Dear Sirs,
Chronic obstructive pulmonary disease (COPD) represents a leading cause of morbidity and mortality in ageing populations.1 However, there is a significant dissociation between guideline recommendations for managing COPD and clinicians’ practice. Several studies have suggested that adoption of the GOLD guidelines has been suboptimal. For the first time, the revised GOLD Guidelines published in 20112 suggest a combined assessment of symptoms, the degree of airflow limitation as measured by spirometry, and the risk of future exacerbation, with patients grouped into four different classes in order to guide therapy.
We therefore conducted a study to compare the regular pharmacological treatment of stable COPD patients in clinical practice with the previous (2010) and current (2011) GOLD guidelines and to investigate whether the new classification of patients improved adherence to GOLD recommendations.
A cohort of 127 consecutively selected patients with stable COPD (122 male, mean age 69.6 ± 8.8years (range: 47–83)) were enrolled in the study. COPD diagnosis was based on global assessment including clinical history and an obstructive spirometry pattern (post-bronchodilator FEV1/FVC ratio <0.70). Initially, the appropriateness and inappropriateness (under- or over-prescription) of pharmacotherapy was established in accordance with the previous GOLD guidelines.3 Afterwards, the study population's treatment was reassessed based on current GOLD recommendations.2 Individuals with a history of upper or lower respiratory tract infection during the previous four weeks, co-existing asthma, cancer or serious uncontrolled disease were excluded from the study. The protocol was approved by the local ethics committee of the University Hospital of Thessaly and all patients provided written informed consent.
A total of 117 patients (92.1%) received bronchodilators. Long-acting antimuscarinic agents (LAMAs) were the most prescribed drugs, being included in the standard therapy of 98 patients (77.1%), and used as monotherapy in 15 patients (11.8%). Long-acting β2-agonists (LABAs) were prescribed in 86 patients (67.7%). Triple therapy (LAMA, LABA and inhaled corticosteroid (ICS)) was used in 57 patients (44.8%) at all stages of the disease.
The patterns (correct, under- and over-treatment) of COPD patients’ treatment in daily practice according to the GOLD 2010 and 2011 recommendations are shown in Table 1. COPD patients with early disease presented higher rates of over-treatment compared to patients with advanced disease according to both versions of the guidelines. Observed adherence to treatment differed from expected in all stages and groups, whereas the differences between groups were marginally statistically significant (p=0.048) only in the case of the 2011 guidelines (Group B differed from the others, exhibiting the lowest adherence percentage of −33%), while no differences between stages were observed in the case of the 2010 guidelines (p=0.0921). However, the combined assessment seemed to benefit more high risk patients, as the percentage dropped to 10.2% and 0% in Groups C and D respectively.
Table 1. Pattern of correct, under- and over-treatment by patient group according to GOLD 2010 and GOLD 2011 recommendations.
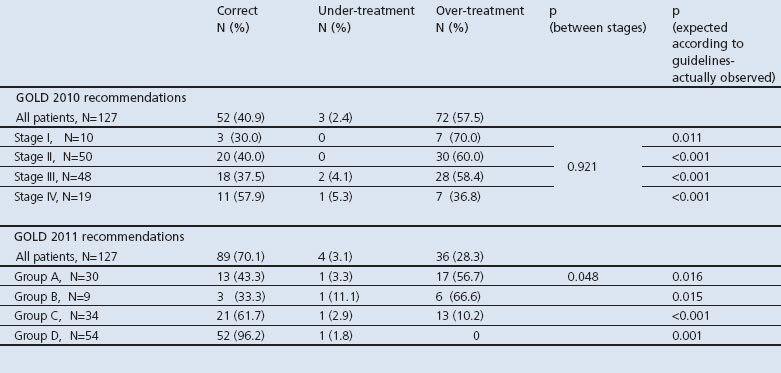
The results of our study show that the rate of adherence to the GOLD guideline has increased from 40.9% with the 2010 version to 70.1% with the 2011 version. Nevertheless, over-treatment remains high in low risk COPD patients.
There are several reasons which might explain the improved adherence to the latest 2011 recommendations. The new categories have led to patients being categorised as having ‘worse’ COPD; consequently, combined medical treatment including ICS as well as LAMAs and LABAs which would have been regarded as over-treatment according to the 2010 guideline is now considered correct according to the 2011 guideline. Moreover, the new guideline includes a wider choice of second choice respiratory medications, so patients previously considered to be over-treated are now treated appropriately; 96.2% of patients in Group D (2011 guidelines) are being treated appropriately as opposed to 57.9% in Stage IV ( 2010 guidelines).
Compliance with the new 2011 guideline is low, despite the appropriate classification of patients and the strategy of early implementation of COPD guidelines. This is not a domestic phenomenon. Recent international research reveals discrepancies between expected and observed treatment regimes: Asche et al. found that 66% of their study population were prescribed medications inconsistent with their spirometry results,4 while other researchers suggest less than optimal adherence with recommended drug therapy treatment for COPD patients based on GOLD guidelines.5–7
The appropriate use of COPD medications is both cost effective and clinically beneficial for patients and stakeholders. Nevertheless, physicians’ knowledge and use of guidelines seems to be insufficient, with deficits in the pharmacological treatment of COPD. Changes in health care systems must include more effective ways to transfer knowledge into clinical practice. High quality education may raise the standards of health care provided for patients with COPD. However, as real life often demands an individualised treatment approach, the contribution of other factors to COPD treatment (co-morbidities, access to health care facilities, patient educational level) also needs to be investigated in the future.
Acknowledgments
Handling editor Paul Stephenson
Funding None.
Footnotes
The authors declare that they have no conflicts of interest in relation to this article.
References
- Minas M, Kostikas K, Papaioannou AI. The association of metabolic syndrome with adipose tissue hormones and insulin resistance in patients with COPD without co-morbidities. COPD 2011;8(6):414–20. http://dx.doi.org/10.3109/15412555.2011.619600 [DOI] [PubMed] [Google Scholar]
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of Chronic Obstructive Lung Disease (revised 2011), www.goldcopd.com.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of Chronic Obstructive Lung Disease (updated 2010), www.goldcopd.com.
- Asche CV, Leader S, Plauschinat C, et al. Adherence to current guidelines for chronic obstructive pulmonary disease (COPD) among patients treated with combination of long-acting bronchodilators or inhaled corticosteroids. Int J Chron Obstruct Pulmon Dis 2012;7:201–09. http://dx.doi.org/10.2147/COPD.S25805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franssen FM, Spruit MA, Wouters EF. Determinants of polypharmacy and compliance with GOLD guidelines in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2011;6:493–501. http://dx.doi.org/10.2147/COPD.S24443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitch K, Iwasaki K, Pyenson B, Plauschinat C, Zhang J. Variation in adherence with Global Initiative for Chronic Obstructive Lung Disease (GOLD) drug therapy guidelines: a retrospective actuarial claims data analysis. Curr Med Res Opin 2011;27(7):1425–9. http://dx.doi.org/10.1185/03007995.2011.583230 [DOI] [PubMed] [Google Scholar]
- Lucas AE, Smeenk FW, Smeele IJ, van Schayck CP. Overtreatment with inhaled corticosteroids and diagnostic problems in primary care patients: an exploratory study. Fam Pract 2008;25(2):86–91. http://dx.doi.org/10.1093/fampra/cmn006 [DOI] [PubMed] [Google Scholar]


