Abstract
Introduction:
Sensorineural hearing loss (SNHL) has been reported to occur at increased frequency in the pediatric sickle cell disease (SCD) population, likely secondary to ototoxic medication regimens and repeat sickling events that lead to end organ damage. Risk and protective factors of SNHL in this population are not fully characterized. The objective of this study was to describe audiology results in children with SCD and the prevalence and sequelae of SNHL.
Methods:
A comprehensive clinical database of 2600 pediatric SCD patients treated at 1 institution from 2010–16 was retrospectively reviewed to identify all patients who were referred for audiologic testing. Audiologic test results, patient characteristics, and SCD treatments were reviewed.
Results:
181 SCD children (97 male, 153 HbSS) underwent audiologic testing, with 276 total audiology encounters, ranging 1–9 per patient. Mean age at first audiogram was 8.9 ± 5.2 years. 29.8% had prior cerebrovascular infarct and an additional 25.4% had prior abnormal transcranial Doppler screens documented at time of first audiogram. Overall, 13.3% had documented hearing loss, with 6.6% SNHL. Mean pure tone average (PTA) among patients with SNHL ranged from mild to profound hearing loss (Right: 43.3 ± 28.9, Left: 40.8 ± 29.7), sloping to more severe hearing loss at higher frequencies.
Conclusions:
Hearing loss was identified in a significant subset of children with SCD and the hearing loss ranged from normal to profound. Though the overall prevalence of SNHL in SCD patients was low, baseline audiology screening should be considered.
Keywords: Sickle cell disease, Sensorineural hearing loss
1. Introduction
Sickle cell disease (SCD) is among one of the most common hemoglobinopathies worldwide and currently affects 1 in 400 African Americans in the United States [1]. SCD results from an amino acid substitution (valine for glutamic acid) on the beta chain of hemoglobin, which results in hemoglobin S. The term SCD encompasses several subtypes of disease, including the homozygous subtype (HbSS), the hemoglobin C variant (HbSC), and sickle cell thalassemia (HbS Beta-Thal) [2].
The mutation resulting in hemoglobin S results in a state of chronic anemia and repeated events of vaso-occlusion [3]. Due to the pathophysiology of SCD, red blood cells are more rigid, have a largely reduced lifespan (20 days compared to 120 days), and are unable to carry oxygen as efficiently compared to normal red blood cells [2]. Over time, this can lead to severe damage and possible failure of multiple end organs, including a largely increased risk for early stroke, and a reduced quality of life due to repeated bouts of pain crises.
A treatment option for patients to reduce stroke risk in SCD patients is chronic transfusion therapy. However, this can result in iron overload and resultant organ damage secondary to this accumulation [4]. This introduces the need for iron chelation therapy, of which multiple options are available, including: Deferoxamine, Deferiprone, Deferasirox, and a combination of these regimens [4]. Despite the necessity and the clinical improvement resultant from these treatments, there are major side effects associated with iron chelation, including sensorineural hearing loss (SNHL). It is important to remember though that stroke is also a possible cause of SNHL in SCD patients. This often makes it difficult to determine the etiology of SNHL in this patient population, as patients on chelation are likely to be at increased risk for stroke or may have already had a prior stroke.
Hearing loss secondary to treatment and end organ damage of SCD occurs likely due to hypoxia or infarction of the Organ of Corti secondary to sickled red blood cells [5]. The Organ of Corti is particularly sensitive to hypoxia and infarction due to the large metabolic requirement necessary to maintain the ionic balance of endolymph in the inner ear coupled with a low tolerance for anaerobic metabolism [6,7]. Loss of hearing secondary to hypoxia and infarction more commonly affects higher frequency hearing [2].
The occurrence of SNHL has been identified in patients with SCD. However, SNHL development in the pediatric SCD population has not yet been fully characterized. Specifically, risk and protective factors associated with SNHL in this patient population remain unknown. To further assess SNHL development in this population, we performed a retrospective analysis of patient characteristics, audiometry screens, and SNHL development in pediatric SCD patients.
2. Methods
A database of SCD patients followed at a pediatric tertiary referral center from 2010 to 2016 was reviewed. Out of approximately 2600 SCD patients in the database, only those who met study criteria were included in this retrospective review. To meet inclusion criteria, patients were required to have a SCD diagnosis of any genotype and have a referral for audiology testing during the study period. Patients were excluded from the study if they had audiology referrals but did not complete the visit.
Patient demographics, clinical characteristics, and audiology test results (including newborn screen results) were collected. Specifically, descriptions and dates of previous infarction and history of abnormal trans-cranial doppler screens were recorded. Results of audiology screenings were recorded, including: range of hearing frequencies tested, corresponding hearing thresholds, side specific pure tone averages, and percentage of patients with absent distortion product otoacoustic emissions (DPOAE)s. To further elaborate, we calculated pure tone averages from audiogram results. Depending on patient age, different hearing assessments were conducted and reviewed. Soundfield testing was conducted on young children who were unable to follow tasks surrounding audiogram testing. Pure tone averages were also collected from soundfield testing, but it should be noted that these results may be less accurate as there are higher inaccuracies associated with soundfield testing.
This study was IRB approved with a waiver of consent of patients included in the study. Descriptive statistics were used to describe patient demographics, clinical characteristics, and audiology screening results. All analyses were conducted using Microsoft Excel, version 14.4.
3. Results
181 patients (153 HbSS, 19 HbSC, 9 HbS-Beta Thal) from the sickle cell database met study criteria for the period of interest and were included in this retrospective study. Demographic information and clinical characteristics at time of first audiogram are represented in Table 1. Mean age at first audiogram was 8.9 ± 5.2 years. The majority of patients (58%(were referred to audiology testing due to hearing monitoring in the presence of an ototoxic medication regimen. There was an approximately even split between male and female patients (53.6% vs. 46.4%). 96% of patients passed a newborn hearing screen. 55.8% of patients were on chronic transfusion therapy, 25.4% of patients had a previous abnormal transcranial Doppler screen, and an additional 29.8% of patients had a previous cerebrovascular accident prior to first audiology screening.
Table 1.
Demographics and clinical characteristics of children with sickle cell disease at time of first audiogram, 2010–2016.
| Parameter | Number of Patients (total n = 181) (%) | Mean ± SD (Range) |
|---|---|---|
| Mean age at first audiogram (years) | 181 | 8.9 ± 5.2 (0–19.6) |
| Mean # of audiograms received | 181 | 1.5 ± 1 (1–9) |
| SCD Genotype: HbSS | 153 (84.5%) | |
| SCD Genotype: HbS Beta Thalassemia | 9 (5.0%) | |
| Sex (male) | 97 (53.6%) | |
| Newborn hearing screen: | 174 (96.1%) | |
| - Passed | 167 (96.0%) | |
| - Failed | 7 (4.0%) | |
| Indication for audiology test: | 181 (100%) | |
| - Hearing concern | 48 (26.5%) | |
| - History of cerebrovascular accident | 5 (2.8%) | |
| - History of ototoxic medication regimen | 105 (58.0%) | |
| - History of recurrent ear infections | 9 (5.0%) | |
| - To establish a hearing baseline | 14 (7.7%) | |
| Indication for transfusion: | ||
| - History of cerebrovascular accident (yes) | 54 (29.8%) | |
| - Abnormal transcranial doppler (yes) | 46 (25.4%) | |
| - On chronic transfusion therapy (yes) | 101 (55.8%) | |
| - SNHL | 12 (6.6%) |
Based on audiology testing, 12 patients (6.6%) had SNHL. Table 2 portrays demographic and clinical characteristics of the 12 patients with SNHL in our study. 10 of 12 patients (83.3%) had the HbSS subtype of SCD. Three patients (25%) had documented cerebrovascular disease (CVD) prior to the first audiogram.
Table 2.
Case analysis of pediatric sickle cell patients with senorineural hearing loss.
| Pt | Age at audiogram (years) | Passed newborn screen | Sex | Genotype | CVD | Abnormal TCD* | On chronic transfusion | R. PTA (dB HL) | L. PTA (dB HL) | DPOAEs (Hz) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2.4 | Yes | M | SC | No | No | No | 48.8 | 47.5 | Not tested |
| 2 | 6.7 | Yes | F | SS | No | No | Yes | 72.5 | 77.7 | Absent 1500–10,000 |
| 3 | 17.6 | Yes | M | SS | Yes | Yes | Yes | 31.3 | 33.8 | Not tested |
| 4 | 14.5 | Yes | F | SS | No | No | No | Not tested | Not tested | Absent 1000–6000 |
| 5 | 8.1 | N/A | F | SC | No | No | No | 100 | 16.3 | Present 1000–10,000 |
| 6 | 15.8 | Yes | M | SS | Yes | No | No | 18.8 | 23.8 | Absent 6000–10,000 |
| 7 | 1.8 | N/A | M | SS | No | No | No | 71.3 | 55 | Absent 2000–6000 |
| 8 | 0.9 | No | F | SS | No | No | No | Not tested | Not tested | Absent 1500–5000 |
| 9 | 14.2 | N/A | F | SS | No | Yes | No | 32.5 | 100 | Not tested |
| 10 | 2.3 | Yes | M | SS | No | No | No | 23.8 | 32.5 | Absent 1000–6000 |
| 11 | 8.8 | Yes | M | SS | No | Yes | Yes | 20 | 12.5 | Absent 5000–10,000 |
| 12 | 13.2 | N/A | M | SS | Yes | No | No | 13.8 | 8.8 | Present 1500–10,000 |
TCD = Transcranial Doppler.
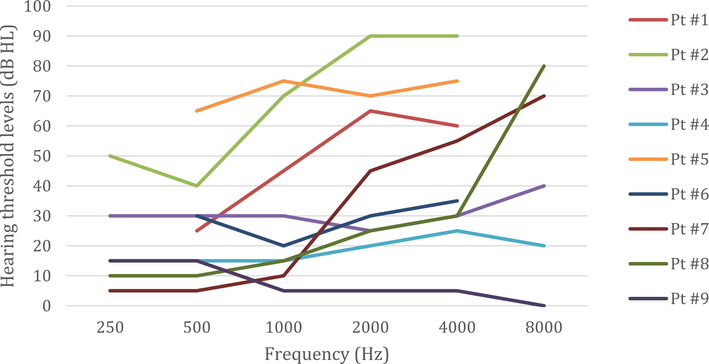
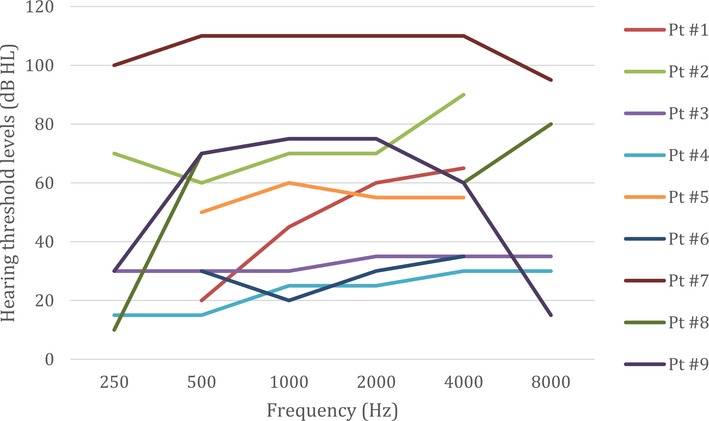
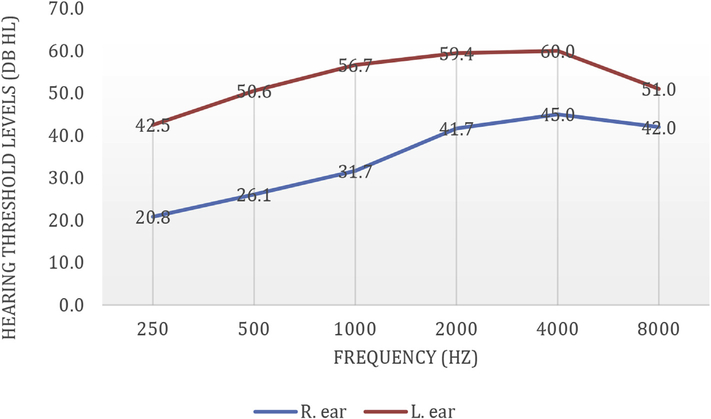
SNHL in these 12 patients is further characterized in Table 3. The average pure tone average in the right ear is 43.3 ± 28.9 dB HL, with two patients experiencing severe hearing loss and one patient experiencing profound hearing loss in this ear. The average pure tone average in the left ear is 40.8 ± 29.7 dB, with one patient experiencing severe hearing loss and one patient experiencing profound hearing loss in this ear. Seven patients (out of 9 tested) had absent DPOAEs for at least some of the range tested. Fig. 1 and Fig. 2 portray hearing thresholds (from 250 to 8000 Hz) of SCD patients with SNHL, right and left ear respectively. Fig. 3 portrays the average hearing thresholds of these patients.
Table 3.
Demographics and hearing loss characteristics in sickle cell patients with sensorineural hearing loss.
| Parameter | Number of Patients (n =12) (%) | Mean ± SD (Range) |
|---|---|---|
| Sex (male) | 7 (58.3%) | |
| Mean age at first audiogram (years) | 12 | 8.8 ± 6.1 (0.9–17.6) |
| Genotype HbSS | 10 (83.3%) | |
| Genotype HbSC | 2 (16.7%) | |
| History of cerebrovascular disease | 3 (25%) | |
| History of abnormal transcranial Doppler screen | 3 (25%) | |
| R. Ear Average Pure Tone Average (dB HL):a | 10 | 43.3 ± 28.9 (13.8–100) |
| Normal hearing (< 20 dB HL) | 2 (20%) | |
| Mild hearing loss (20–40 dB HL) | 4 (40%) | |
| Moderate hearing loss (40–60 dB HL) | 1 (10%) | |
| Severe hearing loss (60–80 dB HL) | 2 (20%) | |
| Profound hearing loss (> 80 dB HL) | 1 (10%) | |
| L. Ear Average Pure Tone Average (dB HL):a | 10 | 40.8 ± 29.7 (8.8–100) |
| Normal hearing (< 20 dB HL) | 3 (30%) | |
| Mild hearing loss (20–40 dB HL) | 3 (30%) | |
| Moderate hearing loss (40–60 dB HL) | 2 (20%) | |
| Severe hearing loss (60–80 dB HL) | 1 (10%) | |
| Profound hearing loss (> 80 dB HL) | 1 (10%) | |
| Absent DPOAEsb | 7 of 9 tested (77.8%) |
Pure tone averages could not be calculated in two patients with SNHL, as at least one hearing frequency was missing from 500 to 2000 Hz.
Counted as absent, if absent at any range within the tested range, suggestive of abnormal outer hair cell function.
Fig. 1.
Right ear hearing thresholds in pediatric patients with sickle cell disease and sensorineural hearing loss, (n =9).
*Though there were 12 patients with documented SNHL, only 9 patients were included in Fig. 1, as 3 patients only had summary reports available in the EMR and thus did not have specific frequencies documented. These 3 patients were excluded from the figure above.
Fig. 2.
Left ear hearing thresholds in pediatric patients with sickle cell disease and sensorineural hearing loss, (n =9).
*Though there were 12 patients with documented SNHL, only 9 patients were included in Fig. 2, as 3 patients only had summary reports available in the EMR and thus did not have specific frequencies documented. These 3 patients were excluded from the figure above.
Fig. 3.
Average hearing thresholds of pediatric patients with sickle cell disease and sensorineural hearing loss, (n = 9).
*Though there were 12 patients with documented SNHL, only 9 patients were included in Fig. 3, as 3 patients only had summary reports available in the EMR and thus did not have specific frequencies documented. These 3 patients were excluded from the figure above.
4. Discussion
SNHL is a well-known complication in patients with SCD [6]. Hearing loss in this patient population has been documented to be bilateral, ranging from mild to profound. The pathogenesis of SNHL development is well documented, thought to occur secondary to hypoxia of the Organ of Corti in the inner ear [7]. However, the prevalence and possible risk and protective factors associated with SNHL development have not been fully explored in the SCD pediatric population.
In our study, overall prevalence of SNHL was 6.6% (12 out of 181 patients), though due to complex medical history, the etiology of SNHL remains uncertain in these patients. In these 12 patients, only one patient did not pass a newborn hearing screen, though hearing screen results were not available for 25% of these patients. This suggests that the hearing loss in these patients was acquired later in life. In this setting, it is important to remember that we only obtained results from patients who were referred for and completed audiology testing. Looking at our data, 58% of patients were referred secondary to monitoring of hearing while on an ototoxic medication regimen, likely chelation therapy, which is often started in patients with SCD who need chronic transfusion therapy to quell symptoms of SCD.
Prevalence of SNHL in SCD patients is wide ranging in the literature, ranging from 12 to 66% [6]. However, these studies have largely looked at the adult population who may also develop SNHL related to environmental and traumatic causes. In the 12 patients with SNHL, the average PTAs were similar in the both ears suggesting that both co-chleas were exposed to the same ototoxic conditions. Hearing loss in this pediatric SCD patient population was manifested as high frequency (6000–8000) to bilateral profound.
Review of the medical records of these SCD patients revealed that 3 of 12 patients with SNHL all had a prior history of CVD, 2 of whom were on chronic transfusion therapy. In addition, 3 of the twelve patients had a prior record of abnormal transcranial doppler screens, Although there is a noticeable association between abnormal TCD and CVD in SCD patients with SNHL, there is insufficient data to demonstrate causality. As seen in Fig. 1, hearing threshold levels in pediatric patients with SNHL slope to increased severity at higher frequencies. Fig. 3 depicts the average hearing thresholds of patients with SNHL, stratified by right and left ear respectively. In our patient population, the left ear consistently displayed more severe hearing loss in all tested frequencies (250 Hz–8000 Hz). This finding may be due to a variety of factors, not limited to past neurological insults in these patients and other pertinent past medical history as hearing loss in SCD patients is a spectrum with many associated factors. Even so, a baseline audiologic screening in pediatric SCD patients may prove beneficial as higher frequency hearing loss may not be detected until hearing loss is more severe in everyday scenarios [8]. The limitations of this study include its retrospective nature. As data between 2010 and 2016 was reviewed retrospectively in the electronic medical record (EMR), our study team did not have access to audiologic testing that was performed prior to implementation of the EMR at our institution. Another limitation of our study includes an inherent selection bias, as patients included in our study received and completed an audiology referral. This introduces a selection bias as patients who were referred for audiology testing may have more severe sequelae of SCD. It is also important to acknowledge the limitations surrounding audiology screens in infants and young children. Of the 12 patients with SNHL, 4 had an audiologic screen younger than three years old. It would prove beneficial to follow these children as they age to perform more detailed and rigorous audiologic testing.
5. Conclusions
In conclusion, the results of our investigation suggest that the overall prevalence of SNHL in SCD patients was lower than reported in the adult population, though higher than that reported in the general pediatric population. Due to the increased prevalence in the SCD population, the importance of baseline audiology screening to identify possible hearing loss in this should be considered. Prospective studies investigating a large cohort of SCD patients with SNHL should be conducted to further characterize possible risk and protective factors in this patient population.
Footnotes
Data
Relevant datasets have been uploaded to Mendeley. https://doi.org/10.17632/fmpt4h773w.1.
Declarations of interest
None.
References
- [1].Pass KA, Lane PA, Fernhoff PM, et al. , US newborn screening system guidelines II: follow-up of children, diagnosis, management, and evaluation. Statement of the Council of Regional Networks for Genetic Services (CORN), J. Pediatr. 137 (2000) S1–S46. [DOI] [PubMed] [Google Scholar]
- [2].Okbi H, Alkindi S, Abri R, Mathew J, Nagwa A, Pathare A, Sensorineural hearing loss in sickle cell disease - a prospective study from Oman, Laryngoscope (2010) 392–396. [DOI] [PubMed] [Google Scholar]
- [3].Wun T, Hassell K, Best practices for transfusion for patients with sickle cell disease, Hematol. Rep 1 (2010) 22. [Google Scholar]
- [4].Tanphaichitr A, Kusuwan T, Limviriyakul S, et al. , Incidence of ototoxicity in pediatric patients with transfusion-dependent thalassemia who are less well-chelated by mono- and combined therapy of iron chelating agents, Hemoglobin 38 (2014) 345–350. [DOI] [PubMed] [Google Scholar]
- [5].Mgbor N, Emodi I, Sensorineural hearing loss in Nigerian children with sickle cell disease, Int. J. Pediatr. Otorhinolaryngol. 68 (2004) 1413–1416. [DOI] [PubMed] [Google Scholar]
- [6].A A, F O, O B, Hearing thresholds in sickle cell anemia-emerging new trends.pdf, J. Natl. Med. Assoc 97 (2005). [PMC free article] [PubMed] [Google Scholar]
- [7].Miller JM, Dengerink H, Control of inner ear blood flow, Am. J. Otolaryngol 9 (1988) 302–316. [DOI] [PubMed] [Google Scholar]
- [8].Wong AC, Ryan AF, Mechanisms of sensorineural cell damage, death and survival in the cochlea, Front. Aging Neurosci. 7 (2015) 58. [DOI] [PMC free article] [PubMed] [Google Scholar]