Abstract
Background:
Self-assessment of asthma and a stronger doctor-patient relationship can improve asthma outcomes. Evidence for the influence of patient enablement on quality of life and the control of asthma is lacking.
Aims:
To assess asthma severity, medication use, asthma control, and patient enablement in patients with asthma treated in primary care and to study the relationship between these variables and quality of life.
Methods:
A cross-sectional study was conducted in an urban clinic in northern Portugal. Data were collected from both clinical records and questionnaires from a random sample of asthma patients. The modified Patient Enablement Instrument, the Asthma Quality of Life Questionnaire, and the Asthma Control Questionnaire were used. Peak expiratory flow and forced expiratory volume in one second (FEV1) were measured. Receiver operating characteristic curve analysis was performed to establish cut-off values for the quality of life measurements. The associations between enablement, asthma control, and quality of life were tested using logistic regression models.
Results:
The study sample included 180 patients. There was a strong correlation between asthma control and quality of life (r=0.81, p<0.001). A weak association between patient enablement and asthma control and quality of life was found in the logistic regression models. Poor control of asthma was associated with female gender, concomitant co-morbidities, reduced FEV1, and increased severity of asthma.
Conclusions:
The weak correlation between enablement and asthma control requires further study to determine if improved enablement can improve asthma outcomes independent of gender, severity, and concomitant co-morbidities. This study confirms the strong correlation between asthma control and quality of life.
Keywords: asthma, management, primary care, observational study
Introduction
Patient empowerment can influence asthma1–3 and other chronic diseases,4,5 affecting disease control. The Global Initiative for Asthma (GINA) suggests that empowering patients can improve outcomes.6 The Portuguese National Asthma Control Program,7 based on the GINA update of 2007,8 also recommends promotion of self-control.
Patient-centred care may lower morbidity, mortality, and costs. This is reflected in the St Vincent Declaration for diabetes mellitus in 1989,9 the GINA program for asthma in 1993,10 and the GOLD project for chronic obstructive pulmonary disease (COPD) in 1997.11
This requires tools to study patient-centred outcomes including the Asthma Control Questionnaire (ACQ),12–14 the Asthma Control Test (ACT),15,16 and the mini Asthma Quality of Life Questionnaire (mini-AQLQ).17–19 The Patient Enablement Instrument (PEI)20 assesses enablement in disease control and physician performance. The modified Patient Enablement Instrument (mPEI) can assess patients with asthma.21
While stronger doctor-patient relationships may improve adherence and outcomes,6 it is necessary to identify the factors that influence enablement and quality of life in patients with asthma to test this hypothesis.
The objectives of the current study were to assess asthma severity and control, medication use, patient enablement, and quality of life in patients with asthma and to study the determinants of quality of life in asthma.
Methods
Study population
This study was conducted in Matosinhos, Portugal, a city with 169,261 inhabitants in 2008. The age/gender distribution of this population and of the Horizonte Health Unit is similar to the age/gender distribution of the total Portuguese population.22
Practice setting
The study practice was formed in 2001 by eight family physicians. It has a stable population with good access to healthcare and continuity of electronic medical records. The clinic is a teaching practice for medical students and family medicine residency training.
Sampling procedures
A random sample of 180 patients with asthma aged ≥18 years treated by seven doctors was selected from the practice database of 450 asthma patients. This was based on the sample size calculation of Peduzzi et al.23 which suggested 10–20 cases for each predictor variable in a linear regression analysis and up to 30 cases per variable for logistic regression models. Six predictors of the asthma outcomes were selected, giving a required sample size of 180 patients.
The diagnosis of asthma was made by the family physicians using the GINA definition,6 as described previously.24 Patients invited to participate were confirmed as having asthma by a doctor's diagnosis or because they were receiving asthma medication. Patients incorrectly selected with other conditions such as COPD were excluded and replaced by the next subject in the sample.
Patients with kyphoscoliosis, absence of one lung, lung cancer, cognitive impairment, pregnant or bedridden patients, or anyone unable to complete the questionnaire were excluded. Five attempts were made to contact selected patients. Patients impossible to reach or unwilling to visit the practice were replaced by patients of the same age and gender from the list.
Questionnaires and tools
Demographic and clinical data were collected in a specially designed questionnaire. Standardised instruments (mini-ACT, modified PEI, and mini-AQLQ) were also used. The study questionnaire was pilot tested in 20 patients between January and March, 2010.
The demographic data collected included the Graffar Social Classification,25 validated for use in Portuguese. The clinical data collected was based on the GINA classification of severity and treatment of asthma.
The mini-AQLQ contains 15 items. The score is the sum of the scores for each item, divided by 15 (the number of items), expressed as a score out of 7. A change in score of >0.5 can be considered clinically important.18,26
The mPEI evaluates enablement, and a score of >6 indicates clinically meaningful enablement. The original version of the PEI was developed and used to assess the enablement of patients after a consultation for an acute or chronic condition. The authors differentiated between satisfaction — which occurs when expectations are met — and enablement — which occurs when benefit has been achieved. The mPEI changed the introductory statement of the original PEI to read: “As a result of the treatment you have been on for your asthma, do you feel you are …” rather than “As a result of your visit to the doctor today …”. The six items assess the patient's ability to deal with life, understand the illness, cope with it, keep healthy, remain confident about health, and help oneself. The original English version was translated into Portuguese and translated back to English. The back translation matched the original version. The questionnaire was pilot tested in 30 patients and was found to be satisfactory.
Asthma control, measured by the ACT, was classified into three categories (controlled, partially controlled, and uncontrolled with cut-off values of 25, 20–24 and ≤19, respectively) or two categories (good control and poor control with cut-off values of 20–25 and ≤19, respectively) for the analysis.
Data collection
The study was conducted between February and November 2010 at the Horizonte Family Health Unit using medical records and a questionnaire. Participants were contacted by telephone or in person and invited for an interview.
Demographic data included gender, age, and social status. Asthma severity was assessed using the 2008 GINA criteria. Relief and control medications were coded using the GINA glossary. Co-morbidities were counted. Asthma control was assessed as full, partial, or uncontrolled using the mini-ACT. Quality of life was measured with the mini-AQLQ. Quantitative assessment of asthma control was made by measuring peak expiratory flow (PEF) and forced expiratory volume in one second (FEV1) using the PiKo-1 spirometer, validated for use in Portugal.27,28 The best of three measurements made under standardised conditions was used.
Statistical analysis
Data were entered and coded with Microsoft Excel and analysed with EpiInfo Version 3.4 and PASW Statistics for Windows Version 18.0. The Student t test and the non-parametric Mann-Whitney test were used for comparisons between two groups. Several groups were compared using analysis of variance or the non-parametric Kruskal-Wallis test. Categorical data were analysed by the χ2 test. Pearson and Spearman rank correlation coefficients were used to study the associations between several variables under study. Receiver operating characteristic (ROC) curve analysis was used to define a cut-off on quality of life as a classification of good and poor asthma control. Logistic regression models were used to study the relation between several independent variables and the dependent variables quality of life and asthma control. Statistical significance was set at p<0.05.
Ethical approval
Approval by the Ethics Committee of the Local Health Authority in Matosinhos (Unidade Local de Saude de Matosinhos) was obtained before data collection. Signed informed consent was obtained from patients after the aims and methods of the study were explained. All patients with uncontrolled asthma were referred back to their family physician for treatment.
Results
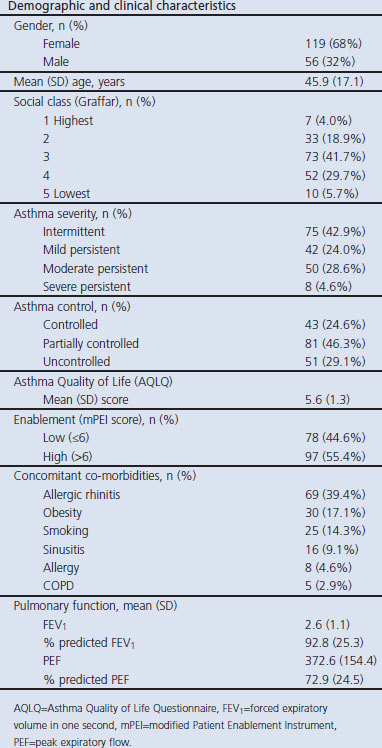
Data were obtained from 175 of the 180 patients selected (response rate 97.2%). Age, gender, social class, and clinical characteristics including severity of asthma, use of medications, co-morbidities, pulmonary function, asthma control (ACT), patient enablement (mPEI), and quality of life (AQLQ) measures are shown in Table 1.
Table 1. Demographic and clinical characteristics of asthma patients (n=175).
Medications
Short-acting β2-agonists were used as relief medication in 49.7% of patients; no relief medication was required by 37% of patients. The most common controller medication was a combination of an inhaled corticosteroid and a long-acting β2-agonist, used by 24% of patients. Inhaled steroids alone were used by 14.9% of patients and no controller medication was used by 49% of patients.
Analysis of outcome variables
Asthma severity, asthma control (ACT), quality of life (mini-AQLQ), and enablement (mPEI) were analysed in relation to gender, age, socioeconomic status, co-morbidities, medication, and pulmonary function (PEF and FEV1). The results are presented in Table 2.
Table 2. Analysis of outcome variables.
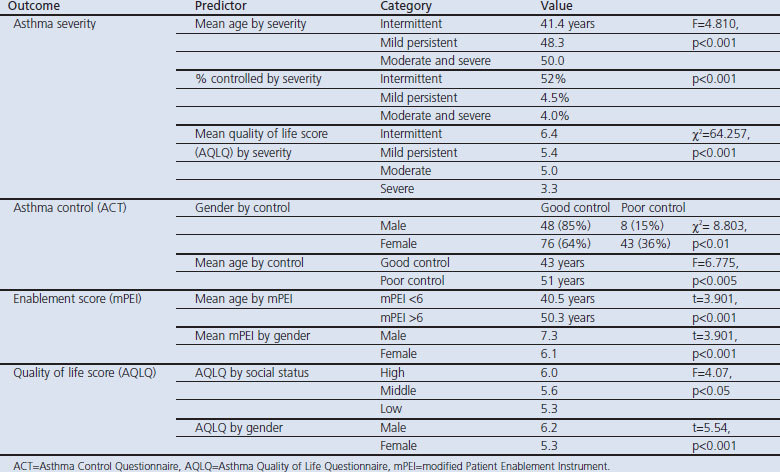
Asthma severity
Asthma severity was dependent on age (ANOVA, F=4.810, p<0.001) and a significantly lower level of asthma control (p<0.001). Quality of life (mini-AQLQ score) varied inversely with severity (Kruskal-Wallis test, χ2 =64.257, p<0.001). However, severity of asthma was found to be independent of gender, social status, and co-morbidities.
Asthma control
Better asthma control was related to male gender (χ2=8.803, p<0.01), younger age (ANOVA, F=6.775, p<0.005), fewer co-morbidities (χ2=12.06, p<0.05), less use of controlling medication (χ2=48.64, p<0.05) and relief medication (χ2=22.43, p<0.001), and pulmonary function.
Quality of life
The analysis of variance revealed a significant association between quality of life (mini-AQLQ) and social status (ANOVA, F=4.07, p<0.05) and gender (t=5.54, p<0.001). The correlation between quality of life (mini-AQLQ) and age, co-morbidities, and pulmonary function was low.
Patient enablement
Patient enablement was measured with the PEI and had a mean (SD) score of 6.5 (3.6) and a median of 6 (range 0–12). The most common values obtained were scores of 0 (13.1%), 6 (28.0%) and 12 (13.7%), but all possible scores between 0 and 12 were obtained with 45.2% of the values obtained outside the most common values.
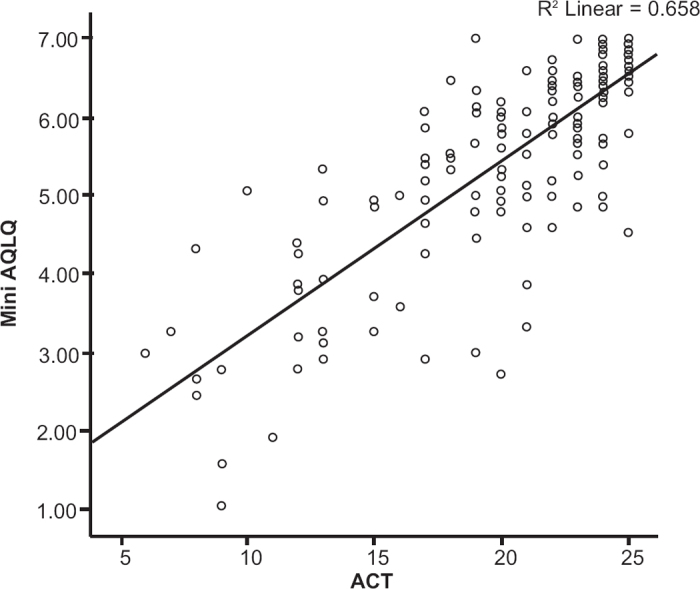
No significant association was found between the mPEI score and the mini-AQLQ score, the ACT score, the level of %FEV1, %PEF, asthma severity, or social status. The correlation between enablement (mPEI) and age was low, but the mean ages of patients with low (≤6) and high (>6) levels of enablement were significantly different (t=3.901, p<0.001). There was a significant association between the mean mPEI score and gender (t=3.901, p<0.001). Analysis of relationships between outcome variables There was a strong correlation between ACT scores and the mini-AQLQ (r=0.81, p<0.001). The scatter plot is shown in Figure 1. However, correlations between mPEI and ACT and mPEI and mini-AQLQ were weak.
Figure 1. Relationship between asthma control test (ACT) scores and quality of life questionnaire (mini- AQLQ) scores (n=175).
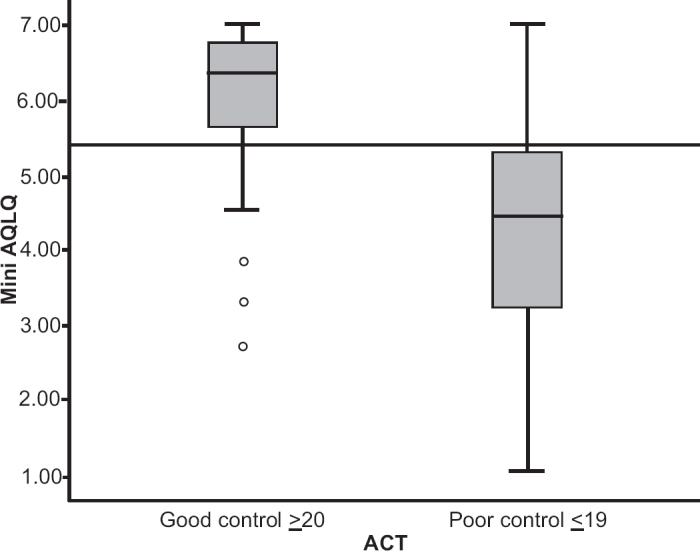
ROC curve analysis was performed to establish cut-off values for the quality of life measurements. Patients were classified as controlled or uncontrolled according to ACT. Using this classification, the distribution of mini-AQLQ scores for the two groups was studied. Assuming that better control is related to better quality of life, ROC analysis29 provides the mini-AQLQ cut-off that minimises the misclassification of patients as controlled or uncontrolled as a function of good and poor quality of life (mini-AQLQ). Figure 2 shows the area under the curve (AUC) of 0.878 (95% CI 0.821 to 0.935). The cut-off value (5.4) was fixed for a specificity and sensitivity of 80% (Figure 3).
Figure 2. Receiver operating characteristics (ROC) curve of asthma quality of life (mini-AQLQ) versus asthma control (ACT).
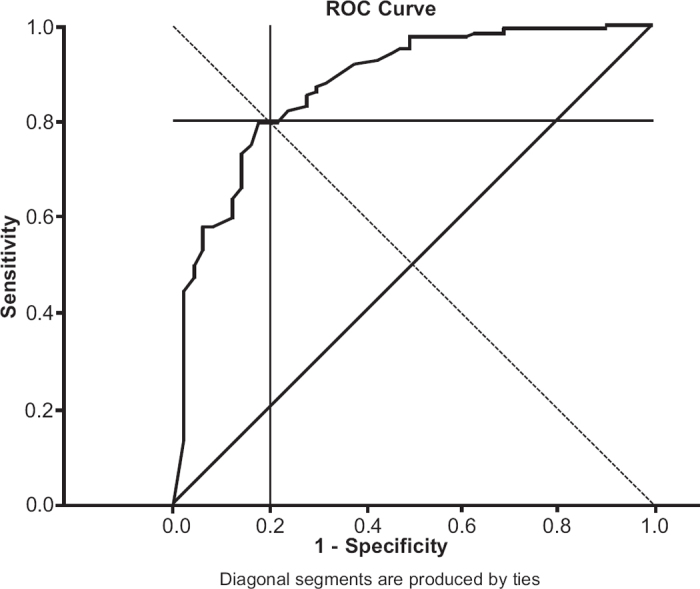
Figure 3. Distribution of asthma quality of life scores (mini-AQLQ) by asthma control scores (ACT) suggesting a quality of life (AQLQ) cut-off score of 5.4 for differentiating between good and poor control.
Logistic regression model
Logistic regression models were constructed to assess the association between demographic and other predictor variables and asthma control (ACT) and quality of life (mini-AQLQ) using a backward conditional method. The choice of variables in the model was based on the bivariate analysis. Asthma control (ACT) and quality of life (mini-AQLQ) were dichotomised for ACT scores <20 and for mini-AQLQ scores <5.40.
The model coefficients for ACT are presented in Table 3. Gender, economic status, concomitant co-morbidities, control medication, severity, enablement (mPEI), %PEF, %FEV1, age, and relief medication were entered into the model.
Table 3. Logistic regression model for poor asthma control (ACT).
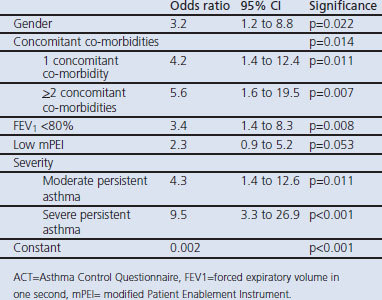
Model fit was assessed by the likelihood ratio statistic (χ2=61.220, df=7, p<0.001) and by the Hosmer and Lemeshow test (χ2=6.047, df=8, p=0.642). The logistic coefficients for all the variables were positive, indicating an increase in the log odds of poor asthma control. These values can be interpreted in terms of the odds ratio (OR), assuming that all other variables are held constant.
The following variables were associated with poor control: female gender (OR=3.2), moderate and severe persistent asthma (OR=4.2 and OR=9.5, respectively), FEV1 <80% of predicted (OR=3.4), and a higher number of concomitant co-morbidities (OR=4.2). Lower patient enablement (mPEI) appears to be associated with poor control, but this finding was not statistically significant (p=0.053).
The model coefficients for mini-AQLQ are presented in Table 4. Gender, economic status, severity and enablement (mPEI) were entered into the model. Model fit was assessed by the likelihood ratio statistic (χ2=49.917, df=5, p<0.001) and by the Hosmer and Lemeshow test (χ2=3.980, df=8, p=0.859).
Table 4. Logistic regression model for poor quality of life (mini-AQLQ).
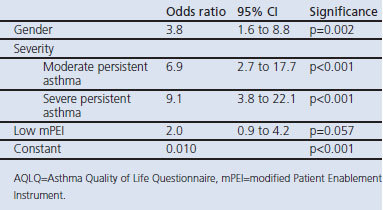
The logistic coefficients for all the variables are positive, indicating an increase in the log odds of poor asthma control. The following variables were associated with a worse quality of life: female gender (OR=3.8) and moderate and severe persistent asthma (OR=6.9 and OR=9.1, respectively). Low enablement (mPEI) appears to be associated with a poor quality of life, but this finding was not statistically significant (p=0.057).
Discussion
Main findings
This study found a strong association between asthma control and quality of life in a random sample of asthma patients treated in general practice. A weak positive correlation was found between patient enablement and asthma control.
Strengths and limitations of this study
The study had a high response rate (97.2%). Non-responders were not significantly different from responders in age or gender, so a response bias is unlikely. The analysis of the reasons for not participating did not show a bias. The study instruments chosen are widely accepted and have been validated for local use.
The assessment of severity of asthma was based on the 2008 update of the GINA report, which has a number of limitations. According to the GINA guidelines, before treatment is initiated the classification of asthma severity is based solely on clinical features. When patients are already receiving medication, the classification of severity should be based on the clinical features present and the daily medication regimen. Although it is still controversial whether any classification system can be used to classify asthma severity reliably in patients receiving drug treatment,30,31 using this approach it was possible to estimate the level of severity of the patients in the survey by matching the medication in use with the level of severity. Severity was classified in this way in the present study. The fact that some patients might need to step-up or step-down treatment and are therefore classified at a higher or lower level might be a source of bias on the severity classification in the results.
Interpretation of findings in relation to previously published work
Asthma control and quality of life
The association between asthma control and quality of life has been described in other studies.32,33 The ACT and the mini-AQLQ have been used to study the relationship between asthma-specific quality of life and asthma control. Asthma control tools reflect the symptom and activity limitation aspects of quality of life. They correlate well with emotional aspects but significantly less well than symptom or activity measures.34 Asthma control measured by the ACQ was negatively correlated with quality of life in one study.35 Co-morbidity has also been found to be associated with poor quality of life in asthma in a Dutch study.36
Enablement, asthma control, and quality of life
Evidence for the value of assessment of patient enablement in asthma is lacking, although the use of peak flow meters, symptom diaries, and written action plans may improve outcomes.2,3,37 The association between patient enablement and asthma control has been tested in some studies.36 Patients may value self-management,38 but this is not always the case as inhaler technique may be faulty despite training.39
Self-management education programmes may result in only small to moderate effects for selected chronic diseases,4 but may improve asthma control in patients compared with usual care.40 They can improve trust in treatment, improving adherence to therapeutic plans.41 Other studies found that a lower sense of self-efficacy may also be associated with worse asthma control and lower quality of life.42
Although we found a low correlation between the mPEI and the mini-AQLQ, there is some evidence that the mPEI may be sensitive enough to detect changes in the patient's quality of life, as shown by Haughney et al. in 2007.21 In that study, the authors also described a low correlation between the mPEI and the mini-AQLQ but found a significant correlation between the mPEI total score and changes in the mini-AQLQ. The original PEI was more a measurement of satisfaction with the consultation than a measure of enablement, while the mPEI aims to measure enablement as a result of asthma management. There are several possible reasons why measures of enablement may give negative results. Patients with less severe forms of asthma, who consult less frequently, might be less able to deal with the condition, as could less-educated, older, or underprivileged patients. We studied the relationship between enablement and socio-demographic and cultural variables and found no statistically significant differences that could explain the negative results. Another explanation could be that the patients in our study belong to a cohort that has often participated in research on asthma, resulting in a higher level of enablement (a PEI score of >6 was found in 97 patients, 55.4%) so that differences could not be detected.
Implications for future research, policy and practice
Patient enablement may be considered as an additional tool for improving asthma management. Improvements in patient enablement may result in better asthma control and quality of life. The mPEI may be useful in future research and be applicable in clinical work.
Conclusions
There was a strong correlation between asthma control and quality of life. A cut-off value for the quality of life measurement score using the mini-AQLQ was established at 5.4. This analysis suggests that a mini-AQLQ score of <5.4 is related to worse asthma control and a lower quality of life and a score of ≥5.4 is related to better control and a higher quality of life.
Gender, concomitant co-morbidities, FEV1, and severity are associated with asthma control. Gender and severity are also associated with quality of life.
The mean mPEI was 6.5, indicating clinically meaningful enablement. Patient enablement was found to be weakly associated with asthma control and quality of life in this population of asthma patients treated in primary care.
Acknowledgments
Handling editor Björn Ställberg
Statistical review Gopal Netuveli
The authors would like to express their gratitude to those who contributed to this study. They thank the family physicians and family medicine registrars (trainees) from Horizonte Family Health Unit who helped in contacting their patients to invite them for the interviews and to our patients who consented to participate in this study. Thanks are due to John Haughney for allowing us to translate and use the modified PEI, to Elisabeth Juniper for consenting to the use of the mini-AQLQ, and to Manuel Montenegro who carefully reviewed the references.
Funding The study required no external funding as it was practice-based research conducted within the National Health Service.
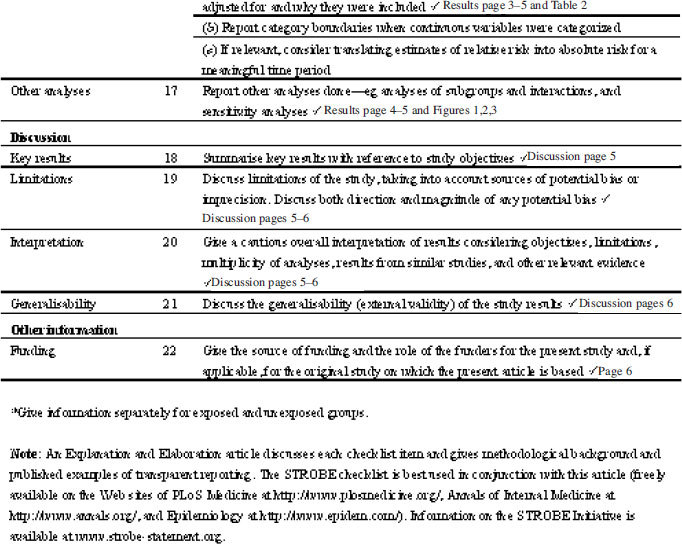
Appendix. STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies
Footnotes
No conflicts of interests are reported for this study. JCS was an unpaid member of the scientific board of AstraZeneca (AZ) Foundation Portugal from June 2009 until August 2011. His department has received research funding from AZ in 2008. He has received sponsorships from or delivered consultancy services to AZ, Nycomed, GSK, MSD, and Novartis. He is a member of the editorial Board of PCRJ.
References
- Fonseca JA, Costa-Pereira A, Delgado L, Fernandes L, Castel-Branco MG. Asthma patients are willing to use mobile and web technologies to support self-management. Allergy 2006;61(3):389–90. http://dx.doi.org/10.1111/j.1398-9995.2006.01016.x [DOI] [PubMed] [Google Scholar]
- Horne R, Price D, Cleland J, et al. Can asthma control be improved by understanding the patient's perspective? BMC Pulm Med 2007;7:8. http://dx.doi.org/10.1186/1471-2466-7-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partridge M, Barnes G, Price D, Barnes J. Guided self management plans for asthma: advice should be simple and patient focused. BMJ 2001;322(7294):1121–2; author reply 1123. http://dx.doi.org/10.1136/bmj.322.7294.1121 [PMC free article] [PubMed] [Google Scholar]
- Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review. Arch Intern Med 2004;164(15):1641–9. http://dx.doi.org/10.1001/archinte.164.15.1641 [DOI] [PubMed] [Google Scholar]
- Jordan JE, Osborne RH. Chronic disease self-management education programmes: challenges ahead. World Hosp Health Serv 2007;43(3):32–6. [PubMed] [Google Scholar]
- Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. NHLBI/WHO Workshop Report. Bethesda, MD: National Institutes of Health, National Heart, Lung and Blood Institute, January 1995. (updated 2010). Available from: http://www.ginasthma.org/pdf/GINA_Report_2010.pdf (cited 23 Jun 2011). [Google Scholar]
- Direcção-Geral da Saúde. Nacional de Controlo da Asma [National Program for Control of Asthma]. Lisboa: Direcção-Geral da Saude, 2000. [Google Scholar]
- Comissao de Coordenação do Programa Nacional de Controlo da Asma. Manual de Boas Práticas na Asma [Asthma Guidelines Manual]. Lisboa: Direcção-Geral da Saude, 2007. [Google Scholar]
- World Health Organization. Saint Vincent Declaration Action Programme. Copenhagen: World Health Organization, 1992. [Google Scholar]
- National Heart, Lung and Blood Institute and World Health Organization. Global Strategy for Asthma Management and Prevention. NHLBI/WHO Workshop Report, Bethesday, MD: National Heart, Lung and Blood Institute, 1995. [Google Scholar]
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease. NHLBI/ WHO Workshop Report. NIH Publication No. 2701. Bethesda, MD: National Heart, Lung and Blood Institute, 2001. [Google Scholar]
- Juniper EF, O'Byrne PM, Gyuatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire of asthma control. Eur Respir J 1999;14(4):902–07. http://dx.doi.org/10.1034/j.1399-3003.1999.14d29.x [DOI] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Ferrie PJ, Griffith LE. Measuring quality of life in asthma. Am Rev Respir Dis 1993;147(4):832–8. [DOI] [PubMed] [Google Scholar]
- Juniper EF, O'Byrne PM, Ferrie PJ, King DR, Roberts JN. Measuring asthma control: clinic questionnaire or daily diary? Am J Respir Crit Care Med 2000;162(4 Pt 11):1330–4. [DOI] [PubMed] [Google Scholar]
- Schatz M, Sorkness CA, Li JT, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol 2006;117(3):549–56. http://dx.doi.org/10.1016/j.jaci.2006.01.011 [DOI] [PubMed] [Google Scholar]
- Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004;113(1):59–65. http://dx.doi.org/10.1016/j.jaci.2003.09.008 [DOI] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health-related quality of life in asthma: development of a questionnaire for use in clinical trial. Thorax 1992;47(2):76–83. http://dx.doi.org/10.1136/thx.47.2.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira PL, Mendonça C, Newparth N, Mata P, Juniper EF, Mear I. Quality of life in asthma: cultural adaptation of Juniper's AQLQ to Portuguese. Qual Life Res 1998;7(7):590. [Google Scholar]
- Lobo FA. Qualidade de vida dos doentes com asma [Quality of life of patients with asthma]. Rev Port Clin Geral 2006;22(6):671–87. [Google Scholar]
- Howie JG, Heaney DJ, Maxwell M, Walker JJ. A comparison of a Patient Enablement Instrument (PEI) against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract 1998;15(2):165–71. http://dx.doi.org/10.1093/fampra/15.2.165 [DOI] [PubMed] [Google Scholar]
- Haughney J, Cotton P, Rosen JP, Rosen JP, Morrison K, Price D. The use of a modification of the Patient Enablement Instrument in asthma. Prim Care Respir J 2007;16(2):89–92. http://dx.doi.org/10.3132/pcrj.2007.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Estatística. Estimativas Provisórias de População Residente Portugal, NUTS II, NUTS III e Municípios — 2005 [Provisional Population Estimates of Residents in Portugal, NUTS II, NUTS III and Municipalities — 2005]. Lisboa: Instituto Nacional de Estatística, 2006. p. 4.
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996;49:1373–9. http://dx.doi.org/10.1016/S0895-4356(96)00236-3 [DOI] [PubMed] [Google Scholar]
- Correia de Sousa J, Silva ML, Lobo FA, Yaphe J. Asthma incidence and accuracy of diagnosis in the Portuguese sentinel practice network. Prim Care Respir J 2010;19(4):352–7. http://dx.doi.org/10.4104/pcrj.2010.00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graffar M. Uneéthode de classification sociale d’échantilons de population. Courrier VI 1956;6:445–59. [Google Scholar]
- Juniper EF, Guyatt GH, Cox FM, Ferrie PJ, King DR. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Respir J 1999;14(1):32–8. http://dx.doi.org/10.1034/j.1399-3003.1999.14a08.x [DOI] [PubMed] [Google Scholar]
- Fonseca JA, Costa-Pereira A, Delgado L, et al. Pulmonary function electronic monitoring devices: a randomized agreement study. Chest 2005;128(3):1258–65. http://dx.doi.org/10.1378/chest.128.3.1258 [DOI] [PubMed] [Google Scholar]
- nSpire: Inspiring Respiratory Health. PiKo-1: Electronic Peak Flow and FEV1 Meter. Available from: http://www.nspirehealth.com/default.asp?LINKNAME=PIKO-1_MONITOR [cited 23 Jun 2011].
- Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982;143(1):29–36. [DOI] [PubMed] [Google Scholar]
- Arnlind MH, Nokela M, Ehrs PO, Wikström Jonsson E. Asthma severity in primary care asthma patients: a comparative study of four different approaches to severity classification. Prim Care Respir J 2010;19(4):383–9. http://dx.doi.org/10.4104/pcrj.2010.00046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liard R, Leynaert B, Zureik M, Beguin FX, Neukirch F. Using Global Initiative for Asthma guidelines to assess asthma severity in populations. Eur Respir J 2000;16(4):615–20. http://dx.doi.org/10.1034/j.1399-3003.2000.16d08.x [DOI] [PubMed] [Google Scholar]
- Australian Centre for Asthma Monitoring. Measuring the impact of asthma on quality of life in the Australian population. AIHW Cat No. ACM 3. Canberra: Australian Institute of Health and Welfare, 2004. [Google Scholar]
- Forrest CB, Starfield B, Riley AW, Kang M. The impact of asthma on the health status of adolescents. Pediatrics 1997;99(2):E1. http://dx.doi.org/10.1542/peds.99.2.e1 [DOI] [PubMed] [Google Scholar]
- Schatz M, Mosen DM, Kosinski M, et al. The relationship between asthma-specific quality of life and asthma control. J Asthma 2007;44(5):391–5. http://dx.doi.org/10.1080/02770900701364296 [DOI] [PubMed] [Google Scholar]
- Lobo FA, Lobo BA. Quality of life in asthmatic outpatients. J Asthma 2008;45(1):27–32. http://dx.doi.org/10.1080/02770900701815495 [DOI] [PubMed] [Google Scholar]
- Wijnhoven HA, Kriegsman DM, Hesselink AE, de Haan M, Schellevis FG. The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respir Med 2003;97(5):468–75. http://dx.doi.org/10.1053/rmed.2002.1463 [DOI] [PubMed] [Google Scholar]
- Gibson PG, Coughlan J, Wilson AJ, et al. Self-management education and regular practitioner review for adults with asthma (Cochrane Review). In: The Cochrane Library, Issue 2. Oxford: Update Software, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoonen BP, Schermer TR, Akkermans RP, den Otter JJ, Grol R, van Schayck OC. Willingness of patients to perform self-management of asthma and the role of inhaled steroids. Scand J Prim Health Care 2002;20(1):60–4. http://dx.doi.org/10.1080/028134302317282770 [DOI] [PubMed] [Google Scholar]
- Hardwell A, Barber V, Hargadon T, McKnight E, Holmes J, Levy ML. Technique training does not improve the ability of most patients to use pressurised metered-dose inhalers (pMDIs). Prim Care Respir J 2011;20(1):92–6. http://dx.doi.org/10.4104/pcrj.2010.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thoonen BP, Schermer TR, van den Boom G, et al. Self-management of asthma in general practice, asthma control and quality of life: a randomised controlled trial. Thorax 2003;58(1):30–6. http://dx.doi.org/10.1136/thorax.58.1.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhl R, Price D. Patients' perceptions of well-being using a guided self-management plan in asthma. Int J Clin Pract 2004;58(Suppl 141):26–32. http://dx.doi.org/10.1111/j.1368-504X.2004.00262.x14994967 [Google Scholar]
- Lavoie KL, Bouchard A, Joseph M, Campbell TS, Favreau H, Bacon SL. Association of asthma self-efficacy to asthma control and quality of life. Ann Behav Med 2008;36(1):100–06. http://dx.doi.org/10.1007/s12160-008-9053-8 [DOI] [PubMed] [Google Scholar]


