65) | 47.02 (7.77)* |
| PROMIS Pain Behavior | 56.67 (6.49) | 55.94 (6.92) | 54.63 (8.09)* |
| PROMIS Pain Interference | 56.39 (8.33) | 56.05 (8.33) | 55.37 (8.72) |
| PROMIS Physical Function | 44.21 (8.66) | 45.09 (8.58)* | 44.99 (8.68) |
| CES-D 10 | 6.60 (4.84) | 7.04 (5.40) | 6.13 (5.08) |
| STAI | 35.00 (11.58) | 36.20 (11.68) | 36.92 (11.42) |
| PCL-5 | 15.91 (20.11) | 14.95 (21.38) | 12.10 (18.04)* |
| PSQI | 7.72 (5.10) | 7.04 (3.17) | 5.96 (2.91)* |
| ISI | 8.56 (5.28) | 6.24 (5.43)* | 6.71 (4.81)* |
| Actigraphy sleep start, h:mm | 23:25 (1.80) | 23:09 (1.81) | 22:55 (1.75)* |
| Actigraphy sleep end, h:mm | 7:10 (1.63) | 6:20 (1.47)* | 6:27 (1.51)* |
| Actigraphy total sleep time, h | 402.47 (75.66) | 372.83 (82.45)* | 383.40 (67.46) |
| Actigraphy sleep efficiency, % | 87.02 (5.23) | 86.87 (5.72) | 85.46 (7.36) |
| DLMO, h:mm | 19:58 (1.57) | 19:29 (1.28)* | 19:11 (1.46)* |
Indicates mean significantly different from baseline at P < 0.05.
CES-D 10 = Center for Epidemiologic Studies Short Depression Scale; DLMO = dim light melatonin onset; ISI = Insomnia Severity Index; PCL-5 = PTSD Checklist for DSM-5; PSQI = Pittsburgh Sleep Quality Index; STAI = State Trait Anxiety Inventory.
Self-Reported Pain, Function, Mood, and Sleep
The online PROMIS assessment failed on two occasions, resulting in only a partial baseline assessment for one subject and a missing final assessment for another subject. Pain Intensity and Pain Behavior significantly decreased from baseline to post-treatment (Table 2). Pain Interference did not significantly decrease from baseline to post-treatment. Physical Function showed a trend toward improvement at post-treatment (P = 0.07). All subjects completed depressive and anxiety symptom questionnaires, but some subjects were unwilling to complete all the PTSD symptom questionnaires (two subjects at baseline, three subjects at midtreatment, and four subjects at post-treatment). There were no significant effects of light treatment on depressive or anxiety symptoms (Table 2). PTSD symptoms were significantly reduced from baseline to post-treatment. All subjects completed the self-report sleep questionnaires. Scores on both the Pittsburgh Sleep Quality Inventory and Insomnia Severity Index were reduced significantly during bright light treatment (Table 2).
Wrist Actigraphy
A wrist actiwatch failed for one subject during the last week of light treatment. There was evidence that the light treatment led to earlier sleep start and sleep end timing. However, total sleep time and sleep efficiency did not significantly change from baseline to post-treatment (Table 2).
Circadian Timing
The DLMOs for seven veterans were not valid due to low levels of melatonin (<5 pg/mL) or to at least one erratic melatonin profile. Two veterans did not dim their home lighting, which likely suppressed their melatonin levels, invalidating calculation of their DLMOs. In the final sample, there were 17 DLMOs at baseline, and 16 DLMOs at both midtreatment and post-treatment. The DLMO significantly phase-advanced (shifted earlier in clock time) from baseline (Table 2).
Correlations Among Change Scores
We generated correlation coefficients among participant treatment expectation ratings and baseline to post-treatment change scores for all outcome variables (Table 3). Given that the sample size was 25 participants for most measures and only 16 participants for the DLMO values, we did not expect many statistically significant correlations. Instead, we examined patterns of correlation coefficients to evaluate to what degree outcome changes were related to DLMO changes—a potential mechanism specific to bright light treatment—and to participant expectations of benefit from treatment—a potential mechanism not specific to bright light treatment. There were two correlation coefficients ≥0.30 for participant ratings of expected benefit and six correlation coefficients ≥0.30 for DLMO changes. Results suggest some evidence for the notion that baseline to post-treatment circadian timing changes may have accounted for outcome improvements, at least to a larger extent than participant expectations of benefitting from the morning bright light treatment.
Table 3.
Correlations among participant treatment expectations, DLMO changes, and outcome changes
| Baseline to Post-treatment Change Scores | Participant Expectations | DLMO Changes |
|---|---|---|
| Ischemic threshold, sec | 0.21 | –0.09 |
| Ischemic tolerance, sec | –0.17 | 0.21 |
| Thermal threshold, °C | –0.01 | –0.23 |
| Thermal tolerance, °C | 0.13 | 0.03 |
| PROMIS Pain Intensity | –0.24 | 0.33 |
| PROMIS Pain Behavior | –0.14 | 0.38 |
| PROMIS Pain Interference | 0.05 | 0.55* |
| PROMIS Physical Function | –0.31 | –0.20 |
| CES-D 10 | 0.23 | 0.28 |
| STAI | 0.17 | 0.35 |
| PCL-5 | –0.06 | –0.27 |
| PSQI | 0.27 | 0.06 |
| ISI | 0.27 | 0.46 |
| Actigraphy sleep start, h:mm | –0.06 | 0.11 |
| Actigraphy sleep end, h:mm | –0.35 | 0.42 |
| Actigraphy total sleep time, h | –0.24 | 0.24 |
| Actigraphy sleep efficiency, % | –0.15 | –0.02 |
Indicates correlation coefficient significant at P < 0.05.
CES-D 10 = Center for Epidemiologic Studies Short Depression Scale; DLMO = dim light melatonin onset; ISI = Insomnia Severity Index; PCL-5 = PTSD Checklist for DSM-5; PSQI = Pittsburgh Sleep Quality Index; STAI = State Trait Anxiety Inventory.
Discussion
US military veterans report a high prevalence of chronic pain [1,2]. Pharmacological approaches for the management of chronic pain are fraught with unwanted side effects, and, in the case of opioid-based analgesic medications, risk of serious misuse [3,4]. We proposed that morning bright light treatment could represent a low-cost, low–side effect, and practical alternative to analgesic medications. The purpose of this open trial was to examine the feasibility, acceptability, and effects of a home-based, self-administered morning bright light treatment on pain, mood, sleep, and circadian timing in a small sample of US military veterans with chronic low back pain. Our results suggest that morning bright light treatment was feasible and acceptable to veterans with chronic low back pain. Although there was significant subject dropout during the baseline phase, only one subject dropped out after initiating the light treatment. Importantly, the subject’s stated reason for dropout was not due to treatment side effects. Treatment expectation and satisfaction scores also suggest good acceptability of this form of treatment in this population. These findings are consistent with the published literature indicating that there are minimal side effects associated with bright light treatment [7,8] and low patient discontinuation rates [8].
We found that self-reports of pain intensity and pain behavior significantly reduced, whereas self-reported physical function significantly improved during the morning bright light treatment. Although the baseline to post-treatment effect sizes for all three factors were no greater than medium (Cohen’s d = 0.26), results suggest that subjects did indeed improve on pain and function in response to this treatment. Both sleep quality and insomnia symptoms showed significant improvement, with larger effect sizes (Cohen’s d = 0.37–0.44). Sleep quality improved, but the average score still reflected some sleep quality problems post-treatment (PSQI ≥ 6). Subjects did move from an average “subthreshold insomnia” score at baseline to “no clinical significant insomnia” at post-treatment on the ISI. However, although the objective sleep variables derived from the wrist actigraphy showed an advance in sleep timing (∼30–45 minutes), there was no significant post-treatment change in total sleep duration or sleep efficiency. Thus the subjective improvement in sleep quality was not observed in the objective sleep variables. These findings are consistent with the results of a meta-analysis reporting a larger effect size for subjective sleep reports but smaller effect sizes for objective sleep variables in response to morning bright light treatment [5].
Results for pain sensitivity changes were not consistent. On the one hand, we found that the morning bright light treatment significantly increased thermal pain threshold. On the other hand, ischemic pain threshold and ischemic pain tolerance did not significantly change. Of note, there is little consensus on the degree to which findings from laboratory-induced pain are relevant to the clinical experience of pain [41]. Results reveal a weak relationship between clinical and laboratory-induced pain, suggesting that these pain experiences represent distinct processes [42–45]. Still, reducing pain sensitivity as indexed by laboratory tasks would appear clinically important insofar as changes in pain sensitivity may reveal changes in central pain modulation.
Despite meta-analyses indicating that morning bright light treatment can significantly reduce depressive symptoms [6] and reports suggesting that light treatment may have some antianxiolytic effects [46,47], we did not observe any significant changes in depressive and anxiety symptoms. The lack of significant change may have been due to subjects in this sample reporting relatively low levels of depressive and anxiety symptoms on average (baseline CES-D 10 < 10 and baseline STAI = 35) (Table 2). However, PTSD symptoms significantly decreased during the light treatment, which is consistent with a recently completed study (clinical trial NCT00701064).
As expected from other studies of the effects of morning bright light [48], the dim light melatonin onset advanced, or shifted earlier, by approximately 50 minutes. This result suggests that the treatment altered circadian timing in a meaningful way. This result also offered the possibility that other treatment effects may have been at least partly wrought via changes in this physiological mechanism. The pattern of correlations among the baseline to post-treatment changes in outcomes and DLMO support this notion. That is, shifts to earlier circadian timing (phase advances) were related to improvements in pain intensity, pain behavior, pain interference, anxiety symptoms, and insomnia symptoms, with correlation coefficients of at least r = 0.30. Far from definitive given the small sample and study design, these findings at least support the notion that circadian timing changes may represent a treatment mechanism through which bright light treatment affects improvement in pain, mood, and function [18].
There were several limitations of the study. The sample size was small, due in part to limited funding and also due to difficulties in recruiting veterans from the community for an intensive 53-day protocol. The study also lacked a placebo control condition, as in this open trial all available resources were aimed at examining the acceptability, feasibility, and initial efficacy of the morning bright light treatment. Thus, some of the positive effects of morning bright light treatment observed here could be placebo effects in response to participating in a study holding the possibility of benefits. We evaluated this possibility by examining correlations between participant expectations of treatment benefit (recorded before treatment) and baseline to post-treatment outcome changes. Only two of 17 correlations were at least r = 0.30. These findings do not support the notion that placebo (via expectancy) effects were largely responsible for treatment gains. Further, we found significant effects on two separate assessment methods, subjective pain reports and one pain sensitivity metric, which is especially noteworthy considering our small sample size. We also observed that when present, the benefits of light treatment generally continued to increase from six days to 13 days of light treatment, which is consistent with the antidepressant time course of morning bright light treatment [6] and suggests that continuing the morning bright light treatment for more than two weeks could yield larger treatment effects.
Conclusions
Results from this open trial suggest that a home-based morning bright light treatment, one hour per day, starting at habitual wake time, is a feasible and acceptable treatment protocol for US military veterans with chronic low back pain. As a proof of concept study, our results also support the efficacy of morning bright light treatment for improving pain, function, mood, and subjective sleep. Finally, preliminary findings suggest that circadian timing changes could represent an active mechanism of morning bright light treatment for pain and function. Thus, in conclusion, more research studies, with larger sample sizes and a placebo control condition, should further explore morning bright light as a potentially effective innovative treatment for chronic pain populations.
Acknowledgments
We thank Morgan Corich, Joshua Dein, Aahad Kahn, Catherine Keefner, Mary Kennedy, Fumitaka Kikyo, Athanasios Kondilis, Othon Nunez-Montelongo, Daria Orlowska, Philip Sanchez, Monica Thomas, Marie Vallido, and Amanda Vatinno for their assistance with data collection. We thank Mark Aloia, PhD, at Philips, Inc., who donated the light boxes for this pilot study.
Funding sources: Research reported in this publication was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under award number R34AT008347.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure and conflicts of interest: Dr. Burgess is a consultant for Natrol, LLC. All other authors report no conflicts of interest.
References
- 1. Lew HL, Otis JD, Tun C, et al. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: Polytrauma clinical triad. J Rehabil Res Dev 2009;46(6):697–702. [DOI] [PubMed] [Google Scholar]
- 2. Kerns RD, Otis J, Rosenberg R, Reid MC.. Veterans’ reports of pain and associations with ratings of health, health-risk behaviors, affective distress, and use of the healthcare system. J Rehabil Res Dev 2003;40(5):371–9. [DOI] [PubMed] [Google Scholar]
- 3. Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev 2010;(1):CD006605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011;305(13):1315–21. [DOI] [PubMed] [Google Scholar]
- 5. van Maanen A, Meijer AM, Van der Heijden KB, Oort FJ.. The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Med Rev 2016;29:52–62. [DOI] [PubMed] [Google Scholar]
- 6. Al-Karawi D, Jubair L.. Bright light therapy for nonseasonal depression: Meta-analysis of clinical trials. J Affect Disord 2016;198:64–71. [DOI] [PubMed] [Google Scholar]
- 7. Pail G, Huf W, Pjrek E, et al. Bright-light therapy in the treatment of mood disorders. Neuropsychobiology 2011;64(3):152–62. [DOI] [PubMed] [Google Scholar]
- 8. Terman M, Terman JS.. Light therapy for seasonal and nonseasonal depression: Efficacy, protocol, safety, and side effects. CNS Spectrums 2005;10(08):647–63. [DOI] [PubMed] [Google Scholar]
- 9. Gallin PF, Terman M, Reme CE, et al. Ophthalmologic examination of patients with seasonal affective disorder, before and after bright light therapy. Am J Ophthalmol 1995;119(2):202–10. [DOI] [PubMed] [Google Scholar]
- 10. St Hilaire MA, Gooley JJ, Khalsa SB, et al. Human phase response curve to a 1h pulse of bright white light. J Physiol 2012;590(Pt 13):3035–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Castillo RC, MacKenzie EJ, Wegener ST, Bosse MJ.. Prevalence of chronic pain seven years following limb threatening lower extremity trauma. Pain 2006;124(3):321–9. [DOI] [PubMed] [Google Scholar]
- 12. Beck JG, Clapp JD.. A different kind of co-morbidity: Understanding posttraumatic stress disorder and chronic pain. Psychol Trauma 2011;3(2):101–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kaaria S, Laaksonen M, Rahkonen O, Lahelma E, Leino-Arjas P.. Risk factors of chronic neck pain: A prospective study among middle-aged employees. Eur J Pain 2012;16(6):911–20. [DOI] [PubMed] [Google Scholar]
- 14. Smith MT, Klick B, Kozachik S, et al. Sleep onset insomnia symptoms during hospitalization for major burn injury predict chronic pain. Pain 2008;138(3):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gupta A, Silman AJ, Ray D, et al. The role of psychosocial factors in predicting the onset of chronic widespread pain: Results from a prospective population-based study. Rheumatology (Oxford) 2006;46(4):666–71. [DOI] [PubMed] [Google Scholar]
- 16. Roehrs TA, Harris E, Randall S, Roth T.. Pain sensitivity and recovery from mild chronic sleep loss. Sleep 2012;35(12):1667–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vitiello MV, Rybarczyk B, Von Korff M, Stepanski EJ.. Cognitive behavioral therapy for insomnia improves sleep and decreases pain in older adults with co-morbid insomnia and osteoarthritis. J Clin Sleep Med 2009;5(4):355–62. [PMC free article] [PubMed] [Google Scholar]
- 18. Burgess HJ, Park M, Ong JC, et al. Morning versus evening bright light treatment at home to improve function and pain sensitivity for women with fibromyalgia: A pilot study. Pain Med 2017;18(1):116–23. [DOI] [PubMed] [Google Scholar]
- 19. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP.. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999;131(7):485–91. [DOI] [PubMed] [Google Scholar]
- 20. Hening WA, Allen RP.. Restless legs syndrome (RLS): The continuing development of diagnostic standards and severity measures. Sleep Med 2003;4(2):95–7. [DOI] [PubMed] [Google Scholar]
- 21. Terman M, Williams J.. Personal Inventory for Depression and SAD (PIDS). J Prac Psychiatry Behav Health 1998;5:301–3. [Google Scholar]
- 22. Murphy PJ, Myers BL, Badia P.. Nonsteroidal anti-inflammatory drugs alter body temperature and suppress melatonin in humans. Physiol Behav 1996;59(1):133–9. [DOI] [PubMed] [Google Scholar]
- 23. Cowen PJ, Bevan JS, Gosden B, Elliott SA.. Treatment with B-adrenoceptor blockers reduces plasma melatonin concentration. Br J Clin Pharmacol 1985;19(2):258–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Patel SR, Weng J, Rueschman M, et al. Reproducibility of a standardized actigraphy scoring algorithm for sleep in a US Hispanic/Latino population. Sleep 2015;38(9):1497–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Eaton W, Muntaner C, Smith C, Tien A, Ybarra M.. Center for Epidemiologic Studies Depression scale: Review and revision (CESD and CESD-R) In: Maruish ME, ed. The Use of Psychological Testing for Treatment Planning and Outcomes Assesment. 3rd ed.Mahwah, NJ: Lawrence Erlbaum; 2004:363–77. [Google Scholar]
- 26. Spielberger CD, Gorsuch RL, Lushene RE.. The State-Trait Anxiety Inventory Manual. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- 27. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD. 2013. Available at: www.ptsd.va.gov. (accessed August 27, 2018).
- 28. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ.. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 29. Bastien CH, Vallieres A, Morin CM.. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2(4):297–307. [DOI] [PubMed] [Google Scholar]
- 30. Maurset A, Skoglund LA, Hustveit O, Klepstad P, Oye I.. A new version of the ischemic tourniquet pain test. Methods Find Exp Clin Pharmacol 1991;13(9):643–7. [PubMed] [Google Scholar]
- 31. Bruehl S, Burns JW, Gupta R, et al. Endogenous opioid function mediates the association between laboratory evoked pain sensitivity and morphine analgesic responses. Pain 2013;154(9):1856–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bruehl S, Dengler-Crish CM, Smith CA, Walker LS.. Hypoalgesia related to elevated resting blood pressure is absent in adolescents and young adults with a history of functional abdominal pain. Pain 2010;149(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fillingim RB, Ness TJ, Glover TL, et al. Morphine responses and experimental pain: Sex differences in side effects and cardiovascular responses but not analgesia. J Pain 2005;6(2):116–24. [DOI] [PubMed] [Google Scholar]
- 34. Burgess HJ, Wyatt JK, Park M, Fogg LF.. Home circadian phase assessments with measures of compliance yield accurate dim light melatonin onsets. Sleep 2015;38(6):889–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Burgess HJ, Park M, Wyatt JK, Fogg LF.. Home dim light melatonin onsets with measures of compliance in delayed sleep phase disorder. J Sleep Res 2016;25(3):314–7. [DOI] [PubMed] [Google Scholar]
- 36. Lewy AJ, Sack RL.. The dim light melatonin onset as a marker for circadian phase position. Chronobiol Int 1989;6(1):93–102. [DOI] [PubMed] [Google Scholar]
- 37. Klerman EB, Gershengorn HB, Duffy JF, Kronauer RE.. Comparisons of the variability of three markers of the human circadian pacemaker. J Biol Rhythms 2002;17(2):181–93. [DOI] [PubMed] [Google Scholar]
- 38. Voultsios A, Kennaway DJ, Dawson D.. Salivary melatonin as a circadian phase marker: Validation and comparison to plasma melatonin. J Biol Rhythms 1997;12(5):457–66. [DOI] [PubMed] [Google Scholar]
- 39. Molina TA, Burgess HJ.. Calculating the dim light melatonin onset: The impact of threshold and sampling rate. Chronobiol Int 2011;28(8):714–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Eastman CI, Young MA, Fogg LF, Liu L, Meaden PM.. Bright light treatment of winter depression: A placebo-controlled trial. Arch Gen Psychiatry 1998;55(10):883–9. [DOI] [PubMed] [Google Scholar]
- 41. Gracely RH. Pain measurement. Acta Anaesthesiol Scand 1999;43(9):897–908. [DOI] [PubMed] [Google Scholar]
- 42. Edwards RR, Haythornthwaite JA, Sullivan MJ, Fillingim RB.. Catastrophizing as a mediator of sex differences in pain: Differential effects for daily pain versus laboratory-induced pain. Pain 2004;111(3):335–41. [DOI] [PubMed] [Google Scholar]
- 43. Lautenschlager J, Seglias J, Bruckle W, Muller W.. Comparisons of spontaneous pain and tenderness in patients with primary fibromyalgia. Clin Rheumatol 1991;10(2):168–73. [DOI] [PubMed] [Google Scholar]
- 44. Lautenbacher S, Rollman GB, McCain GA.. Multi-method assessment of experimental and clinical pain in patients with fibromyalgia. Pain 1994;59(1):45–53. [DOI] [PubMed] [Google Scholar]
- 45. Scudds RA, McCain GA, Rollman GB, Harth M.. Improvements in pain responsiveness in patients with fibrositis after successful treatment with amitriptyline. J Rheumatol Suppl 1989;19:98–103. [PubMed] [Google Scholar]
- 46. Youngstedt SD, Kripke DF.. Does bright light have an anxiolytic effect?—an open trial. BMC Psychiatry 2007;7:62.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Baxendale S, O'Sullivan J, Heaney D.. Bright light therapy for symptoms of anxiety and depression in focal epilepsy: Randomised controlled trial. Br J Psychiatry 2013;202(05):352–6. [DOI] [PubMed] [Google Scholar]
- 48. Burgess HJ, Fogg LF, Young MA, Eastman CI.. Bright light therapy for winter depression - is phase advancing beneficial? Chronobiol Int 2004;21(4–5):759–75. [DOI] [PubMed] [Google Scholar]