Abstract
Asthma is one of the most important chronic diseases in childhood. For several decades, a steady increase in prevalence has been observed worldwide. In the structural collaboration between the Centre for Population Health Services in Edinburgh and the Research Institute CAPHRI of Maastricht we investigated the possibilities for primary prevention of asthma in childhood. We found that a multifaceted approach might be effective in delaying or preventing asthma, whereas a mono-intervention does not seem to have such a protective effect. The most likely explanation is that the development of a multifactorial disease, such as asthma, is extremely difficult, if not impossible, to prevent by eliminating only one risk factor.
Underdiagnosis of asthma is still a big problem in primary care. Most patients do not present bronchial symptoms to the general practitioner, even though they have decreased lung function, so they remain unknown and undiagnosed. However, patients who do present with respiratory problems and who have reduced lung function are not always recognised as such. We found that the perception of dyspnoea seems to determine, at least in part, the presentation to the general practitioner with symptoms.
These observations show that both the prevention of the development of asthma in early childhood, as well as case finding of asthma in adulthood, do not seem to be very effective in primary care. More research is needed to clarify what steps can be taken to reduce the global burden from asthma.
Keywords: Asthma, global burden, prevalence, diagnosis, prevention, case finding, primary care, research
Onno van Schayck is an Assistant Editor of the PCRJ. Following his Inaugural Lecture to the Centre for Population Health Sciences in October 2012, the Editors-in-Chief commissioned this article to celebrate the occasion and to give readers the opportunity to read about Professor van Schayck's contribution to primary care respiratory research over the last 25 years. We will publish summaries of other Inaugural lectures given by key figures in primary care respiratory medicine from time-to-time in future issues.
Introduction
In 1998 I was appointed as Professor of Medicine at the Departments of General Practice of both Maastricht University and Nijmegen University. Since 2008 the Research Institute CAPHRI of Maastricht University and the Centre for Population Health Services of the University of Edinburgh have had a structural cooperation, especially in the area of childhood asthma. In 2010, I was invited to become Honorary Professor here at the Centre for Population Health Services in Edinburgh, and on October 1st, 2012 I had the honour to give my inaugural lecture at the University of Edinburgh.
My lecture focused on strategies for reducing the burden from asthma, covering the work of the research groups in Maastricht and Edinburgh, and especially the collaboration between these groups.
The burden of asthma
Asthma is one of the most important chronic diseases in childhood.1 The prevalence of childhood asthma is high.2 For several decades, a steady increase in prevalence has been observed worldwide.3,4 However, in some parts of the world, the first signs of stabilisation5 or even a decrease in prevalence2 have been reported. Asthma poses a great burden on patients, their family members, health care services, and society. Asthma is the main cause of school absence.6 The number of asthma-related contacts and hospitalisations is high, which results in substantial costs of treating asthma (for instance 20.4% of the total health care costs in infants under the age of 1 year, and 24.1% in infants and children aged 1–14 years in the Netherlands).7
Research interests
a) The deleterious effects of continuous bronchodilatation
My research started in the late 1980s/early 1990s with the discovery that continuous use of bronchodilators in asthma resulted in deleterious effects, especially when no anti-inflammatory medication is used.8–11 This finding was especially important for primary care as bronchodilators were until then often used as the sole medication for asthma in general practice. It stimulated efforts to ensure the early introduction of inhaled steroids in asthma as well as the use of combination drugs (inhaled long-acting bronchodilators together with corticosteroids in one device), which are nowadays the mainstay of asthma treatment both in primary and secondary care. But it also stimulated efforts to obtain an early diagnosis of asthma in order to avoid untreated progression. Moreover, it stimulated in our research groups the investigation of non-pharmacological preventive measures such as inhalant and food allergen avoidance in order to prevent asthma in genetically predisposed infants.
b) Risk factors for asthma
The risk of developing asthma is determined by genetic, as well as environmental, factors. Because specific genes for asthma have not been fully identified, the focus has been on a family history of asthma. This approach is especially useful in primary care, with family doctors having access to all information of all family members. With regard to environmental factors, passive smoking and house dust mite, cat, and dog allergens are thought to be associated with sensitisation and allergic disease, whereas breastfeeding is thought to have a protective effect.12–16
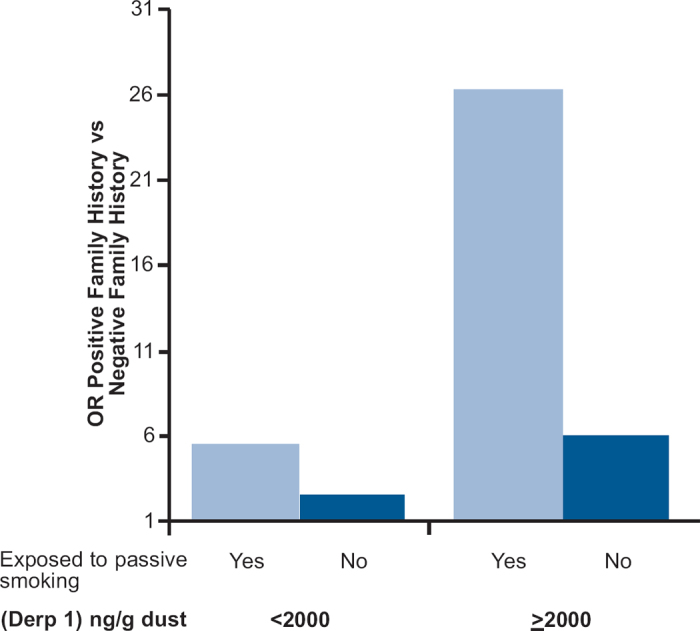
In the late 1990s, we began in the Netherlands a prospective birth cohort with almost 800 children recruited prenatally in primary care. Family history of asthma as determined in primary care was a significant risk factor for the occurrence of respiratory tract and asthma-related morbidity during the first 2 years of life. A particularly intriguing finding was that the relationship between a positive family history and respiratory morbidity was modified by postnatal exposure to parental smoking, house dust mite and breast-feeding.17 Parental smoking and house dust mite exposure increased the effect of a positive family history on wheezing. Moreover, when these infants were exposed to both parental passive smoking and house dust mite, this increase was even more pronounced (see Figure 1).
Figure 1. Interactive effect on wheezing of exposure to passive smoking and to house dust mite. Used with permission from the editor of J Allergy Clin Immunol. From Kuiper et al. JACI 2007;120:388–9517.
c) The interaction between genotype and environment — childhood asthma
On the basis that the interaction between genotype and environment plays a crucial role, it is reasonable to assume that reducing exposure to potentially relevant allergens should lead to a reduction in the risk of asthma. This concept is, however, mainly based on observations made in the early 1980s, which found that dramatic reduction of house dust mite (Derp 1) exposure, by moving children with asthma into a hospital or to a mountain sanatorium, could considerably reduce symptoms of asthma.18,19 But translating these secondary prevention findings into feasible-to-deliver primary prevention strategies had proved extremely difficult, as demonstrated by the disappointing results of large, carefully designed, randomised clinical trials of house dust mite avoidance strategies in birth cohorts.20,21 However, this is also true in relation to the more direct comparison of secondary prevention strategies.22 The reasons behind their lack of effectiveness remain unclear, however.
Since people with asthma are usually sensitised to more than one allergen, the successful elimination of one allergen is only likely to have limited clinical benefit. It is therefore logical, although experimentally somewhat complex, to test the efficacy and effectiveness of multifaceted approaches to allergen avoidance. The main potential disadvantage of a multifaceted approach is that it is difficult to disentangle the effects of one intervention from those of another. A number of randomised clinical trials have been conducted in new-born children to investigate whether the development of asthma can be prevented or delayed by reducing exposure to inhalant allergens, feeding allergens, or both. Although the majority of these studies investigated only one measure, others have used a multifaceted approach. Because there was no published systematic review on possible differences between these two approaches, researchers from Maastricht and Edinburgh together performed a search of the Cochrane Central Register of Controlled trials. In total, 10 high-quality studies (enrolling 3473 patients) were included, of which 1124 had a multifaceted intervention design23–25 and 2349 had a mono-intervention design.21,26–31 Several studies had repeated measurements on different ages of the children. The results suggested that a multifaceted approach might be effective in delaying or preventing asthma, whereas a mono-intervention does not seem to have such a protective effect. The most likely explanation is that the development of a multifactorial disease, such as asthma, is extremely difficult, if not impossible, to prevent by eliminating only one risk factor.32,33
d) Detecting and diagnosing adult asthma
Asthma is not only a problem in childhood, but also in adulthood. In childhood the major challenge is to prevent the development of asthma. In adulthood the major challenge is to detect and diagnose asthma as early as possible. There is still an increase in the morbidity and mortality of adult asthma,34,35 which seems to apply to patients diagnosed as having asthma as well as to those in whom a diagnosis of asthma has not yet been made.36 Under-diagnosis and consequent undertreatment might be important in the increased morbidity and mortality of asthma.37,38 Early detection and treatment of asthma might improve the long-term prognosis of these patients10 and this secondary prevention may also prevent irreversible loss of function.39 It is not clear whether the physician or the patient is to blame: is under-diagnosis of asthma caused by the physician who does not adequately interpret the symptoms presented to him (or her)? Or is it caused by the patient who does not present his or her symptoms to the physician?40 In the latter case, it is not clear why a patient does not present his or her symptoms to the general practitioner. Is this caused by poor perception of the symptom of dyspnoea in particular?41–43
Our research group from the Department of General Practice in Nijmegen investigated several questions:
- 1. Is underdiagnosis of asthma caused by the physician or is it caused by the patient?
- 2. If it is caused by the patient why do patients not present their symptoms to their physicians?
We recruited a random sample of 1155 subjects aged 25–70 selected from 10 urban and rural general practices in the eastern part of the Netherlands.44 In the Netherlands, all subjects in the general population are registered with a general practitioner. These 1155 subjects went through an extensive screening programme which included several measurements of forced expiratory volume in one second (FEV1) and a questionnaire which included a question on whether they had ever presented with respiratory problems such as wheezing, coughing, or dyspnoea to the general practitioner.36 Special attention was paid to the number of subjects with objective airway obstruction and symptoms suggestive of asthma (wheezing, recurrent coughing, or dyspnoea) to investigate further under-presentation and under-diagnosis in this group of higher risk subjects. FEV1 was measured twice in a four-month period under standard conditions. The medical files at the surgeries of the general practitioner were analysed for asthma-related consultations. All files were checked if either asthma-related complaints and symptoms, or prescribed asthma drugs, or both, were present. All asthma-related consultations were scored.
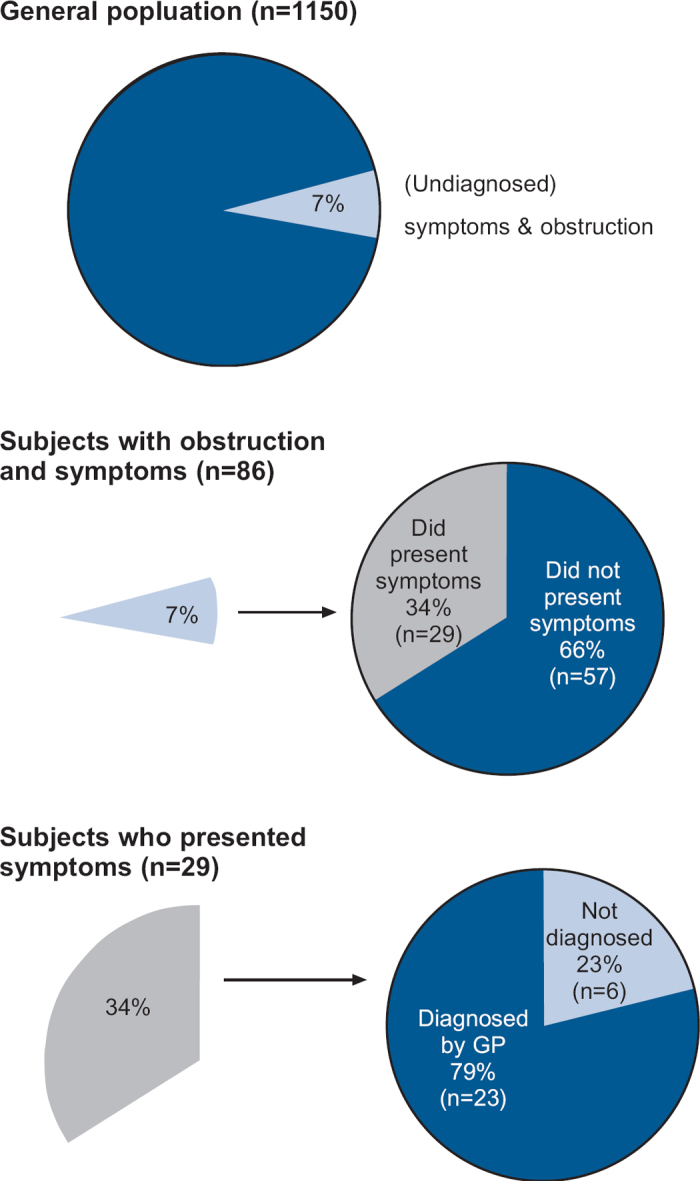
Of the random sample of 1155 subjects, 86 (7%) had objective airflow obstruction as well as symptoms suggestive of asthma (see Figure 2).44 The question of the extent to which the presentation of symptoms by the patient to the general practitioner is picked up and translated into a diagnosis is preceded by another question -namely, whether or not the patient presents the symptoms to the general practitioner. From the results of this study it appears that most patients (66%) do not present bronchial symptoms to their general practitioner, even though they have decreased lung function, so they remain unknown and undiagnosed. However, patients who do present with respiratory problems and who have reduced lung function are not always recognised as such. In this group, the interpretation of the complaint at presentation has probably been a wrong one. In looking for possible causes of under-diagnosis of asthma, this study indicated that the problem is mainly due to the patient and only partly to the general practitioner.
Figure 2. Underdiagnosed asthma in primary care (based on data from van Schayck CP, et al. Thorax 2000;55: 562–5)44.
For the second question, a random sample of subjects with objective lung function was selected. Of the 86 subjects with reduced lung function, 47 were further investigated to determine their ability to perceive dyspnoea by assessing the change in Borg score during a histamine provocation test carried out using the method described by Brand et al.41 After the measurements the subjects were classified into two groups: “good perceivers”, in whom a decrease in FEV1 was accompanied by an increase in the Borg score; and “poor perceivers”, in whom there was a 20% decrease in FEV1 or an observed decrease in FEV1 after the last doubling dose of 32 mg/ml histamine which was not accompanied by any increase in the Borg score.41 It was then determined whether or not patients in the two groups with reduced lung function had consulted their general practitioner with asthma-related symptoms.
We investigated whether the ability to perceive airway obstruction determines whether or not a patient visits his or her general practitioner with concomitant airway symptoms (dyspnoea). This study showed that the perception of dyspnoea seems to determine, at least in part, the presentation to the general practitioner with symptoms. Of the subjects with bronchial obstruction who did visit the general practitioner with airways symptoms, 6% had poor perception of dyspnoea; however, of the subjects who did not visit the general practitioner in spite of bronchial obstruction, the percentage with a poor perception of dyspnoea was more than four times higher at 26%.44
Future research
These observations show that both prevention of the development of asthma in early childhood, as well as case finding of asthma in adulthood, do not seem to be very effective in primary care. More research has to be done to clarify what steps can be taken to reduce the global burden from asthma.
There are at least three topics that require more attention in the coming years:
Early detection of (high-risk) asthma in infancy by means of noninvasive measurements in exhaled breath (e.g. Exhaled Breath Condensate [EBC] and Volatile Organic Compounds [VOCs]).
Studying gene-environment interaction in large cohorts with well-defined phenotypes of asthma.
Studying the effects of (exposure to) smoking during pregnancy, infancy and adults, by using large cohorts of general practice registries.
All three of these topics are being studied as part of the structural cooperation between the Research Institute of Maastricht University and the Centre for Population Health Services of the University of Edinburgh.
Acknowledgments
I would like to thank Professor Aziz Sheikh and Dr Paul Stephenson for their valuable comments on this paper.
Funding None in relation to this article.
Footnotes
The author declares that he has no conflicts of interest in relation to this article. He is an Assistant Editor of the PCRJ, but was not involved in the editorial review of, nor the decision to publish, this article.
References
- Von Mutius E. The burden of childhood asthma. Arch Dis Child 2000;2:112–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Schayck CP, Smit HA. The prevalence of asthma in children: a reversing trend. Eur Respir J 2005;26:647–50. http://dx.doi.org/10.1183/09031936.05.00019805 [DOI] [PubMed] [Google Scholar]
- The International Study of Asthma and allergies in Childhood (ISAAC) steering Committee. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. Lancet 1998;351(9111):1225–32. [PubMed] [Google Scholar]
- Eldeirawi K, Persky VW. History of ear infections and prevalence of asthma in a national sample of children aged 2 to 1 years: the Third National Health And Nutrition Examination Survey, 1988 to 1994. Chest 2004;125:1685–9. http://dx.doi.org/10.1378/chest.125.5.1685 [DOI] [PubMed] [Google Scholar]
- Mommers M, Gielkens-Sijstermans C, Swaen GMH, van Schayck CP. Trends in prevalence of respiratory symptoms and treatment in Dutch children over a 12 year period: results of the fourth consecutive survey. Thorax 2005;60:97–9. http://dx.doi.org/10.1136/thx.2004.024786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin JB, Sekvaraj S, Russell G. Childhood asthma in the highlands of Scotland-Morbidity and school absence. Scott Med J 2004;49:18–21. [DOI] [PubMed] [Google Scholar]
- Polder JJ, Takken J, Merding WJ, Kommer GJ, Stokx LJ. Cost of illness in the Netherlands. (RIVM report 270751005/2002) Available at: www.rivm.nl/kostenvanziekten. Accessed April 30, 2007.
- van Schayck CP, Graafsma SJ, Visch MB, Dompeling E, van Weel C, van Herwaarden CLA. Increased bronchial hyperresponsiveness after inhaling salbutamol during one year is not caused by subsensitization to salbutamol. J Allergy Clin Immunol 1990;86(5):793–800. http://dx.doi.org/10.1016/S0091-6749(05)80185-X [DOI] [PubMed] [Google Scholar]
- van Schayck CP, Dompeling E, van Herwaarden CLA, et al. Bronchodilator treatment in moderate asthma or chronic bronchitis: continuous or on demand? A randomized controlled study. BMJ 1991;303:1426–31. http://dx.doi.org/10.1136/bmj.303.6815.1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dompeling E, van Schayck CP, van Grunsven PM, et al. Slowing the deterioration of asthma and chronic obstructive pulmonary disease observed during bronchodilator therapy by adding inhaled corticosteroids. Ann Intern Med 1993;118:770–8. http://dx.doi.org/10.7326/0003-4819-118-10-199305150-00003 [DOI] [PubMed] [Google Scholar]
- van Schayck CP, van den Broek PJJA, den Otter JJ, van Herwaarden CLA, Molema J, van Weel C. Periodic treatment regimens with inhaled steroids in asthma or chronic obstructive pulmonary disease. Is it possible? JAMA 1995;274(2):161–4. http://dx.doi.org/10.1001/jama.1995.03530020079036 [DOI] [PubMed] [Google Scholar]
- DiFranza JR, Aligne CA, Weitzman M. Prenetal and postnatal environmental tobacco exposure and children's health. Pediatrics 2004;113:1007–15. [PubMed] [Google Scholar]
- Wahn U, Lau S, Bergmann R, et al. Indoor allergen exposure is a risk factor for sensitization during the first three years of life. J Allergy Clin Immunol 1997;99:763–9. http://dx.doi.org/10.1016/S0091-6749(97)80009-7 [DOI] [PubMed] [Google Scholar]
- Vanto T, Koivikko A. Dog hypersensitivity in asthmatic children. Acta Paediatr Scand 1983;72:571–5. http://dx.doi.org/10.1111/j.1651-2227.1983.tb09773.x [DOI] [PubMed] [Google Scholar]
- Warner JA, Little SA, Pollock I, Longbottom JL, Warner JO. The influence of exposure to house dust mite, cat and pollen allergens in the homes on primary sensitization in asthma. Pediatr Allergy Immunol 1991;1:79–86. http://dx.doi.org/10.1111/j.1399-3038.1990.tb00015.x [Google Scholar]
- Chantry CJ, Howard CR, Auinger P. Full breastfeeding duration and associated decrease in respiratory tract infection in US children. Pediatrics 2006;117:425–32. http://dx.doi.org/10.1542/peds.2004-2283 [DOI] [PubMed] [Google Scholar]
- Kuipers S, Muris JWM, Dompeling E, et al. Interactive effect of family history and environmental factors on respiratory tract-related morbidity in infancy. J Allergy Clin Immunol 2007;120(2):388–95. http://dx.doi.org/10.1016/j.jaci.2007.03.038 [DOI] [PubMed] [Google Scholar]
- Boner Al, Niero E, Antolini I, Valletta EA, Gaburro D. Pulmonary function and bronchial hyper-reactivity in asthmatic children with house dust mite allergy during prolonged stay in the Italian Alps (Misurina, 1756 m.) Ann Allergy 1985;54:42–5. [PubMed] [Google Scholar]
- Platt-Mills TA, Tovery ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperactivity during proglonged allergen avoidance. Lancet 1982;2(8300):675–8. http://dx.doi.org/10.1016/S0140-6736(82)90709-7 [DOI] [PubMed] [Google Scholar]
- Koopman LP, van Strien RT, Kerkhof M, et al. Placebo-controlled trial of house dust mite-impermeable mattress covers: effect on symptoms in early childhood. Am J Respir Crit Care Med 2002;166:307–13. http://dx.doi.org/10.1164/rccm.2106026 [DOI] [PubMed] [Google Scholar]
- Woodcock A, Lowe LA, Murray CS, et al. Early life environmental control: effect on symptoms, sensitization, and lung function at age 3 years. Am J Respir Crit Care Med 2004;170:433–9. http://dx.doi.org/10.1164/rccm.200401-083OC [DOI] [PubMed] [Google Scholar]
- Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev 2004. Oct 18;(4):CD001187. [DOI] [PubMed] [Google Scholar]
- Hide DW, Matthews S, Matthews L, et al. Effect of allergen avoidance in infancy on allergic manifestations at age two years. J Allergy Clin Immunol 1994;93:842–6. http://dx.doi.org/10.1016/0091-6749(94)90375-1 [DOI] [PubMed] [Google Scholar]
- Becker A, Watson W, Ferguson A, Dimich-Ward H, Chan-Yeung M. The Canadian asthma primary prevention study: outcomes at 2 years of age. J Allergy Clin Immunol 2004;113:650–6. http://dx.doi.org/10.1016/j.jaci.2004.01.754 [DOI] [PubMed] [Google Scholar]
- Schonberger HJ, Dompeling E, Knottnerus JA, et al. The PREVAC study: the clinical effect of a multi-facet educational intervention to prevent childhood asthma. Eur Respir J 2005;25:1–11. http://dx.doi.org/10.1183/09031936.05.00067704 [DOI] [PubMed] [Google Scholar]
- Mallet E, Henocq A. Long-term prevention of allergic diseases by using protein hydrolysate formula in at-risk infants. J Pediatr 1992;121(suppl):S95–100. http://dx.doi.org/10.1016/S0022-3476(05)81415-5 [DOI] [PubMed] [Google Scholar]
- Zeiger RS, Heller S. Genetic and environmental factors affecting the development of atopy through age 4 in children of atopic parents: a prospective randomized study of food allergen avoidance. Pediatr Allergy Immunol 1992;3:110–27. http://dx.doi.org/10.1111/j.1399-3038.1992.tb00035.x [Google Scholar]
- Horak FJr, Matthews S, Ihorst G, et al. Effect of mite-impermeable mattress encasings and an educational package on the development of allergies in a multinational randomized, controlled birth-cohort study — 24 months results of the Study of Prevention of Allergy in Children in Europe. Clin Exp Allergy 2004;34:1220–5. http://dx.doi.org/10.1111/j.1365-2222.2004.02024.x [DOI] [PubMed] [Google Scholar]
- Peat JK, Mihrshahi S, Kemp AS, et al. Three-year outcomes of dietary fatty acid modification and house dust mite reduction in the Childhood Asthma Prevention Study. J Allergy Clin Immunol 2004;114:807–13. http://dx.doi.org/10.1016/j.jaci.2004.06.057 [DOI] [PubMed] [Google Scholar]
- Johnstone DE, Dutton AM. Dietary prophylaxis of allergic disease in children. N Engl J Med 1966;247:715–19. http://dx.doi.org/10.1056/NEJM196603312741305 [DOI] [PubMed] [Google Scholar]
- Kjellman NIM, Johansson SGO. Soy versus cow's milk infants with a biparental history of atopic disease: development of atopic disease and immunoglobulins from birth to 4 years of age. Clin Allergy 1979;9:347–58. http://dx.doi.org/10.1111/j.1365-2222.1979.tb02493.x [DOI] [PubMed] [Google Scholar]
- van Schayck CP, Maas T, Kaper J, Knottnerus AJA, Sheikh A. Is there any role for allergen avoidance in the primary prevention of childhood asthma? J Allergy Clin Immunol 2007;119:1323–8. http://dx.doi.org/10.1016/j.jaci.2007.02.024 [DOI] [PubMed] [Google Scholar]
- Maas T, Kaper J, Sheikh A, et al. Mono and multifaceted inhalant and/or food allergen reduction interventions for preventing asthma in children at high risk of developing asthma. Cochrane Database of Systematic Reviews 2009; Jul 8(3):Art. No.: CD006480. http://dx.doi.org/10.1002/14651858.CD006480.pub2 [DOI] [PubMed] [Google Scholar]
- Ayres JG, Noah ND, Fleming DM. Incidence of episodes of acute asthma and acute bronchitis in general practice 1976-87. Br J Gen Pract 1993;43:361–4. [PMC free article] [PubMed] [Google Scholar]
- Lange P, Ulrik CS, Vestbo J, for the Copenhagen City Heart Study Group. Mortality in adults with self reported asthma. Lancet 1996;347:1285–9. [DOI] [PubMed] [Google Scholar]
- van den Boom G, van Schayck CP, Rutten-van Mölken MPMH, et al. Active detection of COPD and asthma in the general population: results and economic consequencies of the DIMCA programme. Am J Respir Crit Care Med 1998;158:1730–8. http://dx.doi.org/10.1164/ajrccm.158.6.9709003 [DOI] [PubMed] [Google Scholar]
- Speight AN, Lee DA, Hey EN. Underdiagnosis and undertreatment of asthma in childhood. BMJ 1983;286:1253–6. http://dx.doi.org/10.1136/bm [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes PJ. Blunted perception and death from asthma. N Engl J Med 1994;30:1383–4. http://dx.doi.org/10.1056/NEJM199405123301910 [DOI] [PubMed] [Google Scholar]
- Haahtela T, Järvinen M, Kava T, et al. Effects on reducing or discontinuing inhaled budesonide in patients with mild asthma. N Engl J Med 1994;331:700–05. http://dx.doi.org/10.1056/NEJM199409153311103 [DOI] [PubMed] [Google Scholar]
- Levy M. Delay in diagnosing asthma. Is the nature of general practice to blame? J R Coll Gen Pract 1986;36:52–3. [PMC free article] [PubMed] [Google Scholar]
- Brand PLP, Rijcken B, Schouten JP, et al. Perception of airways obstruction in a random population sample: relationship to airways hyperresponsiveness in the absence of respiratory symptoms. Am Rev Respir Dis 1992;146:396–401. http://dx.doi.org/10.1164/ajrccm/146.2.396 [DOI] [PubMed] [Google Scholar]
- Kendrick AH, Hoggs CMB, Whitfield MJ, et al. Accurancy of perception of severity of asthma patients treated in general practice. BMJ 1993;307:422–4. http://dx.doi.org/10.1136/bmj.307.6901.422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes PJ. Poorly perceived asthma. Thorax 1992;47:408–09. http://dx.doi.org/10.1136/thx.47.6.408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Schayck CP, van der Heijden FMMA, van den Boom G, Tirimanna PRS, van Herwaarden CLA. Underdiagnosis of asthma: is the doctor or the patient to blame? The DIMCA-project. Thorax 2000;55(7):562–5. http://dx.doi.org/10.1136/thorax.55.7.562 [DOI] [PMC free article] [PubMed] [Google Scholar]


