Abstract
Pheochromocytomas are rare catecholamine-producing neuroendocrine tumors that can lead to detrimental outcomes; if identified and treated, they are associated with a good prognosis. The clinical presentation can vary greatly but is classically associated with tachycardia, headaches, and hypertension. Bradyarrhythmias and sinus node dysfunction are uncommon complications of this condition. We present a case of pheochromocytoma associated with sinus pauses and junctional escape rhythms that had complete resolution of sinus node dysfunction after adrenalectomy.
Keywords: Catecholamine, junctional escape rhythms, pheochromocytoma, sick sinus syndrome, sinus arrest, sinus node dysfunction
Pheochromocytomas are rare tumors reported in 0.2% of hypertensive patients and, if unidentified, can lead to fatal outcomes.1,2 Symptoms result from excessive catecholamine secretion by the tumor and are classically associated with palpitations, headache, and diaphoresis. However, most patients present with varied symptoms that are often missed, making the diagnosis more challenging.3,4 More commonly reported cardiovascular signs include tachyarrhythmias, myocardial infarction, and cardiomyopathy; less common presentations include sinus pauses and atrioventricular dissociations.5–8 We present a patient with sinus node dysfunction caused by a pheochromocytoma.
CASE REPORT
A 56-year-old white woman, who had enjoyed good health until about 2 years before presentation, began having anxiety and hot flashes associated with palpitations, which she attributed to perimenopause and social stressors. About that time, she was diagnosed with hypertension after presenting to an emergency department with a severe occipital headache. Her blood pressure (BP) was 203/74 mm Hg. After initiation of metoprolol and felodipine by her primary care physician, her symptoms resolved and BP was well controlled for several months. Unfortunately, in the 3 months before her presentation to the authors’ clinic, severe headaches, palpitations, and hot flashes reappeared. She also noticed sporadic elevated home BP readings with systolic BP frequently >180 mm Hg.
On examination, she was anxious but not ill appearing. Her BP was 118/75 mm Hg, heart rate was 72 beats per minute, and respirations were 16 breaths per minute. Comprehensive metabolic panel, complete blood count, and thyroid-stimulating hormone results were within normal limits. A previous electrocardiogram showed normal sinus rhythm with incomplete right bundle branch block, and the previous echocardiogram was unremarkable. A 48-hour Holter monitor revealed sinus pauses and junctional escape rhythms. Metoprolol was then held for a week but she remained symptomatic. A repeat 48-hour Holter monitor off the medication redemonstrated sinus pauses and junctional escape rhythms.
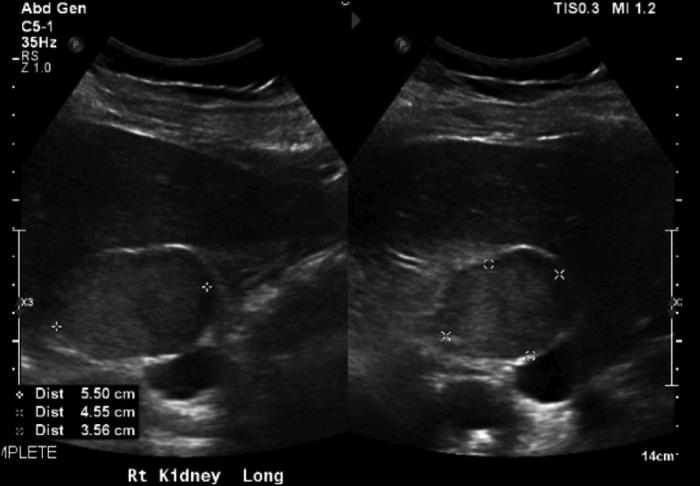
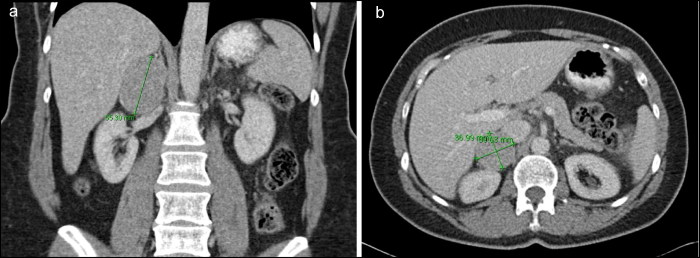
Renal ultrasound revealed a 5.5-cm soft tissue lesion near the superior medial aspect of the right kidney without evidence of renal artery stenosis (Figure 1). Computed tomography of the abdomen showed a 3.7 × 4.0 × 5.5 cm right adrenal lesion that corresponded to renal ultrasound findings (Figure 2). Enhancement washout characteristics were not consistent with adenoma, so biochemical studies were obtained. Studies revealed elevated levels of serum metanephrine, 6.30 nmol/L (normal <0.50 nmol/L); serum normetanephrine, 16 nmol/L (normal <0.90 nmol/L); 24-hour urine norepinephrine, 298 µg/24 h (normal 16–71 µg/24 h); 24-hour urine epinephrine, 124 µg/24 h (normal 1–7 µg/24 h); and 24-hour urine metanephrine, 6365 mcg/24 h (normal 30–180 mcg/24 h), confirming the diagnosis of pheochromocytoma. She was referred for endocrine surgery, started on phenoxybenzamine, and underwent a successful uncomplicated laparoscopic adrenalectomy of the right adenoma. Pathology confirmed a benign tumor (pheochromocytoma of the adrenal gland, scaled score of 2) with clear surgical margins.
Figure 1.
Doppler renal ultrasound revealing a 5.5-cm soft tissue lesion near the superomedial aspect of the right kidney.
Figure 2.
Computed tomography of the abdomen with contrast: (a) coronal plane, revealing a right adrenal lesion measuring up to 5.5 cm, and (b) transverse plane, revealing right adrenal lesion measuring 3.7 × 4.0 × 5.5 cm.
One month later, she reported complete and near-immediate resolution of all of her symptoms. Serial BP monitoring demonstrated sustained normotension while not taking any antihypertensive medications. Repeat serum metanephrine of <20 nmol/L (normal <0.50 nmol/L) and serum normetanephrine of 0.4 nmol/L (normal <0.90 nmol/L) were within normal limits. A repeat 48-hour Holter monitor 2 months postoperatively did not show any evidence of sinus node dysfunction.
Discussion
Pheochromocytoma is a rare neuroendocrine tumor reported in 0.2% of hypertensive patients.1 Symptoms result from the release of various catecholamines. The adrenal medulla predominantly releases epinephrine. However, most pheochromocytomas predominantly release norepinephrine, which stimulates alpha-1 and beta-1 receptors and results in vasoconstriction and positive chronotropic, dromotropic, and inotropic effects. Although commonly associated with hypertension and tachyarrhythmia, ectopic atrial and ventricular beats, episodic nodal rhythms, and abrupt changes in sinus interval have been reported during norepinephrine infusions.9 Proposed mechanisms include increased vagal discharge by the baroreceptor reflex in response to sudden increasing atrial pressure and subsequent adrenergic receptor desensitization leading to bradycardia, but this is more often seen in patients with elevated epinephrine vs norepinephrine levels.5,8
Sinus node dysfunction is an uncommon presentation of this disease, with only four other published case reports.8–11 Notably, symptoms and arrhythmia resolved after the resection of the tumor in all four cases. In our patient, her initial presentation of episodic hypertension and hot flashes may have been confounded by perimenopause. Hypertension, which occurs in 46% of adults in the United States, would not typically prompt workup of an uncommon disease.7 However, the persistent paroxysmal presentation of symptoms may be an important indicator to warrant further investigation.12
References
- 1.Pacak K, Linehan WM, Eisenhofer G, Walther MM, Goldstein DS. Recent advances in genetics, diagnosis, localization, and treatment of pheochromocytoma. Ann Intern Med. 2001;134:315–329. doi: 10.7326/0003-4819-134-4-200102200-00016. [DOI] [PubMed] [Google Scholar]
- 2.Khorram-Manesh A, Ahlman H, Nilsson O, Odén A, Jansson S. Mortality associated with pheochromocytoma in a large Swedish cohort. Eur J Surg Oncol. 2004;30:556–559. doi: 10.1016/j.ejso.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Baguet JP, Hammer L, Mazzuco TL, et al. Circumstances of discovery of phaeochromocytoma: a retrospective study of 41 consecutive patients. Eur J Endocrinol. 2004;150(5):681–686. [DOI] [PubMed] [Google Scholar]
- 4.Sutton MG, Sheps SG, Lie JT. Prevalence of clinically unsuspected pheochromocytoma. Review of a 50-year autopsy series. Mayo Clin Proc. 1981;56(6):354–360. [PubMed] [Google Scholar]
- 5.Berra E, Gonzalez MC, Scavée C, et al. High prevalence of cardiac electric abnormalities in patients with phaeochromocytomas. J Hypertens. 2017;35(4):899–901. doi: 10.1097/HJH.0000000000001236. [DOI] [PubMed] [Google Scholar]
- 6.Espersen T, Jorgensen J. Electrocardiographic changes in paroxysmal hypertension due to chromaffin adrenal tumor. Act Med Scandinav. 2009;127(5):494–500. doi: 10.1111/j.0954-6820.1947.tb13163.x. [DOI] [PubMed] [Google Scholar]
- 7.Tulppo MP, Mäkikallio TH, Seppänen T, Airaksinen JK, Huikuri HV. Heart rate dynamics during accentuated sympathovagal interaction. Am J Physiol Heart Circ Physiol. 1998;274(3):H810–H816. doi: 10.1152/ajpheart.1998.274.3.H810. [DOI] [PubMed] [Google Scholar]
- 8.Forde TP, Yormak SS, Killip T 3rd. Reflex bradycardia and nodal escape rhythm in pheochromocytoma. Am Heart J. 1968;76(3):388–392. doi: 10.1016/0002-8703(68)90235-4. [DOI] [PubMed] [Google Scholar]
- 9.Mulder NH. Bradycardia in a patient with pheochromocytoma [in Dutch]. Ned Tijdschr Geneeskd. 1975;119:267–272. [PubMed] [Google Scholar]
- 10.Bruch C, Dagres N, Wieneke H, Herborn C, Brandt-Mainz K, Erbel R. Sinus node dysfunction with intermittent sinus arrest and AV-nodal escape rhythm as initial manifestation of pheochromocytoma [in German]. Z Kardiol. 2002;91(1):81–87. doi: 10.1007/s392-002-8376-8. [DOI] [PubMed] [Google Scholar]
- 11.Zweiker R, Tiemann M, Eber B, et al. Bradydysrhythmia-related presynope secondary to pheochromocytoma. J Intern Med. 1997;242(3):249–253. doi: 10.1046/j.1365-2796.1997.00198.x. [DOI] [PubMed] [Google Scholar]
- 12.Lenders JW, Duh QY, Eisenhofer G, et al; Endocrine Society . Pheochromocytoma and paraganglioma: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2014;99(6):1915–1942. doi: 10.1210/jc.2014-1498. [DOI] [PubMed] [Google Scholar]