Abstract
Rationale
Physical rehabilitation (encompassing early mobilisation) of the critically ill patient is recognised best practice; however, further work is needed to explore the patients’ experience of rehabilitation qualitatively; a better understanding may facilitate implementation of early rehabilitation and elucidate the journey of survivorship.
Objectives
To explore patient experience of physical rehabilitation from critical illness during and after a stay on intensive care unit (ICU).
Design
Exploratory grounded theory study using semistructured interviews.
Setting
Adult medical/surgical ICU of a London teaching hospital.
Participants
A purposive sample of ICU survivors with intensive care unit acquired weakness (ICUAW) and an ICU length of stay of >72 hours.
Analysis
Data analysis followed a four-stage constant comparison technique: open coding, axial coding, selective coding and model development, with the aim of reaching thematic saturation. Peer debriefing and triangulation through a patient support group were carried out to ensure credibility.
Main results
Fifteen people were interviewed (with four relatives in attendance). The early rehabilitation period was characterised by episodic memory loss, hallucinations, weakness and fatigue, making early rehabilitation arduous and difficult to recall. Participants craved a paternalised approach to care in the early days of ICU.
The central idea that emerged from this study was recalibration of the self. This is driven by a lost sense of self, with loss of autonomy and competence; dehumanised elements of care may contribute to this. Participants described a fractured life narrative due to episodic memory loss, meaning that patients were shocked on awakening from sedation by the discrepancy between their physical form and cognitive representation of themselves.
Conclusions
Recovery from ICUAW is a complex process that often begins with survivors exploring and adapting to a new body, followed by a period of recovering autonomy. Rehabilitation plays a key role in this recalibration period, helping survivors to reconstruct a desirable future.
Keywords: rehabilitation medicine, patient experience, recovery, physiotherapy
Strengths and limitations of this study.
This was an exploratory qualitative grounded theory study using semistructured interviews with survivors of critical illness to explore their experience of physical rehabilitation after critical illness; the approach adopted and the data generated provided an extremely rich source of individual experience with many consistent features.
A constant comparison technique of data analysis was used, and enrolment continued until thematic saturation was reached.
Triangulation and peer debriefing were completed to ensure credibility of the study findings that clearly resonated with an independent group of critical illness survivors.
The patients were all recruited from one centre, which may limit transferability of findings. Qualitative studies of this kind innately have a small sample size; however, the richness of the data produced allows deep exploration of meaning and model development, and thematic saturation was also reached.
The variation in time to interview may be considered a limitation of this study in view of impaired recall for longer gaps; however, there was no notable difference in the richness of memories and insight provided by those interviewed at different time points. The variation in time to interview also elucidated the process of recovery over time.
Introduction
Rapid muscle wasting,1 2 functional decline3 and delirium4 are common consequences of critical illness. In the long term, they can lead to prolonged periods of weaning from mechanical ventilation, disability, reduced endurance, anxiety and depression.5–9 To combat these issues, mobilisation, minimising sedation and spontaneous breathing should be instigated early, with research demonstrating safety and likely efficacy.10–13 Furthermore, ongoing rehabilitation following discharge from critical care and attendance at intensive care unit (ICU) follow-up clinics are also advocated, although research showing direct benefit of these interventions is limited.14 15
Although implementation of early mobilisation protocols and post-ICU rehabilitation is inconsistent,14 16 17 early adopters of these strategies are striving for them to become the norm.12 13 18 In such centres, it is not uncommon for patients to receive active out-of-bed physical rehabilitation while receiving full mechanical ventilation, renal replacement therapy and inotropic support.18 Due to the severity of weakness that can be associated with prolonged critical illness, these rehabilitation sessions are often delivered by two or more therapists/nurses and can require technical equipment and physical handling. It is perhaps unsurprising that pain, fatigue, weakness, anxiety, fear, lack of motivation and patient confidence are reported as barriers and reasons for cessation of early rehabilitation.19 20
Sottile and colleagues21 completed a survey of patient experience of early mobilisation in ICU concluding that patients recognised the importance of early mobilisation but found it difficult, tiring and uncomfortable.
In spite of current enthusiasm, there is a paucity of literature exploring survivors’ experience of early mobilisation and physical rehabilitation during and after a stay in ICU in an in-depth manner. For the purpose of this manuscript, the term ‘rehabilitation’ is used to encompass early mobilisation and physical rehabilitation implemented by physiotherapists from admission to ICU.
Aim
To explore the patient experience of recovery from critical illness, with emphasis on their experience of rehabilitation, and to develop a theoretical model grounded in these data.
Methods
Qualitative approach and research paradigm
Constructivist grounded theory study22 using semistructured interviews with a purposive sample of adult ICU survivors. Constructivism contends that individuals’ views are directly influenced by their experiences, and it is these individual experiences and views that shape their perspective of reality. Constructivists believe that individuals have different realities that will be influenced by context—this is a ‘relativist’ ontological stance.22
Constructivist grounded theory is an appropriate methodology for this study because it allows the researcher to develop a theoretical model to explain the data based on an iterative process of data immersion, analysis and interpretation, which recognises and accounts for contextual factors.22
Setting
Participants were recruited from the adult medical/surgical ICU of a 430-bedded London teaching hospital between November 2015 and September 2016.
Participants and sampling
Participants were purposively sampled. Screening and inclusion criteria were: English speaking, a critical stay of >72 hours, capable of providing informed consent determined using the Mental Capacity Act assessment,23 anticipated to survive, aged over 18 years and documented intensive care unit acquired weakness (ICUAW) determined via case note review (this was to ensure that the participants had exposure to rehabilitation interventions).
The clinical team identified potential participants against the broad inclusion criteria stated above to ensure that it was appropriate for them to be approached by the research team. Notes were screened with the aim of purposively selecting a varied sample of participants that could speak to the breadth of emerging themes. If deemed appropriate, participants were then approached by the lead researcher (EJC) and provided with written information. If they had capacity to consent and agreed to participate, written informed consent was gained. Participants who could not provide informed consent were excluded.
At the discretion of the participant, relatives were also invited to be present in the interview to enable exploration and elucidation of any ICU-associated memory loss. As the study progressed, participants were selected to ensure a heterogeneous sample, with the aim of achieving thematic saturation,22 24–26 for example, targeting varying degrees of ICUAW, different genders and specific age categories.
Data collection methods
The semistructured interviews were conducted by EJC. For reflexivity, EJC is research physiotherapist with expertise in critical care and prior training in qualitative methods research. EJC also has personal experience of major injury and as a close relative of an ex-ICU patient. SJB is an ICU medical consultant and is involved with ICU follow-up clinics, and EJM is a researcher focusing on management and change in the health sector, with expertise in qualitative methodology.
The interviews followed a topic guide designed with input from the Intensive Care Society Patient and Relatives Group (box 1). The questions in the topic guide focused on the memory of the admission to ICU, any physical weakness that they encountered and patients’ experience of rehabilitation in the ICU and following discharge. The questions were intentionally left open to initiate reflections and to allow subsequent detailed exploration of the issues that appeared important to the interviewee. The first interview was used as a pilot; however, as no changes were made and those data collected from this interview were rich and informative, it was retained and analysed in the results.
Box 1. Topic guide.
Opening
Introduction.
Consent confirmed.
Questions
Do you have any questions about the about the patient information sheet?
Could you tell me about the events leading up to your admission to the intensive care unit (ICU)?
Could you summarise, as you remember it, your stay on the ICU including the length of your stay and the procedures you experienced (eg, surgery, tracheostomy and so on)?
Could you describe any physical problems that you had during and after your stay, such as weakness, pain, joint stiffness and so on?
-
Could you describe your rehabilitation experience?
Memories of rehabilitation.
Rehabilitation equipment.
Interaction with the therapist.
Intensity of rehabilitation.
Rehabilitation goal setting.
Closing
Do you have any additional information you would like to add?
Do you have any questions?
End
As the study progressed and themes emerged, participants were asked to elaborate and probed on specific issues in line with the constant comparison technique, for example: how the perception of the physiotherapist’s strength influenced their rehabilitation experience; how they perceived their body now; what differences there were between their current and previous physical function; how they saw their future; and what they defined as physical rehabilitation.
The interviews were carried out either in the hospital or in the community after ICU discharge. Enrolment and interviews continued until thematic saturation was reached; that is, no new ideas were emerging, as per the criteria outlined by Bonde.26 This was to challenge the emergent model and ensure credibility. The interviews were anonymised, recorded and transcribed verbatim by a professional transcription company. All transcripts were double-checked for accuracy by EJC.
All interviewees were given pseudonyms to ensure anonymity. Further demographic and clinical data were also collected from the case notes: age, critical care and hospital length of stay, APACHE II score, admission diagnosis, residence prior to admission, premorbid functional level and hospital discharge destination.
Data processing and analysis
Transcripts were uploaded onto NVivo software (QSR International, Doncaster, Australia) for analysis. They were read and reread by EJC to ensure full immersion in the data. Memo writing was used throughout. The first stage of the analysis process is ‘open coding’, which is the identification of primary broad categories; these may be around a theme or topic, or more conceptual, such as emotion or attitude. The second stage is ‘axial coding’; here categories are clustered together into meaningful, related groups. The third stage is ‘selective coding’, where core themes are identified. Lastly, the themes are used to generate a theoretical framework to explain the data.22 24–26 Data collection and analysis occur concurrently, so that constant comparison was made between emerging themes (both within and between narratives) and the literature, allowing model refinement. After the fourth interview had been transcribed and open coding had been completed, axial codes began to form. These ideas were then discussed in detail with the research team. This was followed by a dynamic process of reflection after each interview to develop and refine the axial codes into selective codes until a model encompassing all elements was developed. The last interviews were used to challenge this model and to assess for data saturation. This process allowed a central phenomenon to emerge from the data.22 24–26 The words used for coding were based on the lead researchers interpretation and terms in related literature.
Techniques to enhance trustworthiness
Peer debriefing
Peer debriefing was completed via in-depth discussion with SB and EM. This was done regularly throughout the course of the study.
Patient and public involvement
A patient representative from an ICU support group was consulted in the development of the topic guide. An initial draft of the topic guide was developed by the research team, and it was then sent to the patient representative for review and modification; all of their recommended changes were made. Patients and public were not involved in the recruitment or conduct of the study. Participants were given the opportunity to receive information on the results of the study at their request.
Triangulation
Triangulation and sense checking was completed through presentation to an ICU survivor support group with subsequent dialogue to assess the dependability, confirmability and credibility of the model (this did not include interview participants).
At the support group, the model was presented and then there was opportunity for questions and answers with the researcher (EJC). The group were then left to discuss the study between themselves and feed back to the research team with any thoughts at a later date to allow them to speak openly and frankly with each other. The leader of the support group fed back to the research team that the participants resoundingly agreed with the concepts and felt that the work ‘encompassed all the areas that were important and relevant to those who have experienced critical illness’. The presentation also led to a very tearful response from some attendees who reported to have felt ‘understood’.
Results
Eleven hours of qualitative data from 15 participants (with four additional relatives present) were collected. The patients are described in table 1.
Table 1.
Summary of each participant
| Pseudonym | Relative present? | Age range (years) | APACHE II | Diagnosis | Length of stay, ICU (days) | Length of stay, hospital (days) | Discharge location |
| Richard | No. | 30–39 | 17 | Acute porphryia. | 9 | 102 | Long-term, inpatient rehabilitation. |
| Martin | No. | 30–39 | 14 | Drug overdose, aspiration pneumonia and rhabdomyolysis. | 26 | 32 | Home, outpatient rehabilitation. |
| Sadiq | No. | 50–59 | 22 | Exacerbation of COPD. | 33 | 34 | Home, full care package. |
| Sarah | No. | 60–69 | 24 | Open hernia repair – postoperative MOF | 115 | 197 | Long-term, inpatient rehabilitation. |
| Tom | No. | 60–69 | 10 | Pneumonia and pulmonary embolism. | 10 | 16 | Home, outpatient rehabilitation. |
| Evan | No. | 60–69 | 15 | Acute bowel obstruction – colon cancer. | 5 | 48 | Home, no rehabilitation. |
| Sasha | Yes, daughter. | 50–59 | 10 | Neuromyelitis opitica. | 19 | 98 | Long-term, inpatient rehabilitation. |
| John | No. | 40–49 | 27 | Influenza. | 33 | 71 | Long-term, inpatient rehabilitation. |
| George | No. | 50–59 | 12 | Drug overdose – respiratory failure. | 25 | 36 | Home, no rehabilitation. |
| Michelle | No. | 80–89 | 14 | Exacerbation of COPD. | 6 | 42 | Declined inpatient rehabilitation – home, full care package. |
| Jim (M) | Yes, wife. | 50–59 | 11 | Food poisoning – MOF. | 10 | 18 | Home, no rehabilitation. |
| Matthew (M) | No. | 70–79 | 18 | Hospital-acquired pneumonia – fractured NOF. | 5 | 178 | Nursing home. |
| Caroline (F) | Yes, husband. | 70–79 | 22 | Anterior resection for bowel cancer. | 13 | 63 | Short stay, inpatient rehabilitation. |
| Ben (M) | No. | 40–49 | 15 | Drug overdose. | 65 | 107 | Home, care package. |
| David (M) | Yes, wife present. | 63 | 21 | Influenza. | 150 | 232 | Long-term, inpatient rehabilitation. |
APACHE, Acute Physiology and Chronic Health Evaluation II; COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; MOF, multiorgan failure; NOF, neck of femur.
The median ICU and hospital length of stay were 19 days (IQR 8–33) and 63 days (IQR 34–107), respectively. The median time between ICU discharge and interview was 56 days (IQR: 36–80). Ten (66.6%) of the interviews took place at the hospital while the patients were still inpatients, and five (33.3%) took place after discharge in the patient’s home (n=2), work (n=1) or in a clinic room (n=2). The interviews lasted a median of 39 min (IQR: 28–50).
The central phenomenon grounded in these data was recalibration of the self. There were two themes contributing to this temporal model of recovery: the transition ‘from prior self to current self’ and the transition ‘from current self to construction of the future self’. When questioned about early physical function, patients recalled a discrepancy at the time of recovering awareness between their current self, which incorporates their physical dependency, fatigue, clarity of mind and self-image, and the mental representation of themselves, which is still consistent with their preadmission self. This discrepancy seemed to be due to episodic memory loss of their admission period. Additionally, patients lacked some of the cognitive requirements for prospection at this point,26 and therefore they struggled to envisage a compelling future self. This appears to lead on to a period of recalibration.
Although this central phenomenon of recalibration may seem distinct from the early physical rehabilitation experience that was the focus of this study, it was quite the opposite, with the process of recalibration seeming inextricably linked to the rehabilitation experience. Physical independence and function are core components of the concept of self. When physical ability deteriorates so unexpectedly, rapidly and without obvious causation (as in ICUAW), it comes as a shock to the patient blurring their sense of self. Physical rehabilitation aims to improve impairments and function by challenging patients’ physical ability thereby, in this extreme context, inadvertently challenging their self-perception as well.
This model suggests that physical rehabilitation within ICU helps patients to challenge and explore their current functional level and reconcile their self-discrepancy, that is, difference between their physical self and the cognitive image of themselves. The process of therapy goal setting also challenges their capacity to think about the future; discussing goal setting with participants therefore elucidated the difficulties they may have in constructing a compelling future to act as a motivational force.
The rationale and contributing themes are presented below. Supporting evidence is presented in table 2.
Table 2.
Supporting data
| Central phenomenon: recalibration of the self | |
|
Main theme 1: ‘From prior self to current self’
Sasha: ‘I didn’t realize I couldn’t walk. I thought I could and I tried to get out of bed loads of times, but up here I was weak (legs) and the top of my arms were weak as well. I couldn’t do it’. Sarah: ‘I don’t ever look at myself in the mirror and there is a mirror in that bathroom, I just happened to catch sight of my whole body almost and I nearly died. I thought; that doesn’t resemble the person that I am’. | |
| Episodic memory loss |
ICU admission
Sasha: ‘… that’s when I don’t know, it’s a real black after that (the emergency room)’. Sadiq: ‘That is a black. That is a blank. Totally blank’. John: ‘I must have been in and out of consciousness, because I don’t remember anything’. Ben: ‘I had a bad fall, collapsed… that’s all I remember’. |
|
Rehabilitation and mobilisation
EJC: ‘[W]hat was your memory of getting moving after you woke up with the tubes attached?’ Ben: ‘I don’t really have much memory of it’. EJC: ‘Do you remember any of the rehab on ICU?’ Martin: ‘Not to start with, no’. David: ‘It was Dan (ward physiotherapist) who taught me to sit on the edge of the bed’. EJC: ‘Do you remember getting into the chair for the first time?’ Michelle: ‘It was with Tom (the ward physical therapist)’. | |
| Hallucinations and delusions | John: ‘I kept thinking I could see like people with hoodies and they were like assassins, trying to get in’. David: ‘I was taken into Soho (Central London) by some people and stuck under a glass floor, lying under a glass floor with formaldehyde around me. I was encased’. Ben: ‘I operated on Margaret Thatchers cat and there was eight other people in the house and three of them got shot… I remember waking up with the fear that I was going to get shot’. Carolyn: ‘I was trying to use my mobile (to escape), and the same number kept on pressing and I remember panicking’. |
| Weakness | George: ‘Nothing, I couldn’t move my hand. I couldn’t move and that was really scary. Really scary’. Richard: ‘I couldn’t do anything. I was paralyzed from the neck down… I still felt like I had sensation in my legs and my arms, I just couldn’t move them’. Carolyn: ‘I couldn’t even stand up. I was really very, very weak’. John: ‘I couldn’t do anything. I mean literally, I couldn’t move, I could just barely move my fingers’. David: ‘I couldn’t move. I couldn’t move at all. I could blink, that’s about it’. Martin: ‘… couldn’t walk, couldn’t do nothing’. Richard: ‘You are reliant entirely on the people around you, for everything really… that’s difficult’. |
| Noxious cycle of ICU | Sarah: ‘I didn’t want to do it (physiotherapy). I used to dread them coming, any excuse to get out of it. I was just so tired’. John: ‘Physically tiring, emotionally… you’re like “sh*t really? I’ve got to do it (mobilization) now? I haven’t got any energy at all”’. George: ‘There were some days when they’d (physiotherapist) come and they’d get me into the chair, and they’d want to do some work on the zimmer frame. They’d come back (from getting the zimmer frame) and I’d be asleep’. Sarah: ‘People kept telling me to read, but I couldn’t. I couldn’t’ actually physically read. They’d bring me the menu and I just couldn’t do it, and then I’d fall asleep’. Sarah: ‘… then I just accepted it (weakness), going… on the hoist and, you lose all dignity when you’re in that state you just accept it, and you just let them help you as much as possible and when you’ve done your, you know bits of physio, exhausted, you go back to bed again, sleep again. You know it tended to be like that’. |
|
Main theme 2: ‘From current self to construction of the future self’
Ben: ‘The first days when I couldn’t move… I was disillusioned with the whole thing, and I thought, “This is never going to work”… I couldn’t see how anything could turn round, but I was told just to trust. But that period was very difficult because when you don’t see any light at the end of the tunnel, it’s difficult to sort of engage with it, and it’s difficult to trust… There was plans in my head, but it’s difficult to kind of have them if you think it’s just a waste of time what you’re doing. Now I know that there is (light at the end of the tunnel)… and I believe I’ll be walking next week, they’ve (physiotherapists) let me believe that’. | |
| Recovery milestones and goal setting | Matthew: ‘Let the patient realize that he is not capable of doing that, or this, or whatever… don’t tell him’. Tom: ‘Everyone’s functions, and how they are improving, might not be quite so obvious to the patient’. Carolyn: ‘The other day the whole ward congratulated me- and even now I feel embarrassed – because I washed myself. I didn’t wait until now to know how to wash myself; I thought it was so stupid’. Jim’s wife: ‘We didn’t want to set the goals, because we didn’t know what goals to set’. Sadiq: ‘It depends on the person. If a person is shooting to the high, they might do it (achieve their goal), but sometimes shooting too much to the high might break your neck. If they are too sick, they cannot talk, you are in the dark and you have to put your own objectives’. Researcher: ‘What have been the things that have kept you going?’ Sasha: ‘I think Gemma (daughter) and her dad, they’ve been so supportive. He’s been down every day, and Gemma sometimes twice a day *starts crying*… sorry… I suppose if it wasn’t for them, I wouldn’t be… *crying- unable to finish sentence*’. Richard: ‘obviously I was doing it (rehab) for me primarily, but knowing how much concern and love she has for me, and knowing how much it would mean to her and how much of a relief it would be to her… The fact that she was, you know with me for as long as she was, and as strong as she was… I don’t know. I never thought my mum was that strong’. |
ICU, intensive care unit.
‘From prior self to current self’
Episodic memory loss
Fundamental to the patient experience of rehabilitation, and underpinning the theoretical interpretation, was patients’ episodic memory loss (ie, loss of a specific autobiographical event) of their admission to ICU, regardless of their admission background or diagnosis. In some cases, this memory gap lasted weeks, with some participants unable to recall any rehabilitation sessions on ICU at all, citing their ward rehabilitation sessions as their first experiences. The first clear memory for all participants was a family member at the bedside. This frequently elicited a tearful response; for example, George stated: ‘(my first memory on awakening) was my mother stroking my arm, saying “Mum’s here”… that was some 30 days after my admission’. This memory loss is of paramount importance, as it made it difficult for participants to rationalise and understand their current situation.
Hallucinations and delusions
All patients experienced vivid hallucinations that often involved torture and trying to escape. Some of the hallucinations, however, were pleasant experiences, such as a friendly dog in the ICU. Those with a history of recreational drug use seemed less shocked by hallucinations and able to rationalise their mental state; for example, John stated: ‘you’re pumped full of so many drugs, it doesn’t surprise me that you’re tripping out’. Perceived stigma influenced patients’ comfort in discussing hallucinations with staff; for example, EJC asked Tom: ‘Did you tell anyone about the hallucinations at the time?’ Tom replied: ‘No… I just felt a bit silly’.
Weakness
On awakening patients reported frustration at their inability to communicate and were shocked by the severity of their weakness, as mentally they still saw themselves as capable of the physical tasks they were able to do preadmission; for example, Sasha stated: ‘I didn’t realise I couldn’t walk. I thought I could and I tried to get out of bed loads of times, but up here I was weak (legs) and the top of my arms were weak as well. I couldn’t do it’. Their actual physical self and cognitive representation of themselves did not match; for example, Sarah said: ‘I just happened to catch sight of my whole body (in the mirror) and I nearly died. I thought; “that doesn’t resemble the person that I am”’. However, it was the psychological symptoms that were of the greatest concern to patients initially; for example, Evan felt that: ‘there were tubes all over the place… but that was the least of my worries. The specialists were there, and my son. I said “I don’t know who that is (son)”. My son came back on the Monday, then I recognised him and things started falling back into place’.
‘Noxious cycle’ of ICU
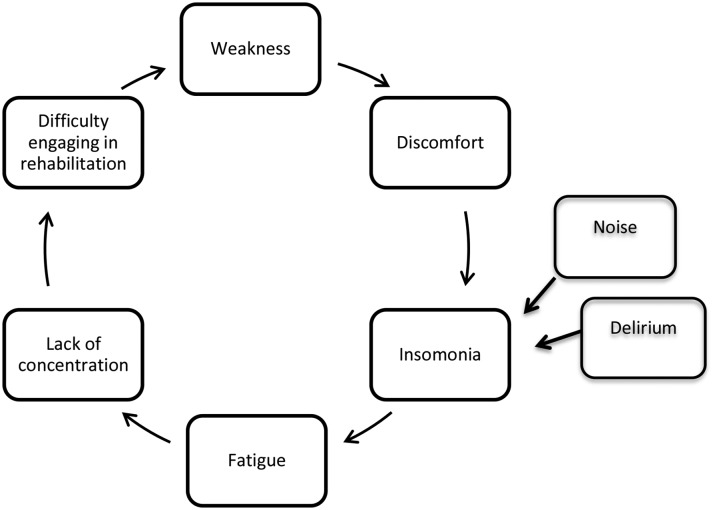
Overwhelming fatigue, insomnia (due to noise and disruption), boredom and the inability to concentrate were prevalent, which had a negative impact on the ability to engage in both physical rehabilitation and cognitive tasks and made many fear early rehabilitation; for example, John stated: ‘Physically tiring, emotionally, you’re like “sh*t, really? I’ve got to do it (physiotherapy) now. I haven’t got any energy at all”’. Procedural pain was reported in only a few instances, but discomfort was problematic, for example, from being ‘swaddled’ in blankets (John). For many, this seemed to form a ‘noxious cycle’ (figure 1).
Figure 1.
The noxious cycle of critical illness.
Humanisation of care
Participants valued ‘humanised’ care,27 often remembering the staff members who made them laugh and feel safe, for example, Caroline said: ‘I remember one bloke, one nurse, who- he would come in and smile, and I said “Oh, you’re always smiling. You make me so happy”’. Trust in the clinical team was also important; if trust was compromised, then it had a negative impact on participants’ engagement with rehabilitation. Trust seemed dependent on the rapport the staff member developed with the patient, including their ability to communicate honestly and to maintain patient’s hope, for example, Michelle stated: ‘I trust him… because when Tom (physiotherapist) says something, it’s true. Everything he said was true’. However, the staff–patient interaction was not always positive, with many patients describing examples of de-humanised care.27 This included loss of agency: ‘I feel so not free, everyone is doing what they want, I’m like a puppet and I hate that’ (Michelle), and feeling isolated: ‘I don’t think I had a voice at one point, which was probably one of the most difficult things to experience, because you can’t talk to people’ (Richard).
Although not related to humanisation of care, the physical attributes of staff also influenced patients’ rehabilitation experience, if physiotherapists looked small, young and weak, then patients had less trust in their physical ability to keep them safe during rehabilitation, an example came from David: ‘He (the physio) was strong of course. One admires that. It’s an ability, you know; and of course, not everybody’s going to have that ability’.
‘From current self to construction of the future self’
Recognising milestones to recovery and goal setting
The vulnerability described by patients and relatives seemed to lead to a sense of desired paternalism in the early days; they did not feel ready to be in control. This was further perpetuated by a lack of understanding of the stages of recovery; for example, Tom stated: ‘how you are improving may not be quite so obvious to the patient’. The memory loss of their admission meant that patients did not recall their acute stages of illness, and hence their physical decline; the weakness that they were experiencing did not make sense and was often so severe that it made it difficult to envisage the next steps in their recovery. As a result, patients did not always recognise basic functional tasks as rehabilitation or indeed their achievements as progress; for example, Michelle stated: ‘The other day the whole ward congratulated me- and even now I feel embarrassed – because I washed myself. I didn’t wait until now to know how to wash myself; I thought it was so stupid’. Therapeutic adjuncts, such as the use of a bed bike or tilt table, were more commonly recalled as rehabilitation.
As patients had limited understanding of the recovery milestones early on, they wanted the multidisciplinary team to set their rehabilitation goals as ‘they did not know what goals to set’ (Jim). The main thing that kept them focused on engaging in rehabilitation at this point was their family and loved ones; Sarah described this: ‘I cry a lot…something helped me to keep going, an inner strength came…the kids…’.
Patient involvement in early goal setting was described as like ‘being in a car crash and someone asking you how you want to be cut out’. Most patients had a ‘just get on with it’ approach to rehabilitation. Martin: ‘I just blind folded said, “if this is what I am supposed to do, I will do it”’. However, despite desiring early clinician-led rehabilitation, all patients identified a high-level goal that aligned to the core values of who they are; examples include returning to work, going on holiday, finishing a PhD and getting married.
As patients progressed through the stages of recovery, they started to recognise smaller functional gains as improvement and engaged more in the goal setting and rehabilitation planning process; for example, Sarah stated: ‘Well, I was shocked at how little I could do, but now, it’s the other way, I’m actually shocked at how much I can do and I am doing. It’s really good’. Their yardstick for comparison now became who they were on awakening and not who they were prior to admission; they were recalibrating.
Discussion
This work focused on exploring the experience of physical rehabilitation after critical illness; however, as with inductive research, what transpired was a complex model of recovery extending beyond the physical. Patients demonstrated an interruption to personal narrative, a lost sense of self associated with loss of autonomy, temporary desired paternalism and gave examples of accidental dehumanised care (although mostly non-maleficent in intent). Delirium, sleep deprivation, fatigue and memory loss acted as potent mediators between the patients’ physical impairments and their ability to recalibrate to their new disability and engage in rehabilitation.
It is interesting to consider these findings in the context of established psychological theory. Deci and Ryan’s Self-Determination Theory28 29 attempts to explain why people engage in goal-orientated behaviour, exploring how this leads to well-being and personal growth. Its three core concepts are: autonomy (the ability to be in control of oneself), competence (the ability to manage the situation they are in) and relatedness (the ability to have an emotional connection with others). Only when these needs are met can intrinsic motivation flourish. Critical illness can strip patients of autonomy and competence, and perhaps for a shorter period, relatedness. In the initial stages of critical illness, patients may be unable to communicate and talk, be unable to move easily due to weakness, may have hallucinations and be too fatigued to engage in decision making. Hence, loss of autonomy and competence are key features of the patient experience. Relatedness, which may recover earlier (or be encouraged), is of paramount importance to them and was a motivator to engage in rehabilitation.
Markus and Nurius30 developed a theory called ‘The Possible Self’. They contend that humans have different cognitive representations of who we are (current self) and who we could be (possible self). Possible selves drive behaviour. A notion of the possible self helps us to assess our current self by creating a benchmark for comparison for self-evaluation. It can also provide tangible rehabilitation goals. The possible self and goal setting also rely heavily on temporality, therefore requiring narrative of the past, and the capacity to prospect. Physiologically, prospection depends on episodic memory, prospective memory, emotional stability and hypothetical thinking,31 some of which can be impaired in critical illness due to sleep deprivation, fatigue and delirium.
On awakening, patients’ immediate cognitive representation of their current self matched their preadmission self because they do not remember their functional decline; however, their body had changed. Their mental image of their current self and their physical self were not aligned. Furthermore, patients could not remember the totality of their past, they did not recognise their present and they struggled to construct a compelling future self. This impaired their ability to engage in rehabilitation goal setting and led to a sense of vulnerability, desired paternalism and emphasis on relatedness.
This model of recalibration ties these established psychological ideas together, reflecting the need for patients to explore their new self, adapt to it and allow it to become their new yardstick. When this was achieved, smaller milestones in recovery became meaningful goals. Others have described similar concepts as a liminal state. Liminality is an anthropological term from the Latin word līmen, meaning threshold.32 It refers to someone who is transitioning. It is often associated with a change in role/identity or a loss of one self to be replaced with another. This can create inner turmoil, especially if that change is not invited.
This idea of liminality in ICU has been touched on by a number of authors.32–35 Kean and colleagues32 identified ‘unscheduled status passage’ from prior self to critically ill self as a theme in a longitudinal study of ICU survivorship. They found that this unscheduled liminal stage is worsened by memory loss and delirium and that this process of change is temporal in nature, both progressing and regressing (in the event of decline). In order to move on, patients need to regain autonomy.
Lindberg and colleagues35 described what recovering autonomy looks like, suggesting that patients go through four stages: the first is to acknowledge their dependence (or paternalism), and then they strive to be recognised as a person (‘humanised’ care). These two stages echo the findings of this study. The latter two stages are ‘invited participation in care’ and ‘becoming a co-partner in the decision-making’. These stages describe how staff coach patients to take control again through mutual trust, understanding and codetermination.
Although these may seem like abstract concepts, it is the authors’ view that they have direct relevance to clinical practice, especially as early rehabilitation becomes a key aspect of acute care. The reason for this is that perception of self and engagement in rehabilitation and goal setting are inextricably linked.
If a person’s mind is telling them one thing about who they are and what they are capable of doing and their body is telling them another, they cannot start thinking about the future until they reconcile that difference. They cannot reconcile that difference with delirium, hallucinations and lack of episodic memory to justify their current situation and facilitate hypothetical thinking and prospection.31 Combining psychological intervention with physiotherapy intervention may help to address this.
Goal setting depends on the capacity to prospect. It is also a key recommendation in the UK National Institute for Health and Care Excellence (NICE) Guidelines for Rehabilitation after Critical Illness36 and NICE Quality Standards.37 The Quality Standards state that rehabilitation goals should be set within 4 days of admission and ideally should be patient agreed. These data would suggest that asking patients to set goals at day 4 may be premature. Further research exploring the application of the model of recovering autonomy described by Lindberg et al 35 may assist in tailoring rehabilitation guidelines to the specific needs of the critically ill.
Further focus on how rehabilitation is delivered, not just what is delivered could also be instructive. The impact of the dynamic between a sports coach and the players is well known, yet this coaching dynamic is neglected somewhat in ICU rehabilitation. If clinicians are able to assist patients in recalibrating to their new current self, and the reconstruction of a compelling future self, it may improve patient care and outcome. Further research will be needed to confirm the concepts identified in this initial exploratory study. However, we believe the concepts identified are sufficiently plausible and robust to pose challenges to clinicians working with recovering critically ill patients (outlined in box 2).
Box 2. Key observations and challenges to practice.
Key observations
-
Patients recovering consciousness during or after a critical illness are likely to be shocked by the transition through which they have gone. Part of that shock is the due to the unplanned interruption of their autobiographical story.
How can you help to fill the gaps in autobiographical memory?
-
Patients’ immediate memory is of who they were and what they were able to do before there critical illness. This is in collision with what they can actually do, and a period of recalibration is needed to allow people to align the two and develop reasonable ambitions and goals.
How can you support patients to explore their current function and settle the discrepancy between expectations and reality?
-
This recalibration is the development of an understanding of the relationships between their past, present and possible futures selves.
How can you help patients to envisage a compelling future?
-
Because of this need for recalibration along with delirium and impaired cognition, patients may need, and wish for, assistance in planning early rehabilitation. As autonomy recovers, patients desire to become fully involved increases.
How can you recognise and support recovering autonomy?
-
Motivation and engagement are crucial in maximising the benefits of rehabilitation. Leveraging human relationships (relatedness) and encouraging autonomy are likely to be helpful; care that is dehumanising, even if ‘efficient’, is likely to impair recovery.
How can humanisation of care be optimised in your ICU?
Supplementary Material
Acknowledgments
We would like to thank Dr Cherry Kilbride and Dr William Young (Brunel University London) for their input into the theoretical interpretation of these data. Thank you to Gordon Sturmey and the ICU support network in Reading for their involvement and support with the study.
Footnotes
Contributors: All authors were involved in the methodological design, data analysis and writing and reviewing the manuscript. EJC did all of the interviews and data collection.
Funding: This study was kindly funded by The Joint Research Committee at Chelsea and Westminster Hospital on behalf of a joint collaboration between the Chelsea and Westminster Medical School Research Trust (Registered Charity No. 247808) and Chelsea and Westminster Health Charity and Brunel University London. EJM acknowledges the support of The Health Foundation. SJB is grateful for the support of the National Institute for Health Research (NIHR) comprehensive Biomedical Research Centre based at Imperial College Healthcare NHS Trust and Imperial College London.
Disclaimer: The views expressed are those of the authors and not necessarily those of the NHS, The Health Foundation, the NIHR or the Department of Health.
Competing interests: None declared.
Ethics approval: This study was granted approval by the East of England Ethics committee (REC reference number 14/EE/1027) and from the Research and Development Department at the study site.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All available data can be obtained by contacting the corresponding author.
Patient consent for publication: Not required.
References
- 1. Puthucheary ZA, Rawal J, McPhail M, et al. . Acute skeletal muscle wasting in critical illness. JAMA 2013;310:1591–600. 10.1001/jama.2013.278481 [DOI] [PubMed] [Google Scholar]
- 2. Friedrich O, Reid MB, Van den Berghe G, et al. . The sick and the weak: neuropathies/myopathies in the critically Ill. Physiol Rev 2015;95:1025–109. 10.1152/physrev.00028.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hermans G. & Van den Berghe G. Clinical review: intensive care unit acquired weakness. Crit Care 2015;5:274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cavalazzi R, Saad M, Marik PE. Delirium in the ICU: an overview. Ann Intensive Care 2012;2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kress JP, Hall JB. Intensive care unit acquired weakness and recovery from critical illness. N Eng J Med 2014;370:1626–35. [DOI] [PubMed] [Google Scholar]
- 6. Cuthbertson BH, Elders A, Hall S, et al. . Mortality and quality of life in the five years after severe sepsis. Crit Care 2013;17:R70 10.1186/cc12616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kaukonen KM, Bailey M, Suzuki S, et al. . Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA 2014;311:1308–16. 10.1001/jama.2014.2637 [DOI] [PubMed] [Google Scholar]
- 8. Hill AD, Fowler RA, Pinto R, et al. . Long-term outcomes and healthcare utilization following critical illness–a population-based study. Crit Care 2016;20:76 10.1186/s13054-016-1248-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pandharipande PP, Girard TD, Jackson JC, et al. . Long-term cognitive impairment after critical illness. N Engl J Med 2013;369:1306–16. 10.1056/NEJMoa1301372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nydahl P, Sricharoenchai T, Chandra S, et al. . Safety of patient mobilization and rehabilitation in the intensive care unit. systematic review with meta-analysis. Ann Am Thorac Soc 2017;14:766-777 10.1513/AnnalsATS.201611-843SR [DOI] [PubMed] [Google Scholar]
- 11. Castro-Avila AC, Serón P, Fan E, et al. . Effect of early rehabilitation during intensive care unit stay on functional status: systematic review and meta-analysis. PLoS One 2015;10:e0130722 10.1371/journal.pone.0130722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Balas MC, Burke WJ, Gannon D, et al. . Implementing the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle into everyday care: opportunities, challenges, and lessons learned for implementing the ICU pain, agitation, and delirium guidelines. Crit Care Med 2013;41:S116–S127. 10.1097/CCM.0b013e3182a17064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Balas MC, Vasilevskis EE, Olsen KM, et al. . Effectiveness and safety of the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle. Crit Care Med 2014;2014:1024–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Connolly B, Douiri A, Steier J, et al. . A UK survey of rehabilitation following critical illness: implementation of NICE Clinical Guidance 83 (CG83) following hospital discharge. BMJ Open 2014;4:e004963 10.1136/bmjopen-2014-004963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jensen JF, Thomsen T, Overgaard D, et al. . Impact of follow-up consultations for ICU survivors on post-ICU syndrome: a systematic review and meta-analysis. Intensive Care Med 2015;41:763–75. 10.1007/s00134-015-3689-1 [DOI] [PubMed] [Google Scholar]
- 16. Nydahl P, Ruhl AP, Bartoszek G, et al. . Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med 2014;42:1178–86. 10.1097/CCM.0000000000000149 [DOI] [PubMed] [Google Scholar]
- 17. Berney SC, Rose JW, Bernhardt J, et al. . Prospective observation of physical activity in critically ill patients who were intubated for more than 48 hours. J Crit Care 2015;30:658–63. 10.1016/j.jcrc.2015.03.006 [DOI] [PubMed] [Google Scholar]
- 18. Hodgson CL, Stiller K, Needham K, et al. . Expert consensus and recommendations on safety criteria for active mobilisation of mechanically ventilated critically ill patients. Critical Care 2014;16:658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Parry SM, Knight LD, Connolly B, et al. . Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med 2017;43:531–42. 10.1007/s00134-017-4685-4 [DOI] [PubMed] [Google Scholar]
- 20. Wright SE, Thomas K, Watson G, et al. . Intensive versus standard physical rehabilitation therapy in the critically ill (EPICC): a multicentre, parallel-group, randomised controlled trial. Thorax 2018;73 10.1136/thoraxjnl-2016-209858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sottile PD, Nordon-Craft A, Malone D, et al. . Patient and family perceptions of physical therapy in the medical intensive care unit. J Crit Care 2015;30:891–5. 10.1016/j.jcrc.2015.04.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mills J, Bonner A, Francis K. The development of constructivist grounded theory. Int J Qual Methods 2006;5:25–35. 10.1177/160940690600500103 [DOI] [Google Scholar]
- 23. UK legislation. Mental Capacity Act. 2005. https://www.legislation.gov.uk/ukpga/2005/9/contents.
- 24. Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory. 4th edn London, 2015. [Google Scholar]
- 25. Heath H, Cowley S. Developing a grounded theory approach: a comparison of Glaser and Strauss. Int J Nurs Stud 2004;41:141–50. [DOI] [PubMed] [Google Scholar]
- 26. Bonde D. Qualitative interviews: when enough is enough. Research by Design. 2013.
- 27. Todres L, Galvin KT, Holloway I. The humanization of healthcare: a value framework for qualitative research. International Journal of Qualitative Studies on Health and Well-being 2009;4:68–77. 10.1080/17482620802646204 [DOI] [Google Scholar]
- 28. Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York, NY: Plenum, 1985. [Google Scholar]
- 29. Deci EL, Ryan RM. Theory. 2017. http://selfdeterminationtheory.org/theory/ (Accessed 30th Mar 2017).
- 30. Markus H, Nurius P. Possible selves. American Psychologist 1986;41:954–69. 10.1037/0003-066X.41.9.954 [DOI] [Google Scholar]
- 31. Osman M. What are the essential cognitive requirements for prospection (thinking about the future)? Front Psychol 2014;5:626 10.3389/fpsyg.2014.00626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kean S, Salisbury LG, Rattray J, et al. . ‘Intensive care unit survivorship’ - a constructivist grounded theory of surviving critical illness. J Clin Nurs 2017;26:3111–24. 10.1111/jocn.13659 [DOI] [PubMed] [Google Scholar]
- 33. Johnston LB. Surviving critical illness: a case study in ambiguity. J Soc Work End Life Palliat Care 2011;7:363–82. 10.1080/15524256.2011.623471 [DOI] [PubMed] [Google Scholar]
- 34. Darbyshire JL. “I Can Remember Sort of Vivid People… but to Me They Were Plasticine.” Delusions on the Intensive Care Unit: what do patients think is going on? PLoS ONW;11:e0153775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lindberg C, Sivberg B, Willman A, et al. . A trajectory towards partnership in care–patient experiences of autonomy in intensive care: a qualitative study. Intensive Crit Care Nurs 2015;31:294–302. 10.1016/j.iccn.2015.04.003 [DOI] [PubMed] [Google Scholar]
- 36. National Institute for Health and Clinical Excellence. Great Britain. Rehabilitation after critical illness Great Britain. 2009. www.nice.org.uk. [PubMed]
- 37. National Institute for Health and Clinical Excellence. Rehabilitation after critical illness in adults: quality standard. 2017. nice.org.uk/guidance/qs158 (Accessed 13th Sep 2017)). [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.