Abstract
Background Degenerative arthritis of the first carpometacarpal (CMC) joint is a common degenerative condition in the hand. Many different surgical procedures have been applied for years. However, in the studies there is no consensus about the superiority of one technique to another.
Questions/Purposes In this study, we evaluated the results of the patients with first CMC Eaton–Littler stage 2–3 arthrosis who were operated to prevent first metacarpal joint lateral subluxation and migration with arthroscopic hemitrapeziectomy and suture button suspensionplasty.
Patients and Methods Between 2011 and 2014, 21 patients (16 female, five male) were evaluated retrospectively. Mean age was 52.3 years. The preoperative and postoperative assessments were performed with visual analog scale (VAS) and disabilities of the arm, shoulder, and hand score (DASH) scores. The Kapandji's thumb opposition score was used to assess thumb range of movement. The patients were assessed after arthroscopy according to Badia classification.
Results Mean follow-up period was 50.1 months. According to Badia classification, seven patients were found to be type 2 and 14 patients were type 3. The mean preoperative Kapandji's score was 7.6 and the mean postoperative Kapandji's score was 9.2. The mean VAS values were 8.2 preoperatively and 1.9 postoperatively. The mean preoperative DASH value was 23.4 and the mean postoperative DASH value was 5.5. The mean preoperative grip strength was 66.2 and the mean postoperative grip strength was 75.1. The mean preoperative pinch strength was 14.8 and the mean postoperative pinch strength was 20.2.
Conclusion Arthroscopic hemitrapeziectomy and suture button suspensionplasty is a minimal invasive technique and can be performed with low morbidity in the treatment of first CMC joint Eaton–Littler stage 2–3 arthrosis. By this technique, the patients' existing instability and pain problems can be solved. Complications, such as loosening of the suture button at the first metacarpal at the postoperative period due to direct trauma to the first CMC joint, could be avoided using a new suture button.
Type of Study/ Level of Evidence Therapeutic IV.
Keywords: arthroscopy, carpometacarpal, CMC, suture button
Degenerative arthritis of the first carpometacarpal (CMC) joint is a common degenerative condition in the hand that affects the activities of daily living. 1 2 Many different surgical procedures such as arthroscopic treatment, trapeziectomy, ligament reconstruction, interposition arthroplasty, suspensionplasty, osteochondral allograft applications, carpometacarpal prosthesis, and arthrodesis are used for years. 1 However, in the studies there is no consensus about the superiority of one technique to another. 3 4 5 6 Today there is not a provided consensus between the authors about the treatment methods of first CMC Eaton–Littler stage 2–3 arthrosis.
The aim of this study is to assess the results of the patients, diagnosed with first CMC Eaton–Littler stage 2–3 arthrosis 7 and treated by arthroscopic hemitrapeziectomy and suture button suspensionplasty.
Patients and Methods
Between 2011 and 2014, 21 patients (16 female, 5 male) were operated by a single surgeon. Mean age was 52.3 years (range: 40–60 years). Mean duration of symptoms of the patients prior to surgery was 8.2 months (range: 6–14 months). The hand splints were applied at least 1 month to all patients since the date of admission to hospital. The patients whose pain symptoms were not improved after this period were indicated for surgical treatment. Fourteen patients' dominant hands and seven patients' nondominant hands were operated. In nine patients, Eaton–Littler stage 2 and in 12 patients stage 3 osteoarthritis were present ( Table 1 ). 7 All the patients were assessed during arthroscopy according to Badia's arthroscopic classification ( Table 2 ). 8 All patients underwent arthroscopic hemitrapeziectomy. Eaton–Littler stage 4 patients were not included in this study. The preoperative and postoperative assessments were performed with Kapandji's score, 9 VAS (visual analog scale) score, and DASH (disabilities of the arm, shoulder and hand score) score. The preoperative and postoperative grip and pinch strengths compared with the other extremity were assessed by Jamar hand dynamometer (Jamar Hydraulic Hand Dynamometer, Sammons Preston, Bolingbrook, IL). All the patients were assessed about the time to return to daily activity and work in the postoperative period.
Table 1. Eaton–Littler classification of basilar thumb arthritis 8 .
| Stage 1 | Slight joint space widening (prearthritis), articular contours are normal, < 1/3 subluxation |
| Stage 2 | Slight narrowing of CMC joint with sclerosis, significant capsular laxity, 1/3 subluxation of the joint, osteophytes < 2 mm |
| Stage 3 | Mild narrowing of CMC joint with osteophytes, > 1/3 subluxation of the joint, osteophytes > 2 mm |
| Stage 4 | Severe degenerative changes, major subluxation of the joint, very narrow joint space, cystic ans sclerotic subchondral bone changes, significant erosion of the scaphotrapezial joint, pantrapezial arthritis |
Abbreviation: CMC, carpometacarpal.
Table 2. Badia's arthroscopic classification for thumb carpometacarpal arthritis 9 .
| Stage 1 | Diffuse synovitis, intact articular cartilage, volar capsular laxity |
| Stage 2 | Central fovea articular cartilage loss of trapezium, deep metacarpal base loss, and synovitis |
| Stage 3 | Widespread articular cartilage loss, deep osteophyte on trapezium |
The study protocol was approved by our hospital's institutional review board. All the patients signed an informed consent form about the study.
Surgical Technique
Under regional anesthesia, after tourniquet was applied, traction of first CMC joint was performed using Chinese finger trap. By radial, ulnar, and volar portals, the proliferative synovial tissue in the joint was resected using the 1.9 mm optical camera and 2.0 mm shaver ( Fig. 1 ). Osteophytes were resected by 2.0 mm shaver and 2.9 mm burr. In patients with mild narrowing of CMC joint space with osteophytes greater than 2 mm, 1 to 2 mm, hemitrapeziectomy was performed by 2.9 mm burr. By the traction of the first finger the thumb CMC joint widens as the 2.9 mm burr can enter. The efficacy of debridement and the amount of bone resection was visualized both by arthroscopic and fluoroscopic examination. The 1 to 2 mm resection is usually enough to completely remove the osteophytes and the recovery of the symptoms. After an assistant has provided enough horizontal traction by the Chinese finger trap a K-wire was directed from the proximal part of the first metacarpal toward the center of the middle-third of the second metacarpal in an oblique manner by fluoroscopic control ( Fig. 2 ). The K-wire was taken out of the skin and a 1 cm skin incision was made around the K-wire. By protecting the extensor tendons, the K-wire was continued to be moved. Then a suture was passed through the hook of the special K-wire which is thicker at the proximal two-thirds. Then one of the suture buttons was placed in the tenar area, under the muscles to prevent the button from being felt under the skin. To decide the tension for suture button arthroplasty, after terminating the thumb traction without removing the Chinese finger trap from the thumb, the thumb was positioned by an assistant in sufficient traction and abduction position ( Figs. 3A and B ). Once the suture button has been applied, the suture button tension was adjusted by determining the appropriate amount of suspension and abduction at the fluoroscopic control. By placing a second button to the second metacarpal, under appropriate traction and abduction by an assistant, 6 to 8 knots were placed on the suture. The knot and the suture were pushed into the intermetacarpal space which was covered with interosseous muscles. The skin incisions were sutured by a rapid vicryl and a cast was not applied. The rehabilitation was started on the 2nd postoperative day and the patients were admitted to use their operated hands after the pain relief. The patients were allowed to do pinching and grip exercises as much as they could tolerate pain in the postoperative 2nd day. We did not apply a splint to our patients during postoperative period. Please refer to online version for Videos 1 , 2 , 3 .
Fig. 1.

The arthroscopic evaluation of the CMC joint by using a 1.9 mm optical camera. CMC, carpometacarpal.
Fig. 2.
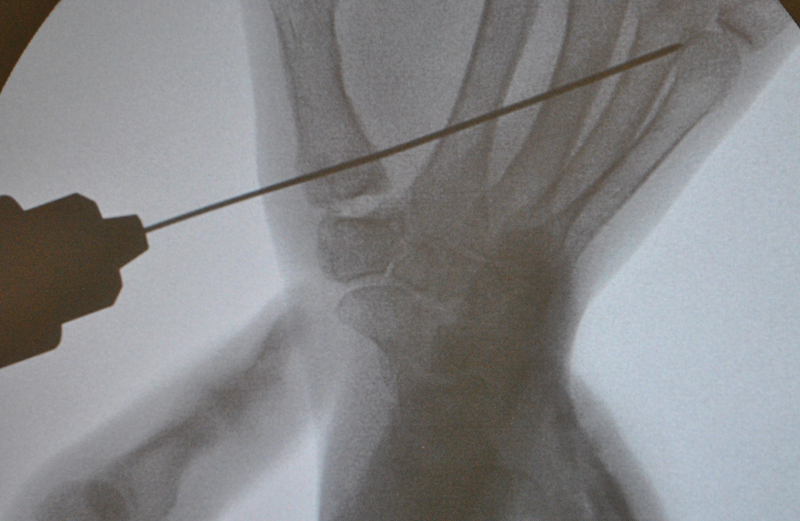
A guide K-wire passing from the basis of the first metacarpal to the diaphysis of the second metacarpal.
Fig. 3.

(A) Preoperative radiographs of a 47-year-old man with a first CMC Eaton–Littler stage 2 arthrosis. ( B) Postoperative day 1 radiographs of the same patient with first CMC Eaton–Littler stage 2 arthrosis treated by arthroscopic hemitrapeziectomy and suture button suspensionplasty. CMC, carpometacarpal.
Video 1
Peroperative management of arthroscopic hemitrapeziectomy and suture button suspensionplasty.
Video 2
Preoperative 3D computerized tomography imaging of the first CMC joint.
Video 3
Postoperative 3D computerized tomography imaging of the first CMC joint.
We used a paired t -test to compare the preoperative and postoperative results of Kapandji's scores, VAS scores, and DASH scores. A value p < 0.05 was considered statistically significant.
Results
Mean follow-up period was 50.1 months (range: 48–60 months). According to Badia's classification 7 patients were found to be type 2 and 14 patients were type 3. The mean preoperative Kapandji's score was 7.6 (range: 7–8) and the postoperative Kapandji's score was 9.2 (range: 9–10). The mean VAS values were 8.2 (range: 6–10) preoperatively and 1.9 (range: 0–4) postoperatively. The mean preoperative DASH value was 23.4 (range: 15.9–38.6) and the mean postoperative DASH value was 5.5 (range: 2.3–9.1). The mean preoperative grip strength was 66.2 (range: 46–102) and the mean postoperative grip strength was 75.1 (range:52–102). The mean preoperative pinch strength was 14.8 (range: 10–22) and the mean postoperative pinch strength was 20.2 (range:15–28). There was statistically significant difference between the mean preoperative and postoperative VAS and DASH values ( p < 0.05) but there was no significant difference between the mean preoperative and postoperative Kapandji's scores ( p > 0.05). There was statistically significant difference between the mean preoperative and postoperative pinch and grip strengths ( p < 0.05). The mean time for patients to return to their daily activities was 9.7 days (range: 5–14 days) and the mean time to return to work was 28.6 days (range: 22–40 days).
The radial instability was evaluated by preoperative computerized tomography (CT) in all patients ( Video 2 ) and by preoperative dynamic fluoroscopy examination in four patients ( Video 4 ). All patients had one-third lateral subluxation of the first CMC joint. It was observed that postoperative radial instability was significantly improved in all patients and at the end of the follow-up period radial instability was not observed in any patient. The preoperative narrowing of the trapezial interval was observed in all patients. On the postoperative first radiographs, the mean 2 mm trapezial interval was maintained with the same level at the end of the follow-up period due to both proximal placement of the suture button and hemitrapeziectomy. Furthermore, additional arthrosis of the adjacent joints was not observed at the end of follow-up period.
Video 4
Peroperative dynamic fluoroscopic imaging of the first CMC joint subluxation.
Loosening of the suture button at the first metacarpal was detected in one patient at the postoperative 2nd week due to direct trauma to the first CMC joint. This patient was reoperated by using a new suture button.
Discussion
First CMC arthritis is common cause of arthrosis in the hand that frequently requires surgery when symptoms are not resolved with conservative means. 10 11 12 13 14 15 16 17 18 19 20 21 22 23 Surgical treatments commonly performed for first CMC arthrosis include trapeziectomy (T), T + hematoma distraction arthroplasty, T + tendon interposition (TI), T + ligament reconstruction (LR), T + LRTI (ligament reconstruction and tendon interposition), and open or arthroscopic T + suspensionplasty. 11 In Eaton–Littler stage 2–3, CMC arthrosis surgical management is recommended but there are debates about treatment which include arthroscopic procedure, metacarpal extension osteotomy, and reconstruction of beak ligament (thermal shrinkage of Beak ligament), etc. 10 12 13
Trapeziectomy, was described by Gervis, is one of the earliest and most reliable treatments for pain associated with first CMC arthritis. 24 In a young and high demand patient trapeziectomy is often augmented by a procedure that promotes first CMC joint height, such as a suspensionplasty to prevent proximal migration of the first metacarpal toward the trapezial interval. 25 As the subsidence of the metacarpal decreases, the lever arm of the thumb and limits pinch strength which lead up to first CMC-scaphoid impingement. 25 26 Field and Buchanan described the first CMC joint stabilization after trapeziectomy with the use of a suture anchor without the need for tendon harvest. 27 The decreased operative time, decreased recovery time, limited dissection, and sparing of the flexor carpi radialis (FCR) tendon were the benefits of this technique. 27 However, the strength of the suture was questioned in the treatment of young males who necessitate greater strength for occupations and hobbies. 23
Suspensionplasty was first introduced by Thompson in 1986 as “salvage intervention” and the joint was reconstructed with tendon graft, after bone was totally resected. 17 The procedure resulted with patient satisfaction similar to that of LRTI, along with a technical advantage. 17 Sai et al and Sirotakova et al obtained good outcomes with tendon suspensionplasty. 18 19
Suspensionplasty was performed with tendon grafts in CMC arthrosis at early times, and the surgeons started using suture anchor over the time 14 but suture button suspensionplasty is the final modality of this technique. The main goal of suture button suspensionplasty is to eliminate pain while maintaining mobility and stability of the first CMC joint to restore the function. 2 Recently, suture button gained a place among other therapeutic modalities. 15 Offering semirigid fixation, this system has been long used in orthopaedic practice for acromioclavicular surgery, injury of syndesmosis in ankle, Lisfranc's fracture-dislocation and hallux valgus surgery. There are promising studies which demonstrate that early stage stability obtained in ankle procedures, where the device is exposed to high loading is maintained in the long term. 16
Putnam et al, in a series of 44 cases, performed trapeziectomy followed by suture suspensionplasty and they found improvement in pain and functional status in 91% of patients. Authors determined that the technique required less steps and does not lead to extra comorbidity. 14 Suture button suspensionplasty is a technique that can be implemented effectively and in a short surgery time with a 1 cm skin incision. The average surgery time in our practice was 20 minutes. By using two suture buttons, the first CMC joint subluxation reduction can be maintained the first metacarpal basis to second metacarpal.
In a series of suture button suspensionplasty following partial or total trapeziectomy, Szalay et al performed suspensionplasty with suture button in a series of 31 patients. They obtained good and very good outcomes in 75% of patients and satisfactory or poor outcomes in 12.5% of patients at the end of 13.5 months of follow-up period. 20 Endress and Kakar emphasized the technical superiority and provision of early daily life of suture button applications after trapeziectomy. 19 Yao and Song reported less complication and better outcomes relative to alternatives. The author mentioned that the technique does not require time for recovery and rehabilitation can be started soon, not later than 10 days. 1 Although K-wire stabilization and thumb spica cast for up to 6 weeks are described for hematoma and distraction arthroplasty, 27 Roman et al did not suggest K-wire stabilization and prolonged immobilization owing to the metacarpal suspension with this technique. 23 We did not apply a splint to our patients during postoperative period.
Suspensionplasty has similar results with LRTI but there are no long-term results. 22 23 Suspensionplasty with suture button supported by arthroscopy is combined with partial trapeziectomy. It is thought that the oblique vector of suture button created between the metacarpals optimally corrects both proximal migration and subluxation. 7 28 In our series, the impaired inclination of the joint was corrected and a more stable joint with normal load distribution was obtained with suture button in this technique and no tendon was used for suspension. Thus, the operation time is short and there is no morbidity for the donor site.
Song et al, in a cadaver model, showed that the obliquity of the tunnel between the metacarpals does not cause any difference in the range of motions and safely far from neurovascular structures in both application methods. 29 No symptoms associated with neurovascular injury were observed with suture button application in our patients. Yao and Song placed the suture button beneath a portion of the radial aspect of the abductor pollicis brevis tendon, thus decreasing the chance of postoperative hardware prominence. 1 We believe that the placement of the metal part of the suture button toward the abductor muscles would prevent the skin irritation of the metal part of the suture button.
Arthroscopy is effective in the treatment of first CMC arthrosis. 30 31 32 First CMC arthrosis treatment supported by arthroscopy in especially symptomatic patients with positive subluxation but no arthrosis signs, not only has low morbidity but also has the advantage of observing intraarticular pathologies and applying debridement, synovectomy, and thermal shrinkage. 33
Although trapeziectomy is recommended due to short surgery time, relative ease, absence of morbidity secondary to extra procedures, and alleviation of pain, it was considered that the procedure leads to decrease in gripping and grasping force and short digit–a cosmetic problem. 34 35 Because of these problems, we suggest to apply arthroscopic partial trapeziectomy instead of total trapeziectomy except in high stage disease. We believe that this will provide structural support for joint biomechanics and for reconstructive procedures (interposition or suspensionplasty) and will be important in clinical well-being for the long term. 23 Our method is effective for the young patients with it protecting the normal anatomy more and being less invasive. To our opinion, the prevention of the lateral subluxation of the first metacarpal in the early stages of the first CMC arthritis would be beneficial to prevent pantrapezial arthritis. In other words, a protective treatment would be applied to the patients. The technique and the material still need further biomechanical studies and evaluation in bigger series with longer follow-up periods.
This study has some limitations. First it was a retrospective study with a small number of patients. Landes et al reported the results of 153 cases of arthroscopic trapeziectomy with suture button suspensionplasty performed in 136 patients with the 58 weeks of follow-up period. 36 The follow-up period in our study was 50.1 months (range: 48–60 months). In our study, we did not include the patients with the early and midterm follow-up period. Because of this reason we did not have a large series as Landes et al. In our study, we included only the patients with Eaton–Littler stage 2 and 3 arthrosis but the 38% of the patients in the study of Landes et al were Eaton–Littler stage 4. 36 This is the another important difference between the patients numbers of our study and the study of Landes et al Additionally, they included 56 patients that they had treated with total trapeziectomy. 36 We included only those patients who were treated with partial trapeziectomy to our study. Landes et al highlighted that long-term follow-up studies are necessary to evaluate both the longevity and efficacy of this procedure. 36 To our opinion, our study responds to what Landes et al emphasizes and we plan to publish the results of our long-term series in the future. Another important limitation is that this technique was not compared with another technique. Additionally, we did not include a control group in our study.
Conclusion
In conclusion, there are several treatments of first CMC arthrosis but based on published studies none of these treatment methods are superior to others. Most of Eaton–Littler stage 2 and 3 patients are left to live with pain decreasing their quality of life, to be operated at older ages with a more progressed disease. Arthroscopic hemitrapeziectomy and suture button suspensionplasty, are minimal invasive techniques, control the lateral subluxation and instability, provide pain relief with functional hand, and can be performed with low morbidity in the treatment of first CMC joint Eaton–Littler stage 2 and 3 arthrosis. By this technique, the patients' existing instability and pain problems can be solved and the patients can return to daily activities and work in the postoperative early period of time.
Conflict of Interest None declared.
Note
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The study was approved by our institutional review board and ethics committee. This study was performed in IST-EL Hand Surgery, Microsurgery, and Rehabilitation Group, Gaziosmanpaşa.
References
- 1.Yao J, Song Y. Suture-button suspensionplasty for thumb carpometacarpal arthritis: a minimum 2-year follow-up. J Hand Surg Am. 2013;38(06):1161–1165. doi: 10.1016/j.jhsa.2013.02.040. [DOI] [PubMed] [Google Scholar]
- 2.Yao J, Zlotolow D A, Murdock R, Christian M. Suture button compared with K-wire fixation for maintenance of posttrapeziectomy space height in a cadaver model of lateral pinch. J Hand Surg Am. 2010;35(12):2061–2065. doi: 10.1016/j.jhsa.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Brunton L M, Wilgis E F. A survey to determine current practice patterns in the surgical treatment of advanced thumb carpometacarpal osteoarthrosis. Hand (N Y) 2010;5(04):415–422. doi: 10.1007/s11552-010-9275-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kapoutsis D V, Dardas A, Day C S. Carpometacarpal and scaphotrapeziotrapezoid arthritis: arthroscopy, arthroplasty, and arthrodesis. J Hand Surg Am. 2011;36(02):354–366. doi: 10.1016/j.jhsa.2010.11.047. [DOI] [PubMed] [Google Scholar]
- 5.Park M J, Lichtman G, Christian J B et al. Surgical treatment of thumb carpometacarpal joint arthritis: a single institution experience from 1995-2005. Hand (N Y) 2008;3(04):304–310. doi: 10.1007/s11552-008-9109-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vermeulen G M, Slijper H, Feitz R, Hovius S E, Moojen T M, Selles R W. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36(01):157–169. doi: 10.1016/j.jhsa.2010.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Eaton R G, Littler J W. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55(08):1655–1666. [PubMed] [Google Scholar]
- 8.Badia A. Trapeziometacarpal arthroscopy: a classification and treatment algorithm. Hand Clin. 2006;22(02):153–163. doi: 10.1016/j.hcl.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Kapandji A. [Clinical test of apposition and counter-apposition of the thumb] Ann Chir Main. 1986;5(01):67–73. doi: 10.1016/s0753-9053(86)80053-9. [DOI] [PubMed] [Google Scholar]
- 10.Croog A S, Rettig M E. Newest advances in the operative treatment of basal joint arthritis. Bull NYU Hosp Jt Dis. 2007;65(01):78–86. [PubMed] [Google Scholar]
- 11.Gillis J, Calder K, Williams J. Review of thumb carpometacarpal arthritis classification, treatment and outcomes. Can J Plast Surg. 2011;19(04):134–138. doi: 10.1177/229255031101900409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glickel S Z, Gupta S. Ligament reconstruction. Hand Clin. 2006;22(02):143–151. doi: 10.1016/j.hcl.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 13.Wilson J N. Basal osteotomy of the first metacarpal in the treatment of arthritis of the carpometacarpal joint of the thumb. Br J Surg. 1973;60(11):854–858. doi: 10.1002/bjs.1800601106. [DOI] [PubMed] [Google Scholar]
- 14.Putnam M D, Meyer N J, Baker D, Brehmer J, Carlson B D. Trapezium excision and suture suspensionplasty (TESS) for the treatment of thumb carpometacarpal arthritis. Tech Hand Up Extrem Surg. 2014;18(02):102–108. doi: 10.1097/BTH.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 15.Putnam M D, Rattay R, Wentorf F. Biomechanical tests of three methods to treat thumb CMC arthritis. J Wrist Surg. 2014;3(02):107–113. doi: 10.1055/s-0034-1372518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rigby R B, Cottom J M. Does the Arthrex TightRope provide maintenance of the distal tibiofibular syndesmosis? A 2-year follow-up of 64 TightRopes in 37 patients. J Foot Ankle Surg. 2013;52(05):563–567. doi: 10.1053/j.jfas.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 17.Thompson J S. Surgical treatment of trapeziometacarpal arthrosis. Adv Orthop Surg. 1986;10:105–120. [Google Scholar]
- 18.Sai S, Fujii K, Chino H, Inoue J. Tendon suspension sling arthroplasty for degenerative arthritis of the thumb trapeziometacarpal joint: long-term follow-up. J Orthop Sci. 2004;9(06):576–580. doi: 10.1007/s00776-004-0826-z. [DOI] [PubMed] [Google Scholar]
- 19.Sirotakova M, Figus A, Elliot D. A new abductor pollicis longus suspension arthroplasty. J Hand Surg Am. 2007;32(01):12–22. doi: 10.1016/j.jhsa.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 20.Szalay G, Scheufens T, Alt V, Boecker W, Schnettler R. [Operative treatment of rhizarthrosis with trapezectomy and suspension of the first metacarpal with a Mini TightRope] Handchir Mikrochir Plast Chir. 2014;46(03):179–185. doi: 10.1055/s-0034-1368715. [DOI] [PubMed] [Google Scholar]
- 21.Endress R D, Kakar S. Double tightrope for basilar thumb arthritis. J Hand Surg Am. 2014;39(12):2512–2516. doi: 10.1016/j.jhsa.2014.09.012. [DOI] [PubMed] [Google Scholar]
- 22.Bednar M S. Philadelphia: Lippincott Williams & Wilkins; 2004. Osteoarthritis of the hand and digits: thumb; pp. 1279–1288. [Google Scholar]
- 23.Roman P B, Linnell J D, Moore J B. Trapeziectomy arthroplasty with suture suspension: short- to medium-term outcomes from a single-surgeon experience. J Hand Surg Am. 2016;41(01):34–390. doi: 10.1016/j.jhsa.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 24.Gervis W H.Excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint J Bone Joint Surg Br 194931B04537–539., illust [PubMed] [Google Scholar]
- 25.Hooke A W, Parry J A, Kakar S. Mini tightrope fixation versus ligament reconstruction–tendon interposition for maintenance of post-trapeziectomy space height: a biomechanical study. J Hand Surg Am. 2016;41(03):399–403. doi: 10.1016/j.jhsa.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 26.Tomaino M M. Suspensionplasty for basal joint arthritis: why and how. Hand Clin. 2006;22(02):171–175. doi: 10.1016/j.hcl.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Field J, Buchanan D. To suspend or not to suspend: a randomised single blind trial of simple trapeziectomy versus trapeziectomy and flexor carpi radialis suspension. J Hand Surg Eur Vol. 2007;32(04):462–466. doi: 10.1016/J.JHSB.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 28.Cox C A, Zlotolow D A, Yao J. Suture button suspensionplasty after arthroscopic hemitrapeziectomy for treatment of thumb carpometacarpal arthritis. Arthroscopy. 2010;26(10):1395–1403. doi: 10.1016/j.arthro.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Song Y, Cox C A, Yao J. Suture button suspension following trapeziectomy in a cadaver model. Hand (N Y) 2013;8(02):195–200. doi: 10.1007/s11552-012-9473-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Earp B E, Leung A C, Blazar P E, Simmons B P. Arthroscopic hemitrapeziectomy with tendon interposition for arthritis at the first carpometacarpal joint. Tech Hand Up Extrem Surg. 2008;12(01):38–42. doi: 10.1097/BTH.0b013e31813e0c3b. [DOI] [PubMed] [Google Scholar]
- 31.Adams J E, Merten S M, Steinmann S P. Arthroscopic interposition arthroplasty of the first carpometacarpal joint. J Hand Surg Eur Vol. 2007;32(03):268–274. doi: 10.1016/J.JHSB.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 32.Menon J. Arthroscopic management of trapeziometacarpal joint arthritis of the thumb. Arthroscopy. 1996;12(05):581–587. doi: 10.1016/s0749-8063(96)90198-x. [DOI] [PubMed] [Google Scholar]
- 33.Badia A. Arthroscopy of the trapeziometacarpal and metacarpophalangeal joints. J Hand Surg Am. 2007;32(05):707–724. doi: 10.1016/j.jhsa.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 34.Pellegrini V D., Jr . New York: McGraw-Hill; 1996. The basal articulations of the thumb: pain, instability, and osteoarthritis; pp. 1019–1039. [Google Scholar]
- 35.Murley A HG. Excision of the trapezium in osteoarthritis of the first carpo-metacarpal joint. J Bone Joint Surg Br. 1960;42B(03):502–507. [Google Scholar]
- 36.Landes G, Gaspar M P, Goljan P, Jacoby S M, Bachoura A, Culp R W. Arthroscopic trapeziectomy with suture button suspensionplasty: a retrospective review of 153 cases. Hand (N Y) 2016;11(02):232–237. doi: 10.1177/1558944715616955. [DOI] [PMC free article] [PubMed] [Google Scholar]


