Abstract
The substantial majority of patients with asthma can expect minimal breakthrough symptoms on standard doses of inhaled corticosteroids with or without additional add-on therapies. SIMPLES is a structured primary care approach to the review of a person with uncontrolled asthma which encompasses patient education monitoring, lifestyle and pharmacological management and addressing support needs which will achieve control in most patients. The small group of patients presenting with persistent asthma symptoms despite being prescribed high levels of treatment are often referred to as having ‘difficult asthma’. Some will have difficult, ‘therapy resistant’ asthma, some will have psychosocial problems which make it difficult for them to achieve asthma control and some may prove to have an alternative diagnosis driving their symptoms. A few patients will benefit from referral to a ‘difficult asthma’ clinic. The SIMPLES approach, aligned with close co-operation between primary and specialist care, can identify this patient group, avoid inappropriate escalation of treatment, and streamline clinical assessment and management.
Keywords: difficult asthma, primary care, asthma control
Introduction: the problem of poor asthma control
Asthma has a high prevalence throughout Europe and the industrialised nations, with increasing prevalence in developing economies probably as a consequence of life style changes.1,2 For a variety of (often correctable) reasons many people with asthma do not gain full control of their condition,3 and there are marked variations in outcomes of care between hospitals and between primary care practices.4,5 The only example of a systematic national approach to the management of asthma (in Finland) demonstrated significant patient benefit coupled with large cost savings.6 This programme was based on education of healthcare professionals and promotion of self-management, with the aim of achieving accurate diagnosis and high quality structured management.
The SIMPLES approach to poorly controlled asthma
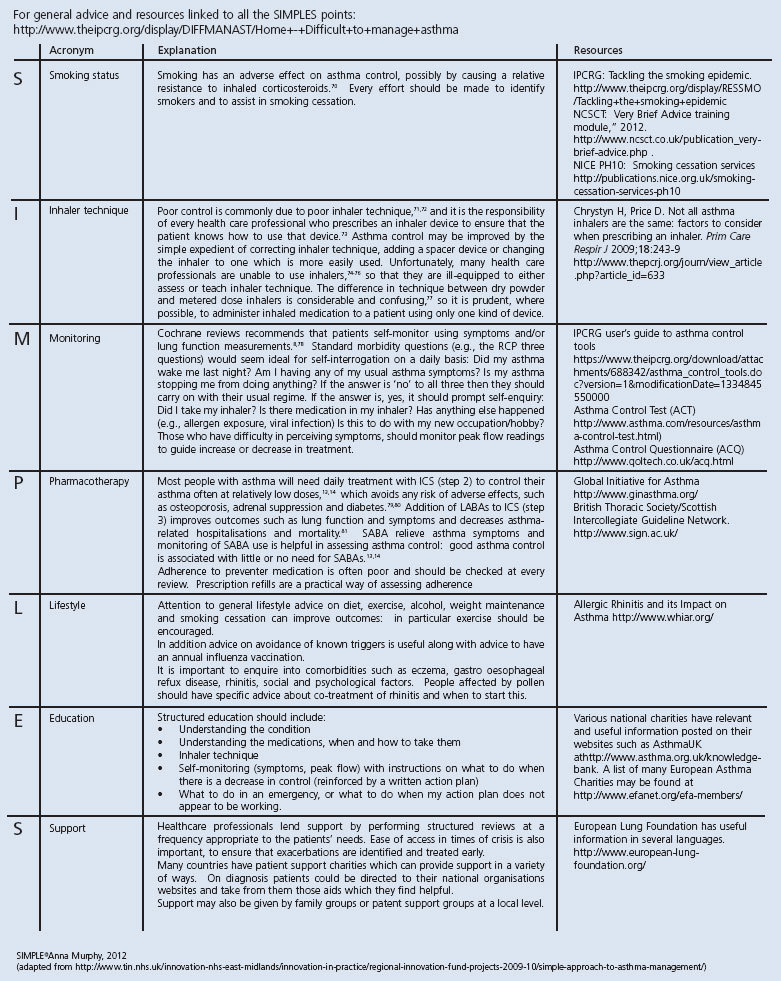
SIMPLES is a structured approach to the review of a person with uncontrolled asthma which encompasses self-management education monitoring, lifestyle and pharmacological management and addressing support needs. See Table 1 for a summary of the components of SIMPLES.
Table 1. The SIMPLES approach to the primary care management of ‘difficult to manage’ asthma.
After a succession of structured reviews over a short time frame, most patients' asthma will have been brought under control. Those who have not achieved control by this process are identified as needing referral to specialist care for further evaluation. Some of these patients will have severe or atypical ‘therapy resistant’ asthma (see the first case study), some will have psychosocial problems which make it difficult for them to achieve asthma control (see the second case study) and some may prove to have an alternative diagnosis driving their symptoms.7 If the diagnosis is in doubt, spirometry performed while the patient is symptomatic should confirm reversible obstruction. Referral for a bronchial challenge test or assessment of airway inflammation may be needed.
Regular review and self-monitoring
Ideally monitoring should be undertaken both by a healthcare professional during regular planned and structured reviews, and by daily self-monitoring (of symptoms and/or peak expiratory flow, as preferred) by the patient. These overlap, of course, as self-monitoring should always be supported by the healthcare team during structured reviews at a frequency appropriate to the patient's needs.8 Ease of access in times of crisis is also important, to ensure that exacerbations are identified and treated early.
In order to self-monitor effectively the patient needs to have an accurate understanding of their condition after receiving education about various aspects of asthma and its management. The literature on self-management education stretches back over some thirty years. The single most consistent finding is that patients who receive structured education and have a written personalised plan have a significant reduction in exacerbations or hospital admissions.8
The advent of telehealth and internet-based applications may help improve outcomes by enabling real-time support for self-monitoring.9 A recent study of self-monitoring using traditional paper charts or recording data on a mobile phone and receiving instantaneous feedback did not demonstrate a difference in control between the groups, though patients in both groups demonstrated a clinically meaningful improvement in asthma control.10 Comprehensive internet-based guided self-management improved asthma control, with more patients achieving a clinically significant improvement than in the usual care group.11 Recently, the utility of mobile phone technology to identify exacerbations of asthma has been demonstrated.12 Improving technology may produce a digital solution which can be used to support patients with ‘difficult to control’ asthma in gaining and maintaining control.
Pharmacotherapy
Asthma guidelines recommend a stepwise approach to the treatment of asthma.13,14 The aim is to achieve and maintain control by stepping up treatment as necessary and stepping down when control is good. A decision to increase treatment should not be made until it has been confirmed that a person can demonstrate optimal inhaler technique, has access to and is taking their treatment as recommended, and is taking adequate measures to avoid allergens and triggers.15 Correcting these factors can often improve asthma control and prevent unnecessary escalation of treatment.16–19
Non-adherence to inhaled corticosteroids (ICS) is a common cause of poor asthma control.20 For many reasons (including lack of understanding of the roles of different forms of therapy, fear of steroids, financial concerns) only 30–70% of patients take preventative therapy as instructed.21 Many patients forget to take one or more doses each day or stop taking their preventative inhaler when they feel better, only to have a recurrence of asthma symptoms a few weeks later. Identification of non-adherence is fundamental to managing apparently refractory disease. Medication adherence can be improved by providing information on treatment, allaying fears, and negotiating with the patient as to how they can take their therapy taking into account their individual lifestyle.18,19
Resources
As part of an initiative on ‘difficult to manage asthma’,22 the International Primary Care Respiratory Group (IPCRG) has produced a desktop helper with the SIMPLES checklist and a number of other tools to support primary health care professionals in their daily practice. This and other useful resources are given in Table 1.
Case study 1. A woman with difficult to manage asthma.
A 40 year old non-smoking woman, working as a teacher, with a history of asthma since she was 25 years old, attends the clinic to request another prescription. Despite taking a moderate/high dose combination inhaler (inhaled steroid + long-acting β2-agonist) which she is requesting regularly, she uses two reliever inhalers a month. She had two exacerbations in the previous year which responded well to oral corticosteroids. Over the years she has tried a leukotriene receptor antagonist, oral long-acting β2-agonist, and theophylline, none of which produced any lasting benefit. Four years ago, spirometry showed moderate obstruction with good reversibility though the post-bronchodilator forced expiratory volume in one second (FEV1) did not return to normal.
Difficult to manage asthma in adults is a challenge.23 Even if this case history is not the most common among asthma patients in primary care practice it is still not unusual. The review of a patient with difficult to manage asthma includes evaluation of several factors: the SIMPLES approach provides a helpful checklist.
Medical history: co-existing conditions
It is important to review the clinical history. The patient is a non-smoker. Does she have any other co-existing conditions or co-morbidities which may have an impact on her asthma control?
Non-steroidal anti-inflammatory drugs and aspirin intolerance are recognised causes of severe asthma and often overlooked. In clinical practice it is not unusual that asthma patients have been prescribed an oral β-blocker for hypertension or ischaemic heart disease, or topical β-blockers for glaucoma which may worsen their asthma.
Cough may be an indicator of gastro-oesophageal reflux, but the relationship between reflux and poorly controlled asthma is not clear.24 Treatment with proton-pump inhibitors does not improve asthma control in patients with asymptomatic reflux.25
It is also important to consider allergic and non-allergic triggers which may worsen her asthma. Asthma and rhinitis frequently coexist and if this patient has symptoms of rhinitis it will be important to treat the rhinitis according to guidelines.26 This is important, as both rhinitis and asthma symptoms could be aggravated by allergies. Allergy testing may help confirm or refute a suspected allergic cause for her poor control.
Another cause which needs to be considered is occupational asthma,27 though this is unlikely in this lady who is a teacher.
Looking for dysfunctional breathing and other conditions such as vocal cord dysfunction and bronchiectasis is also important as they may contribute to asthma-like symptoms.28,29
Monitoring asthma control
Assessing the patient's asthma control is important. There are several tools which are easy to use — for example, the RCP 3 Questions30 — which have been tested in clinical practice.31 Other common validated questionnaires are the Asthma Control Test (ACT) with five questions assessing symptoms over the last four weeks,32 the Asthma Control Questionnaire (ACQ) with seven questions about symptoms in the last week,33 and CARAT, a 10-question test assessing the control of both allergic rhinitis and asthma in the last four weeks.34 In their clinical review in this issue of the PCRJ, Blakey et al. discuss the importance of not only assessing asthma control but also the future risk of asthma attacks.35
In this case, the patient's history of frequent exacerbations and frequent use of relievers not only indicate uncontrolled asthma but also a significant future risk of further exacerbations despite a high treatment level. Self-management education supported by a personalised asthma action plan and an emergency supply of oral steroids is an important aspect of this lady's care.8,13,14
In patients with difficult to manage asthma and persistent exertional breathlessness such as this lady it is important to look for fixed airflow obstruction (usually related to airway remodelling or smoking) which may not be responsive to treatment escalation.36 In this case, the post-bronchodilator FEV1 four years ago could not be reversed to normal suggesting that this might be a problem. Up-to-date spirometry would be helpful to assess any deterioration in fixed airflow obstruction.
Inhaler technique
This patient has uncontrolled asthma despite ‘step 3’ treatment,13,14 and she assures her doctor that she uses her inhalers regularly (although this should be confirmed by assessing the refill prescribing record, as patient report may be unreliable). There is evidence that many patients are unable to use their inhalers correctly, regardless of the device. Poor inhaler technique is associated with poor asthma control.37,38
Guidelines recommend that inhaler technique should be checked in all patients, particularly those with uncontrolled asthma,13,14 and this is highlighted in the SIMPLES tool. Inhaler technique training is a cornerstone in the management of all patients with asthma in order to ensure optimal therapy,39 with a range of different possibilities in the choice of inhaler.40
Pharmacotherapy
Before evaluating whether the patient is treated at the right step to achieve control, the SIMPLES approach recommends discussing both adherence and understanding of the treatment. The teacher in this case had no specific reasons for her poor control so a step-up in treatment should be considered. There are several treatment options at step 4: increasing ICS up to a daily dose of 1,000 μg fluticasone (FP) or equivalent, adding a leukotriene receptor antagonist (LTRA), or treatment with a theophylline.13,14 If a trial of additional treatment is ineffective it is important to stop the add-on treatment or reduce the dose of ICS to previous levels to minimise the risk of systemic side effects. Considering the safety profile of ICS is important. Doses up to 400 μg daily FP or equivalent are regarded as having minimal long-term side effects, whereas patients treated with higher doses of ICS for a longer period or with repeated courses of oral corticosteroids have an increased risk of steroid-related adverse effects.13,14
There is increasing evidence that abnormalities in the small airways may contribute to severity of disease. A recent systematic review showed that small-airways dysfunction was associated with worse asthma control and suggested that treatment with extra-fine particle ICS could improve symptoms and asthma control in those patients with small-airways disease.41 This may be another option for treatment in this lady.
Case study 2. A man who has difficulty managing his asthma.
A 32 year-old man attends for an unscheduled appointment asking for a course of oral corticosteroids and another sick note as his asthma is worse than usual. From his history it is clear that he has had troublesome asthma since childhood. His regular prescription is for a high dose inhaled steroid/long-acting β2-agonist combination inhaler, as well as montelukast, theophylline and a nasal steroid spray. He has also taken citalopram intermittently over the last few years. The prescribing record shows that he has had eight courses of oral corticosteroids in the last year, and he has had three hospital admissions in the last few years. His last routine review at the asthma clinic was six years ago, when it was noted that he was trying to quit smoking.
This man attends frequently for healthcare but when he does he is in crisis and it is often too late for primary care management alone. These emergency visits will inevitably focus on acute management but attempts should also be made to engage him in a follow-up visit in order to work through the reasons for his loss of control. Creating an opportunity for a holistic review should be a key aim, since planned care with a GP when asthma is stable can improve asthma control.42 UK standards now recommend booking a review by a GP within 48 hours of an unplanned asthma event.43 A key component of the review will be the provision of a personalised action plan.
In the presence of such complexity the use of the SIMPLES algorithm can support a comprehensive overview that can be followed up with focused appointments about the identified adherence and precipitating factors.
Smoking cessation
Smoking worsens asthma symptoms, increases exacerbations and hospitalisations and is associated with an increased risk of mortality.44,45 This man has received or is currently receiving pharmacotherapy for conditions known to worsen asthma such as nasal allergy and depression or anxiety, but there is no evidence that he has received smoking cessation medication and this may be a potential blind spot when considering treatment of exacerbating factors. The last recorded smoking status in this patient was six years previously with no record of an intervention to support his quit attempt. This could have been a result of his failure to attend planned care but could also be due to the health professionals' attitudes or beliefs about the effectiveness of smoking cessation in highly addicted smokers who persist despite the effect on their illness.46
Stopping smoking can both decrease the risk of future disease and help improve his current control.47 This man is at risk of fixed airways disease (COPD) because of the combination of poor control and smoking.48 In this (and at every appropriate) general practice consultation we need to provide brief advice using behavioural change techniques. This involves assessing current and past smoking, possibly monitoring carbon monoxide levels, advising on effects of continued smoking, explaining briefly how stop smoking treatments work and then initiating appropriate pharmacotherapy and arranging future support. Patients expect and are happy to be asked this in a healthcare setting.49
One of the benefits of stopping smoking — and an important factor to communicate to this man — is that lower doses of ICS may then be effective. Tobacco smoke inhibits the effect of steroids on airway inflammation so that smokers require escalating doses of ICS, putting them at risk of systemic steroid effects. His combined steroid use from nasal, inhaled and oral routes currently exceeds 1000 μg FP equivalent per day and he should therefore be provided with a steroid card. Whilst working with this man to help him quit smoking there is some evidence that other medicines such as LTRAs, inhaled anticholinergics and LABAs may improve asthma outcomes in smokers.50–53
Lifestyle factors
The SIMPLES checklist reminds us to explore lifestyle factors and for this man there is some evidence that his work may be important. He asks for a sick note at the same time as a crisis. A number of factors may play a part, such as work stress that may be exacerbating anxiety or depression, or he may have specific occupational exposure from which he needs to be removed. Removal from, or reduced exposure to, an occupational trigger should improve control (especially if it is initiated soon after the onset of sensitisation). It is important to balance the clinical benefit against the social or psychological harms that may arise from the risk of unemployment that follows a diagnosis of occupational asthma.54
Psychosocial problems
Depression is associated with difficult asthma and the record of citalopram prescribing suggests he has been treated for this condition. Support for this man therefore needs to be considered from a number of perspectives such as depression, work and smoking. We know that low levels of health-related quality of life in asthma are associated with current or past smoking history, severity of symptoms and absence from work.55 As a clinician it is possible to support him not just through direct medical care but also through signposting to support that may be available locally. This might include a counselling service, a health trainer, online and telephone support from organisations such as patient charities. However, patients may also have personal resources locally that they have not considered using. How can family, friends, neighbours or even work colleagues be utilised to support him? Has he told them what is happening and could you help him consider resources close to home?
Referral to the ‘difficult asthma’ clinic
When should a referral be made?
The substantial majority of patients with asthma can expect minimal breakthrough symptoms on standard doses of ICS therapy with or without additional add-on therapies. In the primary care setting, a ‘red flag’ strategy of proactively identifying and systematically reviewing patients who are prescribed treatment at Step 4 or 5,13,14 particularly those who fail to achieve symptom control or have recurrent ‘exacerbations’, should be applied. This will prevent inappropriate escalation of treatment and identify patients who should be assessed in more detail, both within the primary care setting or with referral to a difficult asthma service.
The small group of patients presenting with persistent asthma symptoms despite being prescribed high levels of treatment are often referred to as having ‘difficult asthma’. A pragmatic definition of difficult asthma is persistent respiratory symptoms despite treatment with a LABA and high dose ICS (≥1000 μg FP equivalent) which equates to people who remain symptomatic at step 4 or requiring treatment at step 5 of guidelines.13,14 It is important to differentiate the term ‘difficult asthma’ from ‘therapy-resistant asthma’ or ‘severe refractory asthma’; these latter terms encompass patients who are relatively treatment resistant and generally require high doses of steroid therapy or additional biological treatments to achieve control, whereas patients with ‘difficult asthma’ often have more therapy-responsive disease but may have different factors which cause them to have persistent symptoms.23,56,57
What can a ‘difficult asthma’ clinic offer?
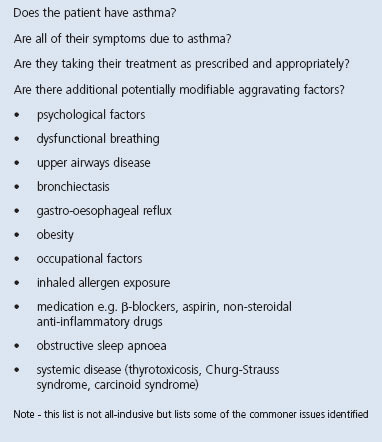
The initial phase of assessment in a ‘difficult asthma’ clinic involves addressing the fundamental issues using a systematic approach, and a series of key questions about accuracy of diagnosis, medication adherence and inhaler technique, and potentially modifiable aggravating factors which should be considered before committing patients to further high dose treatment (see Table 2).
Table 2. Potentially modifiable aggravating factors which should be considered before escalating treatment.
In the ‘difficult asthma’ clinic, these issues are systematically identified and managed by the multi-disciplinary team;23,56,57 this can include trials of therapy along with more detailed investigation such as detailed lung function, high resolution CT scanning, measures of airway inflammation (e.g. induced sputum, exhaled nitric oxide), psychological assessment and management with either medication or clinical psychology input, echocardiography, cardiopulmonary exercise testing, plus other investigations as required. Clinical assessment with spirometry during an episode of worsening symptoms can help to distinguish patients with worsening asthma from other conditions causing increased breathlessness, as this can sometimes be the reason for acute events unresponsive to asthma treatment.
Specific conditions
Specific problems such as vocal cord dysfunction, dysfunctional breathing, and bronchiectasis will be managed with appropriate multi-disciplinary input, along with optimisation of asthma therapy (if appropriate) to try and achieve symptom control.
After thorough evaluation and management, some patients will have ‘refractory asthma’, which is defined as persisting asthma symptoms despite adherence with high dose treatment. These patients often have a propensity to asthma exacerbations, with frequent use of courses of oral corticosteroids despite prescription of add-on therapies e.g. LTRAs or theophylline, and may require maintenance oral corticosteroids.58,59 In general, following systematic evaluation and a detailed assessment, between one-third and a half of patients with ‘difficult asthma’ will have therapy resistant disease, with other diagnoses, co-morbidities, non-adherence or psychosocial factors explaining symptoms in the others.19,56
Therapeutic options
There are a number of therapeutic options available in refractory asthma. For some patients, low dose maintenance oral corticosteroid therapy is well tolerated and effective, but for many, systemic steroid therapy either causes significant side-effects or does not produce disease control, and some patients display steroid insensitivity.
Current therapeutic options for such patients include:
Immunomodulatory corticosteroid-sparing drugs such as methotrexate, cyclosporin and gold. These agents have marked variability in efficacy, may result in significant adverse effects and benefits do not persist after stopping treatment.14 Guidelines recommend that these medications should be reserved for patients who have not responded to usual treatments, and that risks and benefits should be closely monitored.13,14
Omalizumab. This humanised monoclonal antibody reduces free IgE by almost 95% by blocking the binding of IgE to its specific high-affinity receptor.60 Over 50% of patients with refractory asthma have allergic IgE-mediated disease,59 and omalizumab is a therapeutic option for those patients with serum IgE levels in the range 30 to 1500 IU/ml. Anti-IgE therapy is recommended by guidelines for patients at step 513,14 and is administered by subcutaneous injection at 2- or 4-weekly intervals. Due to the high cost of this treatment, different countries have specific criteria to maximise benefit in selected populations of patients. Treatment should be initiated only after specialist assessment, should be monitored closely, and discontinued if it is not beneficial.
Inhaled long acting anti-muscarinic agents (LAMAs). Recent data with tiotropium shows some additional benefit in patients already prescribed LABA/ICS with persistent symptoms and airflow obstruction.61 In the next few years other ultra-long-acting LAMA and LABA preparations will become available and will require evaluation in severe asthma.
Bronchial thermoplasty is a technique that involves the delivery of radio frequency energy to the airways during bronchoscopy with the aim of reducing airway smooth muscle mass and responsiveness in asthma.62 Several studies have demonstrated efficacy and safety for this treatment in selected patients,63 but the degree and duration of benefit, and which patients with severe asthma will benefit most, remain to be clearly established.
Novel biological agents which will target ‘Th2 inflammation’ (elevated interleukin-4, interleukin-5 and interleukin-13) and are likely to be available in the next 2 – 3 years.64–66 Although there is likely to be some overlap with the population suitable for omalizumab, these new therapies are not specifically targeted at allergic disease. A ‘stratified’ approach to severe asthma, which focusses on targeting complex therapies at patients with the appropriate inflammatory phenotype is likely to be a core component of work in the severe asthma clinic in the future.67
Anti-fungal therapy may have a role in patients with chronic allergic bronchopulmonary aspergillosis (ABPA) and other fungally-sensitised severe asthma patients.68,69
How can the primary care physician help support care? — the ideal referral letter…
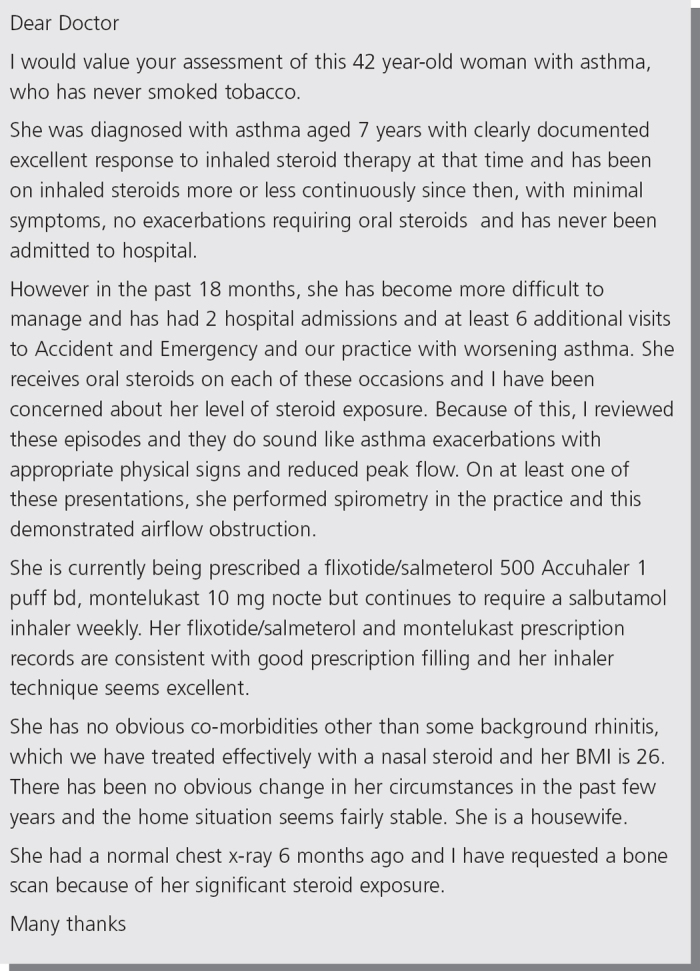
As with many conditions, the assessment and control of patients with difficult asthma can be optimised with a close cohesive partnership between primary and secondary care. Many of the initial questions around diagnosis, adherence and co-morbidity can be addressed in primary care and this detail can be covered in the referral letter. This will provide much of the information required in the initial assessment in the difficult asthma clinic. By way of example, a referral letter with much of the relevant detail is presented in Figure 1.
Figure 1. An exemplar referral letter.
Conclusion
‘Difficult to manage’ asthma is not in itself a diagnosis but is a clinical problem which is clearly defined and which requires detailed assessment as outlined above. The SIMPLES approach, aligned with close co-operation between primary and specialist care, can identify this patient group, avoid inappropriate escalation of treatment, and streamline clinical assessment and management. Some patients will have severe refractory asthma. Novel therapies, many with companion disease biomarkers to allow targeting of these therapies to the correct patient, will be available in the difficult asthma clinic in the coming years.
Acknowledgments
Handling editor Hilary Pinnock
The authors gratefully acknowledge their debt to Hilary Pinnock, the Handling editor, whose encouragement, input and editing was invaluable.
Funding This work received no funding.
Footnotes
DR has no conflicts of interest to declare in relation to this article.
AM has had speaker fees (Almirall, AstraZeneca, Cheisi, GSK, Pfizer, Teva), Advisory Boards (Almirall, Boehringer, Chiesi Ltd, Napp, Novartis) and research funds (Almirall, GSK, Napp)
BS has received honorariums for educational activities and lectures from AstraZeneca, GlaxoSmithKline, Meda, MSD, Nycomed and has served on an advisory board arranged by AstraZeneca, Novartis and Boehringer Ingelheim. NB has no conflicts of interest to declare
LGH has received grant funding from Medimmune, Novartis UK, Genentech Inc, and GlaxoSmithKline, has taken part in Advisory Boards and given lectures at meetings supported by GlaxoSmithKline, Merck Sharpe & Dohme, Nycomed, Boehringer Ingelheim, Napp, Chiesi, Novartis and AstraZeneca. He has received support funding to attend International Respiratory meetings (AstraZeneca, Chiesi, Novartis, Boehringer Ingelheim, Napp and GlaxoSmithKline) and has taken part in asthma clinical trials (GSK, Roche and Genentech) for which his Institution was remunerated. None of these activities have any direct relationship to the content of this manuscript.
References
- Masoli M.Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004;59:469–78. http://dx.doi.org/10.1111/j.1398-9995.2004.00526.x [DOI] [PubMed] [Google Scholar]
- Valovirta E for European Federation of Allergy and Airways Diseases Patients' Associations, EFA Book on Respiratory Allergies. Available from http://www.efanet.org (accessed July 2013)
- Rabe K F, Adachi M, Lai C K W, et al. Worldwide severity and control of asthma in children and adults: the global Asthma Insight and Reality surveys. J Allergy Clin Immunol 2004;114:40–47. http://dx.doi.org/10.1016/j.jaci.2004.04.042 [DOI] [PubMed] [Google Scholar]
- Price D, Horne R, Ryan D, Freeman D, Lee A. Large variations in asthma control between UK general practices participating in the asthma control, concordance and tolerance (ACCT) Initiative. Prim Care Respir J 2006;15:206 (ABS74) [Google Scholar]
- Department of Health. Interactive Health Atlas for Lung conditions in England (INHALE) Avalable from http://www.inhale.nhs.uk (accessed July 2013)
- Haahtela T, Tuomisto LE, Pietinalho A, et al. A 10 year asthma programme in Finland: major change for the better. Thorax 2006;61:663–70. http://dx.doi.org/10.1136/thx.2005.055699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney LG, Robinson DS. Severe asthma treatment: need for characterising patients. Lancet 2005;365:974–976. http://dx.doi.org/10.1016/S0140-6736(05)71087-4 [DOI] [PubMed] [Google Scholar]
- Gibson PG, Powell H, Wilson A, et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database of Systematic Reviews 2002, Issue 3. Art. No.: CD001117. http://dx.doi.org/10.1002/14651858.CD001117 [DOI] [PubMed]
- Pinnock H, Slack R, Pagliari C, Price D, Sheikh A. Understanding the potential role of mobile phone based monitoring on asthma self-management: qualitative study. Clin Exp Allergy 2007;3:794–802. http://dx.doi.org/10.1111/j.1365-2222.2007.02708.x [DOI] [PubMed] [Google Scholar]
- Ryan D, Price D, Musgrave SD, et al. Clinical and cost effectiveness of mobile phone supported self monitoring of asthma: multicentre randomised controlled trial. BMJ 2012;344:e1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Meer V, Bakker M, van den Hout WB, et al. for the SMASHING Study Group. Internet-Based Self-management Plus Education Compared With Usual Care in Asthma: A Randomized Trial. Ann Intern Med 2009;151:110–20. http://dx.doi.org/10.7326/0003-4819-151-2-200907210-00008 [DOI] [PubMed] [Google Scholar]
- Kupczyk M, Haque S, Sterk PJ, et al. Detection of exacerbations in asthma based on electronic diary data: results from the 1-year prospective BIOAIR study. Thorax 2013;68:611–18. http://dx.doi.org/10.1136/thoraxjnl-2012-201815 [DOI] [PubMed] [Google Scholar]
- Global Initiative for Asthma (GINA). The Global Strategy for Asthma Management and Prevention, Updated 2012. Available from: http://www.ginasthma.org (accessed July 2013)
- British Thoracic Society/Scottish Intercollegiate Guidelines Network. British Guideline on the Management of Asthma 2008, Thorax 2008;63(Suppl 4):1–121 Update 2012 available from: http://www.brit-thoracic.org.uk and http://www.sign.ac.uk (accessed July 2013)18156562 [Google Scholar]
- Pinnock H, Fletcher M, Holmes S, et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010;19:75–83. http://dx.doi.org/10.4104/pcrj.2010.00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Jahdali H, Anwar A, Abdullah Al-H, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy, Asthma Clin Immunol 2013;9:8. http://dx.doi.org/10.1186/1710-1492-9-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RJ, Smith BJ, Ruffin RE. Factors associated with hospital admissions and repeat emergency department visits for adults with asthma. Thorax 2000;55:566–573. http://dx.doi.org/10.1136/thorax.55.7.566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews 2008, Issue 2. Art. No.: CD000011. http://dx.doi.org/10.1002/14651858.CD000011.pub3 [DOI] [PubMed]
- Gamble J, Stevenson M, McClean E, Heaney LG. The Prevalence of Non-adherence in Difficult Asthma. Am J Respir Crit Care Med 2009;180:817–22. http://dx.doi.org/10.1164/rccm.200902-0166OC [DOI] [PubMed] [Google Scholar]
- Suissa S, Ernst P, Benayoun S, Baltzan M, Cai B. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med 2000;343:332–6. http://dx.doi.org/10.1056/NEJM200008033430504 [DOI] [PubMed] [Google Scholar]
- Bender B, Milgrom H, Rand C. Non-adherence in asthmatic patients: is there a solution to the problem? Ann Allergy Asthma Immunol 1997;79:177–18. http://dx.doi.org/10.1016/S1081-1206(10)63001-3 [DOI] [PubMed] [Google Scholar]
- International Primary Care Respiratory Group. Difficult to manage asthma. Available from http://www.theipcrg.org/display/DIFFMANAST/Home+-+Difficult+to+manage+asthma (Accessed July 2013)
- Currie GP, Douglas JG, Heaney LG. Difficult to treat asthma in adults. BMJ 2009;338:593–7. http://dx.doi.org/10.1136/bmj.b494 [DOI] [PubMed] [Google Scholar]
- Pacheco-Galván A, Hart SP, Morice AH. Relationship between gastro-oesophageal reflux and airway diseases: the airway reflux paradigm. Arch Bronconeumol 2011;47:195–203. http://dx.doi.org/10.1016/j.arbres.2011.02.001 [DOI] [PubMed] [Google Scholar]
- Mastronarde JG, Anthonisen NR, Castro M, et al. Efficacy of esomeprazole for treatment of poorly controlled asthma. N Engl J Med 2009;360:1487–99. http://dx.doi.org/10.1056/NEJMoa0806290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brozek JL, Bousquet J, Baena-Cagnani CE et al. Global Allergy and Asthma European Network. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol 2010;126:466–76. http://dx.doi.org/10.1016/j.jaci.2010.06.047 [DOI] [PubMed] [Google Scholar]
- Fishwick D, Barber C, Walker S, Scott A. Asthma in the workplace: a case-based discussion and review of current evidence. Prim Care Respir J 2013;22:244–8. http://dx.doi.org/10.4104/pcrj.2013.00038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas M, McKinley RK, Freeman E, Foy C. Prevalence of dysfunctional breathing in patients treated for asthma in primary care: cross sectional survey. BMJ 2001;322:1098–100. http://dx.doi.org/10.1136/bmj.322.7294.1098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bott J, Blumenthal S, Buxton M, et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax 2009;64(Suppl 1):i1–51. http://dx.doi.org/10.1136/thx.2008.110726 [DOI] [PubMed] [Google Scholar]
- Thomas M, Gruffydd-Jones K, Stonham C, Ward S, Macfarlane TV. Assessing asthma control in routine clinical practice: use of the Royal College of Physicians ‘ 3 questions’. Prim Care Respir J 2009;18:83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinnock H, Burton C, Campbell S, et al. Clinical implications of the Royal College of Physicians three questions in routine asthma care: a real-life validation study. Prim Care Respir J 2012;21:288–94. http://dx.doi.org/10.4104/pcrj.2012.00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004;113:59–65. http://dx.doi.org/10.1016/j.jaci.2003.09.008 [DOI] [PubMed] [Google Scholar]
- Juniper EE, Bousquet J, Abetz L, Bateman ED. Identifying ‘well-controlled’ and ‘not well-controlled asthma using the Asthma Control Questionnaire. Respir Med 2006;100:616–21. http://dx.doi.org/10.1016/j.rmed.2005.08.012 [DOI] [PubMed] [Google Scholar]
- Azevedo P, Correia de Sousa J, Bousquet J, et al. in collaboration with the WHO Collaborative Center for Asthma and Rhinitis, Montpellier. Control of Allergic Rhinitis and Asthma Test (CARAT): dissemination and applications in primary care. Prim Care Respir J 2013;22:112–16. http://dx.doi.org/10.4104/pcrj.2013.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakey JD, Woolnough K, Fellows J, Walker S, Thomas M, Pavord ID. Assessing the risk of attack in the management of asthma: a review and proposal for revision of the current control-centred paradigm. Prim Care Respir J 2013;22(3)344–52. http://dx.doi.org/10.4104/pcrj.2013.00063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James AL, Wenzel S. Clinical relevance of airway remodelling in airway diseases. Eur Respir J 2007;30:134–55. http://dx.doi.org/10.1183/09031936.00146905 [DOI] [PubMed] [Google Scholar]
- Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011;105:930–8. http://dx.doi.org/10.1016/j.rmed.2011.01.005 [DOI] [PubMed] [Google Scholar]
- Molimard M, Gros VL. Impact of patient-related factors on asthma control. J Asthma 2008;45:109–13. http://dx.doi.org/10.1080/02770900701815727 [DOI] [PubMed] [Google Scholar]
- Capstick TG, Clifton IJ. Inhaler technique and training in people with chronic obstructive pulmonary disease and asthma. Expert Rev Respir Med 2012;6:91–101. http://dx.doi.org/10.1586/ers.11.89 [DOI] [PubMed] [Google Scholar]
- Chrystyn H, Price D. Not all asthma inhalers are the same: factors to consider when prescribing an inhaler. Prim Care Respir J 2009;18:243–9. http://dx.doi.org/10.4104/pcrj.2009.00029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Wiel E, ten Hacken NH, Postma DS, van den Berge M. Small-airways dysfunction associates with respiratory symptoms and clinical features of asthma: a systematic review. J Allergy Clin Immunol 2013;131:646–57. http://dx.doi.org/10.1016/j.jaci.2012.12.1567 [DOI] [PubMed] [Google Scholar]
- Backer V, Bornemann M, Knudsen D, Ommen H. Scheduled asthma management in general practice generally improve asthma control in those who attend. Respir Med 2012;106:635–41. http://dx.doi.org/10.1016/j.rmed.2012.01.005 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. Quality standard 25, Asthma 2013. Available from http://publications.nice.org.uk (accessed July 2013)
- Ikeue T, Nakagawa A, Furuta K, et al. The prevalence of cigarette smoking among asthmatic adults and association of smoking with emergency department visits. J Japanese Respir Soc 2010;48:99–103. [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ. Asthma and cigarette smoking: a review of the empirical literature. J Asthma 2010;47:345–61. http://dx.doi.org/10.3109/02770900903556413 [DOI] [PubMed] [Google Scholar]
- Self TH, Wallace JL, Gray LA, Usery JB, Finch CK, Deaton PR. Are we failing to document adequate smoking histories? A brief review 1999-2009. Curr Med Res Opin 2010;26:1691–6. http://dx.doi.org/10.1185/03007995.2010.486574 [DOI] [PubMed] [Google Scholar]
- To T, Daly C, Feldman R, McLimont S. Results from a community-based program evaluating the effect of changing smoking status on asthma symptom control. BMC Public Health 2012;12:293. http://dx.doi.org/10.1186/1471-2458-12-293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmsen L, Gottlieb V, Rasmussen LM, Backer V. Asthma patients who smoke have signs of chronic airflow limitation before age 45. J Asthma 2010;47:362–6. http://dx.doi.org/10.3109/02770901003692819 [DOI] [PubMed] [Google Scholar]
- Slama KJ, Redman S, Cockburn J. Community views about the role of general practitioners in disease prevention. Fam Pract 1989;6:203–09. http://dx.doi.org/10.1093/fampra/6.3.203 [DOI] [PubMed] [Google Scholar]
- Brusselle G, Peché R, van den Brande P, Verhulst A, Hollanders W, Bruhwyler J. Real-life effectiveness of extrafine beclometasone dipropionate/formoterol in adults with persistent asthma according to smoking status. Respir Med 2012;106:811–19. http://dx.doi.org/10.1016/j.rmed.2012.01.010 [DOI] [PubMed] [Google Scholar]
- Thomson NC, Spears M. Asthma guidelines and smokers: it's time to be inclusive. Chest 2012;141:286–8. http://dx.doi.org/10.1378/chest.11-1424 [DOI] [PubMed] [Google Scholar]
- Price D, Popov TA, Bjermer L, et al. Effect of montelukast for treatment of asthma in cigarette smokers. J Allergy Clin Immunol 2013;131:763–71. http://dx.doi.org/10.1016/j.jaci.2012.12.673 [DOI] [PubMed] [Google Scholar]
- Ahmad Z, Singh SK. Relative and additional bronchodilator response of salbutamol and ipratropium in smoker and nonsmoker asthmatics. J Asthma 2010;47:340–3. http://dx.doi.org/10.3109/02770900903584456 [DOI] [PubMed] [Google Scholar]
- de Groene GJ, Pal TM, Beach J, et al. Workplace interventions for treatment of occupational asthma. Cochrane Database of Systematic Reviews 2011, Issue 5. Art. No.: CD006308. http://dx.doi.org/10.1002/14651858.CD006308.pub3 [DOI] [PubMed]
- Leander M, Lampa E, Janson C, Svärdsudd K, Uddenfeldt M, Rask-Andersen A. Determinants for a low health-related quality of life in asthmatics. Upsala J Med Sciences 2012;117:57–66. http://dx.doi.org/10.3109/03009734.2011.638730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney LG, Conway E, Kelly C, et al. Predictors of therapy resistant asthma: outcome of a systematic evaluation protocol. Thorax 2003;58:561–56. http://dx.doi.org/10.1136/thorax.58.7.561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson DS, Campbell DA, Durham SR, Pfeffer J, Barnes PJ, Chung KF. Asthma and Allergy Research Group of the National Heart and Lung Institute. Systematic assessment of difficult-to-treat asthma. Eur Respir J 2003;22:478–83. http://dx.doi.org/10.1183/09031936.03.00017003 [DOI] [PubMed] [Google Scholar]
- American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med 2000;162:2341–51. http://dx.doi.org/10.1164/ajrccm.162.6.ats9-00 [DOI] [PubMed] [Google Scholar]
- Bel EH, Sousa A, Fleming L, for U-BIOPRED Consortium, Consensus Generation. Diagnosis and definition of severe refractory asthma: an international consensus statement from the Innovative Medicine Initiative (IMI). Thorax 2011;66:910–17. http://dx.doi.org/10.1136/thx.2010.153643 [DOI] [PubMed] [Google Scholar]
- Hamelmann E. The rationale for treating allergic asthma with anti-IgE. Eur Respir Rev 2007;16:61–6. http://dx.doi.org/10.1183/09059180.00010401 [Google Scholar]
- Kerstjens HA, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med 2012;367:1198–207. http://dx.doi.org/10.1056/NEJMoa1208606 [DOI] [PubMed] [Google Scholar]
- Cox PG, Miller J, Mitzner W, Leff AR. Radiofrequency ablation of airway smooth muscle for sustained treatment of asthma: preliminary investigations. Eur Respir J 2004;24:659–63. http://dx.doi.org/10.1183/09031936.04.00054604 [DOI] [PubMed] [Google Scholar]
- Castro M, Rubin AS, Laviolette M, et al. Effectiveness and Safety of Bronchial Thermoplasty in the Treatment of Severe Asthma: A Multicenter, Randomized, Double-Blind, Sham-Controlled Clinical Trial. Am J Respir Crit Care Med 2010;181:116–24. http://dx.doi.org/10.1164/rccm.200903-0354OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corren J, Lemanske RF, Hanania NA, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med 2011;365:1088–98. http://dx.doi.org/10.1056/NEJMoa1106469 [DOI] [PubMed] [Google Scholar]
- Pavord ID, Korn S, Howarth P, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet 2012;380:651–9. http://dx.doi.org/10.1016/S0140-6736(12)60988-X [DOI] [PubMed] [Google Scholar]
- Wenzel S, Ford L, Pearlman D, et al. Dupilumab in persistent asthma with elevated eosinophil levels. N Engl J Med 2013;368:2455–66. http://dx.doi.org/10.1056/NEJMoa1304048 [DOI] [PubMed] [Google Scholar]
- Holgate ST. Asthma: a simple concept but in reality a complex disease. Eur J Clin Invest 2011;41:1339–52. http://dx.doi.org/10.1111/j.1365-2362.2011.02534.x [DOI] [PubMed] [Google Scholar]
- Wark P, Gibson PG, Wilson A. Azoles for allergic bronchopulmonary aspergillosis associated with asthma. Cochrane Database of Systematic Reviews 2004(3): Art. No.: CD001108. http://dx.doi.org/10.1002/14651858.CD001108.pub2 [DOI] [PMC free article] [PubMed]
- Denning DW, O'Driscoll BR, Powell G, et al. Randomized Controlled Trial of Oral Antifungal Treatment for Severe Asthma with Fungal Sensitization: The Fungal Asthma Sensitization Trial (FAST) Study. Am J Respir Crit Care Med 2009;179:11– 18. http://dx.doi.org/10.1164/rccm.200805-737OC [DOI] [PubMed] [Google Scholar]
- Lazarus SC, Chinchilli VM, Rollings NJ, et al. Smoking affects response to inhaled corticosteroids or leukotriene receptor antagonists in asthma. Am J Respir Crit Care Med 2007;175:783–90. http://dx.doi.org/10.1164/rccm.200511-1746OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J 2002;19:246–51. http://dx.doi.org/10.1183/09031936.02.00218402 [DOI] [PubMed] [Google Scholar]
- Crompton GK, Barnes PJ, Broeders M, et al. The need to improve inhalation technique in Europe: A report from the Aerosol Drug Management Improvement Team. Respir Med 2006;100:1479–94. http://dx.doi.org/10.1016/j.rmed.2006.01.008 [DOI] [PubMed] [Google Scholar]
- Mulloy E, Donaghy D, Quigley C, McNicholas WT. A one-year prospective audit of an asthma education programme in an out-patient setting. Ir Med J 1996;89:226–8. [PubMed] [Google Scholar]
- Plaza V, Sanchis J, Roura P, et al. Physicians' knowledge of inhaler devices and inhalation techniques remains poor in Spain. J Aerosol Med Pulm Drug Deliv 2012;25:16–22. http://dx.doi.org/10.1089/jamp.2011.0895 [DOI] [PubMed] [Google Scholar]
- Hanania NA, Wittman R, Kesten S, Chapman KR. Medical personnel's knowledge of and ability to use inhaling devices. Chest 1994;105:111–16. http://dx.doi.org/10.1378/chest.105.1.111 [DOI] [PubMed] [Google Scholar]
- Plaza V, Sanchis J. Medical personnel and patient skill in the use of metered dose inhalers: a multicentre study. CESEA Group. Respiration 1998;6:195–8. http://dx.doi.org/10.1159/000029259 [DOI] [PubMed] [Google Scholar]
- van der Palen J, Klein JJ, van Herwaarden CL, Zielhuis GA, Seydel ER. Multiple inhalers confuse asthma patients. Eur Respir J 1999;14:1034–7. http://dx.doi.org/10.1183/09031936.99.14510349 [DOI] [PubMed] [Google Scholar]
- Gibson PG, Powell H. Written action plans for asthma: an evidence-based review of the key components. Thorax 2004;59:94–99. http://dx.doi.org/10.1136/thorax.2003.011858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipworth BJ. Systemic adverse effects of inhaled corticosteroid therapy. A systematic review and meta-analysis. Arch Intern Med 1999;159:941–55. http://dx.doi.org/10.1001/archinte.159.9.941 [DOI] [PubMed] [Google Scholar]
- Suissa S, Kezouh A, Ernst P. Inhaled corticosteroids and the risks of diabetes onset and progression. Am J Med 2010;123:1001–06. http://dx.doi.org/10.1016/j.amjmed.2010.06.019 [DOI] [PubMed] [Google Scholar]
- Salpeter MD, Buckley NS, Ormiston TM, Salpeter EE. Meta-Analysis: Effect of Long-Acting β-Agonists on Severe Asthma Exacerbations and Asthma-Related Deaths. Ann Intern Med 2006;144:904–12. http://dx.doi.org/10.7326/0003-4819-144-12-200606200-00126 [DOI] [PubMed] [Google Scholar]


