ABSTRACT
Background: There is increasing interest in understanding racial differences in adiposity in specific body depots as a way to explain differential health risks associated with obesity.
Objective: Our aim was to examine the differences in abdominal visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) between white and African American adults.
Design: The sample included 1967 adults aged 18–84 y, including 790 white women, 435 African American women, 606 white men, and 136 African American men. Total body fat was measured by using dual-energy X-ray absorptiometry, whereas abdominal VAT and SAT cross-sectional areas (L4–L5 level) were measured by using computed tomography. Sex-specific differences in SAT and VAT between racial groups were analyzed by the use of general linear models, which controlled for age and total body fat. Additional models tested for racial differences in VAT and SAT and controlled for age, total body fat, smoking, and menopausal status. Statistical significance was accepted at P < 0.05.
Results: Abdominal VAT was significantly higher in white than in African American men and women, even after adjustment for covariates. White women had significantly lower SAT than did African American women, both before and after adjustment for covariates. White men had significantly higher SAT than did African American men, but after adjustment for covariates, their SAT was lower than that of African American men.
Conclusions: Abdominal visceral adiposity is significantly greater in white men and women. After adjustment for covariates, white men and women had significantly lower SAT than did African American men and women. The results of this study highlight the heterogeneity of human body fat distribution across racial groups.This trial was registered at clinicaltrials.gov as NCT00959270.
See corresponding editorial on page 1.
INTRODUCTION
A major public health goal in the United States is to significantly reduce racial disparities in health (1). In 2003, white men and women could expect to live 6.3 and 4.5 y longer than African American men and women, respectively, under current mortality patterns (2, 3). A total of 51% and 64% of the racial gap in life expectancy in men and women, respectively, can be explained by differences in mortality rates from diabetes, cardiovascular disease, and cancer (2). Thus, it is clear that efforts to reduce racial disparities in mortality should focus on understanding and reducing disparities in chronic disease rates. The causes of these racial disparities are difficult to explain as they likely arise from complex interactions between socioeconomic position, behavior, and biology.
Recent data suggest that racial differences in the prevalence of generalized obesity [body mass index (BMI; in kg/m2) ≥30] exist. Among adults, the prevalence of obesity in the 2003–2004 National Health and Nutrition Examination Survey (NHANES) was 30.6% among white Americans and 45% among African Americans (4). These differences are also evident during childhood and adolescence as the prevalence of generalized obesity (BMI ≥95th percentile) among those 2–19 y of age was 16.3% among white Americans and 20.0% among African Americans (4). The degree to which these racial differences in the prevalence of general obesity contribute to the differential chronic disease burden is currently unknown.
There is increasing interest in defining excess adiposity in specific body depots as a way to explicate the health risks of obesity. For example, abdominal adiposity, in particular visceral adipose tissue (VAT), has been identified as a marker of health risk with potentially greater specificity than total fat mass or generalized obesity (5). Given the complex nature of measuring depot-specific adipose tissue in living humans, relatively few studies have examined racial differences in abdominal adiposity by using magnetic resonance imaging or computed tomography (CT). The existing evidence indicates that African American men have lower amounts of VAT compared with white men (6–11), even when adjusting for total body fat (8–10). However, racial differences in VAT are not as clear in women. Six studies have reported that African American women have lower VAT amounts than white women (6, 10–14), and 5 studies have reported that differences are not significant (7–9, 15, 16). Racial differences in abdominal subcutaneous adipose tissue (SAT) mass (6, 9, 11, 13) appear to be minimal. Three studies have reported higher amounts of abdominal SAT in African American women compared with white women; however, these studies did not adjust for total adiposity, and the African American women in these studies also had significantly higher amounts of total body fat (6–8). One study has reported significantly higher SAT in African American women compared with white women after statistically controlling for percentage body fat (16). The purpose of this study is to examine racial differences in total fat and abdominal VAT and SAT in a large cohort of white and African American men and women.
SUBJECTS AND METHODS
Sample
The Pennington Center Longitudinal Study (PCLS) is an ongoing investigation of obesity, lifestyle, and the development of common chronic diseases such as cardiovascular disease, type 2 diabetes, cancer, and premature mortality. The PCLS sample is composed of volunteers who have participated in a variety of clinical studies, including diet interventions, weight loss, and other metabolic/physiologic studies conducted at the Pennington Biomedical Research Center (PBRC) since 1992. The present investigation is limited to cross-sectional analyses of baseline data for the current sample of participants who underwent dual-energy X-ray absorptiometry (DXA) scans and CT scans of the abdomen (1996–2008). In cases in which participants had multiple baseline measurements, the earliest complete record was used. All DXA and CT measurements were conducted within 60 d of the initial screening visit (DXA mean: 22.7 d; CT mean: 26.2 d). The total sample includes 1967 adults 18–84 y of age (mean: 45.1 y), including 790 white women, 435 African American women, 606 white men, and 136 African American men. All procedures employed by the PCLS were approved by the PBRC Institutional Review Board, and all participants provided written, informed consent.
Anthropometric measures
During their initial visit to the PBRC screening site, a nurse measured the volunteer's height in duplicate by using a wall-mounted stadiometer and weight in duplicate by using a digital scale after the volunteer removed outer clothing, heavy pocket items, and shoes. BMI was calculated as weight in kilograms divided by height in meters squared.
DXA
Total body fat mass (in kg) was estimated by DXA, which is currently measured at PBRC by using a Hologic QDR4500A whole-body scanner (Bedford, MA). The current DXA (QDR4500; n = 1039) has been used since 2001; an older machine (QDR2000; n = 928) was phased out and decommissioned in 2006. A validation study (n = 32) was performed to develop correction equations for the QDR2000 data to the current QDR4500 output by subjecting participants to same-day scans on both machines. There is a high degree of concordance between the total body fat mass measurements of the 2 machines (R2 = 0.993), and the following equation was used to convert the QDR2000 data to be comparable with QDR4500: Y = 0.832X + 1.528. For both DXA instruments, a single phantom was used before each day's data collection to 1) confirm calibration and 2) document stability (ie, drift) over time. Twice-yearly calibrations by the manufacturer are used to correct for minor changes in the instruments due to small expected drift in the X-ray tube characteristics over 6-mo time intervals.
Computed tomography
CT scans were performed with the participant lying in the supine position with the arms over the head. A cross-sectional axial image was obtained at the level of the L4–L5 intervertebral space. The CT scans were performed at the Baton Rouge General Medical Center, Baton Rouge, Louisiana, with a General Electric computed tomography scanner (GE Company, Milwaukee, WI). Three different machines have been used over the course of data collection: GE High Speed Advantage (1996–2000; n = 888), GE LightSpeed Plus (2000–2007; n = 989), and GE LightSpeed VCT (2007–2008; n = 90). The CT scanner is calibrated to air [Hounsfield units (HU) = 0] daily. Image data were transferred to PBRC, and commercially available software (Analyze; Analyze Direct, Rochester, MN) was used to electronically measure areas of adipose tissue by selecting regions of interest defined by attenuation values (−30 to −190 HU for adipose tissue). Abdominal VAT and SAT cross-sectional areas (cm2) were measured as previously described (17).
A subsample of 1034 participants had multislice CT scans of the abdomen (an initial image was obtained at the level of the L4–L5 intervertebral space, 2 images were obtained 5 and 10 cm below L4–L5, and an additional 5 images were obtained every 5 cm above L4–L5). Abdominal VAT and SAT volumes (in L) were computed from the cross-sectional images as previously described (17). Due to the strong correlations between VAT area and volume (r = 0.89; range across sex-by-race groups: 0.89–0.94) and SAT area and volume (r = 0.96; range across sex-by-race groups: 0.93–0.99) (Figure 1), SAT and VAT areas, rather than volumes, were used to accomplish the aims of this article to maintain adequate sample sizes in the sex-by-race groups.
FIGURE 1.

Associations between abdominal (A) visceral adipose tissue (VAT) volume and area (L4–L5) and (B) subcutaneous adipose tissue (SAT) volume and area (L4–L5) in a subsample of 1034 men and women with multislice computed tomography scans available in the Pennington Center Longitudinal Study.
Covariates
Age was computed from birth and observation dates. Self-reported smoking status was determined from questionnaire responses during screening, and participants were categorized as nonsmokers, current smokers, or former smokers. Menopausal status (premenopausal/postmenopausal) was determined in women from their age and responses to questions regarding their reproductive history. Women aged ≥55 y or those who indicated that they can no longer have children because of achieving menopause were considered to be postmenopausal. Unfortunately data on physical activity, dietary intake, and socioeconomic position were not available, so the influence of these variables on the observed relationships could not be explored.
Statistical analysis
Data management and analysis were performed by using SAS 9.1 software (SAS Institute, Cary, NC). Differences in abdominal SAT and VAT between racial groups within sex were analyzed by general linear models, which controlled for age (y) and total body fat (kg). Additional models were analyzed to test for racial differences in abdominal VAT and SAT; these models controlled for age (y), total body fat (kg), smoking status (non/current/former), and menopausal status (pre/post; women only). To further explore the effects of age, the sample was dichotomized into 2 age groups (<45 and ≥45 y), and stratified analyses were conducted.
RESULTS
The descriptive characteristics of the sample are presented in Table 1. African American men and women were significantly younger than white men and women, respectively. Racial differences in height were not significant; however, African American women had significantly greater body weight, BMI, and total body fat compared with white women, and white men had significantly greater total body fat compared with African American men.
TABLE 1.
Characteristics of the subjects1
| Men | Women | |||
| African American (n = 136) | White (n = 606) | African American (n = 435) | White (n = 790) | |
| Age (y) | 38.4 ± 13.92 | 44.9 ± 13.43 | 40.8 ± 11.4 | 48.9 ± 11.03 |
| Age range (y) | 18–70 | 18–72 | 18–73 | 18–84 |
| Height (cm) | 177.2 ± 6.7 | 177.2 ± 6.5 | 163.5 ± 6.0 | 163.1 ± 5.8 |
| Weight (kg) | 93.1 ± 17.4 | 95.5 ± 16.3 | 83.4 ± 14.9 | 78.3 ± 14.53 |
| BMI (kg/m2) | 29.6 ± 5.2 | 30.4 ± 4.9 | 31.2 ± 5.2 | 29.4 ± 5.13 |
| Body fat (kg) | 22.0 ± 9.7 | 26.8 ± 9.73 | 32.4 ± 9.2 | 31.2 ± 9.03 |
| VAT (cm2) | 97.7 ± 63.9 | 148.6 ± 73.43 | 96.7 ± 50.7 | 126.8 ± 63.73 |
| SAT (cm2) | 289.4 ± 156.6 | 319.3 ± 141.83 | 452.7 ± 141.6 | 412.0 ± 137.93 |
| Smoking status (%) | ||||
| Current | 12 | 2 | 4 | 5 |
| Former | 14 | 24 | 8 | 19 |
| Never | 73 | 70 | 88 | 76 |
| Postmenopausal (%) | — | — | 13 | 41 |
VAT, abdominal visceral adipose tissue area measured at L4–L5; SAT, abdominal subcutaneous adipose tissue area measured at L4–L5.
Mean ± SD (all such values).
Significantly different from African Americans, P < 0.05 (within-sex t test).
The correlations among the indicators of body fatness are presented in Table 2. All indicators were significantly intercorrelated (P < 0.0001), and the magnitude and pattern of correlations were remarkably similar across the sex and race groups. Total body fat mass was more highly correlated with SAT (r = 0.91–0.96) than with VAT (r = 0.57–0.68). VAT was moderately correlated with SAT (r = 0.44–0.56) in each of the sex-by-race groups.
TABLE 2.
Correlation coefficients between indicators of total and depot-specific body fat in the 4 sex-by-race groups1
| Total body fat | VAT | SAT | |
| Men | |||
| Total body fat | 0.67 | 0.94 | |
| VAT | 0.68 | 0.51 | |
| SAT | 0.96 | 0.56 | |
| Women | |||
| Total body fat | 0.62 | 0.91 | |
| VAT | 0.57 | 0.44 | |
| SAT | 0.91 | 0.48 |
Correlations for white participants are presented above the diagonal, and correlations for African American participants are presented below the diagonal. The sample sizes were 136 African American men, 606 white men, 435 African American women, and 790 white women. VAT, abdominal visceral adipose tissue area measured at L4–L5; SAT, abdominal subcutaneous adipose tissue area measured at L4–L5. All correlations are significantly greater than zero at P < 0.0001.
Abdominal VAT was significantly higher in white compared with African American men and women. These differences were significant both before adjustment (Table 1) and after adjustment for age and total body fat mass (Figure 2A) and for age, total body fat mass, smoking, and menopausal status (women only) (Figure 2B).
FIGURE 2.

Mean (95% CI) abdominal visceral adipose tissue (VAT) area (L4–L5) in African American and white men and women. A: Age- and total fat mass–adjusted means. B: Means adjusted for age, total fat mass, smoking, and menopausal status (women only). Sex-specific differences in subcutaneous adipose tissue and VAT between racial groups were analyzed by the use of general linear models. The sample sizes were 136 African American men, 606 white men, 435 African American women, and 790 white women.
Abdominal SAT was significantly higher in white men compared with African American men (Table 1); however, after adjustment for covariates, SAT was lower among white men compared with African American men (Figure 3, A and B). Abdominal SAT was significantly higher in African American compared with white women. These differences were significant both before adjustment (Table 1) and after adjustment for age and total body fat mass (Figure 3A) and for age, total body fat mass, smoking, and menopausal status (Figure 3B).
FIGURE 3.

Mean (95% CI) abdominal subcutaneous adipose tissue (SAT) area (L4–L5) in African American and white men and women. A: Age- and total fat mass–adjusted means. B: Means adjusted for age, total fat mass, smoking, and menopausal status (women only). Sex-specific differences in SAT and visceral adipose tissue between racial groups were analyzed by the use of general linear models. The sample sizes were 136 African American men, 606 white men, 435 African American women, and 790 white women.
Age (in y) was a significant covariate in all models. To further explore the effects of age on the observed relationships, the sample was dichotomized into 2 age groups (<45 and ≥45 y). The inclusion of the dichotomous age variable in the models did not change the results. Furthermore, age-stratified analyses were conducted (Figure 4). The effects of race on both abdominal VAT and abdominal SAT were similar in all age and sex groups.
FIGURE 4.
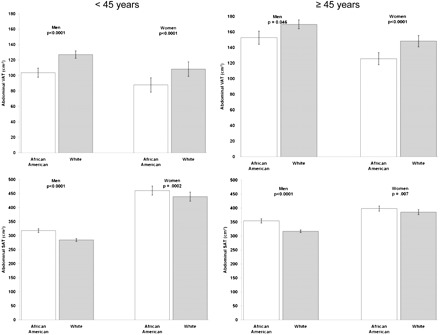
Mean (95% CI) abdominal visceral adipose tissue (VAT) area (top panels) and subcutaneous adipose tissue (SAT) area (bottom panels) in African American and white men and women aged <45 and ≥45 y. Sex-specific differences in SAT and VAT between racial groups were analyzed by general linear models with age, total fat mass, smoking, and menopausal status (women only) included as covariates. The sample sizes were 136 African American men, 606 white men, 435 African American women, and 790 white women.
The relation between total body fat mass and abdominal VAT and SAT in all 4 race-by-sex groups is presented in Figure 5. The correlations between total body fat mass and VAT are lower than the correlations with SAT (Table 2), and this is also evident in the difference in the spread of points depicted in A and B of Figure 5. Abdominal VAT is higher in white men and women compared with African American men and women across all amounts of body fat mass, and the difference becomes more pronounced at higher amounts of total body fat. The results depicted in Figure 5B indicate that the differences in SAT between white and African American women and men for a given amount of total body fat are fairly consistent but tend to increase with higher amounts of total body fat.
FIGURE 5.

Relations between abdominal areas (L4–L5) of (A) visceral adipose tissue (VAT) and (B) subcutaneous adipose tissue (SAT) and total body fat mass in African American men (AAM), white men (WM), African American women (AAW), and white women (WW). The sample sizes were 136 African American men, 606 white men, 435 African American women, and 790 white women.
DISCUSSION
To our knowledge, this is the largest study published to date that examines racial differences in abdominal depot–specific body fat both before and after controlling for amounts of total body fat and other covariates. Given the observed correlations between VAT and SAT and total body fat, it was important to adjust for total body fat to determine the effects of race on abdominal depot–specific adiposity per se. The results of this study indicate that significant racial differences exist in abdominal depot–specific body fatness, even for a given amount of total body fat. African American men and women have lower amounts of abdominal VAT for a given amount of total body fat than white Americans, and these differences increase with the amount of total body fat. Furthermore, after adjustment for age, total body fat mass, and other covariates, abdominal SAT was observed to be higher in African American men and women compared with white men and women, respectively.
The results of this study both support and contradict the results of earlier studies. The majority of previous studies have also reported lower amounts of abdominal VAT in African American compared with white men (6–11). However, previous studies of racial differences in abdominal VAT among women have produced mixed results (6–13, 15, 16). The results of the present study confirm those of 6 previous studies that have also reported significantly lower VAT in African American women compared with white women (6, 10–14). Three other studies have reported lower VAT in African American women; however, these differences were not statistically significant (8, 15, 16). Among women in the Coronary Artery Risk Development in Young Adults study, African Americans had higher total body fat and abdominal VAT than white Americans; however, the VAT differences disappeared after adjustment for differences in total body fat (9). Among women enrolled in 3 community-based studies in Ohio, African Americans and white Americans had similar amounts of VAT, but the differences were not adjusted for potential differences in total adiposity (7). Thus, the results of this study lend further support to the weighted evidence that abdominal VAT is lower in African American men and women after controlling for differences in overall adiposity.
The finding that African Americans have lower amounts of abdominal VAT yet have higher mortality rates from diabetes, cardiovascular disease, and cancer than white Americans is a paradox. There are observed disparities in health risks among white and African Americans (18, 19), and part of this paradox might be explained by examining racial differences in absolute compared with relative risks of disease and/or mortality. The finding of higher abdominal VAT in white men and women, after adjustment for total body fat, may partially explain the observed racial differences in the relative risk of mortality associated with BMI, particularly in women (20–22). In a large cohort of US adults, the relative risk of death from all causes increased with higher BMI across normal weight, overweight, and obese BMI categories in white men and women; however, the relative risks were much lower in African American men and women (20). Furthermore, African American women experienced only a small elevation in mortality risk at the highest BMIs (≥35) (20). If the health hazards of obesity are differentially expressed through abdominal VAT, then the fact that African American women have a lower relative risk of mortality associated with BMI may be a reflection of their lower abdominal VAT amounts. On the other hand, the absolute risk of mortality in the study at every level of BMI was higher among African Americans than among white Americans, particularly in the normal weight category, which suggests that other mechanisms are likely involved in explaining these mortality rate differences. Furthermore, given the high rates of obesity among African Americans in general, the lower amounts of abdominal VAT for a given amount of body fat may not compensate. Further research is required to disentangle the effects of depot-specific adiposity on population-level mortality rates from specific causes to better explain this paradox.
The existing evidence from previous studies provides no clear understanding of racial differences between African American and white men and women in abdominal SAT. These mixed results may be partially explained by the use of different measures of SAT (magnetic resonance imaging compared with CT, cross-sectional area compared with volume, etc), a mix of analytic strategies (with adjustment for age, total body fat, etc), and differences in the mean and range in age and adiposity of the samples. The results of the present study provide some clarity on this issue. African American women were observed to have higher amounts of abdominal SAT than their white women counterparts, even after statistically adjusting for differences in age and total body fat mass (Figure 3). Although white men had higher abdominal SAT than African American men, these differences reversed after adjustment for total body fat. Thus, the higher abdominal SAT among white men was largely explained by their higher amounts of total body fat. An independent effect of race appears to exist for abdominal SAT: African American men and women have higher amounts of SAT than white men and women after adjustment for total body fatness.
The health effects associated with SAT in the abdomen compared with other anatomic regions are not well understood. Some studies have suggested that higher amounts of gluteo-femoral SAT for a given amount of abdominal fat may be associated with a more favorable cardiometabolic risk factor profile (23); however, the degree to which abdominal SAT provides cardiometabolic protection is largely unknown. A recent study from the Framingham Heart Study has shown that, when stratified by tertiles of abdominal VAT, many cardiometabolic risk factors do not increase across tertiles of abdominal SAT (24). The role of the anatomical location of SAT in defining health risk is an important area for future research.
Few studies have employed prospective designs to study racial differences in the relation between obesity and the development of risk factors (19). Data from the Atherosclerosis Risk in Communities Study indicated that the incidence of diabetes over a 9-y period was higher at all levels of BMI in African American compared with white adults (25). This is in contrast to results from the NHANES Epidemiologic Follow-up Study in which the 20-y incidence of diabetes was higher in African Americans than in white Americans at low BMI values and equivalent at higher BMI values (26). These results highlight the need to clarify racial differences in both the relative and the absolute risk of disease.
The strengths and limitations of this study warrant discussion. The precise measurement of total body fat mass and abdominal SAT and VAT areas in a large biracial cohort by using advanced imaging techniques is a marked strength of this study. Single CT images at the level of L4–L5 were used for all primary analyses, and the adipose tissue areas were highly correlated with total volumes in a subsample with multi-slice data. However, there is some evidence to suggest that maximum VAT areas may occur at different anatomical levels in white and African American men and women (7), which could not be accounted for in the present study. The PCLS cohort is not a representative sample of the US population; rather, it represents local volunteers who have been screened for a wide variety of clinical research studies at PBRC. However, the sample (60% white, 40% African American) is reflective of the racial diversity in southern Louisiana, and the individuals range in BMI from 17 to 49. The range of BMI and total body fat represented in the sample is a marked strength of the study because it allowed us to examine the associations between race and depot-specific body fat across a large range of human variability. Unfortunately, an indicator of socio-economic position was not available for the participants in this study to examine the extent to which socio-economic position may explain the observed race differences. A further limitation of this study is that volunteers whose self-reported race or ethnicity was other than African American or white were not included in the cohort. This study also did not include children or adolescents <18 y of age, so caution should be used in extrapolating the observed racial differences further backward into childhood, as the temporal sequence of the emergence of these differences is unknown.
The results of this investigation highlight the heterogeneity of human body fat distribution across racial groups. More research is required to determine the immediate and long-term health consequences of the observed racial differences in abdominal depot–specific body fatness. Carefully conducted prospective studies in biracial cohorts of men and women with measurements of depot-specific body fatness are required to determine the long-term health effects of these observed differences. The results of these investigations will provide important information that will ultimately inform the need for race-specific obesity guidelines.
Acknowledgments
We especially thank Emily Mire and Connie Murla for data management and the many clinical scientists and staff of the Pennington Biomedical Research Center who have contributed data to the development of the Pennington Center Longitudinal Study and, in particular, William Cefalu, Nikhil Dhurandhar, Lilian Levitan, Timothy Church, Paula Geiselman, Alok Gupta, Corby Martin, and Thomas Gettys. We also acknowledge Julia St Amant for her expert supervision of the CT acquisition and for the analysis of the majority of the CT scans reported here.
The authors' responsibilities were as follows—PTK: conceived the study, analyzed the data, and drafted the manuscript; WDJ: oversaw analysis of the data and edited the manuscript; GAB, FLG, ER, DHR, and SRS: collected the data and edited the manuscript; CB: aided in study conception and edited the manuscript; and RLN: edited the manuscript. None of the authors had a conflict of interest.
FOOTNOTES
Supported by the Pennington Biomedical Research Center. PTK is supported, in part, by the Louisiana Public Facilities Authority Endowed Chair in Nutrition; CB is funded, in part, by the George A Bray, Jr, Chair in Nutrition; and ER is funded, in part, by the Douglas L Gordon Chair in Diabetes and Metabolism.
REFERENCES
- 1. US Department of Health and Human Services. Healthy people 2010, 2nd ed. Understanding and improving health and objectives for improving health. 2 vols. Washington, DC: US Government Printing Office, 2000. [Google Scholar]
- 2. Harper S, Lynch J, Burris S, Davey Smith G.. Trends in the black-white life expectancy gap in the United States, 1983–2003. JAMA 2007;297:1224–32. [DOI] [PubMed] [Google Scholar]
- 3. National Center for Health Statistics. Health, United States, 2007, with chartbooks on trends in the health of Americans. Hyattsville, MD: US Department of Health and Human Services, 2007. [Google Scholar]
- 4. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM.. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA 2006;295:1549–55. [DOI] [PubMed] [Google Scholar]
- 5. Després J-P, Lemieux I.. Abdominal obesity and metabolic syndrome. Nature 2006;444:881–7. [DOI] [PubMed] [Google Scholar]
- 6. Carroll JF, Chiapa AL, Rodriquez M, et al. Visceral fat, waist circumference, and BMI: impact of race/ethnicity. Obesity (Silver Spring) 2008;16:600–7. [DOI] [PubMed] [Google Scholar]
- 7. Demerath EW, Sun SS, Rogers N, et al. Anatomical patterning of visceral adipose tissue: race, sex, and age variation. Obesity (Silver Spring) 2007;15:2984–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Després J-P, Couillard C, Gagnon J, et al. Race, visceral adipose tissue, plasma lipids, and lipoprotein lipase activity in men and women: the Health, Risk Factors, Exercise Training, and Genetics (HERITAGE) family study. Arterioscler Thromb Vasc Biol 2000;20:1932–8. [DOI] [PubMed] [Google Scholar]
- 9. Hill JO, Sidney S, Lewis CE, Tolan K, Scherzinger AL, Stamm ER.. Racial differences in amounts of visceral adipose tissue in young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Am J Clin Nutr 1999;69:381–7. [DOI] [PubMed] [Google Scholar]
- 10. Hoffman DJ, Wang Z, Gallagher D, Heymsfield SB.. Comparison of visceral adipose tissue mass in adult African Americans and whites. Obes Res 2005;13:66–74. [DOI] [PubMed] [Google Scholar]
- 11. Bray GA, Jablonski KA, Fujimoto WY, et al. Relation of central adiposity and body mass index to the development of diabetes in the Diabetes Prevention Program. Am J Clin Nutr 2008;87:1212–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Conway JM, Yanovski SZ, Avila NA, Hubbard VS.. Visceral adipose tissue differences in black and white women. Am J Clin Nutr 1995;61:765–71. [DOI] [PubMed] [Google Scholar]
- 13. Perry AC, Applegate EB, Jackson ML, et al. Racial differences in visceral adipose tissue but not anthropometric markers of health-related variables. J Appl Physiol 2000;89:636–43. [DOI] [PubMed] [Google Scholar]
- 14. Kanaley JA, Giannopoulou I, Tillapaugh-Fay G, Nappi JS, Ploutz-Snyder LL.. Racial differences in subcutaneous and visceral fat distribution in postmenopausal black and white women. Metabolism 2003;52:186–91. [DOI] [PubMed] [Google Scholar]
- 15. Araneta MR, Barrett-Connor E.. Ethnic differences in visceral adipose tissue and type 2 diabetes: Filipino, African-American, and white women. Obes Res 2005;13:1458–65. [DOI] [PubMed] [Google Scholar]
- 16. Lovejoy JC, Smith SR, Rood JC.. Comparison of regional fat distribution and health risk factors in middle-aged white and African American women: the Healthy Transitions Study. Obes Res 2001;9:10–6. [DOI] [PubMed] [Google Scholar]
- 17. Smith SR, Lovejoy JC, Greenway F, et al. Contributions of total body fat, abdominal subcutaneous adipose tissue compartments, and visceral adipose tissue to the metabolic complications of obesity. Metabolism 2001;50:425–35. [DOI] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention. Health disparities experienced by black or African Americans—United States. MMWR Morb Mortal Wkly Rep 2005;54:1–3. [PubMed] [Google Scholar]
- 19. Kurian AK, Cardarelli KM.. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis 2007;17:143–52. [PubMed] [Google Scholar]
- 20. Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr.. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 1999;341:1097–105. [DOI] [PubMed] [Google Scholar]
- 21. Stevens J, Keil JE, Rust PF, Tyroler HA, Davis CE, Gazes PC.. Body mass index and body girths as predictors of mortality in black and white women. Arch Intern Med 1992;152:1257–62. [PubMed] [Google Scholar]
- 22. Stevens J.. Obesity and mortality in Africans-Americans. Nutr Rev 2000;58:346–53. [DOI] [PubMed] [Google Scholar]
- 23. Snijder MB, van Dam RM, Visser M, Seidell JC.. What aspects of body fat are particularly hazardous and how do we measure them? Int J Epidemiol 2006;35:83–92. [DOI] [PubMed] [Google Scholar]
- 24. Porter SA, Massaro JM, Hoffmann U, Vasan RS, O'Donnel CJ, Fox CS.. Abdominal subcutaneous adipose tissue: a protective fat depot? Diabetes Care 2009;32:1068–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stevens J, Couper D, Pankow J, et al. Sensitivity and specificity of anthropometrics for the prediction of diabetes in a biracial cohort. Obes Res 2001;9:696–705. [DOI] [PubMed] [Google Scholar]
- 26. Resnick HE, Valsania P, Halter JB, Lin X.. Differential effects of BMI on diabetes risk among black and white Americans. Diabetes Care 1998;21:1828–35. [DOI] [PubMed] [Google Scholar]


