Abstract
Objective
The aim of this study is to assess the odds of caesarean section (CS) for uninsured women in the USA and understand the underlying mechanisms as well as consequences of lower use.
Study design
Systematic review and meta-analysis.
Data sources
PubMed, Embase, the Cochrane Library and CINAHL from the first year of records to April 2018.
Eligibility criteria
We included studies that reported data to allow the calculation of ORs of CS of uninsured as compared with insured women.
Outcomes
The prespecified primary outcome was the adjusted OR of deliveries by CS of uninsured women as compared with privately or publicly insured women. The prespecified secondary outcome was the crude OR of deliveries by CS of uninsured women as compared with insured women.
Results
12 articles describing 16 separate studies involving more than 8.8 million women were included in this study. We found: 0.70 times lower odds of CS in uninsured as compared with privately insured women (95% CI 0.63 to 0.78), with no relevant heterogeneity between studies (τ2=0.01); and 0.92 times lower odds for CS in uninsured as compared with publicly insured women (95% CI 0.80 to 1.07), with no relevant heterogeneity between studies (τ2=0.02). We found 0.70 times lower odds in uninsured as compared with privately and publicly insured women (95% CI 0.69 to 0.72).
Conclusions
CSs are less likely to be performed in uninsured women as compared with insured women. While the higher rates for CS among privately insured women can be explained with financial incentives associated with private insurance, the lower odds among uninsured women draw attention at barriers to access for delivery care. In many regions, the rates for uninsured women are above, close or below the benchmarks for appropriate CS rates and could imply both, underuse and overuse.
Keywords: caesarean section, health insurance, uninsured, self-pay, medical practice variation, underuse
Strengths and limitations of this study.
Extensive literature search, screening and data extraction performed in duplicate, review and analysis of study characteristics as well as thorough quality assessment of included studies.
All studies are from one country, that is, the USA, and this limits the effect of contextual factors.
A major limitation of our study is the variation across studies, in terms of the study populations characteristics, type of data used, types of caesarean section analysed and adjusting variables used in statistical analyses.
The results of this study are driven by the largest study which contains over two-thirds of the population included in this review. Only 5 out of 16 studies included in the review report data after year 2000.
While a population-level caesarean section rate of less than 9%, 10% or 19% suggests underuse, we cannot determine the mix of under, over and appropriate use in a specific population.
Introduction
Introduction of clinical procedures in medical practice has saved and improved the lives of many people worldwide. But with time, these clinical procedures become subject to overuse or underuse.1 Overuse may result in unnecessary harm due to the side effects of the procedures or, in case of underuse, not receiving the care they need.1–3 These adverse effects occur due to differing health systems and other contextual factors.3 4 These factors include financial and non-financial barriers in accessing healthcare, present even in the most advanced economies of the world, such as the USA. Consequently, specific segments of the population may be underserved as healthcare systems are unable to address structural problems that leave patients without the care they need.1
Globally, caesarean section (CS) is an example of overuse and underuse of clinical procedures. Once introduced into clinical practice, it greatly improved maternal and newborn outcomes.5 Presently, many countries have long exceeded the 9%–16% or 10%–15% thresholds or 19% benchmark for CS out of total deliveries, argued to be the ideal rates of CS in terms of improving the health of women and newborns.6–9 CS rates average as high as 40.5% among countries in Latin America and the Caribbean region,10 32.3% in Northern America10 (32.2% in USA),11 while on the other extreme, it is as low as 7.3% in Africa10: 1% in Nepal and Cambodia to 0.6% in Ethiopia and Niger.12 Variations are also observed within countries.5 12 13 For instance, in the USA, a recent study reported a range between 4% and 65% across health markets.14
Insurance coverage is one of the health system factors known to influence the use of medical procedures,15 16 including CS.17–20 While private insurance, for example, seems to increase the odds of having a CS delivery,17 the lack of insurance appears to decrease it.20–22 Millions of people worldwide, as well as in the USA, are not covered by any insurance scheme and are exposed to the hazard of being underserved with clinical procedures,23–27 including perinatal services.28 The USA has a mixed health insurance system dominated by private insurance.24 The Federal Medicare program covers people over 64 years old and/or disabled, which accounts for about 16.7% of the population.24 State Medicaid programs cover children and parents from low-income families as well as partially caring for Medicare beneficiaries with low incomes and, in total, accounts for about 19.4% of the US population.29 Over half of US population is covered with voluntary employer-based private insurance.29 The remaining population is uninsured and can range from 2.5% (Massachusetts) to 16.6% (Texas) according to 2016 estimates.29 For decades, in the USA, there has been an ongoing debate for and against universal health coverage and related topics with limited but substantial progress towards more coverage through the Affordable Care Act.23 30–37 Nonetheless, millions of Americans remain uninsured for various reasons and are not able to access the healthcare they need.23 31 38 The aim of this study is to assess the odds of CS for uninsured women in the USA and understand the underlying mechanisms as well as consequences of lower use in the US context.39
Materials and methods
Search strategy and data sources
Search words referring to CS, such as ‘caesarean section’, ‘caesarean delivery’, caesarean’, were combined with words referring to factors contributing to variation and increase of CS rates, such as ‘insurance’, ‘social class’, ‘socioeconomic’ and words referring to the study design, such as ‘geographical variation’, ‘medical practice variation’ (online supplementary appendix 1). No publication date or language restrictions were applied. We searched PubMed, Embase, the Cochrane Library and CINAHL from the beginning of records to the end of April 2018, when we last updated our search. A manual search was applied on the reference lists of included studies and previous systematic reviews.
bmjopen-2018-025356supp001.pdf (6.1KB, pdf)
Study selection and outcomes
To be included in the analysis, studies had to report OR or data that enabled the calculation of OR of CS comparing uninsured against privately and/or publicly insured women. More specifically, we did not exclude studies based on any population characteristic. Studies had to report normal (vaginal) and CS deliveries with uninsured and privately and/or publicly insured comparisons. In an ideal situation, studies would report adjusted OR of uninsured as compared with privately and/or publicly insured women, but in cases, ORs were not calculated by the authors, we would extract data (rates and regression coefficients) and perform calculations that would allow for the derivation of OR. We did not exclude studies by type of study design, variables used for adjustment or any other study characteristic. Adjusted OR of deliveries by CS of uninsured women in comparison to insured women was the prespecified primary outcome. Crude OR of deliveries by CS of uninsured women in comparison to insured women was the prespecified secondary outcome.
Data extraction
Papers screening and independent data extraction was done by two researchers (IH and MB). Differences were resolved based on consensus. We extracted data on study population, study design, data sources, setting, type of CS analysed, statistical analysis and (primary and secondary) outcome measures (online supplementary appendix 2).
bmjopen-2018-025356supp002.pdf (132.4KB, pdf)
Quality assessment
We used Quality In Prognosis Studies (QUIPS) to assess the risk of bias across six study domains.40 Each study was evaluated independently by two researchers (IH and MB) and any differences among evaluators were discussed and resolved. A single rating was assigned for all studies. As specified in the QUIPS tool, a ‘high’, ‘moderate’ or ‘low’ rating was applied for individual domains and overall rating of a study.40 If a study was rated with a low risk of bias across all the six domains, it would receive an overall rating of low risk of bias.17 If one or more domains of a study were rated with a moderate risk of bias, it would receive an overall moderate risk of bias.17 If one or more domains of a study were rated with a high risk of bias, it would receive an overall high risk of bias.17
Main analysis
Standard inverse-variance random-effects meta-analysis was used to combine the overall ORs. An OR lower than one implies a lower frequency of CS in uninsured than in insured women. We calculated τ2 to measure heterogeneity between studies.41 Prespecified cut-offs of τ2 of 0.04, 0.16 and 0.36 were used to represent low, moderate and high heterogeneity between studies.42 Subgroup analysis by study design, period of data collection, state, type of CS analysed, parity, inclusion of women with previous CS, pregnancy risk of included women and level of (QUIPS) risk of bias was performed to examine between-study heterogeneity and X2 test was used to calculate p values for interaction among subgroups. Test for linear trend was performed in case of more than two ordered strata. All p values were two sided. STATA, release V.13, was used for analyses (StataCorp).
Additional analysis
We calculated CS rates among different insurance subgroups for the studies included in the analysis.
Patient involvement
No patients were involved in this study. We used data from published papers only.
Results
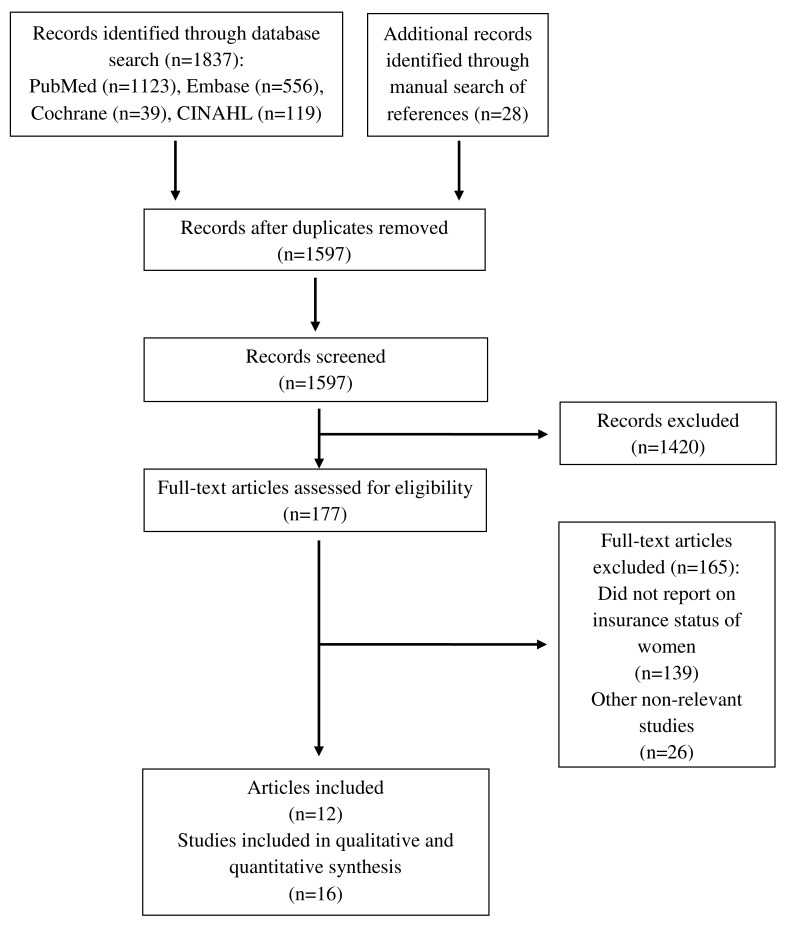
We identified a total of 1837 records: 1123 from PubMed; 556 from Embase; 39 from the Cochrane Library, 119 from CINAHL and 28 from manual search (figure 1). We removed 240 duplicates. A total of 1597 records were screened for eligibility. We performed full-text examination on 177 records. We excluded 139 that did not report insurance status of women43–181 and 26 that were otherwise irrelevant182–207 (online supplementary appendix 3). Finally, 12 records describing 16 separate studies20–22 62 208–215 including more than 8.8 million women were included in the review and meta-analysis.
Figure 1.
The flow diagram of review.
bmjopen-2018-025356supp003.pdf (166.4KB, pdf)
Characteristics of studies are presented in table 1 and online supplementary appendix 4–7. All studies were from the USA. Thirteen studies were cross-sectional and three were retrospective cohort studies. Population size of studies ranged from 9017 to 6 717 486 cases. Studies used data from years 1986 to 2011 and most studies used hospital records data (online supplementary appendix 4). Case exclusion criteria varied considerably (online supplementary appendix 5) as well as variables studies used for statistical adjustment (online supplementary appendix 6). Online supplementary appendix 7 reports evaluation of studies using QUIPS risk of bias tool. Four studies were classified with low risk of bias, two studies with moderate risk, and 10 studies with high risk of bias (online supplementary appendix 7).
Table 1.
Characteristics of included studies
| Author | Year | State | Study design | No of cases | No of hospital units | Year of data collection | Population | Sampling | Type of CS analysed |
| Stafford20 | 1990 | California | Cross-sectional | 461 066 | Not reported | 1986 | Primipara and multipara; any risk | Consecutive | Any |
| Haas et al 15 A | 1993 | Massachusetts | Cross-sectional | 57 257 | Not reported | 1984 | Primipara and multipara; any risk | Consecutive | Any |
| Haas et al 15 B | 1993 | Massachusetts | Cross-sectional | 64 346 | Not reported | 1987 | Primipara and multipara; any risk | Consecutive | Any |
| Braveman et al 209 | 1995 | California | Retrospective cohort | 213 761 | Unclear | 1991 | Primipara; no previous CS; any risk | Consecutive | Any |
| Burns et al 21 | 1995 | Arizona | Cross-sectional | 33 233 | 36 | 1989 | Primipara and multipara; any risk | Consecutive | Any |
| Onion et al 210 A | 1999 | Maine | Cross-sectional | 41 177 | Not reported | 1990–1992 | Primipara; no previous CS; any risk | Consecutive | Any |
| Onion et al 210 B | 1999 | New Hampshire | Cross-sectional | 41 401 | Not reported | 1990–1992 | Primipara; no previous CS; any risk | Consecutive | Any |
| Onion et al 210 C | 1999 | Vermont | Cross-sectional | 19 077 | Not reported | 1990–1992 | Primipara; no previous CS; any risk | Consecutive | Any |
| Aron et al 211 | 2000 | Ohio | Retrospective cohort | 25 697 | 21 | 1993–1995 | Primipara; no previous CS; any risk | Consecutive | Any |
| Grant22 A | 2005 | All states | Cross-sectional | 9017 | Not reported | 1988 | Primipara and multipara; any risk | Random | Any |
| Grant22 B | 2005 | Florida | Cross-sectional | 147 821 | Not reported | 1992 | Primipara and multipara; any risk | Consecutive | Any |
| Coonrod et al 62 | 2008 | Arizona | Cross-sectional | 28 863 | 40 | 2005 | Primipara; low risk | Consecutive | Any |
| Huesch212 | 2011 | New Jersey | Cross-sectional | 182 108 | Not reported | 2004–2007 | Primipara and multipara; no previous CS; low risk | Consecutive | Planned |
| Kozhimannil et al 103 | 2014 | All states | Cross-sectional | 6 717 486 | Over 1000 | 2002–2009 | Primipara and multipara; any risk | Random | Any |
| Huesch et al 213 | 2014 | California | Cross-sectional | 408 355 | 254 | 2010 | Primipara and multipara; no previous CS; any risk | Consecutive | Planned |
| Sebastião et al 214 | 2016 | Florida | Retrospective cohort | 412 192 | 122 | 2004–2011 | Primipara; no previous CS; low risk | Consecutive | Emergency |
CS, caesarean section.
bmjopen-2018-025356supp004.pdf (14.9KB, pdf)
bmjopen-2018-025356supp005.pdf (117.3KB, pdf)
bmjopen-2018-025356supp006.pdf (31.3KB, pdf)
bmjopen-2018-025356supp007.pdf (23.4KB, pdf)
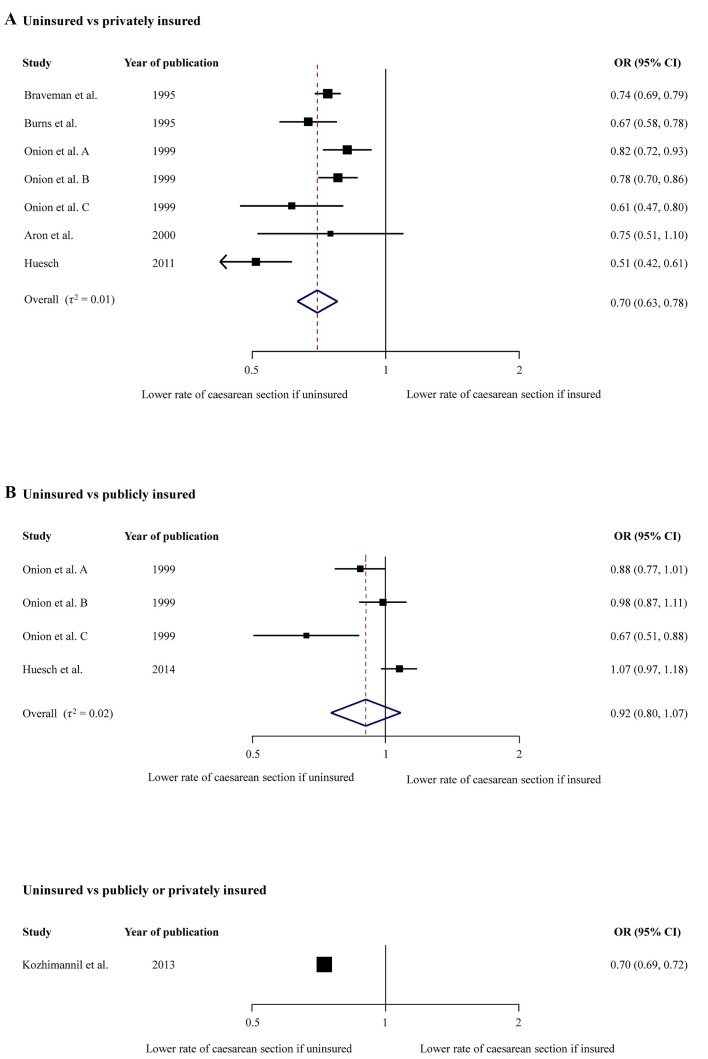
Figure 2 presents meta-analyses for primary outcome measure, that is, adjusted ORs of CS in uninsured women as compared with privately or publicly insured. Since there was a positive interaction between uninsured versus privately insured group and uninsured versus publicly insured group (p=0.016), we performed meta-analyses for each group separately. In the meta-analysis comparing uninsured with privately insured women, including seven studies in 556 454 women, we found that the odds of CS were 0.70 times lower in uninsured as compared with privately insured women (95% CI 0.63 to 0.78), with no relevant heterogeneity between studies (τ2=0.01). In meta-analysis comparing uninsured with publicly insured women, including four studies in 510 010 women, we found that the odds of CS were 0.92 times lower in uninsured as compared with publicly insured women (95% CI 0.80 to 1.07), with no relevant heterogeneity between studies (τ2=0.02). An additional study in 6 717 486 women, which did not distinguish between privately and publicly insured women,215 reported that the odds of CS were 0.70 times lower in uninsured as compared with insured women (95% CI 0.69 to 0.72).
Figure 2.
Adjusted ORs of caesarean section.
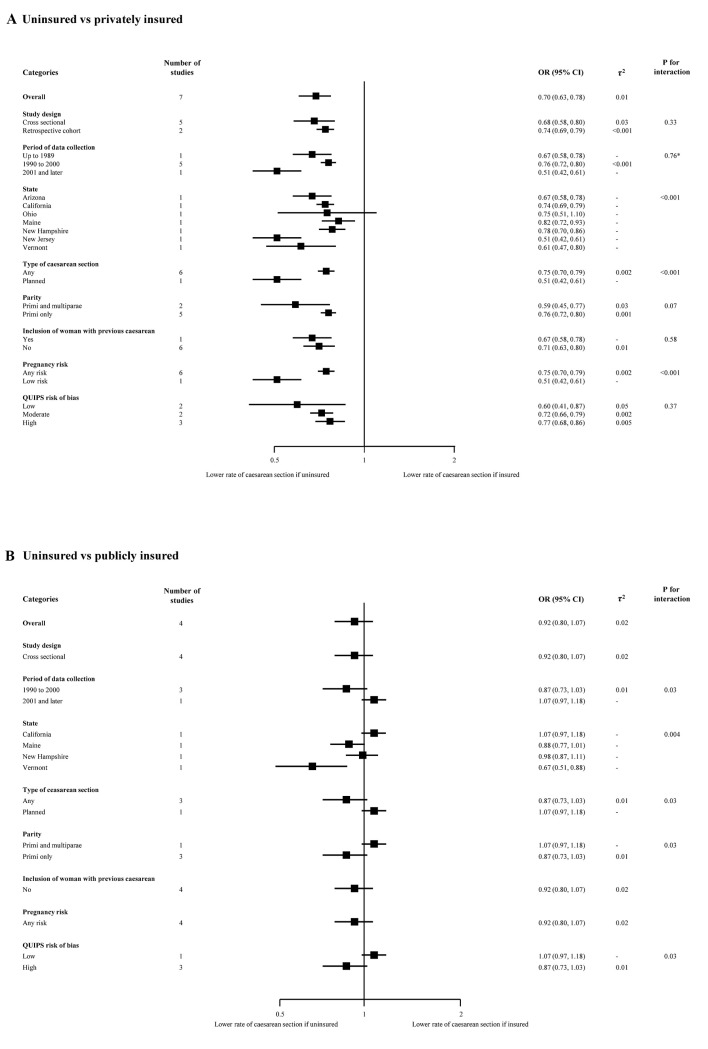
Figure 3 presents results of subgroup analyses of adjusted ORs in uninsured versus privately insured women (Figure 3A) and in uninsured versus publicly insured women (Figure 3B). In the analysis of uninsured versus privately insured women, estimates varied for subgroups state (p for interaction <0.001), type of CS (p for interaction <0.001), parity (p for interaction=0.07), and pregnancy risk (p for interaction <0.001). There was no positive trend in the period of data collection subgroup. In the lower panel, which presents subgroup analyses of adjusted ORs in uninsured versus publicly insured women, estimates varied for subgroups period of data collection (p for interaction=0.03), state (p for interaction=0.004), type of CS (p for interaction=0.03), parity (p for interaction=0.03) and QUIPS risk of bias (p for interaction=0.03).
Figure 3.
Subgroup analyses for adjusted estimates. *P for trend. QUIPS, Quality In Prognosis Studies.
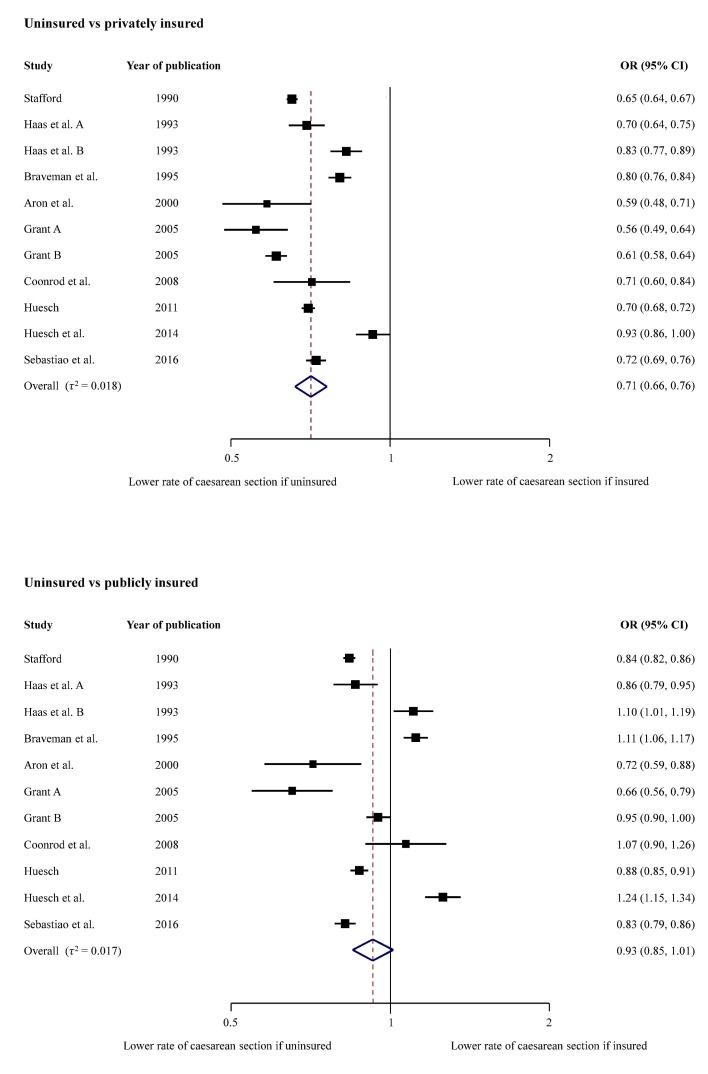
In figure 4, we present meta-analyses for crude ORs of CS in uninsured as compared with privately or publicly insured women as secondary outcome. In the meta-analysis comparing uninsured with privately insured women, including 11 studies in 2 010 483 women, we found that the odds of CS were 0.71 times lower in uninsured as compared with privately insured women (95% CI 0.66 to 0.76), with no relevant heterogeneity between studies (τ2=0.018). In the meta-analysis comparing uninsured with publicly insured women, including 11 studies in 2 010 483 women, we found that the odds of CS were 0.93 times lower in uninsured as compared with publicly insured women (95% CI 0.85 to 1.01), with no relevant heterogeneity between studies (τ2=0.017).
Figure 4.
Crude ORs of caesarean section.
Table 2 presents rates of CS among groups with different insurance status for individual studies. Six studies found CS rates for uninsured women below the 19% benchmark. One study found CS rates below the 10% benchmark. The rates of other studies range from 19.3% to 23.0%, close to 19% benchmark.
Table 2.
Caesarean section (CS) rates among groups with different insurance status
| Author | Year | State | Year of data collection | CS rate of privately insured (%) | CS rate of publicly insured (%) | CS rate of uninsured (%) |
| Stafford20 | 1990 | California | 1986 | 26.8 | 22.1 | 19.3 |
| Haas et al 15 A | 1993 | Massachusetts | 1984 | 23.0 | 19.4 | 17.2 |
| Haas et al 15 B | 1993 | Massachusetts | 1987 | 25.9 | 20.8 | 22.4 |
| Braveman et al 209 | 1995 | California | 1991 | 27.1 | 21.2 | 23.0 |
| Burns et al 21 | 1995 | Arizona | 1989 | n/a | n/a | n/a |
| Onion et al 210 A* | 1999 | Maine | 1990–1992 | 15.9 | 14.9 | 13.4 |
| Onion et al 210 B* | 1999 | New Hampshire | 1990–1992 | 16.1 | 13.2 | 13.0 |
| Onion et al 210 C* | 1999 | Vermont | 1990–1992 | 14.5 | 13.5 | 9.4 |
| Aron et al 211 | 2000 | Ohio | 1993–1995 | 17.0 | 14.2 | 10.7 |
| Grant22 A | 2005 | All states | 1988 | 27.0 | 23.7 | 17.1 |
| Grant22 B | 2005 | Florida | 1992 | 30.0 | 21.6 | 20.7 |
| Coonrod et al 62 | 2008 | Arizona | 2005 | 26.0 | 19.0 | 20.0 |
| Huesch212 | 2011 | New Jersey | 2004–2007 | 26.7 | 22.5 | 20.3 |
| Kozhimannil et al 103 | 2014 | All states | 2002–2009 | n/a | n/a | n/a |
| Huesch et al 213 | 2014 | California | 2010 | 13.9 | 10.7 | 13.0 |
| Sebastião et al 214 | 2016 | Florida | 2004–2011 | 25.2 | 22.8 | 19.7 |
*The rates are adjusted as compared with the rates from other studies which are crude rates.
Dark grey, CS rates below 10% benchmark.
Light grey, CS rates below 19% benchmark.
n/a, not applicable.
Discussion
Our systematic review and meta-analyses estimated that the overall odds of receiving a CS are on average 0.70 times lower for uninsured women as compared with privately insured women (95% CI 0.63 to 0.78), 0.92 times lower for uninsured women as compared with publicly insured women (95% CI 0.80 to 1.07) and 0.70 times lower for uninsured women as compared with privately and publicly insured women (95% CI 0.69 to 0.72). The lower odds were noticed across all subgroups of studies in subgroup analyses as well as in crude analyses.
Context
To our knowledge, this is the first meta-analysis that examines CS rates of uninsured women compared with insured women. Two recently published meta-analyses by our group reported the association of CS with for-profit status of hospitals and type of insurance.17 216 Investigating the association of for-profit versus non-profit status of hospital with the odds of CS, we found that the odds of CS were 1.41 higher in for-profit hospitals as compared with non-profit hospitals (95% CI 1.24 to 1.60).216 The findings were consistent in subgroup analyses.216 Investigating the association of CS with private insurance, we found that the odds of CS were 1.13 times higher for privately insured women compared with women covered with public insurance (95% CI 1.07 to 1.18).17 Again, the increased risk was observed across all subgroups.17
Strengths and limitations
The major strengths of our meta-analysis include an extensive literature search, screening and data extraction performed in duplicate, review and analysis of study characteristics as well as thorough quality assessment of included studies. In addition, all studies are from one country, that is, the USA, and this limits the effect of contextual factors. A major limitation is the variation across studies, in terms of the study populations characteristics (ie, parity, inclusion of women with previous CS, risk for CS), type of data used, types of CS analysed and adjusting variables used in statistical analyses. The results of this study are driven by the largest study which contains over two-thirds of the population included in this review. Only 5 out of 16 studies included in the review report data after year 2000. It should also be taken into consideration, that despite similar features, the uninsured are a diverse group of US citizens.26 27 We considered but could not make use of the Robson criteria to classify studies and analyse CS rates among the studies reviewed. Only 2 out of 16 studies could be classified using the Robson criteria.62 214 While a population-level CS rate of less than 9%, 10% or 19% suggests underuse, we cannot determine the mix of under, over and appropriate use in a specific population.
Mechanism
There are several possible explanations why uninsured women have lower odds of CS when compared with insured women. One likely factor is that financial incentives are stronger with private insurance than in the publicly insured or uninsured.17 18 These incentives result from higher payment for CS by private insurers, reimbursement arrangements that encourage more expensive procedures as means to increase profits, as well as providers’ (hospitals and individual physicians) responses to these incentives.17 70 216 The responses to incentives by hospitals exist in the form of patient scheduling policies that direct privately insured patients to profit inclined physicians.20 216 It is also a known that physicians who have a higher share of privately insured patients will tend to overuse CS.21 22 216 They do so as they perceive patients to have a higher social class, that is, able to pay higher fees or fear malpractice liability.18 111 208 216
Additional reasons are likely reflected in the comparison between uninsured and publicly insured women. A first set of reasons are related to deliberate or forced decisions of uninsured women to keep out-of-pocket payments low.18 The uninsured patients are more likely to seek less expensive care when they face the need for healthcare services.18 In the case of giving birth, this would lead to a greater preference for vaginal delivery. A second set of reasons may be discrimination of providers towards uninsured women. Providers prefer profitable, privately insured patients, a preference commonly referred to as ‘cream skimming’.21 22 216 217
Implications for uninsured women
Most studies included in our meta-analysis, including the most recent studies from California213 and Florida,214 show that rates for CS among uninsured women are below or close to the 10% and 19% benchmarks.6–8 Even in instances where the average state rates are slightly above the 19% benchmark, some hospitals service areas are likely to have CS rates lower than 19% or even 9% for uninsured women because of the well established within state variation in CS rates.5 111 Uninsured women in these areas are highly likely to be underserved with CS during delivery. Uninsured patients generally have higher unmet needs than insured patients due to access barriers.23 24 26 28 218–222 Such barriers encourage inappropriate health seeking behaviours among uninsured.23–25 32 220 223–225 Consequently, uninsured populations face higher health risks and have worse healthcare outcomes.23–26 32 218–221 223 224 226 227
The uninsured also face financial burdens which result from out-of-pocket payments that are more severe/extensive than copayments or premiums that are paid by people that are publicly or privately insured. The uninsured are known to pay higher prices for services as compared with other payers for the same care,27 228 spend a high portion of income to cover medical expenses24 (although they spend less on their health compared with patients who have insurance),26 are frequently charged for full price for healthcare services,24 228 often do not benefit from discounts from providers24 27 and face severe financial difficulties.23 24 Uninsured manage to pay only part of the costs for their care.26 The remaining costs are uncompensated costs23 26 229 230 and most of such costs are covered by the local, state or federal government,26 229 eventually resulting in tax increases.26
Implications for research and policy-making
Future studies should examine the association of a lack of insurance in pregnant women across healthcare markets with varying CS rates and assess if delivery outcomes were correspondingly worse, in the effort to investigate the presence of underuse of CS.
In parallel, policy options that could lead to improvements of insurance coverage for delivering women should be assessed in terms of their ability to address healthcare outcomes while keeping overall costs at minimum. In the past, states have adopted different strategies for covering uninsured people.24 25 39 231 While there are many known benefits to insurance coverage,23 24 32–35 37 221 224 230 232–234 other important policy aspects should be considered. At a time of rising healthcare costs,24 35 234 235 the regulation of financial incentives is crucial. A revision of payment policies should be pursued17 18 24 216 to align financial incentives with proper health outcomes.17 24 216 Reimbursement policies that would pay the same amount for CS and vaginal delivery is one option.216 236
Conclusion
CSs are less likely to be performed in uninsured women as compared with insured women. The lower odds are consistent in all subgroups and in crude analyses. While the higher rates for CS among privately insured women can be explained with financial incentives associated with private insurance, the lower odds among uninsured women draw attention at barriers to access for delivery care. In many regions, the rates for uninsured women are above, close or below the benchmarks for appropriate CS rates and imply both, underuse and overuse. Therefore, efforts to assess the delivery outcomes as well as policy options that could improve insurance coverage for women giving birth are important.
Supplementary Material
Acknowledgments
We thank Doris Kopp and Beatrice Minder for their valuable help during development of the search strategy, Arjana Shala for her help with literature search and Hossein Meyer-Troeltsch and Rand Engel for their support with editing.
Footnotes
Contributors: IH, DCG and PJ conceived and designed the study. IH and MB performed the data extraction and preparation. IH and LS analysed the data. IH, MB and LS drafted the paper, which was critically reviewed and approved by all authors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional unpublished data are available from the study.
Patient consent for publication: Not required.
References
- 1. Saini V, Brownlee S, Elshaug AG, et al. Addressing overuse and underuse around the world. The Lancet 2017;390:105–7. 10.1016/S0140-6736(16)32573-9 [DOI] [PubMed] [Google Scholar]
- 2. Berwick DM. Avoiding overuse—the next quality frontier. The Lancet 2017;390:102–4. 10.1016/S0140-6736(16)32570-3 [DOI] [PubMed] [Google Scholar]
- 3. Wennberg JE. Tracking medicine: a researcher’s quest to understand health care. 1st Edition Oxford: Oxford University Press, 2011. [Google Scholar]
- 4. Poma PA. Effects of obstetrician characteristics on cesarean delivery rates: A community hospital experience. Am J Obstet Gynecol 1999;180:1364–72. 10.1016/S0002-9378(99)70021-9 [DOI] [PubMed] [Google Scholar]
- 5. Hoxha I, Busato A, Luta X, et al. Medical Practice Variations in Reproductive, Obstetric, and Gynecological Care: Medical Practice Variations. Boston, MA: Springer US, 2016:141–60. [Google Scholar]
- 6. Molina G, Weiser TG, Lipsitz SR, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA 2015;314:2263–70. 10.1001/jama.2015.15553 [DOI] [PubMed] [Google Scholar]
- 7. Betran AP, Torloni MR, Zhang JJ, et al. WHO Statement on caesarean section rates. BJOG 2016;123:667–70. 10.1111/1471-0528.13526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Appropriate technology for birth. Lancet 1985;2:436–7. [PubMed] [Google Scholar]
- 9. Betran AP, Torloni MR, Zhang J, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health 2015;12:57 10.1186/s12978-015-0043-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Betrán AP, Ye J, Moller AB, et al. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990-2014. PLoS One 2016;11:e0148343 10.1371/journal.pone.0148343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. OECD. Health at a Glance 2017: OECD Indicators: OECD Publishing, 2017. [Google Scholar]
- 12. Betrán AP, Merialdi M, Lauer JA, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol 2007;21:98–113. 10.1111/j.1365-3016.2007.00786.x [DOI] [PubMed] [Google Scholar]
- 13. Boatin AA, Schlotheuber A, Betran AP, et al. Within country inequalities in caesarean section rates: observational study of 72 low and middle income countries. BMJ 2018;360:k55 10.1136/bmj.k55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Little SE, Orav EJ, Robinson JN, et al. The relationship between variations in cesarean delivery and regional health care use in the United States. Am J Obstet Gynecol 2016;214 735.e1–735.e8. 10.1016/j.ajog.2015.12.023 [DOI] [PubMed] [Google Scholar]
- 15. Haas S, Acker D, Donahue C, et al. Variation in hysterectomy rates across small geographic areas of Massachusetts. Am J Obstet Gynecol 1993;169:150–4. 10.1016/0002-9378(93)90152-9 [DOI] [PubMed] [Google Scholar]
- 16. Jacoby VL, Vittinghoff E, Nakagawa S, et al. Factors associated with undergoing bilateral salpingo-oophorectomy at the time of hysterectomy for benign conditions. Obstet Gynecol 2009;113:1259–67. 10.1097/AOG.0b013e3181a66c42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoxha I, Syrogiannouli L, Braha M, et al. Caesarean sections and private insurance: systematic review and meta-analysis. BMJ Open 2017;7:e016600 10.1136/bmjopen-2017-016600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keeler EB, Brodie M. Economic incentives in the choice between vaginal delivery and cesarean section. Milbank Q 1993;71:365–404. 10.2307/3350407 [DOI] [PubMed] [Google Scholar]
- 19. Haas JS, Udvarhelyi S, Epstein AM. The effect of health coverage for uninsured pregnant women on maternal health and the use of cesarean section. JAMA 1993;270:61 10.1001/jama.1993.03510010067031 [DOI] [PubMed] [Google Scholar]
- 20. Stafford RS. Cesarean section use and source of payment: an analysis of California hospital discharge abstracts. Am J Public Health 1990;80:313–5. 10.2105/AJPH.80.3.313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Burns LR, Geller SE, Wholey DR. The effect of physician factors on the cesarean section decision. Med Care 1995;33:365–82. 10.1097/00005650-199504000-00004 [DOI] [PubMed] [Google Scholar]
- 22. Grant D. Explaining source of payment differences in U.S. cesarean rates: why do privately insured mothers receive more cesareans than mothers who are not privately insured? Health Care Manag Sci 2005;8:5–17. 10.1007/s10729-005-5212-7 [DOI] [PubMed] [Google Scholar]
- 23. Eltorai AE, Eltorai MI. The risk of expanding the uninsured population by repealing the affordable care act. JAMA 2017;317:1407–8. 10.1001/jama.2017.2042 [DOI] [PubMed] [Google Scholar]
- 24. Davis K. Uninsured in America: problems and possible solutions. BMJ 2007;334:346–8. 10.1136/bmj.39091.493588.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ayanian JZ, Weissman JS, Schneider EC, et al. Unmet health needs of uninsured adults in the United States. JAMA 2000;284:2061–9. 10.1001/jama.284.16.2061 [DOI] [PubMed] [Google Scholar]
- 26. Thorpe KE. Protecting the uninsured. N Engl J Med 2004;351:1479–81. 10.1056/NEJMp048160 [DOI] [PubMed] [Google Scholar]
- 27. Melnick GA, Fonkych K. Hospital pricing and the uninsured: do the uninsured pay higher prices?. Health Aff 2008;27:w116–w122. 10.1377/hlthaff.27.2.w116 [DOI] [PubMed] [Google Scholar]
- 28. Hsu JY, Chen L, Gumer AR, et al. Disparities in the management of ectopic pregnancy. Am J Obstet Gynecol 2017;217:49.e1–49.e10. 10.1016/j.ajog.2017.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Barnett JC, Berchick ER. Health insurance coverage in the United States: 2016. Washington, DC: US Government Printing Office, 2017:P60–260. [Google Scholar]
- 30. Sommers BD, Blendon RJ, Orav EJ, et al. Changes in utilization and health among low-income adults after medicaid expansion or expanded private insurance. JAMA Intern Med 2016;176:1501–9. 10.1001/jamainternmed.2016.4419 [DOI] [PubMed] [Google Scholar]
- 31. Bauchner H. Health care in the united states: a right or a privilege. JAMA 2017;317:29 10.1001/jama.2016.19687 [DOI] [PubMed] [Google Scholar]
- 32. Loehrer AP, Chang DC, Scott JW, et al. Association of the affordable care act medicaid expansion with access to and quality of care for surgical conditions. JAMA Surg 2018;153:e175568 10.1001/jamasurg.2017.5568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Holzmacher JL, Townsend K, Seavey C, et al. Association of expanded medicaid coverage with hospital length of stay after injury. JAMA Surg 2017;152:960–6. 10.1001/jamasurg.2017.1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Davis MM, Gebremariam A, Ayanian JZ. Changes in insurance coverage among hospitalized nonelderly adults after medicaid expansion in michigan. JAMA 2016;315:2617–8. 10.1001/jama.2016.6303 [DOI] [PubMed] [Google Scholar]
- 35. Emanuel EJ. How well is the affordable care act doing?: reasons for optimism. JAMA 2016;315:1331–2. 10.1001/jama.2016.2556 [DOI] [PubMed] [Google Scholar]
- 36. Long SK, Bart L, Karpman M, et al. Sustained gains in coverage, access, and affordability under the ACA: A 2017 Update. Health Aff 2017;36:1656–62. 10.1377/hlthaff.2017.0798 [DOI] [PubMed] [Google Scholar]
- 37. Sommers BD, Maylone B, Blendon RJ, et al. Three-year impacts of the affordable care act: Improved medical care and health among low-income adults. Health Aff 2017;36:1119–28. 10.1377/hlthaff.2017.0293 [DOI] [PubMed] [Google Scholar]
- 38. Decker SL, Lipton BJ. Most newly insured people in 2014 were long-term uninsured. Health Aff 2017;36:16–20. 10.1377/hlthaff.2016.0984 [DOI] [PubMed] [Google Scholar]
- 39. Graves JA, Nikpay SS. The changing dynamics of us health insurance and implications for the future of the affordable care act. Health Aff 2017;36:297–305. 10.1377/hlthaff.2016.1165 [DOI] [PubMed] [Google Scholar]
- 40. Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing Bias in Studies of Prognostic Factors. Ann Intern Med 2013;158:280–6. 10.7326/0003-4819-158-4-201302190-00009 [DOI] [PubMed] [Google Scholar]
- 41. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. 10.1016/0197-2456(86)90046-2 [DOI] [PubMed] [Google Scholar]
- 42. da Costa BR, Jüni P. Systematic reviews and meta-analyses of randomized trials: principles and pitfalls. Eur Heart J 2014;35:3336–45. 10.1093/eurheartj/ehu424 [DOI] [PubMed] [Google Scholar]
- 43. Adhikari Dahal K, Premji S, Patel AB, et al. Variation in maternal co-morbidities and obstetric interventions across area-level socio-economic status: A cross-sectional study. Paediatr Perinat Epidemiol 2017;31:274–83. 10.1111/ppe.12370 [DOI] [PubMed] [Google Scholar]
- 44. Armstrong CE, Martínez-Álvarez M, Singh NS, et al. Subnational variation for care at birth in Tanzania: is this explained by place, people, money or drugs? BMC Public Health 2016;16 Suppl 2(S2):795 10.1186/s12889-016-3404-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bailit JL, Landon MB, Thom E, et al. The MFMU cesarean registry: impact of time of day on cesarean complications. Am J Obstet Gynecol 2006;195:1132–7. 10.1016/j.ajog.2006.06.009 [DOI] [PubMed] [Google Scholar]
- 46. Bannister-Tyrrell M, Patterson JA, Ford JB, et al. Variation in hospital caesarean section rates for preterm births. Aust N Z J Obstet Gynaecol 2015;55:350–6. 10.1111/ajo.12351 [DOI] [PubMed] [Google Scholar]
- 47. Blais R. Variations in surgical rates in Quebec: does access to teaching hospitals make a difference?. CMAJ 1993;148:1729–36. [PMC free article] [PubMed] [Google Scholar]
- 48. Brown HS. Lawsuit activity, defensive medicine, and small area variation: the case of Cesarean sections revisited. Health Econ Policy Law 2007;2:285–96. 10.1017/S1744133107004136 [DOI] [PubMed] [Google Scholar]
- 49. Butcher AH, Fos PJ, Zuniga M, et al. Racial variations in cesarean section rates: an analysis of Medicaid data in Louisiana. J Public Health Manag Pract 1997;3:41–8. [DOI] [PubMed] [Google Scholar]
- 50. Cáceres IA, Arcaya M, Declercq E, et al. Hospital differences in cesarean deliveries in Massachusetts (US) 2004-2006: the case against case-mix artifact. PLoS One 2013;8:e57817 10.1371/journal.pone.0057817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Carayol M, Blondel B, Zeitlin J, et al. Changes in the rates of caesarean delivery before labour for breech presentation at term in France: 1972-2003. Eur J Obstet Gynecol Reprod Biol 2007;132:20–6. 10.1016/j.ejogrb.2006.05.017 [DOI] [PubMed] [Google Scholar]
- 52. Carayol M, Zein A, Ghosn N, et al. Determinants of caesarean section in Lebanon: geographical differences. Paediatr Perinat Epidemiol 2008;22:136–44. 10.1111/j.1365-3016.2007.00920.x [DOI] [PubMed] [Google Scholar]
- 53. Carayol M, Zeitlin J, Roman H, et al. Non-clinical determinants of planned cesarean delivery in cases of term breech presentation in France. Acta Obstet Gynecol Scand 2007;86:1071–8. 10.1080/00016340701505242 [DOI] [PubMed] [Google Scholar]
- 54. Carlisle DM, Leake BD, Brook RH, et al. The effect of race and ethnicity on the use of selected health care procedures: a comparison of south central Los Angeles and the remainder of Los Angeles county. J Health Care Poor Underserved 1996;7:308–22. 10.1353/hpu.2010.0319 [DOI] [PubMed] [Google Scholar]
- 55. Chen C, Cheng Z, Jiang P, et al. Effect of the new maternity insurance scheme on medical expenditures for caesarean delivery in Wuxi, China: a retrospective pre/post-reform case study. Front Med 2016;10:473–80. 10.1007/s11684-016-0479-2 [DOI] [PubMed] [Google Scholar]
- 56. Chen CS, Liu TC, Chen B, et al. The failure of financial incentive? The seemingly inexorable rise of cesarean section. Soc Sci Med 2014;101:47–51. 10.1016/j.socscimed.2013.11.010 [DOI] [PubMed] [Google Scholar]
- 57. Clark SL, Belfort MA, Hankins GD, et al. Variation in the rates of operative delivery in the United States. Am J Obstet Gynecol 2007;196:526.e1–526.e5. 10.1016/j.ajog.2007.01.024 [DOI] [PubMed] [Google Scholar]
- 58. Clark SL, Perlin JB, Fraker S, et al. Association of obstetric intervention with temporal patterns of childbirth. Obstet Gynecol 2014;124:873–80. 10.1097/AOG.0000000000000485 [DOI] [PubMed] [Google Scholar]
- 59. Clarke SC, Taffel S. Changes in cesarean delivery in the United States, 1988 and 1993. Birth 1995;22:63–7. 10.1111/j.1523-536X.1995.tb00561.x [DOI] [PubMed] [Google Scholar]
- 60. Clarke SC, Taffel SM. State variation in rates of cesarean and VBAC delivery: 1989 and 1993. Stat Bull Metrop Insur Co 1996;77:28–36. [PubMed] [Google Scholar]
- 61. Clayton HB, Sappenfield WM, Gulitz E, et al. The Florida Investigation of Primary Late Preterm and Cesarean Delivery: the accuracy of the birth certificate and hospital discharge records. Matern Child Health J 2013;17:869–78. 10.1007/s10995-012-1065-0 [DOI] [PubMed] [Google Scholar]
- 62. Coonrod DV, Drachman D, Hobson P, et al. Nulliparous term singleton vertex cesarean delivery rates: institutional and individual level predictors. Am J Obstet Gynecol 2008;198:694.e1–694.e11. 10.1016/j.ajog.2008.03.026 [DOI] [PubMed] [Google Scholar]
- 63. Coulm B, Le Ray C, Lelong N, et al. Obstetric interventions for low-risk pregnant women in France: do maternity unit characteristics make a difference?. Birth 2012;39:183–91. 10.1111/j.1523-536X.2012.00547.x [DOI] [PubMed] [Google Scholar]
- 64. Campi SFdaS, Nascimento LFC. Spatial distribution of C-sections within the state of São Paulo. Revista da Associação Médica Brasileira 2014;60:419–23. [Google Scholar]
- 65. Daw JR, Sommers BD. Association of the affordable care act dependent coverage provision with prenatal care use and birth outcomes. JAMA 2018;319:579–87. 10.1001/jama.2018.0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. de Regt RH, Minkoff HL, Feldman J, et al. Relation of private or clinic care to the cesarean birth rate. N Engl J Med Overseas Ed 1986;315:619–24. 10.1056/NEJM198609043151005 [DOI] [PubMed] [Google Scholar]
- 67. Di Mario S, Cattaneo A, Gagliotti C, et al. Baby-friendly hospitals and cesarean section rate: a survey of Italian hospitals. Breastfeed Med 2013;8:388–93. 10.1089/bfm.2012.0157 [DOI] [PubMed] [Google Scholar]
- 68. Eckerlund I, Gerdtham UG. Econometric analysis of variation in cesarean section rates. A cross-sectional study of 59 obstetrical departments in Sweden. Int J Technol Assess Health Care 1998;14:774–87. 10.1017/S0266462300012071 [DOI] [PubMed] [Google Scholar]
- 69. Edmonds JK, O’Hara M, Clarke SP, et al. Variation in cesarean birth rates by labor and delivery nurses. J Obstet Gynecol Neonatal Nurs 2017;46:486–93. 10.1016/j.jogn.2017.03.009 [DOI] [PubMed] [Google Scholar]
- 70. Epstein AJ, Nicholson S. The formation and evolution of physician treatment styles: an application to cesarean sections. J Health Econ 2009;28:1126–40. 10.1016/j.jhealeco.2009.08.003 [DOI] [PubMed] [Google Scholar]
- 71. França GV, Restrepo-Méndez MC, Maia MF, et al. Coverage and equity in reproductive and maternal health interventions in Brazil: impressive progress following the implementation of the Unified Health System. Int J Equity Health 2016;15:149 10.1186/s12939-016-0445-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Garcia FA, Miller HB, Huggins GR, et al. Effect of academic affiliation and obstetric volume on clinical outcome and cost of childbirth. Obstet Gynecol 2001;97:567–76. [DOI] [PubMed] [Google Scholar]
- 73. Gates PE. Think globally, act locally: an approach to implementation of clinical practice guidelines. Jt Comm J Qual Improv 1995;21:71–85. 10.1016/S1070-3241(16)30129-8 [DOI] [PubMed] [Google Scholar]
- 74. Gittelsohn A, Powe NR. Small area variations in health care delivery in Maryland. Health Serv Res 1995;30:295–317. [PMC free article] [PubMed] [Google Scholar]
- 75. Gomes UA, Silva AA, Bettiol H, et al. Risk factors for the increasing caesarean section rate in Southeast Brazil: a comparison of two birth cohorts, 1978-1979 and 1994. Int J Epidemiol 1999;28:687–94. 10.1093/ije/28.4.687 [DOI] [PubMed] [Google Scholar]
- 76. Gonzalez-Perez GJ, Vega-Lopez MG, Cabrera-Pivaral C, et al. Caesarean sections in Mexico: are there too many?. Health Policy Plan 2001;16:62–7. 10.1093/heapol/16.1.62 [DOI] [PubMed] [Google Scholar]
- 77. Goyert GL, Bottoms SF, Treadwell MC, et al. The physician factor in cesarean birth rates. N Engl J Med Overseas Ed 1989;320:706–9. 10.1056/NEJM198903163201106 [DOI] [PubMed] [Google Scholar]
- 78. Gregory KD, Korst LM, Platt LD. Variation in elective primary cesarean delivery by patient and hospital factors. Am J Obstet Gynecol 2001;184:1521–34. 10.1067/mob.2001.115496 [DOI] [PubMed] [Google Scholar]
- 79. Gross MM, Matterne A, Berlage S, et al. Interinstitutional variations in mode of birth after a previous caesarean section: a cross-sectional study in six German hospitals. J Perinat Med 2015;43:177–84. 10.1515/jpm-2014-0108 [DOI] [PubMed] [Google Scholar]
- 80. Grytten J, Monkerud L, Hagen TP, et al. The impact of hospital revenue on the increase in Caesarean sections in Norway. A panel data analysis of hospitals 1976-2005. BMC Health Serv Res 2011;11:267 10.1186/1472-6963-11-267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Grytten J, Monkerud L, Sørensen R. Adoption of diagnostic technology and variation in caesarean section rates: a test of the practice style hypothesis in Norway. Health Serv Res 2012;47:2169–89. 10.1111/j.1475-6773.2012.01419.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Gumede S, Black V, Naidoo N, et al. Attendance at antenatal clinics in inner-city Johannesburg, South Africa and its associations with birth outcomes: analysis of data from birth registers at three facilities. BMC Public Health 2017;17(Suppl 3):443 10.1186/s12889-017-4347-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Hanley GE, Janssen PA, Greyson D. Regional variation in the cesarean delivery and assisted vaginal delivery rates. Obstet Gynecol 2010;115:1201–8. 10.1097/AOG.0b013e3181dd918c [DOI] [PubMed] [Google Scholar]
- 84. Haraldsdottir S, Gudmundsson S, Bjarnadottir RI, et al. Maternal geographic residence, local health service supply and birth outcomes. Acta Obstet Gynecol Scand 2015;94:156–64. 10.1111/aogs.12534 [DOI] [PubMed] [Google Scholar]
- 85. Heffner LJ, Elkin E, Fretts RC. Impact of labor induction, gestational age, and maternal age on cesarean delivery rates. Obstet Gynecol 2003;102:287–93. [DOI] [PubMed] [Google Scholar]
- 86. Helfand M, Zimmer-Gembeck MJ. Practice variation and the risk of low birth weight in a public prenatal care program. Med Care 1997;35:16–31. 10.1097/00005650-199701000-00002 [DOI] [PubMed] [Google Scholar]
- 87. Henke RM, Wier LM, Marder WD, et al. Geographic variation in cesarean delivery in the United States by payer. BMC Pregnancy Childbirth 2014;14:387 10.1186/s12884-014-0387-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Hopkins K, de Lima Amaral EF, Mourão AN. The impact of payment source and hospital type on rising cesarean section rates in Brazil, 1998 to 2008. Birth 2014;41:169–77. 10.1111/birt.12106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Hsu KH, Liao PJ, Hwang CJ. Factors affecting taiwanese women’s choice of cesarean section. Soc Sci Med 2008;66:201–9. 10.1016/j.socscimed.2007.07.030 [DOI] [PubMed] [Google Scholar]
- 90. Hueston WJ, Lewis-Stevenson S. Provider distribution and variations in statewide cesarean section rates. J Community Health 2001;26:1–10. 10.1023/A:1026580929659 [DOI] [PubMed] [Google Scholar]
- 91. Jessee WF, Nickerson CW, Grant WS. Assessing medical practices through PSRO cooperative studies, an evaluation of Cesarean births in nine PSRO areas. Med Care 1982;20:75–84. [DOI] [PubMed] [Google Scholar]
- 92. Johnson N, Ansell D. Variation in caesarean and instrumental delivery rates in New Zealand hospitals. Aust N Z J Obstet Gynaecol 1995;35:6–11. 10.1111/j.1479-828X.1995.tb01821.x [DOI] [PubMed] [Google Scholar]
- 93. Joyce R, Webb R, Peacock J. Predictors of obstetric intervention rates: case-mix, staffing levels and organisational factors of hospital of birth. J Obstet Gynaecol 2002;22:618–25. 10.1080/0144361021000020385 [DOI] [PubMed] [Google Scholar]
- 94. Keskimäki I, Aro S, Teperi J. Regional variation in surgical procedure rates in Finland. Scand J Soc Med 1994;22:132–8. 10.1177/140349489402200209 [DOI] [PubMed] [Google Scholar]
- 95. Khan MN, Islam MM, Shariff AA, et al. Socio-demographic predictors and average annual rates of caesarean section in Bangladesh between 2004 and 2014. PLoS One 2017;12:e0177579 10.1371/journal.pone.0177579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Kim SJ, Han KT, Kim SJ, et al. Impact of a diagnosis-related group payment system on cesarean section in Korea. Health Policy 2016;120:596–603. 10.1016/j.healthpol.2016.04.018 [DOI] [PubMed] [Google Scholar]
- 97. Kim YM, Kim SY. Factors on the gap between predicted cesarean section rate and real cesarean section rate in tertiary hospitals. Korean Journal of Women Health Nursing 2012;18:200–8. 10.4069/kjwhn.2012.18.3.200 [DOI] [PubMed] [Google Scholar]
- 98. Kimsey L, Olaiya S, Smith C, et al. Geographic variation within the military health system. BMC Health Serv Res 2017;17:271 10.1186/s12913-017-2216-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Klassen DF. Cesarean section rates: time trends and comparisons among hospital sizes, census regions, and teaching and nonteaching hospitals. PAS Reporter 1975;13. [Google Scholar]
- 100. Klemetti R, Che X, Gao Y, et al. Cesarean section delivery among primiparous women in rural China: an emerging epidemic. Am J Obstet Gynecol 2010;202:65.e1–65.e6. 10.1016/j.ajog.2009.08.032 [DOI] [PubMed] [Google Scholar]
- 101. Koroukian SM, Bush D, Rimm AA. Comparison of cesarean section rates in fee-for-service versus managed care patients in the Ohio Medicaid population, 1992-1997. Am J Manag Care 2001;7:134–42. [PubMed] [Google Scholar]
- 102. Korst LM, Gornbein JA, Gregory KD. Rethinking the cesarean rate: how pregnancy complications may affect interhospital comparisons. Med Care 2005;43:237–45. [DOI] [PubMed] [Google Scholar]
- 103. Kozhimannil KB, Arcaya MC, Subramanian SV. Maternal clinical diagnoses and hospital variation in the risk of cesarean delivery: analyses of a National US Hospital Discharge Database. PLoS Med 2014;11:e1001745 10.1371/journal.pmed.1001745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Han KT, Kim SJ, Ju YJ, et al. Do hospital characteristics influence Cesarean delivery? Analysis of National Health Insurance claim data. Eur J Public Health 2017;27:801–7. 10.1093/eurpub/ckx061 [DOI] [PubMed] [Google Scholar]
- 105. Lee K, Lee S. Effects of the DRG-based prospective payment system operated by the voluntarily participating providers on the cesarean section rates in Korea. Health Policy 2007;81:300–8. 10.1016/j.healthpol.2006.05.019 [DOI] [PubMed] [Google Scholar]
- 106. Lee Yuen Yi (Cathy), Roberts CL, Patterson JA. Unexplained variation in hospital caesarean section rates. Med J Aust 2014;200:84–5. [DOI] [PubMed] [Google Scholar]
- 107. Leung GM, Lam TH, Thach TQ, et al. Rates of cesarean births in Hong Kong: 1987-1999. Birth 2001;28:166–72. 10.1046/j.1523-536x.2001.00166.x [DOI] [PubMed] [Google Scholar]
- 108. Li HT, Luo S, Trasande L, et al. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. JAMA 2017;317:69–76. 10.1001/jama.2016.18663 [DOI] [PubMed] [Google Scholar]
- 109. Librero J, Peiró S, Calderón SM. Inter-hospital variations in caesarean sections. A risk adjusted comparison in the Valencia public hospitals. J Epidemiol Community Health 2000;54:631–6. 10.1136/jech.54.8.631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Lidegaard O, Jensen LM, Weber T. Technology use, cesarean section rates, and perinatal mortality at Danish maternity wards. Acta Obstet Gynecol Scand 1994;73:240–5. [DOI] [PubMed] [Google Scholar]
- 111. Little SE, Orav EJ, Robinson JN, et al. The relationship between variations in cesarean delivery and regional health care use in the United States. Am J Obstet Gynecol 2016;214 10.1016/j.ajog.2015.12.023 [DOI] [PubMed] [Google Scholar]
- 112. Liu TC, Chen CS, Tsai YW, et al. Taiwan’s high rate of cesarean births : impacts of national health insurance and fetal gender preference. Birth 2007;34:115–22. 10.1111/j.1523-536X.2007.00157.x [DOI] [PubMed] [Google Scholar]
- 113. Localio AR, Lawthers AG, Bengtson JM, et al. Relationship between malpractice claims and cesarean delivery. JAMA 1993;269:366–73. 10.1001/jama.1993.03500030064034 [DOI] [PubMed] [Google Scholar]
- 114. Lundsberg LS, Illuzzi JL, Gariepy AM, et al. Variation in hospital intrapartum practices and association with cesarean rate. J Obstet Gynecol Neonatal Nurs 2017;46:5–17. 10.1016/j.jogn.2016.07.011 [DOI] [PubMed] [Google Scholar]
- 115. Lutomski JE, Morrison JJ, Lydon-Rochelle MT. Regional variation in obstetrical intervention for hospital birth in the Republic of Ireland, 2005-2009. BMC Pregnancy Childbirth 2012;12:123 10.1186/1471-2393-12-123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Lutomski JE, Murphy M, Devane D, et al. Private health care coverage and increased risk of obstetric intervention. BMC Pregnancy Childbirth 2014;14:13 10.1186/1471-2393-14-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Maeda E, Ishihara O, Tomio J, et al. Cesarean section rates and local resources for perinatal care in Japan: A nationwide ecological study using the national database of health insurance claims. J Obstet Gynaecol Res 2018;44:208–16. 10.1111/jog.13518 [DOI] [PubMed] [Google Scholar]
- 118. Márquez-Calderón S, Ruiz-Ramos M, Juárez S, et al. Frecuencia de la cesárea en Andalucía: relación con factores sociales, clínicos y de los servicios sanitarios (2007-2009). Revista Española de Salud Pública 2011;85:205–15. 10.1590/S1135-57272011000200008 [DOI] [PubMed] [Google Scholar]
- 119. McKenzie L, Stephenson PA. Variation in cesarean section rates among hospitals in Washington State. Am J Public Health 1993;83:1109–12. 10.2105/AJPH.83.8.1109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Menard MK. Cesarean delivery rates in the United States. The 1990s. Obstet Gynecol Clin North Am 1999;26:275–86. 10.1016/S0889-8545(05)70074-7 [DOI] [PubMed] [Google Scholar]
- 121. Mendlovic J, Gordon ES, Haklai Z, et al. Geographic variation in selected hospital procedures and services in the Israeli health care system. Isr J Health Policy Res 2017;6 10.1186/s13584-016-0127-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Mesterton J, Ladfors L, Ekenberg Abreu A, et al. Case mix adjusted variation in cesarean section rate in Sweden. Acta Obstet Gynecol Scand 2017;96:597–606. 10.1111/aogs.13117 [DOI] [PubMed] [Google Scholar]
- 123. Mikolajczyk RT, Schmedt N, Zhang J, et al. Regional variation in caesarean deliveries in Germany and its causes. BMC Pregnancy Childbirth 2013;13:99 10.1186/1471-2393-13-99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Mindell WR, Vayda E, Cardillo B. Ten-year trends in Canada for selected operations. Can Med Assoc J 1982;127:23–7. [PMC free article] [PubMed] [Google Scholar]
- 125. Misra A. Impact of the HealthChoice program on cesarean section and vaginal birth after C-section deliveries: a retrospective analysis. Matern Child Health J 2008;12:266–74. 10.1007/s10995-007-0234-z [DOI] [PubMed] [Google Scholar]
- 126. Mitler LK, Rizzo JA, Horwitz SM. Physician gender and cesarean sections. J Clin Epidemiol 2000;53:1030–5. 10.1016/S0895-4356(00)00221-3 [DOI] [PubMed] [Google Scholar]
- 127. Mossialos E, Allin S, Karras K, et al. An investigation of Caesarean sections in three Greek hospitals: the impact of financial incentives and convenience. Eur J Public Health 2005;15:288–95. 10.1093/eurpub/cki002 [DOI] [PubMed] [Google Scholar]
- 128. Movsas TZ, Wells E, Mongoven A, et al. Does medical insurance type (private vs public) influence the physician’s decision to perform Caesarean delivery?. J Med Ethics 2012;38:470–3. 10.1136/medethics-2011-100209 [DOI] [PubMed] [Google Scholar]
- 129. Murray SF. Relation between private health insurance and high rates of caesarean section in Chile: qualitative and quantitative study. BMJ 2000;321:1501–5. 10.1136/bmj.321.7275.1501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Murray SF, Serani Pradenas F. Cesarean birth trends in Chile, 1986 to 1994. Birth 1997;24:258–63. 10.1111/j.1523-536X.1997.tb00600.x [DOI] [PubMed] [Google Scholar]
- 131. Naiditch M, Levy G, Chale JJ, et al. Cesarean sections in France: impact of organizational factors on different utilization rates]. J Gynecol Obstet Biol Reprod 1997;26:484–95. [PubMed] [Google Scholar]
- 132. Newton ER, Higgins CS. Factors associated with hospital-specific cesarean birth rates. J Reprod Med 1989;34:407–11. [PubMed] [Google Scholar]
- 133. Nicholson WK, Witter F, Powe NR. Effect of hospital setting and volume on clinical outcomes in women with gestational and type 2 diabetes mellitus. J Womens Health 2009;18:1567–76. 10.1089/jwh.2008.1114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Nigam A. The effects of institutional change on geographic variation and health services use in the U.S.A. Soc Sci Med 2012;74:323–31. 10.1016/j.socscimed.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 135. Nilsen C, Østbye T, Daltveit AK, et al. Trends in and socio-demographic factors associated with caesarean section at a Tanzanian referral hospital, 2000 to 2013. Int J Equity Health 2014;13:87 10.1186/s12939-014-0087-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Oleske DM, Glandon GL, Giacomelli GJ, et al. The cesarean birth rate: influence of hospital teaching status. Health Serv Res 1991;26:325–37. [PMC free article] [PubMed] [Google Scholar]
- 137. Ono T, Matsuda Y, Sasaki K, et al. Comparative analysis of cesarean section rates using robson ten-group classification system and lorenz curve in the main institutions in Japan. J Obstet Gynaecol Res 2016;42:1279–85. 10.1111/jog.13069 [DOI] [PubMed] [Google Scholar]
- 138. Paranjothy S, Frost C, Thomas J. How much variation in CS rates can be explained by case mix differences?. BJOG: An International Journal of Obstetrics & Gynaecology 2005;112:658–66. 10.1111/j.1471-0528.2005.00501.x [DOI] [PubMed] [Google Scholar]
- 139. Parazzini F, Cipriani S, Bulfoni G, et al. Mode of delivery and level of neonatal care in Lombardy: a descriptive analysis according to volume of care. Ital J Pediatr 2015;41:24 10.1186/s13052-015-0129-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Placek PJ, Taffel SM. Trends in cesarean section rates for the United States, 1970-78. Public Health Rep 1980;95:540–8. [PMC free article] [PubMed] [Google Scholar]
- 141. Rabilloud M, Ecochard R, Guilhot J, et al. Study of the variations of the cesarean sections rate in the Rhône-Alpes region (France): effect of women and maternity service characteristics. Eur J Obstet Gynecol Reprod Biol 1998;78:11–17. 10.1016/S0301-2115(97)00277-7 [DOI] [PubMed] [Google Scholar]
- 142. Raifman S, Cunha AJ, Castro MC. Factors associated with high rates of caesarean section in Brazil between 1991 and 2006. Acta Paediatr 2014;103:e295–e99. 10.1111/apa.12620 [DOI] [PubMed] [Google Scholar]
- 143. Rattner D. [On the hypothesis of cesarean birth rate stabilization in southeastern, Brazil]. Rev Saude Publica 1996;30:19–33. [DOI] [PubMed] [Google Scholar]
- 144. Ravindran J. Rising caesarean section rates in public hospitals in Malaysia 2006. Med J Malaysia 2008;63:434–5. [PubMed] [Google Scholar]
- 145. Renzi C, Sorge C, Fusco D, et al. Reporting of quality indicators and improvement in hospital performance: the P.Re.Val.E. Regional Outcome Evaluation Program. Health Serv Res 2012;47:1880–901. 10.1111/j.1475-6773.2012.01401.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Ribeiro VS, Figueiredo FP, Silva AA, et al. Why are the rates of cesarean section in Brazil higher in more developed cities than in less developed ones? Braz J Med Biol Res 2007;40:1211–20. 10.1590/S0100-879X2006005000130 [DOI] [PubMed] [Google Scholar]
- 147. Riddell CA, Hutcheon JA, Strumpf EC, et al. Inter-institutional Variation in Use of Caesarean Delivery for Labour Dystocia. J Obstet Gynaecol Can 2017;39:988–95. 10.1016/j.jogc.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 148. Roohan PJ, Josberger RE, Gesten FC. Risk-adjusted primary cesarean delivery rates for managed care plans in New York State, 1998. Matern Child Health J 2001;5:169–77. 10.1023/A:1011395901223 [DOI] [PubMed] [Google Scholar]
- 149. Rossignol M, Moutquin JM, Boughrassa F, et al. Preventable obstetrical interventions: how many caesarean sections can be prevented in Canada? J Obstet Gynaecol Can 2013;35:434–43. 10.1016/S1701-2163(15)30934-8 [DOI] [PubMed] [Google Scholar]
- 150. Rowe RE, Townend J, Brocklehurst P, et al. Service configuration, unit characteristics and variation in intervention rates in a national sample of obstetric units in England: an exploratory analysis. BMJ Open 2014;4:e005551 10.1136/bmjopen-2014-005551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Sarría Santamera A, Sendra Gutiérrez JM. [Evolution of cesarean section rates in Spain: 1984-1988]. Gac Sanit 1994;8:209–14. [DOI] [PubMed] [Google Scholar]
- 152. Schemann K, Patterson J, Nippita TA, et al. Variation in and factors associated with timing of low risk, pre-labour repeat caesarean sections in NSW, 2008-2011. Public Health Res Pract 2016;26:e2611608 10.17061/phrp2611608 [DOI] [PubMed] [Google Scholar]
- 153. Schemann K, Patterson JA, Nippita TA, et al. Variation in hospital caesarean section rates for women with at least one previous caesarean section: a population based cohort study. BMC Pregnancy Childbirth 2015;15:179 10.1186/s12884-015-0609-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Sentell T, Chang A, Ahn HJ, et al. Maternal language and adverse birth outcomes in a statewide analysis. Women Health 2016;56:257–80. 10.1080/03630242.2015.1088114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Shiono PH, Fielden JG, McNellis D, et al. Recent trends in cesarean birth and trial of labor rates in the United States. JAMA 1987;257:494–7. 10.1001/jama.1987.03390040110027 [DOI] [PubMed] [Google Scholar]
- 156. Shorten A, Shorten B. What happens when a private hospital comes to town? The impact of the ‘public’ to ‘private’ hospital shift on regional birthing outcomes. Women Birth 2007;20:49–55. 10.1016/j.wombi.2007.02.001 [DOI] [PubMed] [Google Scholar]
- 157. Signorelli C, Elliott P, Cattaruzza MS, et al. Trend of caesarean section in Italy: an examination of national data 1980-1985. Int J Epidemiol 1991;20:712–6. 10.1093/ije/20.3.712 [DOI] [PubMed] [Google Scholar]
- 158. Snyder CC, Wolfe KB, Loftin RW, et al. The influence of hospital type on induction of labor and mode of delivery. Am J Obstet Gynecol 2011;205:346.e1–346.e4. 10.1016/j.ajog.2011.05.004 [DOI] [PubMed] [Google Scholar]
- 159. Souza JP, Betran AP, Dumont A, et al. A global reference for caesarean section rates (C-Model): a multicountry cross-sectional study. BJOG 2016;123:427–36. 10.1111/1471-0528.13509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Sufang G, Padmadas SS, Fengmin Z, et al. Delivery settings and caesarean section rates in China. Bull World Health Organ 2007;85:755–62. 10.2471/BLT.06.035808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Tang CH, Wu MP, Liu JT, et al. Delayed parenthood and the risk of cesarean delivery--is paternal age an independent risk factor? Birth 2006;33:18–26. 10.1111/j.0730-7659.2006.00070.x [DOI] [PubMed] [Google Scholar]
- 162. Tang S, Li X, Wu Z. Rising cesarean delivery rate in primiparous women in urban China: evidence from three nationwide household health surveys. Am J Obstet Gynecol 2006;195:1527–32. 10.1016/j.ajog.2006.03.044 [DOI] [PubMed] [Google Scholar]
- 163. Tracy SK, Sullivan E, Dahlen H, et al. General obstetrics: Does size matter? A population-based study of birth in lower volume maternity hospitals for low risk women. BJOG: An International Journal of Obstetrics & Gynaecology 2006;113:86–96. 10.1111/j.1471-0528.2005.00794.x [DOI] [PubMed] [Google Scholar]
- 164. Tucker J, McVicar A, Pitchforth E, et al. Maternity care models in a remote and rural network: assessing clinical appropriateness and outcome indicators. Qual Saf Health Care 2010;19:83–9. 10.1136/qshc.2008.028894 [DOI] [PubMed] [Google Scholar]
- 165. Tussing AD, Wojtowycz MA. Health maintenance organizations, independent practice associations, and cesarean section rates. Health Serv Res 1994;29:75–93. [PMC free article] [PubMed] [Google Scholar]
- 166. Vadnais MA, Hacker MR, Shah NT, et al. Quality improvement initiatives lead to reduction in nulliparous term singleton vertex cesarean delivery rate. Jt Comm J Qual Patient Saf 2017;43:53–61. 10.1016/j.jcjq.2016.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Vankan E, Schoorel EN, van Kuijk SM, et al. Practice variation of vaginal birth after cesarean and the influence of risk factors at patient level: a retrospective cohort study. Acta Obstet Gynecol Scand 2017;96:158–65. 10.1111/aogs.13059 [DOI] [PubMed] [Google Scholar]
- 168. Vayda E, Barnsley JM, Mindell WR, et al. Five-year study of surgical rates in Ontario’s counties. Can Med Assoc J 1984;131:111–5. [PMC free article] [PubMed] [Google Scholar]
- 169. Vecino-Ortiz AI, Bardey D, Castano-Yepes RA. Pih45 multilevel analysis to measure hospital variation: The case of cesarean delivery. Value in Health 2011;14:A113 10.1016/j.jval.2011.02.629 [DOI] [PubMed] [Google Scholar]
- 170. Wang X, Hellerstein S, Hou L, et al. Caesarean deliveries in China. BMC Pregnancy Childbirth 2017;17:54 10.1186/s12884-017-1233-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Woolbright LA. Why is the cesarean delivery rate so high in Alabama? An examination of risk factors, 1991-1993. Birth 1996;23:20–5. 10.1111/j.1523-536X.1996.tb00456.x [DOI] [PubMed] [Google Scholar]
- 172. Feng XL, Xu L, Guo Y, et al. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull World Health Organ 2012;90:30–9. 10.2471/BLT.11.090399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Xirasagar S, Lin HC. Cost convergence between public and for-profit hospitals under prospective payment and high competition in Taiwan. Health Serv Res 2004;39:2101–16. 10.1111/j.1475-6773.2004.00334.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Xirasagar S, Lin HC. Maternal request CS--role of hospital teaching status and for-profit ownership. Eur J Obstet Gynecol Reprod Biol 2007;132:27–34. 10.1016/j.ejogrb.2006.05.022 [DOI] [PubMed] [Google Scholar]
- 175. Xirasagar S, Lin HC, Liu TC. Do group practices have lower caesarean rates than solo practice obstetric clinics? Evidence from Taiwan. Health Policy Plan 2006;21:319–25. 10.1093/heapol/czl015 [DOI] [PubMed] [Google Scholar]
- 176. Yang HJ, Kao FY, Chou YJ, et al. Do nurses have worse pregnancy outcomes than non-nurses? Birth 2014;41:262–7. 10.1111/birt.12118 [DOI] [PubMed] [Google Scholar]
- 177. Hong YC, Linn GC. Financial incentives and use of Cesarean delivery: Taiwan birth data 2003 to 2007. Am J Manag Care 2012;18:e35–41. [PubMed] [Google Scholar]
- 178. Zdeb MS, Therriault GD, Logrillo VM. Cesarean sections in upstate New York, 1968-1978. Am J Epidemiol 1980;112:395–403. 10.1093/oxfordjournals.aje.a113005 [DOI] [PubMed] [Google Scholar]
- 179. Zere E, Tumusiime P, Walker O, et al. Inequities in utilization of maternal health interventions in Namibia: implications for progress towards MDG 5 targets. Int J Equity Health 2010;9:16 10.1186/1475-9276-9-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Zhang S, Cardarelli K, Shim R, et al. Racial disparities in economic and clinical outcomes of pregnancy among Medicaid recipients. Matern Child Health J 2013;17:1518–25. 10.1007/s10995-012-1162-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Zwecker P, Azoulay L, Abenhaim HA. Effect of fear of litigation on obstetric care: a nationwide analysis on obstetric practice. Am J Perinatol 2011;28:277–84. 10.1055/s-0030-1271213 [DOI] [PubMed] [Google Scholar]
- 182. Brown HC, Paranjothy S, Dowswell T, et al. Package of care for active management in labour for reducing caesarean section rates in low-risk women. Cochrane Database Syst Rev 2013;103:CD004907 10.1002/14651858.CD004907.pub3 [DOI] [PubMed] [Google Scholar]
- 183. Chauhan SP, Klauser CK, Woodring TC, et al. Intrapartum nonreassuring fetal heart rate tracing and prediction of adverse outcomes: interobserver variability. Am J Obstet Gynecol 2008;199:623.e1–623.e5. 10.1016/j.ajog.2008.06.027 [DOI] [PubMed] [Google Scholar]
- 184. Chen PC, Yang MC, Chiang TL, et al. A study of cross-region admission and the distribution of regional inpatient care resources. Taiwan Journal of Public Health 2003;22:27–32. [Google Scholar]
- 185. Cheng Y, Carpenter A, Main E. 794: Large hospital-level variation in cesarean delivery rates during induction of labor. Am J Obstet Gynecol 2015;212:S384 10.1016/j.ajog.2014.10.1000 [DOI] [Google Scholar]
- 186. Cisse CT, Faye EO, de Bernis L, et al. [Cesarean sections in Senegal: coverage of needs and quality of services]. Sante 1998;8:369–77. [PubMed] [Google Scholar]
- 187. Cressie N. Regional mapping of incidence rates using spatial Bayesian models. Med Care 1993;31(5 Suppl):YS60–YS65. 10.1097/00005650-199305001-00009 [DOI] [PubMed] [Google Scholar]
- 188. da Silva AA, Bettiol H, Barbieri MA, et al. Infant mortality and low birth weight in cities of Northeastern and Southeastern Brazil. Rev Saude Publica 2003;37:693–8. [DOI] [PubMed] [Google Scholar]
- 189. Danishevski K, McKee M, Sassi F, et al. The decision to perform Caesarean section in Russia. Int J Qual Health Care 2008;20:88–94. 10.1093/intqhc/mzm070 [DOI] [PubMed] [Google Scholar]
- 190. Dimitrov A. Pro and con the trend to an increasing frequency of cesarean sections]. Akush Ginekol 1998;37:1–5. [PubMed] [Google Scholar]
- 191. Edmonds JK, Hawkins SS, Cohen BB. Variation in Vaginal Birth After Cesarean by Maternal Race and Detailed Ethnicity. Matern Child Health J 2016;20:1114–23. 10.1007/s10995-015-1897-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Emmett CL, Montgomery AA, Murphy DJ. DiAMOND Study Group. Preferences for mode of delivery after previous caesarean section: what do women want, what do they get and how do they value outcomes? Health Expect 2011;14:397–404. 10.1111/j.1369-7625.2010.00635.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Gama AdeS, Giffin KM, Angulo-Tuesta A, et al. Representações e experiências das mulheres sobre a assistência ao parto vaginal e cesárea em maternidades pública e privada. Cadernos de Saúde Pública 2009;25:2480–8. 10.1590/S0102-311X2009001100017 [DOI] [PubMed] [Google Scholar]
- 194. Haupt BJ. Deliveries in short-stay hospitals: United States, 1980. Adv Data 1982;83:1–11. [PubMed] [Google Scholar]
- 195. Hofmeyr GJ, Kulier R, West HM. Cochrane Pregnancy and Childbirth Group. External cephalic version for breech presentation at term. Cochrane Database Syst Rev 2015;91 10.1002/14651858.CD000083.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Kennare R. Why is the caesarean section rate rising?. MIDIRS Midwifery Digest 2003;13:503–8. [Google Scholar]
- 197. Krivenko CA, Chodroff C. The analysis of clinical outcomes: getting started in benchmarking. Jt Comm J Qual Improv 1994;20:260–6. 10.1016/S1070-3241(16)30070-0 [DOI] [PubMed] [Google Scholar]
- 198. Nirupam S, Yuster EA. Emergency obstetric care: measuring availability and monitoring progress. Int J Gynaecol Obstet 1995;50 Suppl 2(SUPPL. 2):S79–S88. 10.1016/0020-7292(95)02492-U [DOI] [PubMed] [Google Scholar]
- 199. Pel M, Heres MH, Hart AA, et al. Provider-associated factors in obstetric interventions. Eur J Obstet Gynecol Reprod Biol 1995;61:129–34. 10.1016/0301-2115(95)02129-U [DOI] [PubMed] [Google Scholar]
- 200. Phipps H, de Vries B, Hyett J, et al. Prophylactic manual rotation for fetal malposition to reduce operative delivery. Cochrane Database Syst Rev 2014;54:CD009298 10.1002/14651858.CD009298.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Ravindran J. Caesarean section rates in government hospitals in Malaysia, 2000-2001. Med J Malaysia 2003;58:294–5. [PubMed] [Google Scholar]
- 202. Rohrer JE. Small area analysis: descriptive epidemiology in health services research. Clin Perform Qual Health Care 1993;1:35–42. [PubMed] [Google Scholar]
- 203. Sandall J, Soltani H, Gates S, et al. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database of Systematic Reviews 2013;8 http://onlinelibrary.wiley.com/doi/. [DOI] [PubMed] [Google Scholar]
- 204. Singata M, Tranmer J, Gyte GM. Restricting oral fluid and food intake during labour. Cochrane Database Syst Rev 2013;9:CD003930 http://onlinelibrary.wiley.com/doi/ 10.1002/14651858.CD003930.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Ward L, Fenton K, Maher L. The high impact actions for nursing and midwifery. 7: Promoting normal birth. Nurs Times 2010;106:16–17. [PubMed] [Google Scholar]
- 206. Weber T. [Danish] Sectio caesarea-hvorfor varierer hyppigheden? Ugeskrift for laeger 1990;152:3143–4. [PubMed] [Google Scholar]
- 207. Wei S, Wo BL, Qi HP, et al. Early amniotomy and early oxytocin for prevention of, or therapy for, delay in first stage spontaneous labour compared with routine care. Cochrane Database Syst Rev 2013;8:CD006794 10.1002/14651858.CD006794.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Haas JS, Udvarhelyi S, Epstein AM. The effect of health coverage for uninsured pregnant women on maternal health and the use of cesarean section. JAMA 1993;270:61–4. 10.1001/jama.1993.03510010067031 [DOI] [PubMed] [Google Scholar]
- 209. Braveman P, Egerter S, Edmonston F, et al. Racial/ethnic differences in the likelihood of cesarean delivery, California. Am J Public Health 1995;85:625–30. 10.2105/AJPH.85.5.625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Onion DK, Meyer DL, Wennberg DE, et al. Primary cesarean section rates in uninsured, Medicaid and insured populations of predominantly rural northern New England. J Rural Health 1999;15:108–12. 10.1111/j.1748-0361.1999.tb00604.x [DOI] [PubMed] [Google Scholar]
- 211. Aron DC, Gordon HS, DiGiuseppe DL, et al. Variations in risk-adjusted cesarean delivery rates according to race and health insurance. Med Care 2000;38:35–44. 10.1097/00005650-200001000-00005 [DOI] [PubMed] [Google Scholar]
- 212. Huesch MD. Association between type of health insurance and elective cesarean deliveries: New Jersey, 2004-2007. Am J Public Health 2011;101:e1–e7. 10.2105/AJPH.2011.300333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Huesch MD, Currid-Halkett E, Doctor JN. Measurement and risk adjustment of prelabor cesarean rates in a large sample of California hospitals. Am J Obstet Gynecol 2014;210:443.e1–7. 10.1016/j.ajog.2013.12.007 [DOI] [PubMed] [Google Scholar]
- 214. Sebastião YV, Womack L, Vamos CA, et al. Hospital variation in cesarean delivery rates: contribution of individual and hospital factors in Florida. Am J Obstet Gynecol 2016;214:123.e1–123.e18. 10.1016/j.ajog.2015.08.027 [DOI] [PubMed] [Google Scholar]
- 215. Kozhimannil KB, Shippee TP, Adegoke O, et al. Trends in hospital-based childbirth care: the role of health insurance. Am J Manag Care 2013;19:e125–32. [PMC free article] [PubMed] [Google Scholar]
- 216. Hoxha I, Syrogiannouli L, Luta X, et al. Caesarean sections and for-profit status of hospitals: systematic review and meta-analysis. BMJ Open 2017;7:e013670 10.1136/bmjopen-2016-013670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Barros PP. Cream-skimming, incentives for efficiency and payment system. J Health Econ 2003;22:419–43. 10.1016/S0167-6296(02)00119-4 [DOI] [PubMed] [Google Scholar]
- 218. Halpern MT, Ward EM, Pavluck AL, et al. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol 2008;9:222–31. 10.1016/S1470-2045(08)70032-9 [DOI] [PubMed] [Google Scholar]
- 219. Pezzi TA, Schwartz DL, Mohamed ASR, et al. Barriers to combined-modality therapy for limited-stage small cell lung cancer. JAMA Oncol 2018;4:e174504 10.1001/jamaoncol.2017.4504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Ayanian JZ, Kohler BA, Abe T, et al. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med 1993;329:326–31. 10.1056/NEJM199307293290507 [DOI] [PubMed] [Google Scholar]
- 221. Koh H, Tavenner M. Connecting to health insurance coverage. JAMA 2013;309:1893–4. 10.1001/jama.2013.3469 [DOI] [PubMed] [Google Scholar]
- 222. Decker SL, Kostova D, Kenney GM, et al. Health status, risk factors, and medical conditions among persons enrolled in medicaid vs uninsured low-income adults potentially eligible for medicaid under the affordable care act. JAMA 2013;309:2579–86. 10.1001/jama.2013.7106 [DOI] [PubMed] [Google Scholar]
- 223. Decker SL, Kenney GM, Long SK. Characteristics of uninsured low-income adults in states expanding vs not expanding Medicaid. JAMA Intern Med 2014;174:988–9. 10.1001/jamainternmed.2014.518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Hellinger FJ. In four ACA expansion states, the percentage of uninsured hospitalizations for people with hiv declined, 2012-14. Health Aff 2015;34:2061–8. 10.1377/hlthaff.2015.0718 [DOI] [PubMed] [Google Scholar]
- 225. Newton MF, Keirns CC, Cunningham R, et al. Uninsured adults presenting to US emergency departments: assumptions vs data. JAMA 2008;300:1914–24. 10.1001/jama.300.16.1914 [DOI] [PubMed] [Google Scholar]
- 226. Shin JY, Yoon JK, Shin AK, et al. Association of insurance and community-level socioeconomic status with treatment and outcome of squamous cell carcinoma of the pharynx. JAMA Otolaryngol Head Neck Surg 2017;143:899–907. 10.1001/jamaoto.2017.0837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Ellis L, Canchola AJ, Spiegel D, et al. Trends in cancer survival by health insurance status in california From 1997 to 2014. JAMA Oncol 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Xu T, Park A, Bai G, et al. Variation in emergency department vs internal medicine excess charges in the United States. JAMA Intern Med 2017;177:1139–45. 10.1001/jamainternmed.2017.1598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Colvin JD, Hall M, Berry JG, et al. Financial loss for inpatient care of medicaid-insured children. JAMA Pediatr 2016;170:1055–62. 10.1001/jamapediatrics.2016.1639 [DOI] [PubMed] [Google Scholar]
- 230. Dranove D, Garthwaite C, Ody C. Uncompensated Care Decreased At Hospitals In Medicaid Expansion States But Not At Hospitals In Nonexpansion States. Health Aff 2016;35:1471–9. 10.1377/hlthaff.2015.1344 [DOI] [PubMed] [Google Scholar]
- 231. Blavin F, Karpman M, Kenney GM, et al. Medicaid versus marketplace coverage for near-poor adults: Effects on out-of-pocket spending and coverage. Health Aff 2018;37:299–307. 10.1377/hlthaff.2017.1166 [DOI] [PubMed] [Google Scholar]
- 232. Sommers BD, Gunja MZ, Finegold K, et al. Changes in self-reported insurance coverage, access to care, and health under the affordable care act. JAMA 2015;314:366–74. 10.1001/jama.2015.8421 [DOI] [PubMed] [Google Scholar]
- 233. Jacobs PD, Duchovny N, Lipton BJ. Changes In Health Status And Care Use After ACA Expansions Among The Insured And Uninsured. Health Aff 2016;35:1184–8. 10.1377/hlthaff.2015.1539 [DOI] [PubMed] [Google Scholar]
- 234. Mann C, Osius E. MEdicaid’s new role in the health care system. JAMA 2015;314:343–4. 10.1001/jama.2015.8433 [DOI] [PubMed] [Google Scholar]
- 235. James BC, Savitz LA. How Intermountain trimmed health care costs through robust quality improvement efforts. Health Aff 2011;30:1185–91. 10.1377/hlthaff.2011.0358 [DOI] [PubMed] [Google Scholar]
- 236. Brown JR, Sox HC, Goodman DC. Financial incentives to improve quality: skating to the puck or avoiding the penalty box? JAMA 2014;311:1009–10. 10.1001/jama.2014.421 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-025356supp001.pdf (6.1KB, pdf)
bmjopen-2018-025356supp002.pdf (132.4KB, pdf)
bmjopen-2018-025356supp003.pdf (166.4KB, pdf)
bmjopen-2018-025356supp004.pdf (14.9KB, pdf)
bmjopen-2018-025356supp005.pdf (117.3KB, pdf)
bmjopen-2018-025356supp006.pdf (31.3KB, pdf)
bmjopen-2018-025356supp007.pdf (23.4KB, pdf)