Abstract
We present the case of a 55-year-old black man with coccidiomycosis presenting as a cutaneous plaque on the upper lip. Coccidiomycosis, or “valley fever,” is caused by the virulent, dimorphic, soil-dwelling fungus Coccidiodes immitis. Seen in up to 50% of symptomatic patients, skin involvement by coccidiomycosis can present as papules, pustules, plaques, nodules, abscesses, or ulcerations. Diagnosis of coccidiomycosis relies on serology and identification in clinical specimens, and first-line treatment includes fluconazole, ketoconazole, or itraconazole. Recognizing the cutaneous manifestations of this mycotic infection is essential for diagnosis in otherwise asymptomatic patients.
Keywords: Coccidiomycosis, fungus, infection, skin lesion
Coccidiomycosis, or “valley fever,” is caused by the virulent, dimorphic, soil-dwelling fungus Coccidiodes immitis. Endemic areas include the southwestern USA, northern Mexico, and Central and South America. Infection typically occurs via inhalation of arthroconidia and most commonly results in pulmonary disease.1–6 Presenting symptoms can include cough, fever, and arthralgias, although up to 60% of patients are asymptomatic. Disseminated disease occurs in up to 5% of patients.5–7 Filipinos, blacks, pregnant women, and immunosuppressed patients are at increased risk for developing widespread disease.1–6 Skin involvement by coccidiomycosis can present as papules, pustules, plaques, nodules, abscesses, or ulcerations and is seen in up to 50% of symptomatic patients.2–4,6,8,9 In addition, coccidiomycosis can cause hypersensitivity reactions such as erythema nodosum and erythema multiforme.2–4,9 Though any anatomical site may be affected, the head and neck are most commonly affected.3,6 Cutaneous involvement most often results from disseminated disease. Here, we present a patient with coccidiomycosis presenting with a facial plaque.
Case description
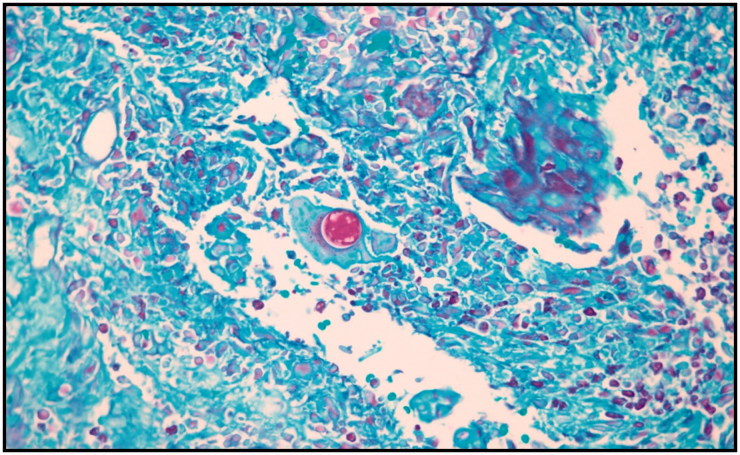
A 55-year-old black man presented with a 15-day history of a growth on his upper lip. Pustules coalescing into a mildly tender pink-tan plaque were present on the right upper lip with focal areas of yellow-brown scale and crust (Figure 1). No cervical or axillary lymphadenopathy was noted. A previous superficial skin swab a week earlier demonstrated Enterobacter aeruginosa, and he had been treated with a course of trimethoprim-sulfamethoxazole with little improvement. He had traveled to Texas, California, and New Mexico. There was no history of human immunodeficiency virus, immunosuppression, or trauma to the area. Five months before presentation in our clinic, he was hospitalized for pneumonia and peripheral eosinophilia, both of which improved with antibiotics. Bronchoscopy was unremarkable. Two punch biopsies demonstrated spherules in the dermis with an inflammatory infiltrate indicative of coccidiomycosis (Figure 2). Our patient is improving on fluconazole 600 mg three times a day with a planned treatment course of 1 year.
Figure 1.
A pink-tan plaque with yellow-brown scale and crust on the patient’s right upper lip.
Figure 2.
Skin biopsy from the right upper lip demonstrating a large endospore-containing spherule with surrounding granulomatous infiltrate in the dermis (periodic acid Schiff, ×200).
Discussion
An infectious etiology should be included in the differential for skin lesions refractory to conventional antibiotics, especially in endemic areas or in immunosuppressed patients. Skin involvement in coccidiomycosis may present with a spectrum of lesional morphology. Cutaneous findings are commonly secondary to hematogenous dissemination of organisms from a pulmonary focus, although reactive conditions such as erythema multiforme, erythema nodosum, and Sweet’s syndrome are well documented.3,4,6 Rarely, direct inoculation may result in skin lesions.
Diagnosis of coccidiomycosis is confirmed using clinical parameters, enzyme immunoassay, culture, histopathology, or a combination thereof.1–3,5 Skin biopsy demonstrates thick-walled spherules in the dermis and subcutis with hematoxylin and eosin, periodic acid Schiff, or silver staining. Mature spherules may demonstrate endospores within, and reactive lesions do not contain organisms.3,10 Skin involvement usually requires systemic antifungal therapy. First-line treatment includes fluconazole, ketoconazole, or itraconazole.2,4,5,9 Voriconazole, posaconazole, and amphotericin B have been used in refractory cases or in severe disease.1,3,5,8 Amphotericin B is the agent of choice in pregnant women.3 Treatment duration may last years, until serological and clinical evidence of disease is absent.4,5
References
- 1.Johnson L, Gaab EM, Sanchez J, et al. Valley fever: danger lurking in a dust cloud. Microbes Infect. 2014;16(8):591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia SCG, Salas-Alanis JC, Flores MG, Gonzalez SEG, Vera-Cabrera L, Ocampo-Candiani J. Coccidioidomycosis and the skin: a comprehensive review. An Bras Dermato. 2015;90(5):610–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiCaudo D. Coccidioidomycosis. Semin Cutan Med Surg. 2014;33(3):140–145. [DOI] [PubMed] [Google Scholar]
- 4.Welsh O, Vera-Cabrera L, Rendon A, Gonzalez G, Bonifaz A. Coccidioidomycosis. Clin Dermatol. 2012;30(6):573–591. doi: 10.1016/j.clindermatol.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Stockamp NW, Thompson GR III, Coccidioidomycosis. Infect Dis Clin North Am. 2016;30(1):229–246. doi: 10.1016/j.idc.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Carpenter JB, Feldman JS, Leyva WH, DiCaudo DJ. Clinical and pathologic characteristics of disseminated cutaneous coccidioidomycosis. J Am Acad Dermatol. 2010;62(5):831–837. doi: 10.1016/j.jaad.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 7.Russell DH, Ager E, Wohltman W. Cutaneous coccidiomycosis masquerading as an epidermoid cyst: case report and review of the literature. Mil Med. 2017;182(1):e1665–e1668. doi: 10.7205/MILMED-D-15-00549. [DOI] [PubMed] [Google Scholar]
- 8.Body BA. Cutaneous manifestations of systemic mycoses. Dermatol Clin. 1996;14(1):125–135. [DOI] [PubMed] [Google Scholar]
- 9.Iyengar S, Chambers CJ, Chang S, Fung MA, Sharon VR. Subcorneal pustular dermatosis associated with Coccidiodes immitis. Dermatol Online J. 2015;21(8).pii: 13030/qt35r6z6bx. [PubMed] [Google Scholar]
- 10.Ocampo-Garza J, Castrejon-Perez AD, Gonzalez-Saldivar G, Ocampo-Candiani J. Cutaneous coccidioidomycosis: a great mimicker. BMJ Case Rep. 2015. pii: bcr2015211680. doi: 10.1136/bcr-2015-211680. [DOI] [PMC free article] [PubMed] [Google Scholar]