Abstract
Context
Obesity is associated with increased incidence of chronic diseases such as type 2 diabetes mellitus, systemic hypertension, and other risk factors for cardiovascular disease. Obesity is also associated with increased use of outpatient clinical services, a metric of health care utilization. However, little is known of temporal changes in health care utilization among obese participants of a medical weight management program.
Objective
To assess changes in 3 health care utilization metrics (primary care physician office visits, ambulatory clinic office visits, and health care touches [encounters]) in weight management program participants across 21 Kaiser Permanente Northern California Medical Centers during a 5-year period.
Design
Retrospective observational study of 10,693 participants, with a linear-mixed effects model to account for repeated-measures analysis.
Main Outcome Measures
Five-year temporal changes in the 3 health care metrics.
Results
At baseline, the participants’ average age (standard deviation) was 51.1 (12.4) years, and their mean body mass index (standard deviation) was 39.7 (7.2) kg/m2. At the end of 4 months, there was a decrease in primary care visits (p < 0.001), with an increase in ambulatory clinic visits and health care touches (p < 0.001), because of increased weight management visits. At the end of 5 years, there was a 25% to 35% decrease from baseline in all 3 health care utilization metrics (p < 0.0001). Although slightly attenuated, these findings were similar in a risk-adjusted model.
Conclusion
Our findings may be useful to other integrated health care delivery systems considering initiating a similar weight management program.
Keywords: health care utilization, medically supervised weight management, obesity, weight loss program
INTRODUCTION
Obesity is associated with an increased incidence of chronic diseases such as type 2 diabetes mellitus, systemic hypertension, and other risk factors for cardiovascular disease. Furthermore, obese patients, compared with healthy-weight individuals, have an approximate 30% increase in outpatient clinical services,1 a measure of health care utilization. However, health care utilization in obese patients has only recently become recognized as a possible surrogate marker of disability.2,3 Because of the rising prevalence of obesity and a paucity of data of the effects of weight loss treatment on health care utilization,4 we sought to study the temporal changes in 3 measures of health care utilization in obese participants of a medically supervised, behaviorally based, weight management program across 21 Kaiser Permanente Northern California (KPNC) Medical Centers.
METHODS
The details of the program along with a description of the underlying cohort have been extensively described in a previous article in The Permanente Journal.5 In brief summary, our prior report documented the changes in weight and lipids and addressed predictors of weight loss of 5% or more from baseline at 5 years in 10,693 participants enrolled in a medically supervised weight management program in KPNC. The weight management program consists of 3 phases: A complete meal replacement up to 16 weeks, a transition to regular food between 17 and 29 weeks, and a long-term lifestyle phase between 30 and 82 weeks. We demonstrated that the absolute average weight change (in kilograms) at 5 years was significantly lower from baseline (−6.4 kg, p < 0.001), with the accompanying average percentage change in weight also significantly lower from baseline (a decrease of 5.8%). Among participants with 5-year data, weight loss of less than 5.0% occurred in 48.5%, weight loss of 5.0% to 9.9% occurred in 16.3%, and weight loss of 10.0% and greater occurred in 35.2%. There were changes in lipids approximately paralleling the weight changes.
This report is a retrospective, observational study of all 10,693 adults (age 18 years and older) enrolled in the weight management program between April 1, 2007, and December 31, 2014, that focused on temporal changes in health care utilization during the 5-year period in program participants. The primary outcome for the current study was temporal changes in 3 health care utilization metrics during 5 years compared with baseline, measured up to 1 year before study entry. Specifically, changes in the number of primary care physician visits (defined as the number of clinic visits with a department code of Adult and Family Medicine, not a weight management visit), the number of ambulatory clinic visits (defined as the number of clinic visits that included subspecialty clinic visits as well as weight management visits), and the number of overall health care touches. Health care touches were defined as any of the following: Ambulatory clinic visits, Emergency Department visits, inpatient hospitalizations, inpatient admissions to nonacute care institutions, home health visits, admission to hospice, use of a laboratory facility (as noted by a visit for a blood draw), any Radiology Department visit for radiologic procedures, and telephone encounters. We specifically did not include the use of email encounters because it was beyond the scope of this project.
Statistical analysis was performed using a linear mixed-effects model with unstructured covariance, a random intercept, and a restricted maximum likelihood test option to assess the changes in health care use over the follow-up period, to account for the repeated-measures analysis. The full risk-adjusted model included baseline demographics (age, body mass index, race, median household income) and baseline comorbidities (prediabetes, diabetes, hypertension, hyperlipidemia, liver disease, lung disease, myocardial infarction, coronary artery disease [that includes history of prior coronary artery bypass grafting, percutaneous coronary intervention], cerebrovascular accident, atrial fibrillation, sleep apnea, depression). All statistical analyses were performed using Stata Version 15 software (StataCorp, College Station, TX). The study was approved by the KPNC institutional review board.
RESULTS
The flow of participants in the study was as follows: Baseline (N = 10,693) and 1-year (N = 10,218), 2-year (N = 8601), 3-year (N = 7941), 4-year (N = 6042), and 5-year follow-up (N = 4261). Patients were included for analysis each year if they reached the first day of that year. At baseline, the average age (standard deviation) was 51.1 (12.4) years, and the mean body mass index (standard deviation) was 39.7 (7.2) kg/m2 (Table 1). Of participants, 72.0% were white and 72.8% were women.
Table 1.
Baseline characteristics and health care utilization metrics of participants of a medically supervised weight management program (N = 10,693) across 21 Kaiser Permanente Northern California Medical Centers
| Variable | Measure |
|---|---|
| Baseline demographics | |
| Age, mean (SD), y | 51.1 (12.4) |
| Women, % | 72.8 |
| Men, % | 27.2 |
| Race, % | |
| White | 72.0 |
| Black/African American | 8.3 |
| Latin American (Hispanic) | 4.6 |
| Asian/Pacific Islander | 6.0 |
| Other | 9.1 |
| Clinical characteristics | |
| Current tobacco use, % | 9.2 |
| Body mass index, mean (SD), kg/m2 | 39.7 (7.2) |
| Neighborhood income, mean (SD), US dollars | 66,683 (25,353) |
| No. baseline comorbidities, median (IQR) | 2 (2) |
| No. baseline medications, median (IQR) | 1 (2) |
| Baseline health care utilization, mean (95% CI) | |
| Primary care visits | 3.9 (3.8–4.0) |
| Ambulatory clinic visits | 14.9 (14.6–15.1) |
| Health care touches | 23.4 (23.0–23.7) |
CI = confidence interval; IQR = interquartile range; SD = standard deviation.
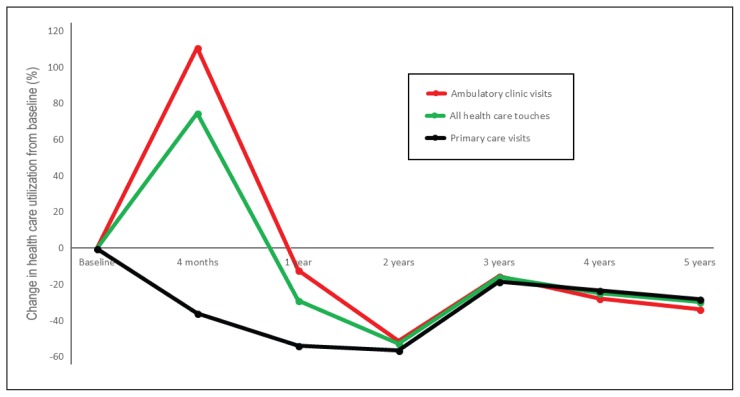
Baseline health care utilization metrics are also shown in Table 1. Table 2 demonstrates the 5-year unadjusted health care utilization changes. Figure 1 demonstrates the corresponding 5-year health care utilization percentile changes. Although slightly attenuated, these findings were similar in the fully risk-adjusted model (results furnished on request).
Table 2.
Five-year temporal changes in 3 health care utilization metrics in weight management program participants
| Time | Change from baseline | p value | 95% confidence interval |
|---|---|---|---|
| Primary care visits | |||
| Baseline | 3.9 | NA | 3.8 to 4.0 |
| 4 mo | −1.4 | < 0.001 | −1.5 to −1.3 |
| 1 y | −2.1 | < 0.001 | −2.2 to −2.0 |
| 2 y | −2.2 | < 0.001 | −2.3 to −2.1 |
| 3 y | −0.7 | < 0.001 | −0.8 to −0.6 |
| 4 y | −0.9 | < 0.001 | −1.0 to −0.8 |
| 5 y | −1.1 | < 0.001 | −1.2 to −0.9 |
| Ambulatory care visits | |||
| Baseline | 14.9 | NA | 14.6 to 15.1 |
| 4 mo | +16.5 | < 0.001 | +16.2 to +16.8 |
| 1 y | −1.8 | < 0.001 | −2.0 to −1.5 |
| 2 y | −7.6 | < 0.001 | −7.9 to −7.3 |
| 3 y | −2.3 | < 0.001 | −2.6 to −1.9 |
| 4 y | −4.1 | < 0.001 | −4.5 to −3.8 |
| 5 y | −5.0 | < 0.001 | −5.4 to −4.7 |
| All health care touches | |||
| Baseline | 23.4 | NA | 23.0 to 23.7 |
| 4 mo | +17.5 | < 0.001 | +17.1 to +17.9 |
| 1 y | −6.7 | < 0.001 | −7.1 to −6.3 |
| 2 y | −12.3 | < 0.001 | −12.7 to −11.9 |
| 3 y | −3.7 | < 0.001 | −4.1 to −3.3 |
| 4 y | −5.8 | < 0.001 | −6.3 to −5.4 |
| 5 y | −6.9 | < 0.001 | −7.4 to −6.3 |
NA = not applicable.
Figure 1.
Five-year temporal percentile changes in 3 health care utilization metrics in participants of a medically supervised weight management program across 21 Kaiser Permanente Northern California Medical Centers.
DISCUSSION
The current study specifically focused on the temporal changes in health care utilization metrics among obese participants enrolled in a weight management program. It did not address changes in weight, lipids, blood pressure, or either associated costs or a cost-effectiveness analysis. Many of these outcomes have been already addressed.5 At the end of 4 months, after the acute weight loss period, we found a lower number of primary care physician visits along with an expected increase in all ambulatory clinic visits and health care touches, as a result of the intensive resources dedicated to the weight management participants. However, the main finding of this study was the significant long-term decrease from baseline, between 25% and 35%, in all 3 health care utilization metrics at the end of 5 years.
There are limited data available on the effects of weight management programs on health care utilization metrics, with only recent acceptance of health care utilization as a possible surrogate marker of disability.3 The primary determinants of health care utilization are thought to be related to health status and access to care.6 However, all study participants had medical insurance and were part of an integrated health care delivery system. Therefore, we hypothesize that the demonstrated changes in health care utilization were possibly related to changes in objective health status related to improvements in weight, blood pressure, and lipid levels and to subjective improvements in self-perceived health status related to the long-term behavioral portion of the weight management program.5
Study limitations are related to the observational nature of the study design and a lack of a control group. Although the KPNC population is representative of the surrounding and statewide population,7 our findings may not be fully generalizable to other weight management programs because program participants had medical insurance and were capable of affording the program fees—a possible selection bias. Although the mechanisms of the change in health care utilization were beyond the scope of this study, the finding from this study of decreased long-term care health care utilization may be pertinent to other integrated and nonintegrated health care delivery systems. Further work in this area should assess cost-effectiveness, changes in quality of life, and disability.
CONCLUSION
In obese participants of a medically supervised, behaviorally based, weight management program in an integrated health care delivery system in Northern California, there was a substantial decrease in 3 health care utilization metrics (primary care physician office visits, ambulatory clinic office visits, and health care touches) at the end of 5 years. Our findings may be useful to other Kaiser Permanente Regions or other health care delivery systems considering initiation of a similar weight management program.
Acknowledgments
We thank Lindsey Hogan, MHSA, for her critical review of the manuscript and her contribution as the program project manager.
Kathleen Louden, ELS, of Louden Health Communications performed a primary copy edit.
Footnotes
Disclosure Statement
This study was supported by a grant from Nestlé HealthCare Nutrition, Inc, Florham Park, NJ. The sponsor did not have access to the primary data; did not participate in data collection, analysis, or interpretation; and did not have a decision to submit the manuscript for publication.
Authors Contributions
Ashok Krishnaswami, MD, the study supervisor, had full access to the study dataset and takes responsibility for data integrity and analysis accuracy; takes primary responsibility for study concept and design and for data interpretation; performed the statistical analysis; and wrote the initial draft of the manuscript. Rohini Ashok, MD; Wayne Smith, MD; and Stephen Sidney, MD, MPH, helped conceptualize and design the study and helped interpret the data. Dr Sidney also assisted with data acquisition from Kaiser Permanente databases. Michael Sorel, MPH, assisted with data acquisition and helped interpret the data. All authors read and approved the final manuscript.
References
- 1.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: Payer- and service-specific estimates. Health Aff (Millwood) 2009 Sep-Oct;28(5):w822–31. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 2.An R, Andrade F, Chiu CY. Overweight and obesity among US adults with and without disability, 1999–2012. Prev Med Rep. 2015 May 12;2:419–22. doi: 10.1016/j.pmedr.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Committee on Health Care Utilization and Adults with Disabilities, Board on Health Care Services, Health and Medicine Division. Health-care utilization as a proxy in disability determination. Washington, DC: The National Academies Press; 2018. [DOI] [PubMed] [Google Scholar]
- 4.Jensen MD, Ryan DH, Apovian CM, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014 Jul 1;63(25 Pt B):2985–3023. doi: 10.1016/j.jacc.2013.11.004. doi: 10.1016/j.jacc.2013.11.004. . Erratum in: J Am Coll Cardiol 2014 Jul 1;63(25 Pt B)3029–30. DOI: https://doi.org/10.1016/j.jacc.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Krishnaswami A, Ashok R, Sidney S, et al. Real-world effectiveness of a medically supervised weight management program in a large integrated health care delivery system: Five year outcomes. Perm J. 2018;22:17–082. doi: 10.7812/TPP/17-082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Figueroa JF, Frakt AB, Lyon ZM, Zhou X, Jha AK. Characteristics and spending patterns of high cost, non-elderly adults in Massachusetts. Healthc (Amst) 2017 Dec;5(4):165–70. doi: 10.1016/j.hjdsi.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Gordon NP. Characteristics of adult members in Kaiser Permanente’s Northern California region, as estimated from the 2011 Kaiser Permanente adult member health survey [Internet] Oakland, CA: Division of Research, Kaiser Permanente Medical Care Program; 2013. May, [cited 2018 Oct 26]. Available from: https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/mhs11reg.pdf. [Google Scholar]