Abstract
Background:
In practice it is logical that inhalers are prescribed only after patients have received training and demonstrated their ability to use the device. However, many patients are unable to use their pressurised metered-dose inhaler devices (pMDIs) correctly. We assessed the relationship between asthma control and patients' ability to use their prescribed pMDIs.
Methods:
Evaluation of 3,981 (46% male) primary care asthma patient reviews, which included inhaler technique and asthma control, by specialist nurses in primary care in 2009. The paper focuses on people currently prescribed pMDI devices.
Results:
Accurate data on reliever and preventer inhaler prescriptions were available for 3,686 and 2,887 patients, respectively. In patients prescribed reliever inhalers, 2,375 (64%) and 525 (14%) were on pMDI alone or pMDI plus spacer, respectively. For those prescribed preventers, 1,976 (68%) and 171 (6%) were using a pMDI without and with a spacer, respectively. Asthma was controlled in 50% of patients reviewed. The majority of patients (60% of 3,686) were using reliever pMDIs, 13% with spacers. Incorrect pMDI use was associated with poor asthma control (p<0.0001) and more short burst systemic steroid prescriptions in the last year (p=0.038). Of patients using beclometasone (the most frequently prescribed preventer drug in our sample), significantly more of those using a breath-actuated pMDI device (p<0.0001) and a spacer (p<0.0001) were controlled compared with those on pMDIs alone.
Conclusions:
Patients who are able to use pMDIs correctly have better asthma control as defined by the GINA strategy document. Beclometasone via a spacer or breath-actuated device resulted in better asthma control than via a pMDI alone. Patients prescribed pMDIs should be carefully instructed in technique and have their ability to use these devices tested; those unable to use the device should be prescribed a spacer or an alternative device such as one that is breath-actuated.
Keywords: asthma, inhaler technique, asthma control, GINA, pMDI
Introduction
There is evidence that many patients are unable to use their pressurised metered-dose inhaler devices (pMDIs) correctly,1–3 and we confirmed this in a recent study where over 60% of patients were unable to use their pMDI correctly after being shown how on three occasions.4 In practice it is logical that inhalers are prescribed only after patients have received training and demonstrated their ability to use the device. Furthermore, according to UK guidelines5 as well as the Global Strategy for Asthma Management and Prevention (GINA) strategy document,6 inhaler technique should be tested in all patients, particularly those with poorly controlled asthma.3 Age7 and gender2 have also been shown to influence the ability of patients to use their pMDI correctly. It is therefore of concern that a recent analysis of 6 years of sales of inhaler devices revealed that nearly 50% were for pMDIs.8 There is also evidence that poor inhaler technique results in a decreased response to medication9 and poor asthma control,10–12 and that correction of a patient's ability to use their device improves control and compliance.12
The Improving the Management of Patients Asthma and COPD Treatment (IMPACT) service, started in March 2009, works with primary care practices in the UK. It includes a service providing clinical asthma reviews of patients by trained nurses according to protocols agreed with the practices based on the UK National Asthma Guidelines.5 Having agreed protocols, each participating practice invites patients to attend the clinics. At the time of writing, around 400 practices have used the service following introduction to the practice by the visiting Teva UK Ltd pharmaceutical representatives as a non-promotional service.
Data collected systematically during the asthma reviews offer a unique opportunity to evaluate aspects of care, including some of the factors affecting asthma control. As part of our service evaluation of the clinics, we assessed the relationship between asthma control and patients' ability to use their pMDIs. In this paper we describe the relationship between asthma control and aspects of inhaler technique in those prescribed pMDIs for their asthma treatment.
Methods
Practices agreeing to the IMPACT service invited selected patients of theirs to attend for a structured asthma review by nurses trained to diploma level in this field. All patients at British Thoracic Society treatment steps 1 and 2 and, in some cases, step 3 were eligible for their asthma to be reviewed (see Figure 1), irrespective of the patient's level of control. However, subsequent refinement of selection was offered as an option for the practices, based mainly on a number of factors identified by a search of the practice's computerised medical record computer systems using 77 predetermined clinical parameters (including prescribing, particularly of short-acting β2-agonist bronchodilators) and healthcare utilisation data. Patients were also sent asthma control questionnaires — the so called ‘Royal College of Physicians 3-Questions’).13 In most instances all patients from the practice asthma register were invited for review unless, for example, they had been reviewed by the practice in the few weeks prior to initiation of the service.
Figure 1. Flow chart showing process from practice request for service by National Services for Health Improvement (NSHI) to asthma review by trained nurses.
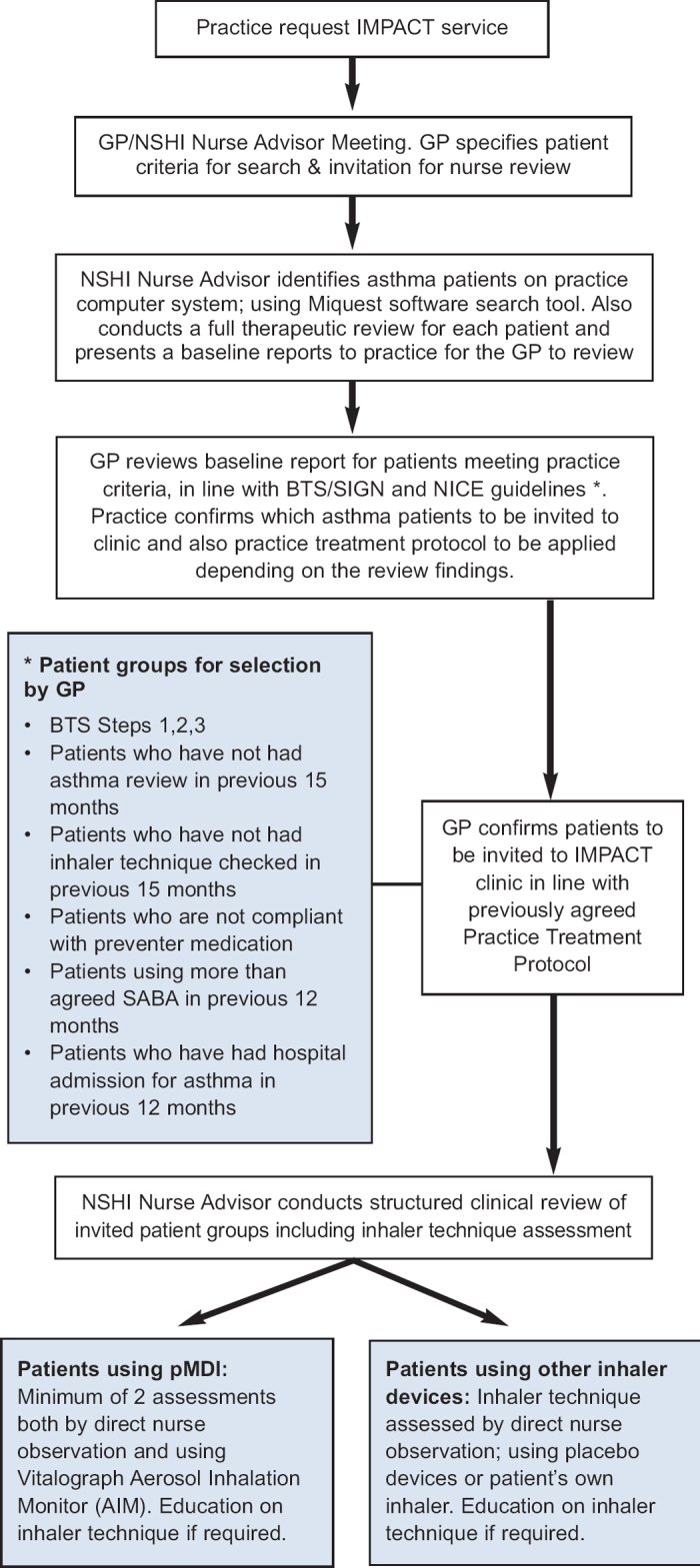
During the asthma review, all patients using pMDIs had at least two assessments both by observation by the nurse and assessment using the Vitalograph Aerosol Inhalation Monitor (AIM),4,14,15 with provision of education on inhaler technique after testing if appropriate. The AIM measures inspiratory flow, ongoing flow, synchronisation, and breath-holding. A colour-coded response indicates the quality of three parameters of the patient's inhaler technique:
Inspiratory flow between 10 and 50L/min: the AIM associates flow with the firing (actuation) of the placebo canister. Firing is acceptable when the canister is depressed while the flow rate is within the acceptable (green) range.
Synchronisation: the green light shows when the patient has achieved the correct flow (i.e. between 10 and 50L/min) for at least 1.5 seconds of the 3 seconds following firing (actuating) the placebo device.
Breath-holding: breath-hold at end of inspiration for at least 5 seconds.
The flowhead (i.e. a ‘dummy’ pMDI) is calibrated to the instrument. All flows have a tolerance of ±5L/min (personal communication, Vitalograph).
All patients previously prescribed and currently using pMDIs had at least two assessments using AIM, with inhaler technique education if appropriate. Visual observation and use of the Clement-Clarke In-Check™ device was used by the nurses in parallel with the AIM assessment. This information was used by the nurses when teaching patients to use their device correctly. Any changes to medication were implemented by the nurses according to the pre-agreed practice protocol. Following clinic assessment, all patients were discussed in detail by the nurses with the patient's GP who decided on future management.
In addition, all patients had their asthma control assessed using the parameters of asthma control described in the GINA strategy,6 which includes the presence of asthma symptoms in the day or night; limitation of activity; use of reliever medication; and lung function in the previous week. This system for assessing asthma control is a working scheme based on current opinion and has not been formally validated. However, this classification has been shown to correlate well with the Asthma Control Test and with assessment of asthma control according to the US National Expert Panel Report 3 guidelines.6
Patients’ asthma was classified as controlled, partly controlled, or uncontrolled using this GINA tool. Controlled asthma is defined according to GINA as follows: <2 episodes of daytime symptoms, <2 episodes of using reliever medication, no night time symptoms, no limitation of activity, and normal lung function in the previous week.6
All information processed was solely for the purpose of carrying out the service and complied fully with the Nursing and Midwifery Council (NMC) Code of Conduct (Nursing Staff),16 ABPI Code of Practice 2008,17 Caldicott Principles,18 and the UK Data Protection Act 1998.19
All identifiable patient data remained in the practice together with any reports generated. As this service was provided by National Services for Health Improvement (NSHI) at the request of and in accordance with agreed practice protocols, ethics approval was not deemed to be necessary.
Data analysis
The results of the inhaler technique testing using the AIM machine were analysed by comparing the success or failure of the test against GINA control using the χ2 statistic using the cross-tabulation function of SPSS V.18 for Mac.
Results
Asthma patient reviews were performed by the IMPACT nurses on 3,981 patients (46% male) in 15 general practices during 2009. The age distribution of these patients was as follows: 806 (20%) <16 years, 1,128 (28%) aged 17–45 years, 1,664 (42%) aged 46–75 years, and 374 (9%) aged >76 years; nine had missing data. Accurate data on reliever and preventer inhaler device prescriptions were available for 3,686 and 2,887 patients, respectively. Reliever devices prescribed included dry powder inhalers (n=316 (9%), comprising Accuhalers, Clickhalers, Diskhalers, Easyhaler, Novolizers, Pulvinal, Turbohalers and Twisthalers) as well as breath-actuated pMDIs (n=469 (13%), comprising Autohaler and Easi-Breathe®). pMDIs alone were prescribed for 2,375 patients (64%) and together with spacers in 525 patients (14%). One patient was on nebulised terbutaline.
Preventer inhaler devices prescribed included dry powder inhalers (n=398 (14%), comprising Accuhalers, Clickhalers, Diskhalers, Easyhalers, Novolizers, Pulvinal, Turbohalers and Twisthalers) as well as breath-actuated devices (n=340 (12%), comprising Autohaler and Easi-Breathe®). pMDIs alone were prescribed for 1,976 patients (68%) and together with spacers in 171 patients (6%). One patient was on nebulised budesonide. Of the available prescribing data, beclometasone dipropionate (BDP) was the most commonly prescribed preventer drug (QVAR® via pMDI and Easi-Breathe®, Clenil® pMDI), comprising 60.2% of the total drugs prescribed for this population. The other 40% of prescriptions for preventer drugs included combination drugs (Seretide™, Symbicort™, and Fostair™), budesonide, fluticasone, and mometasone.
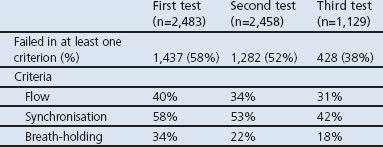
Of the patients who had their inhaler technique tested using the AIM, 58%, 52%, and 38% failed to use the pMDI correctly at the first, second and third tests, respectively. The percentages of patients who failed one or more of the three criteria (flow, synchronisation and breath-holding) for each test are shown in Table 1.
Table 1. Results of the first (before training), second and third Vitalograph Aerosol Inhalation Monitor (AIM) tests after training.
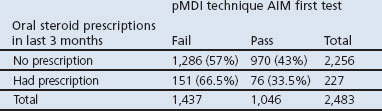
There was a statistically significant association between asthma control and the aspects of inhaler technique tested. Incorrect inhaler use was found in four times as many patients with uncontrolled asthma and over twice as many patients with partly controlled asthma (Table 2, p<0.0001, χ2 value 281.19). Significantly more patients who had one or more asthma exacerbations (68%, p=0.03) failed their first inhaler technique test. Table 3 shows the relationship between previous prescriptions of systemic steroids and inhaler technique: 67% of those prescribed a short course of prednisolone in the previous 3 months (p<0.05; odds ratio (OR) 0.50–0.89) failed their first AIM inhaler technique test when attending the clinic.
Table 2. pMDI technique using the Vitalograph Aerosol Inhalation Monitor (AIM) and GINA control.
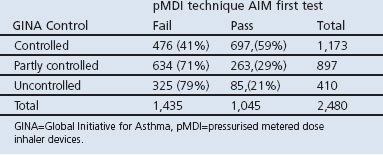
Table 3. First Vitalograph Aerosol Inhalation Monitor (AIM) test and prescription for short courses of oral steroids.
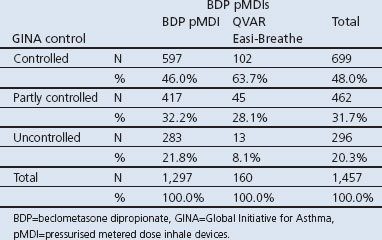
As the most commonly prescribed preventer was BDP, comparisons were made between pMDI with pMDI plus spacer, and BDP pMDIs (Clenil and QVAR) with the breath-actuated BDP QVAR Easi-Breathe inhaler. In patients who were using spacers together with their pMDIs, 68% vs. 51% had better control of their asthma (Table 4, p<0.0001, χ2 value 20.16). Patients using breath-actuated BDP pMDIs (QVAR Easi-Breathe) had significantly better asthma control than those using the same drug via a conventional pMDI (Clenil and QVAR) (Table 5, p<0.0001, χ2 value 23.199).
Table 4. pMDI with and without spacer and GINA control.
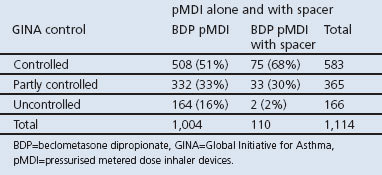
Table 5. GINA control vs BDP pMDI (Clenil and QVAR) vs QVAR Easi-Breathe.
Discussion
Main findings
This real-world service evaluation demonstrated a correlation between patients’ inability to use their prescribed pMDI and poor asthma control. In line with national guidelines, inhaler technique and asthma control were assessed at each review. Nearly 60% of the patients in this population and nearly 80% of those with uncontrolled asthma failed to use their prescribed pMDI device correctly when first tested. The data in Table 3 indicate a strong association between failure to use a pMDI and incidence of asthma exacerbations in the previous year; 66% of those who had exacerbations (i.e. required short courses of oral steroids) were unable to use their pMDIs.
We have also demonstrated that a greater proportion of patients using spacers with their pMDIs have better control than those using pMDIs alone (68% vs. 51%). Furthermore, a greater proportion of patients using breath-actuated pMDIs (QVAR Easi-Breathe) have better control than those using conventional pMDIs (64% vs. 46%). While the numbers of patients in this population using spacers and breath-actuated pMDIs were relatively low, there was a statistically significant difference in the numbers attaining asthma control.
Interpretation of findings in relation to previously published work
While problems have been identified by other researchers in the use of many different types of inhaler devices,20,21 pMDIs are the most commonly prescribed device in the UK so our evaluation focused specifically on aspects of technique related to pMDIs. Cost is the main consideration for UK health service managers in directing prescribing by primary care health professionals. This extremely short-sighted view does not take account of other health economic factors related to asthma such as the healthcare utilisation cost of managing acute asthma attacks and hospitalisations as well as the decreased quality of life and lost productivity for individual patients and their families.
These data support the findings of previously published studies associating poor inhaler handling with adverse outcomes. Bateman and colleagues demonstrated that people with uncontrolled asthma are six times more likely to suffer an exacerbation than those whose asthma is controlled.22 An Italian cross-sectional outpatient study of 1,664 patients with asthma and chronic obstructive pulmonary disease noted an association between inhaler mishandling (dry powder and pMDIs) and increased unscheduled healthcare resource use and poor clinical control.3 Another study involving 915 French general practitioners who observed over 4,000 patients using their pMDIs found an association between poor technique and uncontrolled asthma.11
Studies investigating acute asthma and asthma deaths demonstrate under-prescription of systemic steroids for the fatal attack.23–29 The proportion of patients with poor inhaler technique prescribed systemic steroids shown in Table 3 therefore probably underestimates the true numbers of patients with poor technique who suffer asthma attacks.
Our data strongly support the recommendations in the UK asthma guidelines,5 the international GINA strategy documents,6 as well as the recent NICE Quality Statement 25 on Asthma30 that patients should not be prescribed pMDIs without first checking their ability to use them. Furthermore, if patients cannot use pMDIs, then a spacer or an alternative device that they can use should be prescribed.5,6
Strengths and limitations of this study
One weakness of the study is that it was a retrospective analysis of data collected during provision of an asthma review service for general practices and we did not have a control group of practices. We cannot be sure to what extent those with poor asthma control did not adhere to medical advice or were not treated according to the national guidelines; this is a subject for further research.
We could also be criticised for using the GINA control system; however, in addition to the comments in the Methods section, this classification also correlates well with the Asthma Control Questionnaire (which relates to the previous 7 days).31
This evaluation does not allow for consideration of the relative importance of the three aspects of pMDI inhaler technique (flow, synchronisation, and breath-holding) assessed by the AIM. This may be of importance and for consideration by other researchers; however, as these were objectively measured we believe this composite method is of value.
While there are many aspects of pMDI inhaler technique that patients may get wrong,21 for pragmatic reasons we formally assessed and reported on the three measures tested by the AIM. However, our nurses also observed patients' technique and used the In-Check Dial™ device to evaluate and subsequently base their instructions for patients.
The strength of this study is that the asthma reviews were performed by trained asthma nurses and included a very large multicentre dataset representative of general practice patient populations in the UK. Practices selected which patients were invited to attend clinics, and many of these had previously unrecognised poorly controlled asthma; they were appropriately provided with a quality review by a trained asthma nurse.
Implications for future research, policy and practice
Given the relationship we have demonstrated between poor inhaler technique and asthma control, there is a clear need for clinicians to ensure patients are able to use their inhalers correctly. A number of studies have demonstrated various methods for achieving this goal. Examples include teaching patients during a hospital admission,32 opportunistically on repeated outpatient attendance,33 or when collecting medication from a pharmacist trained in teaching inhaler technique.34 Actively demonstrating the technique with patients showing their ability seems to work better than simply telling patients or providing a leaflet on how to use their device.34,35
Future research involving patients being treated in primary care should include inhaler device usage focused on technical ability in both control and intervention group patients. This research should attempt to identify factors such as age, gender, and the degree to which asthma control is determined by inhaler technique.
We have demonstrated an association between poor pMDI inhaler technique and poor asthma control. Not many studies have done this, so we have highlighted the importance and emphasised the need to check inhaler technique and to take appropriate action to either improve this through education or prescribe a different device. Furthermore, all patients with asthma should have their inhaler technique checked at initial prescription and at every opportunity when consulting.
Conclusions
Patients who are able to use pMDIs correctly have better asthma control as defined by the GINA strategy document. BDP via a spacer or a breath-actuated device resulted in better asthma control than via a pMDI alone. Patients prescribed pMDIs should be carefully instructed in technique and have their ability to use these devices tested; those unable to use the device should be prescribed a spacer or an alternative device such as one that is breath-actuated.
Acknowledgments
Handling editor Björn Ställberg
Statistical review Gopal Netuveli
Funding The IMPACT Service is provided by National Services for Health Improvement (NSHI) and is sponsored by Teva UK Ltd.
Footnotes
EM and AH are both employees of National Services for Health Improvement (NSHI). JH is an employee of Teva UK Limited, Harlow, Essex. MLL has accepted sponsorship from GlaxoSmithKline (GSK), AstraZeneca (AZ), Boehringer Ingelheim (BI), Chiesi, Merck Sharpe and Dohme (MSD), Merck, Altana Pharma, Novartis, Meda Pharmaceuticals, 3M Pharmaceuticals, Napp Pharmaceuticals and Schering Plough for attending conferences. He has accepted lecture fees from BI, GSK, AZ, Chiesi and Alk-Abello. He has been on advisory boards or provided consultancy for GSK, Schering Plough, MSD, Chiesi, Altana Pharma, Ranbaxy, AZ, Clement Clarke International, National Services for Health Improvement (NSHI) and Novartis. He has had research grants from BI, Pfizer and GSK. He is a member of The Aerosol Drug Management Improvement Team (ADMIT) which is supported by an unrestricted educational grant from Consorzio Ferrara Ricerche. MLL is the Editor Emeritus of the PCRJ, but was not involved in the editorial review of, nor the decision to publish, this article.
References
- Crompton GK. Problems patients have using pressurized aerosol inhalers. Eur J Respir Dis 1982;63(Suppl 119):101–4. [PubMed] [Google Scholar]
- Goodman DE, Israel E, Rosenberg M, Johnston R, Weiss ST, Drazen JM. The influence of age, diagnosis, and gender on proper use of metered-dose inhalers. Am J Respir Crit Care Med 1994;150(5 Pt 1):1256–61. http://dx.doi.org/10.1164/ajrccm.150.5.7952549 [DOI] [PubMed] [Google Scholar]
- Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011;105(6):930–8. http://dx.doi.org/10.1016/j.rmed.2011.01.005 [DOI] [PubMed] [Google Scholar]
- Hardwell A, Barber V, Hargadon T, McKnight E, Holmes J, Levy ML. Technique training does not improve the ability of most patients to use pressurised metered-dose inhalers (pMDIs). Prim Care Respir J 2011;20(1):92–6. http://dx.doi.org/10.4104/pcrj.2010.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Thoracic Society, Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. Thorax 2008;63(Suppl 4):iv1–121. Available from: http://www.sign.ac.uk/guidelines/fulltext/101/index.html http://dx.doi.org/10.1136/thx.2008.097741 [DOI] [PubMed] [Google Scholar]
- Global Initiative for Asthma (GINA). The global strategy for asthma management and prevention. Updated 2012. Available from: http://www.ginasthma.org.
- Van Beerendonk I, Mesters I, Mudde AN, Tan TD. Assessment of the inhalation technique in outpatients with asthma or chronic obstructive pulmonary disease using a metered-dose inhaler or dry powder device. J Asthma 1998;35(3):273–9. http://dx.doi.org/10.3109/02770909809068218 [DOI] [PubMed] [Google Scholar]
- Lavorini F, Corrigan CJ, Barnes PJ, et al. Retail sales of inhalation devices in European countries: so much for a global policy. Respir Med 2011;105(7):1099–103. http://dx.doi.org/10.1016/j.rmed.2011.03.012 [DOI] [PubMed] [Google Scholar]
- Lindgren S, Bake B, Larsson S. Clinical consequences of inadequate inhalation technique in asthma therapy. Eur J Respir Dis 1987;70(2):93–8. [PubMed] [Google Scholar]
- Molimard M, Gros VL. Impact of patient-related factors on asthma control. J Asthma 2008;45(2):109–13. http://dx.doi.org/10.1080/02770900701815727 [DOI] [PubMed] [Google Scholar]
- Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J 2002;19(2):246–51. http://dx.doi.org/10.1183/09031936.02.00218402 [DOI] [PubMed] [Google Scholar]
- Giraud V, Allaert FA. Improved asthma control with breath-actuated pressurized Metered Dose Inhaler (pMDI): The SYSTER survey. Eur Rev Med Pharmacol Sci 2009;13(5):323–30. [PubMed] [Google Scholar]
- Pearson MG, Bucknall CE, eds. Measuring clinical outcome in asthma: a patient focused approach. London: Royal College of Physicians Clinical Effectiveness and Evaluation Unit, 1999. [Google Scholar]
- Sarvis CA, Tice AL, Plake KS. Evaluation of inhaler technique using the aerosol inhalation monitor. J Pharmacy Pract 2004;17(4):275–9. http://dx.doi.org/10.1177/0897190004270027 [Google Scholar]
- Lavorini F, Levy ML, Corrigan C, Crompton G. The ADMIT series: issues in inhalation therapy. 6) Training tools for inhalation devices. Prim Care Respir J 2010;19(4):335–41. http://dx.doi.org/10.4104/pcrj.2010.00065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nursing and Midwifery Council. Standards of conduct, performance and ethics for nurses and midwives. Available from: http://www.nmc-uk.org/aArticle.aspx?ArticleID=3056.
- Association of the British Pharmaceutical Industry (ABPI) Code of Practice. Available from: http://www.abpi.org.uk/publications/pdfs/pmpca_code2008.pdf.
- Caldicott Committee. Report on the Review of Patient-Identifiable Information. 1997 Available from: http://www.wales.nhs.uk/sites3/Documents/783/DH%5F4068404%5B1%5D.pdf.
- UK Data Protection Act. 1998 (last accessed 4 April 2010). Available from: http://www.opsi.gov.uk/acts/acts1998/ukpga_19980029_en_1.
- Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol 2007;119(6):1537–8. http://dx.doi.org/10.1016/j.jaci.2007.02.037 [DOI] [PubMed] [Google Scholar]
- Sanchis J, Corrigan C, Levy ML, Viejo JL. Inhaler devices — from theory to practice. Respir Med 2013;107(4):495–502. http://dx.doi.org/10.1016/j.rmed.2012.12.007 [DOI] [PubMed] [Google Scholar]
- Bateman ED, Reddel HK, Eriksson G, et al. Overall asthma control: the relationship between current control and future risk. J Allergy Clin Immunol 2010;125(3):600–8.e6. http://dx.doi.org/10.1016/j.jaci.2009.11.033 [DOI] [PubMed] [Google Scholar]
- British Thoracic Association. Death from asthma in two regions. BMJ 1982;285:1251–5. http://dx.doi.org/10.1136/bmj.285.6350.1251 [PMC free article] [PubMed] [Google Scholar]
- Anagnostou K, Harrison B, Iles R, Nasser S. Risk factors for childhood asthma deaths from the UK Eastern Region Confidential Enquiry 2001–2006. Prim Care Respir J 2012;21(1):71–7. http://dx.doi.org/10.4104/pcrj.2011.00097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson P, Shields M. Asthma deaths: we need to identify risk factors early and construct at-risk asthma registers. Prim Care Respir J 2012;21(1):13–14. http://dx.doi.org/10.4104/pcrj.2012.00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturdy PM, Butland BK, Anderson HR, et al. Deaths certified as asthma and use of medical services: a national case-control study. Thorax 2005;60(11):909–15. http://dx.doi.org/10.1136/thx.2004.025593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher HJ, Ibrahim SA, Speight N. Survey of asthma deaths in the Northern region, 1970–85 [see comments]. Arch Dis Child 1990;65(2):163–7. http://dx.doi.org/10.1136/adc.65.2.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson CF, Rubinfield AR, Bowes G. Deaths from asthma in Victoria: a 12 month survey. Med J Aust 1990;152:511–17. [DOI] [PubMed] [Google Scholar]
- Bucknall CE, Slack R, Godley CC, Mackay TW, Wright SC. Scottish Confidential Inquiry into Asthma Deaths (SCIAD), 1994–6. Thorax 1999;54(11):978–84. http://dx.doi.org/10.1136/thx.54.11.978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence (NICE). Quality Statement 25: Asthma. Available from: http://publications.nice.org.uk/quality-standard-for-asthma-qs25/list-of-quality-statements (accessed 1 July 2013).
- O'Byrne PM, Reddel HK, Eriksson G, et al. Measuring asthma control: a comparison of three classification systems. Eur Respir J 2010;36:269–76. http://dx.doi.org/10.1183/09031936.00124009 [DOI] [PubMed] [Google Scholar]
- Press VG, Arora VM, Shah LM, et al. Teaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trial. J Gen Intern Med 2012;27(10):1317–25. http://dx.doi.org/10.1007/s11606-012-2090-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takemura M, Kobayashi M, Kimura K, et al. Repeated instruction on inhalation technique improves adherence to the therapeutic regimen in asthma. J Asthma 2010;47(2):202–08. http://dx.doi.org/10.3109/02770900903581692 [DOI] [PubMed] [Google Scholar]
- Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma 2010;47:251–6. http://dx.doi.org/10.3109/02770900903580843 [DOI] [PubMed] [Google Scholar]
- Gorifl S, Taflci S, Elmali F. The effects of training on inhaler technique and quality of life in patients with COPD. J Aerosol Med Pulm Drug Deliv 2013. Feb 19 [Epub ahead of print]. http://dx.doi.org/10.1089/jamp.2012.1017 [DOI] [PubMed]


