Abstract
Background:
Pulmonary rehabilitation (PR) is recommended in the management of people with chronic obstructive pulmonary disease (COPD), but referral to this service is low.
Aims:
To identify barriers to, and facilitators for, referral to PR programmes from the perspective of Australian general practitioners.
Methods:
Semi-structured interviews were conducted with general practitioners involved in the care of people with COPD. Interview questions were informed by a validated behavioural framework and asked about participants’ experience of referring people with COPD for PR, and barriers to, or facilitators of, this behaviour. Interviews were audiotaped, transcribed verbatim, and analysed using content analysis.
Results:
Twelve general practitioners participated in this study, 10 of whom had never referred a patient to a PR programme. Four major categories relating to barriers to referral were identified: low knowledge of PR for COPD; low knowledge of how to refer; actual or anticipated access difficulties for patients; and questioning the need to do more to promote exercise behaviour change. Awareness of benefit was the only current facilitator. Three major categories of potential facilitators were identified: making PR part of standard COPD care through financial incentive; improving information flow with regard to referrals and services; and informing patients and public.
Conclusions:
Significant barriers to referral exist, but opportunities to change the organisation of practice and information management were identified. Behaviour change strategies which directly target these barriers and incorporate facilitators should make up the key components of interventions to improve referral to PR by general practitioners who care for people with COPD.
Keywords: chronic obstructive pulmonary disease, primary care, pulmonary rehabilitation, barriers, qualitative research
Background
Chronic obstructive pulmonary disease (COPD) is a common and disabling condition that is frequently managed by primary care practitioners.1 Analysis of data from 187 countries ranked COPD as the third leading global cause of death in 2010.2 In Australia, the prevalence of COPD (Global Initiative for Chronic Obstructive Lung Disease (GOLD)3 stage II or higher) is reported as 7.5% among people aged ≥40 years and 29.2% among those aged ≥75 years.4
Pulmonary rehabilitation (PR) is a programme of structured supervised exercise, education, and psychosocial support which is recommended by international guidelines in the management of people with COPD.3 There is strong evidence that PR improves exercise tolerance, reduces anxiety, and improves symptoms in people with moderate to severe COPD.5 Participation in PR reduces admissions to hospital for exacerbation of symptoms6 and has demonstrated effectiveness in terms of cost per quality-adjusted life years.7
Despite the known benefits of PR, referral to such programmes is low. A systematic review of international surveys and practice audits indicated that between 3% and 16% of suitable COPD patients in general practice were referred to PR.8 While 85% of Australian PR programmes report that they accept referrals from general practitioners,9 referrals appear to be predominantly received from respiratory physicians.6 In contrast, a UK review of a London-based PR programme reported that 57% of referrals were from primary care (13% general practitioner, 21% practice nurse, 23% community COPD clinic).10
In order to address the low implementation of this evidence-based recommendation, more information is needed about the reasons why general practitioners do not refer people with COPD to PR programmes. Perspectives of general practitioners regarding how to improve referral rates to PR are also required.
The research questions explored in this study are: (1) What are the barriers for general practitioners to referral of people with COPD to PR programmes? (2) What does or would facilitate general practitioners to refer people with COPD to PR programmes?
Methods
A qualitative study using semi-structured interviews was undertaken, with questions and analysis based on a theoretical behavioural framework specifically designed to examine implementation of evidence-based practice.11 The study was approved by the relevant ethics committees prior to commencement.
Participants
This study formed part of an evaluation of patients admitted to a large tertiary hospital with a primary diagnosis of COPD exacerbation between March and November 2011. The recruited patients with COPD were potentially eligible for PR programmes (i.e. sufficient English language, cognitive status, and physical capability). One month after each recruited patient had been discharged from hospital, written contact was made with the patient's general practitioner, inviting them to participate in the study. Letters were followed up with one telephone call. In this way, a purposive sample of general practitioners actively involved in the care of COPD patients in the local area was obtained. Informed consent was obtained from all participants.
Data collection
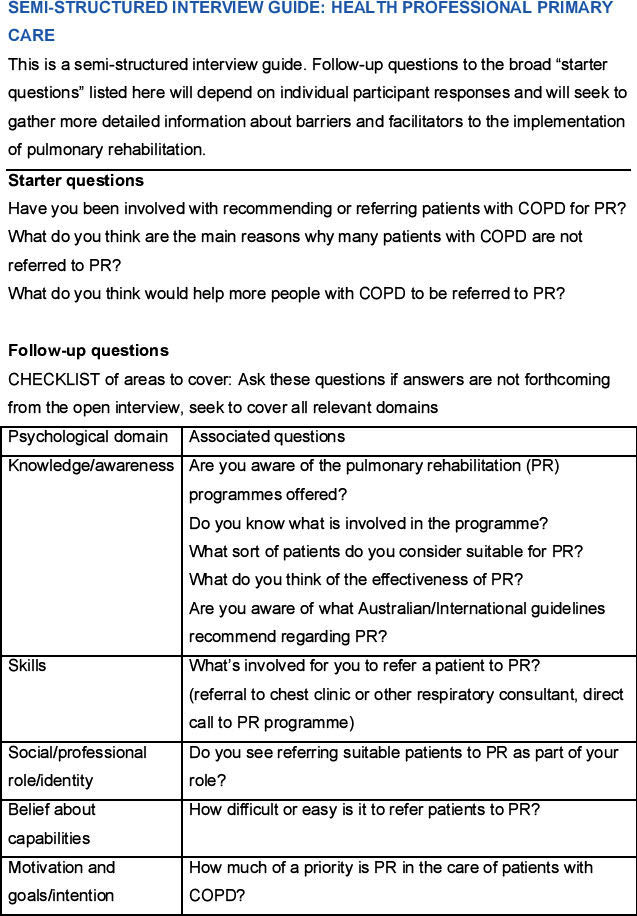
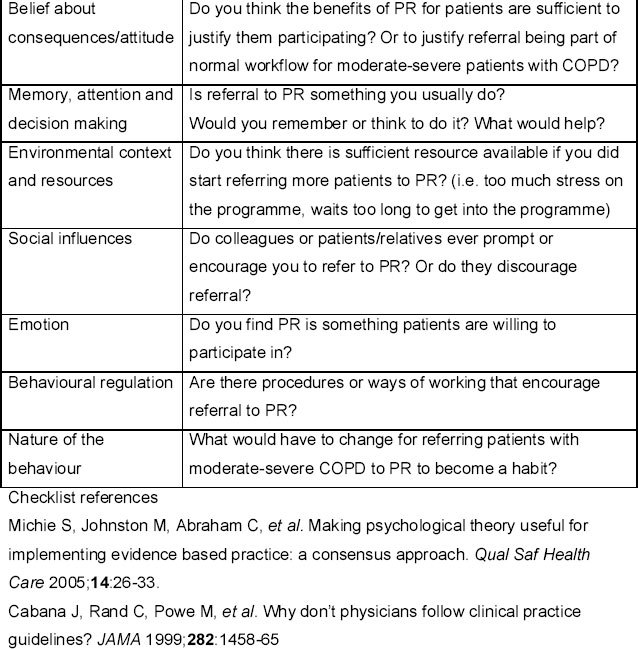
Semi-structured interviews were conducted with general practitioners to ask questions regarding (a) experience of referring people with COPD to PR programmes; (b) barriers to referring people with COPD to PR programmes; and (c) actual or potential facilitators for referral of people with COPD to PR programmes. Interview guide questions (see Appendix 1, available online at www.thepcrj.org) were informed by the Theoretical Domains Framework (TDF).11 This consensus-derived validated framework integrates multiple behaviour change theories and provides a classification of 12 domains that may influence behaviour.12 The TDF was specifically developed to analyse barriers to and facilitators for implementing evidence-based practice by health professionals.11,12
General practitioners were given the option of conducting the interview face-to-face at their practice or by telephone. All interviews were conducted by the same researcher (postdoctoral research fellow with experience in qualitative research and clinical practice in COPD) and were audiotaped. Recordings were transcribed by an independent service and subsequently compared with the audio recording by the interviewer for completeness and accuracy. Demographic information collected directly from participants included their years of experience and practice setting (metropolitan/rural).
Data analysis
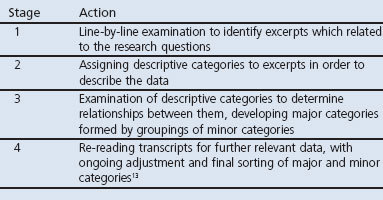
De-identified transcripts were content analysed13,14 to identify and classify categories within the data in relation to the research questions (Table 1). The NVivo9 software (QSR International Pty Ltd) was used to organise the data and facilitate analysis.
Table 1. Content analysis process.
Quotations from the transcripts were extracted to provide supportive data for each category. Excerpts and organisation of major and minor categories were discussed with a second researcher until consensus was reached. Recruitment and data collection were continued until data saturation was achieved and no new categories were being generated from interview data.
Results
Thirty-eight general practitioners were invited to participate in the study and 12 agreed. The remaining 26 did not respond to one letter and one telephone call and were not contacted further. Eleven interviews were conducted face-to-face and one by telephone. Of the 12 participants (two female), one reported 10 years of experience in general practice while all the others had ≥20 years of experience. All were currently working in metropolitan areas and six had worked in rural general practice in the past.
Ten of the 12 general practitioners had never referred a patient to a PR programme. Of the ten who had not referred patients to a PR programme, two had referred patients with COPD to physiotherapists or reported that patients of theirs had been referred to PR programmes by respiratory physicians (n=2) or during a hospital admission (n=2).
Analysis identified four major categories relating to barriers to referral and four major categories which did or could facilitate referral to PR in people with COPD (Table 2). Descriptive categories which later contributed to all eight major categories were established after the first six interviews. Descriptive categories which contributed to all minor categories were established after eight interviews, and major categories were formed and consolidated by the tenth interview. No new major or minor categories were added during the last two interviews and existing categories were further supported.
Table 2. Categories associated with barriers to and facilitators of referral of people with chronic obstructive pulmonary disease (COPD) to pulmonary rehabilitation (PR).
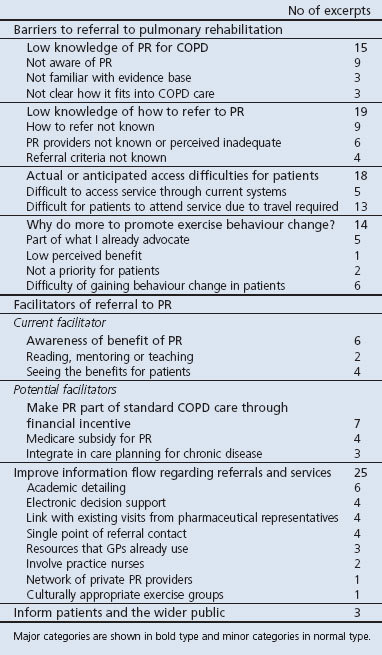
Major barriers to referral to pulmonary rehabilitation
(1) Low knowledge of PR for COPD
Nine transcript excerpts indicated that participants were not aware of the existence of PR programmes:
Three excerpts indicated that participants were unsure of the evidence base for PR. Others were unclear about the place of rehabilitation in overall COPD management.
(2) Low knowledge of how to refer to PR
Lack of detailed knowledge about how to refer potential patients to PR was reflected in nine excerpts:
It was not clear to participants who the providers of PR services actually were (6 excerpts).
Others questioned the quality of the service provided or the specific criteria for referral.
(3) Actual or anticipated access difficulties for patients
Participants gave examples of how difficult it was for their patients with COPD to attend appointments outside the home (13 excerpts).
Participants also described concern about availability or wait time for services in five excerpts:
(4) Why do more to promote exercise behaviour change?
This category reflected general practitioners' perceptions of the relative costs and benefits of PR for their patients with COPD. Five excerpts indicated that participants already gave attention to encouraging exercise, and in some cases did not prioritise another service (i.e. PR) with a similar focus.
However, participants also spoke of the challenge of gaining behaviour change towards more exercise in their patients.
Major facilitators of referral to pulmonary rehabilitation Current facilitator
(1) Awareness of benefit (6 excerpts)
Where participants did refer patients to PR, they had gained awareness through the mentoring and example of respiratory physicians, reading or seeing the benefits experienced by their patients:
Potential facilitators
Participants identified three major strategies that they felt would help more people with COPD be referred to PR:
(1) Make PR part of standard COPD care through financial incentives
Participants (in four excerpts) described how government subsidy for the cost of exercise assessment and intervention in patients with type 2 diabetes had helped to integrate this into the standard care of these patients:
Greater emphasis on inclusion of PR in chronic disease care planning for COPD, again linked to a financial incentive, was also suggested in three excerpts.
(2) Improve information flow regarding referrals and services
Twenty-five citations recommended ways to improve information flow. Visits to practices directly to provide relevant information were identified in 10 excerpts.
Participants suggested integrating relevant local referral and service information into electronic decision support systems (four excerpts) or resources already used by general practitioners including hospital discharge documentation (three excerpts), and promoting a greater role of practice nurses (two excerpts).
A single point of referral contact for PR services was suggested in four excerpts:
The problem of extreme busyness and too much information being provided was raised.
Offering PR services by a network of private providers and programmes in languages other than English were also recommended.
(3) Inform patients and the wider public
Raising public awareness of PR through print/electronic media or advertising in practice waiting areas was identified as a facilitator for referral in three excerpts:
Discussion
Main findings
This study found that 10 of the 12 general practitioners interviewed had not directly referred a person with COPD for PR. Barriers to referral were low knowledge of PR in the management of people with COPD; low knowledge of the referral process; difficulties with access to PR by their patients; and questions about the need to further promote exercise behaviour change in this patient group. General practitioners felt referral rates would be improved by integrating PR into standard care through financial incentive; improving information flow regarding referral and services; and informing the general public.
Strengths and limitations of this study
Study participants were involved in the management of at least one patient with COPD who had recently been discharged from a tertiary hospital. The interview guide and development of this study were based on our pilot research, which identified that referral to PR was low and associated with multiple barriers in comparison with other high-evidence recommendations in the care of people with COPD.15 A strength of our current study was the direct examination of perceived facilitators for referral. These data provide new information and potential solutions that may otherwise be overlooked in studies of barriers to guideline implementation.
Data collection was limited to a single interview and participants were not supplied with transcripts for checking; however, the interviewer made use of notes and reviewed transcripts against audio-recordings to ensure accuracy. We examined the time course of major and minor category development as interviews progressed, in accordance with methods previously described in qualitative research to support the validity of data saturation.16 Our research question was simple and well-defined, which may also have contributed to the timing of data saturation.17
Interpretation of findings in relation to previously published work
Lack of awareness and familiarity is well recognised as a key reason behind low implementation of guidelines in primary care generally,18 and specifically in relation to COPD management.19 Interview data from 16 Australian medical practitioners found complex barriers to PR referral in comparison to implementation of other high-evidence recommendations in COPD (e.g. smoking cessation, influenza vaccination).20 However, better communication about local PR service provision and streamlined referral pathways could embed this knowledge in the daily workflow of general practitioners. Harris and co-authors21 reported similar logistical barriers to PR (referral process and service provision) in focus groups with UK primary care health professionals. They proposed that these barriers resulted in lack of persuasive communication with patients about PR, with a negative effect on referral patterns.
The general practitioners in our study identified the difficulties faced by COPD patients in attending a centre-based rehabilitation programme. These perceptions reflect the reported concerns of people with COPD — namely, difficulties with transport, lack of perceived benefit, and being unwell — as reasons for not taking up an offer of PR.22 Service delivery changes which provide PR at home23 and/or make use of internet platforms24 instead of requiring patient travel may need to be added to the mix of PR modalities to overcome these environmental barriers.
The challenge of achieving change in exercise behaviour was met in some cases with the belief that general practitioners already offered sufficient advice. However, advice and education about the benefits of exercise have been shown not to result in greater exercise capacity in people with COPD.25 Similarly, provision of high-quality evidence-based information to people with COPD resulted in them reading the material without making changes to their disease management.26 Incorporating behaviour change strategies — such as an action plan contract with a general practitioner — has shown short-term benefit in adoption of physical activity in patients with risk factors for coronary heart disease.27 However, it is not known whether this approach would be effective in COPD, where patients' fear of breathlessness is a major limiting factor to exercise participation.28
Study participants identified two major groups of strategies with potential to facilitate referral to PR. The first involved making PR part of standard COPD primary care through financial incentive by extending current legislative and policy frameworks of government subsidisation. In the USA, a Medicare reimbursed benefit for comprehensive PR in patients with moderate to severe COPD was introduced in 2009,29 but it is not yet known how this has affected referral rates. The general practitioners in our study spoke of the introduction of a Medicare subsidy for exercise assessment and supervised exercise sessions in patients with type 2 diabetes introduced in 2007.30 Five years after the introduction of this policy, referral for lifestyle management services was recommended by 82% of Australian general practitioners in a clinical vignette-based survey (n=125) of care of patients with type 2 diabetes.31 Exercise and diet programmes are part of the funded support for patients with diabetes through the universal Medicare programme in Australia, and the data show that referral for modification of diet and exercise behaviour have quickly become part of standard primary care for people with type 2 diabetes following introduction of supporting legislation.
The second major facilitator suggested was improved flow of information regarding referral and services. Participants were aware of the paradox between their need for information about referral pathways and services and the information overload they experienced in a busy practice. A number of the strategies suggested had high potential to integrate referral to PR into workflow through organisational changes and automatic reminders, such as electronic decision support (EDS) systems, academic detailing, single point of referral contact and greater involvement of practice nurses. A systematic review evaluating EDS systems in the management of chronic disease found that just over half of the studies reported improved care processes with some improved patient outcomes.32 However, only four studies in this review included systems to support primary care management of COPD patients, and they did not all incorporate key factors associated with effectiveness.33 Academic detailing has been shown to change prescribing practice34–36 and implementation of non-pharmacological guidelines37 by primary care practitioners, resulting in improved patient outcomes. These two promising interventions could potentially help integrate referral to PR into primary care work practices.
Implications for future research, policy and practice
The findings of this study provide a roadmap for development of interventions to address barriers to change. Having identified barriers and enablers based on a validated theoretical model,11,12 behaviour change techniques can be implemented to address them.38 Specific strategies to integrate PR into the daily workflow of general practitioners are required which address the capability to refer (e.g. a single referral contact accessible electronically at the point of care) and the opportunity to refer (e.g. home-based PR alternatives) which will in turn affect the motivation to refer (e.g. making benefits of PR visible to general practitioners).
While these strategies are transferable, intervention content and modes of delivery need to be developed in a locally relevant, feasible, and cohesive intervention and be appropriately evaluated. This approach has been implemented in a number of studies concerned with changing health professional behaviour to improve quality and safety of healthcare in Australia,39 Canada, and the UK.40
Government subsidisation of PR programmes (through patient rebate for service cost) may increase the number and availability of PR programmes offered in the community. Our data suggest that improved access may facilitate referral. Such change could have a ‘snowball’ effect on referral as greater patient flow through PR programmes provides feedback to general practitioners on the improved outcomes for their patients with COPD.
Conclusions
Referral by general practitioners to PR programmes is a crucial step in achieving implementation of this high-evidence guideline recommendation in the care of people with COPD. Perspectives of study participants indicate that barriers to referral exist at multiple levels, from individual clinicians to local and national healthcare systems. Our findings also point towards appropriate choice of behaviour change techniques for the development of interventions ultimately to help more people with COPD gain access to PR.
Acknowledgments
Handling editor Dianne Goeman
Funding This study was funded by a National Health and Medical Research Council of Australia (NHMRC) Translating Research Into Practice Fellowship awarded to KNJ.
Appendix 1
Footnotes
The authors declare that they have no conflicts of interest in relation to this article.
References
- Bischoff E, Schermer T, Bor H, Brown P, van Weel C, van den Bosch W. Trends in COPD prevalence and exacerbation rates in Dutch primary care. Br J Gen Pract 2009;59:927–33. http://dx.doi.org/10.3399/bjgp09X473079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095–128 http://dx.doi.org/10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management and prevention of COPD. Washington: Medical Communications Resources, 2010. http://www.goldcopd.org/uploads/users/files/GOLDReport_April112011.pdf (accessed 20 Dec 2012). [Google Scholar]
- Toelle BG, Xuan W, Bird TE, et al. Respiratory symptoms and illness in older Australians: the Burden of Obstructive Lung Disease (BOLD) study. Med J Aust 2013;198(3):144–8. http://dx.doi.org/10.5694/mja11.11640. [DOI] [PubMed] [Google Scholar]
- Lacasse Y, Goldstein R, Lasserson T, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2009;4. http://dx.doi.org/10.1002/14651858.CD003793.pub2. [DOI] [PubMed]
- Cecins N, Geelhoed E, Jenkins S. Reduction in hospitalisation following pulmonary rehabilitation in patients with COPD. Aust Health Rev 2008;32(3):415–22. http://dx.doi.org/10.1071/AH080415 [DOI] [PubMed] [Google Scholar]
- Griffiths T, Phillips C, Davies S, Burr M, Campbell I. Cost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programme. Thorax 2001;56:779–84. http://dx.doi.org/10.1136/thorax.56.10.779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston K, Grimmer-Somers K. Pulmonary rehabilitation: overwhelming evidence but lost in translation? Physiotherapy Canada 2010;62:368–73. http://dx.doi.org/10.3138/physio.62.4.368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston CL, Maxwell LJ, Alison JA. Pulmonary rehabilitation in Australia: a national survey. Physiotherapy 2011;97:284–90. http://dx.doi.org/10.1016/j.physio.2010.12.001 [DOI] [PubMed] [Google Scholar]
- Hogg L, Garrod R, Thornton H, McDonnell L, Bellas H, White P. Effectiveness, attendance, and completion of an integrated, system-wide pulmonary rehabilitation service for COPD: prospective observational study. J COPD 2012;9:546–54. http://dx.doi.org/10.3109/15412555.2012.707258 [DOI] [PubMed] [Google Scholar]
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, on behalf of the Psychological Theory Group. Making psychological theory useful for implementing evidence-based practice: a consensus approach. Qual Saf Health Care 2005;14:26–33. http://dx.doi.org/10.1136/qshc.2004.011155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Sci 2012;7(37). http://dx.doi.org/10.1186/1748-5908-7-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo S, Kyngas H. The qualitative content analysis process. J Advan Nursing 2008;62(1):107–15. http://dx.doi.org/10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Hsieh H, Shannon S. Three approaches to qualitative content analysis. Qual Health Res 2005;15(9):1277–88. http://dx.doi.org/10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Johnston K, Grimmer-Somers K, Young M, Antic R, Frith P. Which chronic obstructive pulmonary disease care recommendations have low implementation and why? A pilot study. BMC Res Notes 2012;5(652). http://dx.doi.org/10.1186/1756-0500-5-652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006;18:59–82. http://dx.doi.org/10.1177/1525822X05279903 [Google Scholar]
- Marshall M. Sampling for qualitative research. Fam Pract 1996;13:522–5. http://dx.doi.org/10.1093/fampra/13.6.522 [DOI] [PubMed] [Google Scholar]
- Cabana M, Rand C, Powe N, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999;282(15):1458–65. http://dx.doi.org/10.1001/jama.282.15.1458 [DOI] [PubMed] [Google Scholar]
- Perez X, Wisnivesky J, Lurslurchachai L, Kleinman L, Kronish I. Barriers to adherence to COPD guidelines among primary care providers. Respir Med 2012;106:374–81. http://dx.doi.org/10.1016/j.rmed.2011.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston K, Young M, Grimmer-Somers K, Antic R, Frith P. Why are some evidence-based care recommendations in chronic obstructive pulmonary disease better implemented than others? Perspectives of medical practitioners. Int J COPD 2011;6:659–67. http://dx.doi.org/10.2147/COPD.S26581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris D, Hayter M, Allender S. Factors affecting the offer of pulmonary rehabilitation to patients with chronic obstructive pulmonary disease by primary care professionals: a qualitative study. Prim Health Care Res Dev 2008;8:280–90. http://dx.doi.org/10.1017/S1463423608000832 [Google Scholar]
- Keating A, Lee A, Holland A. Lack of perceived benefit and inadequate transport influence uptake and completion of pulmonary rehabilitation in people with chronic obstructive pulmonary disease: a qualitative study. J Physiother 2011;57:183–90. http://dx.doi.org/10.1016/S1836-9553(11)70040-6 [DOI] [PubMed] [Google Scholar]
- Vieira D, Maltais F, Bourbeau J. Home-based pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med 2010;16:134–43. http://dx.doi.org/10.1097/MCP.0b013e32833642f2 [DOI] [PubMed] [Google Scholar]
- Moy M, Weston N, Wilson E, Hess M, Richardson C. A pilot study of an Internet walking program and pedometer in COPD. Respir Med 2012;106(9):1342–50. http://dx.doi.org/10.1016/j.rmed.2012.06.013 [DOI] [PubMed] [Google Scholar]
- Emery C, Schein R, Hauck E, MacIntyre N. Psychological and cognitive outcomes of a randomized trial of exercise among patients with chronic obstructive pulmonary disease. Health Psychol 1998;17(3):232–40. http://dx.doi.org/10.1037/0278-6133.17.3.232 [DOI] [PubMed] [Google Scholar]
- Harris M, Smith BJ, Veale AJ, Esterman A, Frith PA, Selim P. Providing reviews of evidence to COPD patients: controlled prospective 12-month trial. Chron Respir Dis 2009;6:165–73. http://dx.doi.org/10.1177/1479972309106577 [DOI] [PubMed] [Google Scholar]
- Handley M, MacGregor K, Schillinger D, Shafiri C, Wong S, Bodenheimer T. Using action plans to help primary care patients adopt healthy behaviours: a descriptive study. J Am Board Fam Med 2006;19(3):224–31. http://dx.doi.org/10.3122/jabfm.19.3.224 [DOI] [PubMed] [Google Scholar]
- Harris D, Hayter M, Allender S. Improving the uptake of pulmonary rehabilitation in patients with COPD: qualitative study of experiences and attitudes. Br J Gen Pract 2008;58(555):703–10. http://dx.doi.org/10.3399/bjgp08X342363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Pulmonary Rehabilitation Programs. 4th edn. Champaign, Illinois: Human Kinetics, 2011. [Google Scholar]
- Department of Health and Ageing. Medicare Benefits Schedule Allied Health Services. Government of Australia, Canberra, Australia, 2012. http://www.health.gov.au/internet/mbsonline/publishing.nsf/Content/20953D6469015482CA257A390007D88E/$File/201211-Allied.pdf (accessed 20 Dec 2012). [Google Scholar]
- Jiwa M, Meng X, Sriram D, et al. The management of type 2 diabetes: a survey of Australian general practitioners. Diabetes Res Clin Pract 2012;95:326–32. http://dx.doi.org/10.1016/j.diabres.2011.11.004 [DOI] [PubMed] [Google Scholar]
- Roshanov P, Misra S, Gerstein H, et al. Computerized clinical decision support systems for chronic disease management: a decision maker-researcher partnership systematic review. Implementation Sci 2011;6(92). http://dx.doi.org/10.1186/1748-5908-6-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawamoto K, Houlihan C, Balas E, Lobach D. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 2005;330(7494):765. http://dx.doi.org/10.1136/bmj.38398.500764.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pit S, Byles J, Henry D, Holt L, Hansen V, Bowman D. A Quality Use of Medicines program for general practitioners and older people: a cluster randomised controlled trial. Med J Aust 2007;187(1):23–30. [DOI] [PubMed] [Google Scholar]
- Finkelstein J, Davis R, Dowell S, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics 2001;108(1):1–7. http://dx.doi.org/10.1542/peds.108.1.1 [DOI] [PubMed] [Google Scholar]
- May F, Rowett D, Gilbert A, McNeese J, Hurley E. Outcomes of an educational-outreach service for community medical practitioners: non-steroidal anti-inflammatory drugs. Med J Aust 1999;170:471–4. [PubMed] [Google Scholar]
- Cloutier M, Wakefield D. Translation of a pediatric asthma-management program into a community in Connecticut. Pediatrics 2011;127(1):11–18. http://dx.doi.org/10.1542/peds.2010-1943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Sci 2011;6(42). http://dx.doi.org/10.1186/1748-5908-6-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- French SD, Green SE, O'Connor DA, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implementation Sci 2012;7(38). http://dx.doi.org/10.1186/1748-5908-7-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam R, Tinmouth A, Francis J, et al. A cross-country comparison of intensive care physicians' beliefs about their transfusion behaviour: a qualitative study using the theoretical domains framework. Implementation Sci 2012;7(93). http://dx.doi.org/10.1186/1748-5908-7-93 [DOI] [PMC free article] [PubMed] [Google Scholar]


