Abstract
Social support enhances self-management and prevention of behaviors and is typically assessed using self-report scales; however, little is known about the validity of these scales in HIV-infected or affected populations. This systematic review aims to identify available validated social support scales used in HIV-infected and HIV-affected populations. A systematic literature search using key search terms was conducted in electronic databases. After rounds abstract screenings, full-text reviews, and data abstraction 17 studies remained, two of which assessed multiple social support scales, which increased number of scales to 19. Most scales assessed positive social support behaviors (n=18). Most scales assessed perceived social support (n=14) compared to received social support. Reliability ranged from 0.67 – 0.97. The most common forms of validation reported were content validity and construct validity and the least was criterion-related validity. Future research should seek to build evidence for validation for existing scales used in HIV-infected or HIV-affected populations.
Keywords: social support, HIV/AIDS, measurement, validation, reliability
INTRODUCTION
Social support is a psychosocial factor that has been broadly demonstrated to improve health, including mortality, in a variety of chronic illnesses and conditions (1). Cassel (2) originally conceptualized social support as an environmental variable: a resource that resides outside of the individual. Putting greater emphasis on interaction, the definition of social support has remained fairly consistent in the literature as: “an exchange of resources between two individuals perceived by the provider or recipient to be intended to enhance the well-being of the recipient” (3). While these definitions have operationalized the construct of social support to some extent, they obscure its complexity. Social support is broadly examined as either perceived or received social support (1). Perceived social support refers to an individual’s perception that support would be available, whenever needed. Received social support is the exchange of support resources within a specific timeframe (4). Whether perceived or received, social support is a multifaceted construct that can be characterized as : 1) emotional support (expression of positive affect, encouragement, and empathetic understanding); 2) informational support (offering advice, information, and feedback); 3) instrumental or tangible support (provision of behavioral assistance and material aid); 4) appraisal support (feedback or affirmation on behaviors); 5) positive social interactions; and 6) the extent of a supportive social network (5).
In practice, social support is measured in a variety of ways, typically using self-report scales. While no one social support scale can address all facets of social support, experts suggest that each scale should be theoretically grounded and the types of support they purport to measure clearly outlined (6). For example, social support scales can measure overall social support or one specific dimension of support (i.e., emotional support). They can assess social support from the perspective of the individual or from multiple perspectives (7). They can assess it from the perspective of the individual receiving it or those giving it, and some also assess the type of support or the specific source of support, such as the Friend Emotional Support Scale (8). Alternatively, instead of measuring the presence of support, researchers have also developed scales to measure either a lack of social support in the form of loneliness (e.g., UCLA Loneliness Scale) or poor social interactions (e.g., Unsupportive Social Interactions Inventory) (9, 10).
Social support is not only considered an important determinant that affects general health and well-being but is also recognized as a critical protective factor for people living with or at high risk of chronic illnesses. Uchino (11) conducted a review of the literature and found that social support is associated with more positive immune function, both through behavioral processes and psychological processes. Social support promotes healthier behaviors, such as exercise, quality diet, adhering to medical regimens, and not smoking, which in turn can improve immune function. Social support can directly affect psychological processes such as appraisals, emotions, or moods (11). This has been shown to be particularly important in the case of HIV infection (12, 13). Studies of HIV-positive populations found that high levels of social support can improve physical and psychological health outcomes (14-16). Among people living with HIV, social support enhances self-management and prevention behaviors; among those at high risk for HIV, it is associated with carrying out preventive behaviors. Psychologically, social support systems can alleviate the adverse effects of stressful events, serve as positive reinforcement for healthful behaviors, such as adhering to medication, and discourage harmful behaviors (e.g., excessive alcohol use) (16).
Conversely, low social support is associated with poorer physical and mental function among people infected with HIV, as well as faster progression from HIV to AIDS on two levels, biologically and behaviorally (16-18). Biologically, HIV-positive individuals with lower social support have been shown to have higher cortisol levels, which in turn can stimulate the replication of HIV-1 virus, modify programmed cell death, and alter the pattern of cytokines secreted (19). Behaviorally, an HIV diagnosis can be a stressful or traumatic event, and social support can buffer its effects. Moreover, during the treatment period, an individual’s support system can help them navigate the health system and can improve key adherence behaviors (20). Relatedly, not all forms of social support are inherently positive. Studies have shown that negative social support (e.g., criticism, demands, providing unwanted advice) is associated with adverse physical and mental health conditions (21, 22). Negative social support can be a source of stress, and is associated with tobacco use, physical inactivity, and excessive food consumption as well as poor outcomes among people with HIV (21, 23).
Importantly, social support may be a critical factor for HIV prevention, particularly for populations that are high risk. For example, men who have sex with men (MSM) who are HIV-negative have been found to have more close friends in their support networks compared to HIV-positive MSM (15) and are less likely to report unprotected anal intercourse than those with smaller support networks (24). Moreover, peer social support has been shown to be positively and robustly linked with HIV testing among young Black/African American MSM (13), the population currently most affected by HIV (25). Social support systems have also played a role in helping people who inject drugs (PWID) remain uninfected with HIV by providing meals, shelter, and necessary supplies (e.g., clean needles) (26).
While social support is an important psychosocial determinant of health for both people with and at risk of HIV infection, measuring social support is complex. As researchers and practitioners increasingly utilize scales to measure social support among HIV-affected populations (27) there is a need to facilitate the use of valid and reliable scales to strengthen this body of literature. As the best ways to measure social support vary depending on the specific dimension of interest to researchers, it is important that researchers be able to measure social support not only accurately but also appropriately for the purpose, setting and population of their studies. In addition, researchers may assess an individual’s general level of social support (28) or assess social support specific to an individual, behavior, or setting of interest such as safe sex, sharing needles, or HIV screening (29). To address this need, we conducted a systematic review aimed to identify, characterize, and synthesize available validated self-reported social support scales used among adults at-risk of or living with HIV.
METHODS
Our review of the literature was designed to capture studies from all geographic regions that characterized the psychometric properties of social support scales developed for and/or used in people with HIV or HIV-affected populations. We conducted this systematic review in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (30). We also consulted with faculty and staff at the university Center for AIDS Research (CFAR), who provided technical assistance and expertise in the development of systematic review protocol.
Data Source
Informed by a subject matter expert and University librarian, we conducted the literature search in April 2017 using five electronic databases: Pubmed, PsycTESTS, PsycINFO, CINAHL, and Cochrane Reviews. We generated a tailored list of search terms, for each electronic database, and worked with a subject matter expert to refine terms. Social support terms included: “social support,” “belonging support,” “tangible support,” “emotional support,” “perceived support,” “social network,” “peer support,” “family support,” “alienation,” and “social isolation.” scale-specific terms included: “instrument,’ “survey,” “measure,” “scale,” “questionnaire,” “assessment,” and “psychometric.” Terms we used to help identify studies that assess scale validity were: “valid,” “reliability,” “Cronbach’s alpha,” and “alpha.” Additional keywords were added to the database to specify our topic area, such as “HIV”, “AIDS”, “acquired immune deficiency syndrome” and “human immunodeficiency virus”. In addition to the studies identified from the literature search, we identified studies for data abstraction from hand searches – a review of the reference list from key systematic reviews and meta-analyses. All citations were imported into EndNote X8 for data management. The search yielded 1,757 records.
Inclusion and Exclusion Criteria
We were interested in scales that measured social support from the perspective of the recipient. To do this we identified studies that either (a) measured social support in people living with HIV or HIV-affected populations using a quantitative methodology or (b) reported the association between social support and an HIV-related outcome, such as HIV testing, sexual risk behaviors, or ART or PrEP adherence. Additionally, studies were required to meet all of the following eligibility criteria: (1) were peer-reviewed and published in English prior to April 2017; (2) presented reliability and/or validity information of social support-specific measures; and (3) assessed participants ≥18 years old, including studies that evaluated participants both under and over 18 years. We did not include studies of participants only in the child and adolescent developmental periods because social support manifests itself differently in those populations than in adults (31). Scales developed in a language other than English but presented in an article written in English were included. Studies that reported findings using different study populations or different scales over the same period were counted as separate studies. Systematic reviews or meta-analyses that focused on social support or social support scales were also included.
Studies were excluded if they: (1) measured social support as a sub-scale for a broader domain (i.e. quality of life) or (2) measured constructs theoretically distinct from social support (such as coping, patient/provider decision making, stigma and perceived discrimination, or community mobilization).
Screening
Candidate studies underwent three levels of review: abstract, full-text, and data abstraction, to produce a final list of studies that fit our criteria. To identify eligible studies for data abstraction, we first uploaded abstracts to Abstrackr, an online abstract review tool (http://abstrackr.cebm.brown.edu). Three teams, each comprised of two trained research assistants, screened all titles and abstracts. The full team participated in weekly phone calls to resolve disagreements, reach consensus, and revisit the inclusion/exclusion criteria. Any disagreements regarding abstract inclusion between reviewers for which consensus was not reached were included in full-text review. For the full text review, three teams of two closely assessed studies for whether they had reported on the reliability or validity of a social support-specific scale. We moved studies that presented both reliability and validity forward to full data abstraction. However, studies identified during full text review that otherwise met eligibility but only reported reliability and not validity had a few details extracted (e.g., name of scale, alpha value, population) and are presented in Table IV.
Table IV.
Reliability-only studies (reported alphabetically by scale name)
| Author, Year | Scale Name | Target Population | Country | Alpha |
|---|---|---|---|---|
| Luszczynska (2007) | Berlin Social Support Scales | HIV+ Patients | India | 0.78 |
| Rzeszutek (2015) | Berlin Social Support Scales | HIV+ Patients | Poland | 0.74–0.90 |
| Schulz (2004) | Berlin Social Support Scales | HIV+ Patients | Germany | 0.67-0.85 |
| Hong (2008) | Environmental Support | Female Sex Workers | China | 0.73 |
| Qiao (2016) | Funk & Rogge Social Support Scale | HIV+ Patients | China | 0.81 |
| Siegel (1994) | Index of Negative (illness-related) Network Interactions | HIV+ Gay Men | United States | 0.52 |
| Siegel (1994) | Index of Positive (illness-related) Network Interactions | HIV+ Gay Men | United States | 0.6 |
| Tate (2006) | Instrumental Support Evaluation List | HIV+ Gay and Bisexual Men | United States | 0.94 |
| Gray (1999) | Interpersonal Relationships Inventory Scale | HIV+ Women | United States | 0.9 |
| Gray (2002) | Interpersonal Relationships Inventory Scale | HIV+ Women | United States | 0.87 |
| Shannon (2008) | Interpersonal Relationships Inventory Scale - Short Form |
HIV+ mothers | United States | 0.98 |
| Burrage (2003) | Interpersonal Support Evaluation List (ISEL)–General Population | HIV+ Patients | United States | 0.68-0.92 |
| Emlet (2006) | Lubben Social Network | HIV+ Patients | United States | 0.82 |
| Beaulieu (2012) | Medical Outcomes Social Support Survey (MOS-SSS) | HIV+ Females | Canada | 0.96 |
| Hinnen (2012) | Medical Outcomes Social Support Survey (MOS-SSS) | HIV+ Patients | Amsterdam | 0.95 |
| Mclnerney (2008) | Medical Outcomes Social Support Survey (MOS-SSS) | HIV+/AIDS Patients | South Africa | 0.91 |
| Meade (2005) | Medical Outcomes Social Support Survey (MOS-SSS) | HIV+ Adults with Severe Mental Illness | United States | 0.91 |
| Watt (2010) | Medical Outcomes Social Support Survey (MOS-SSS) | HIV+ Patients | Tanzania | 0.86 |
| Goodman (2016) | Multidimensional Scale of Perceived Social Support | HIV+ Women | Kenya | 0.94 |
| Li (2009) | Multidimensional Scale of Perceived Social Support | HIV+ Patients | Thailand | 0.91 |
| Nyamathi (1996) | Multidimensional Scale of Perceived Social Support | HIV−, Homeless Individuals | United States | 0.74 |
| Sajjadi (2015) | Multidimensional Scale of Perceived Social Support | HIV+/AIDS Patients | Iran | n/r |
| Clingerman (2003) | Norbeck Social Support Questionnaire | HIV+ Patients | United States | 0.95 |
| Kipp (2015) | O’Brien Social Support Scale | HIV+ Patients | United States | 0.91 |
| O"Brien (1993) | Perceived Availability of Support | HIV+ Men | United States | 0.87 |
| Rodgers (1995) | Perceived Social Support - Friends Scale | AIDS, Men | United States | 0.96 |
| Serovich (2001) | Perceived Social Support - Friends Scale (PSS-Fr) | HIV+ Women | United States | 0.89 |
| Chibnall (2002) | Perceived Social Support Inventory | Patients with life threatening conditions | United States | 0.97 |
| Su (2013) | Perceived Social Support Scale | HIV+ Patients | China | 0.89 |
| Serovich (2001) | Perceived Social Support-Family Scale (PSS-Fa) | HIV+ Women | United States | 0.9 |
| Fleishman (1994) | Perceived Tangible Support | HIV+ Patients | United States | 0.85 |
| Chen (2001) | Personal Resource Questionnaire 85 part 2 | HIV+ Patients & Cancer Patients | China | 0.86 |
| Tangkawanich (2008) | Personal Resource Questionnaire 85 part 2 | HIV+ Patients | Thailand | 0.85 |
| Heckman (1997) | Provision of Social Relations Scale | HIV+ Patients | United States | 0.88 |
| Kyle (1994) | Provision of Social Relations Scale | HIV+/AIDS Patients | United States | 0.84 |
| Shah (2015) | Revised Lubben Social Support scale | HIV+ Heterosexual Men | United States | 0.81 |
| Diaz (2001) | Social Isolation Scale | Gay and Bisexual Males | United States | 0.78 |
| Organista (2005) | Social Isolation Scale | Migrant Day Laborers | United States | 0.71 |
| Blaney (1997) | Social Provisions Scale | HIV+ Gay Men | United States | 0.88 |
| Murphy (2002) | Social Provisions Scale | HIV+ Patients | United States | 0.69 |
| Toth (2013) | Social Provisions Scale | HIV+ Women of Color | United States | 0.84 |
| Rongkavilit (2010) | Social Provisions Scale - Short Form | HIV+, Thai youth | Thailand | 0.9 |
| Persons (2010) | Social Relationship Scale | HIV+ Patients with history of child abuse | United States | 0.85 |
| Turner-Cobb (2002) | Social Support Inventory | HIV+ Patients | United States | 0.81 |
| Pinto (2005) | Social Support Network Inventory | HIV−, low-income, young African American women |
United States | 0.79 |
| Hart (2005) | Social Support Questionnaire | Gay and Bisexual Males | United States | 0.86 |
| John (2002) | Social Support Questionnaire | HIV+ Patients | Nigeria | NR |
| Sethosa (2005) | Social Support Questionnaire | HIV+ Patients | South Africa | 0.65 |
| Wyatt (1997) | Social Support Questionnaire | HIV+ Mothers | United States | 0.82 |
| Robbins (2003) | Social Support Questionnaire 6-item version | HIV+ African American Women | United States | 0.67 |
| Prado (2002) | Social Support Questionnaire—Short Form | HIV+ African American Women | United States | 0.87 |
| Ma (2015) | Social Support Rating Scale | Married Migrant Women | China | 0.73 |
| Waddell (2006) | Social Support Scale | HIV+ Patients | United States | 0.89 |
| Gore-Felton (2002) | UCLA Measure of Social Support | HIV+ Patients | United States | 0.96 |
| Gore-Felton (2008) | UCLA Social Support Inventory | HIV+ Patients | United States | 0.87 |
| Simoni (2000) | UCLA Social Support Inventory | HIV+ Black Women | United States | 0.86 |
| Simoni (2006) | UCLA Social Support Inventory | HIV+ African American and Latino adults | United States | 0.69-0.75 |
| Hutton (2014) | Unsupportive Social Interactions Inventory (HIV-version) | HIV+ Patients | Australia | 0.95 |
Notes: NR = not reported
Data Abstraction
We worked with a social support subject matter expert and used the Scientific Advisory Committee of the Medical Outcomes Trust criteria (32) to develop a structured data abstraction form to extract key information in a standardized manner from each article. Each article was doubly extracted via two pairs of trained reviewers that extracted scale names, study characteristics (i.e., population tested, study location), dimensions tested using the names assigned by the study as well as reliability, validity, and structural validity information to ensure selection bias was avoided (33) (see Table I). The first author reviewed all data abstractions for quality assurance. Two studies validated more than one social support scale, resulting in a greater final number of HIV/AIDS social support scales than the number of final studies included in the review.
Table I.
Scale reliability or validity definitions
| Reliability or Validity Type | Definition |
|---|---|
| Reliability | Internal consistency reliability is concerned with the homogeneity of the items in a scale; also called Cronbach’s alpha, coefficient alpha, or simply alpha (α). |
| Test-retest Reliability | Assesses temporal stability of a scale or the consistency of scores from one time to another. |
| Content Validity | The extent to which a set of indicators reflects a content domain (e.g., social support). Methods of engaging in content validity are conducting literature reviews, having items reviewed by a panel of subject-matter experts, having items review by target population through focus groups, pretests, pilot studies, and/or interviews. |
| Criterion-related Validity | The extent item or scale has an empirical association with some criterion, or gold standard. - Predictive validity: concerned with if the scale can predict a process. - Concurrent validity: The extent to which the results of a scale’s score corresponds to those of previously established scales, for the same construct. |
| Construct Validity | The theoretical relationship the item or scale has with other items/scales, such that the scale behaves the way it is expected to behave. - Convergent Validity: Scales or items that are theoretically correlated demonstrate that they are in fact correlated. - Discriminant Validity: Scales or items that are theoretically uncorrelated demonstrate that they are in fact uncorrelated. |
| Known-group Validity | Demonstrates that the scale scores can differentiate between one group and another. Can be considered either construct or criterion-related validity depending on the intention of the researchers. |
| Structural Validity | Use of confirmatory factor analysis to verify the number of latent variables underlie a set of times in a scale. |
RESULTS
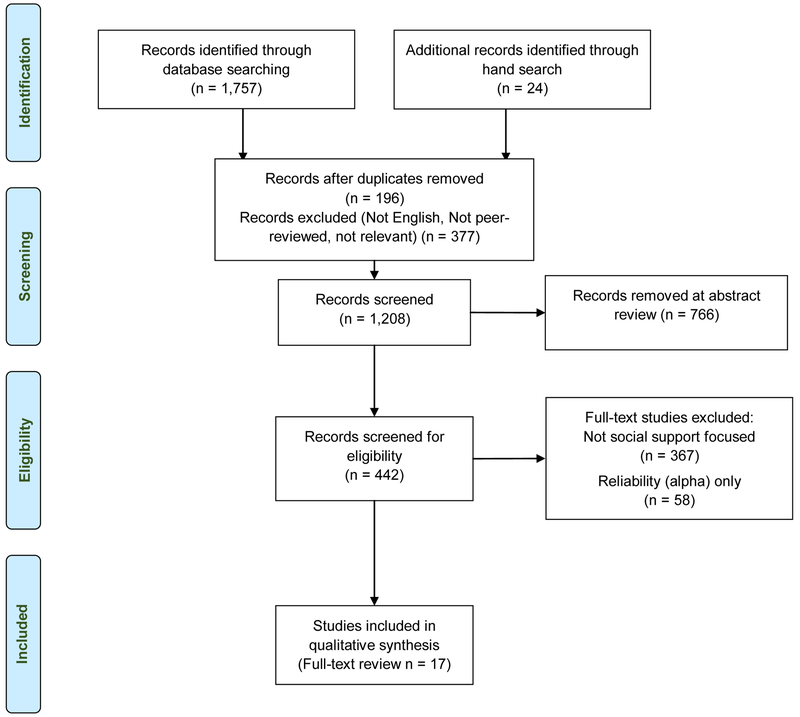
After we screened out duplicates (n=196), non-English studies, and non-peer reviewed studies (n=377) during title and abstract review, 1,208 citations remained for further screening. From these, during title/abstract and full-text review stages, we excluded 766 and 425 additional studies, respectively, leaving 17 studies. Figure 1 summarizes the review process for each step of the review. This review yielded 17 unique studies that presented reliability and validity information for 19 scales. The reliability and validity characteristics of the 19 social support scales as related to HIV-infected or HIV-affected populations are summarized in Table III. Four of the 19 scales had been created specifically to measure social support related to HIV (34-36). In addition, we identified 58 studies that otherwise met eligibility criteria but only reported reliability and not validity information, which are included in Table IV.
Figure 1.
Social Support Systematic Review Flow Diagram
Table III.
Characteristics of Measures of Social Support and Key Findings Pertinent to Measure Characteristics, Reliability and Validity among Studies with Individuals at Risk For or with HIV/AIDS
| Measure of Social Support (Language if Other than English) | Population (Citation) | Key Findings |
|---|---|---|
|
Access to Resources Scale • Evaluates support from relatives, non-using friends, and neighbors Subscales: • Support from family/non-using friends; Support from drug users; Support from program staff |
Injection drug users who injected heroin and/or other drugs (Vazan et al., 2012) |
Language: English # Items: 25 Factor Analysis: Confirmed subscales and items Alpha: 0.86 Content Validity: Pilot tested concept questions that emerged from 35 in-depth interviews with IDU participants; question wording was assessed by IDU participants; assessed correlations between items and dropped poorly reliable items |
|
Duke-UNC Functional Support Questionnaire (DUFSS) • Evaluates perceived social support in family medicine settings Subscales • Perceived social support |
HIV+ adults who initiated ARTs in Rwanda (Epino et al., 2012) Palliative care patients (Saracino et al., 2015) |
Language: Kinyarwanda (Rwanda) # Items: 8 Factor Analysis: Confirmed scale structure and items Alpha: 0.91 Construct Validity: • MOS-HIV mental health were weakly correlated with DUFSS scores [convergent] • Depression scores (HSCL-15) correlated inversely with the DUFSS scale (r = −0.30, p<0.0001) [discriminant validity] • Tested whether scale score predicted clinical indicators of HIV severity (disease stage, body mass index, CD4 cell count). Compared scores with lower physical health scores to those with higher physical health scores. [known group] Language: English # Items: 5 or 14 Factor Analysis: Confirmed scale structure and items Alpha: 0.80 (5-item) & 0.91 (14-item) Content Validity: Patients with advanced AIDS as well as advanced cancer patients were recruited to test initial scale questions Construct Validity: • Assessed correlations between the DUFSS-14 and DUFSS-5 and the Beck Depression Inventory (BDI), McGill Quality of Life Questionnaire (MQoL), and the Schedule o Attitudes Toward Hastened Death (SAHD). [convergent] ∘ 5-item: DUFSS-5 and BDI (r= −0.29, p< 0.001); DUFSS-5 and MQoL (r= 0.36, p<0.001); DUFSS-5 and SAHD (r= −0.27, p<0.001) ∘ 14-item: DUFSS-14 and BDI (r= −0.34, p<0.001); DUFSS-14 and MQoL (r=0.41, p<0.001); DUFSS-14 and SAHS (r= −0.29, p<0.001) |
|
HIV-Negative Social Provisions Scale • Evaluates general social support for individuals who are HIV-negative but are partnered with an individual who is HIV-positive Subscales: Not reported |
Adult, gay couples (Darbes et al., 2005) |
Language: English # Items: 24 Factor Analysis: Not reported Alpha: 0.84 Test -retest: 0.71 Construct Validity: • Compared scores between HIV+ and HIV− groups [known group] Criterion-related Validity: • Greater levels of HIV-specific support predicted less HIV risk behaviors cross-sectionally (F(1, 54) = 7.18, p = 0.01, b = −.166) and longitudinally |
|
HIV-Positive Social Provisions Scale
• Evaluates general social support for individuals who are HIV-positive but are partnered with an individual who is HIV-negative Subscales: Not reported |
Adult, gay couples (Darbes et al., 2005) |
Language: English # Items: 24 Factor Analysis: Not reported Alpha: 0.87 Test-retest: 0.74 Construct Validity: • Compared scores between HIV+ and HIV− groups [known group] Criterion-related Validity: • Greater levels of HIV-specific support predicted less HIV risk behaviors cross-sectionally (F(1, 54) = 7.18, p = 0.01, b = −.166) and longitudinally |
|
Instrument Support Evaluation List
• Examines social support in HIV-positive individuals Subscales: • Tangible, Appraisal, Emotional |
HIV+ individuals in Venezuela attending support groups (Bastardo et al., 2000) |
Language: Spanish # Items: 40 Factor Analysis: Confirmed scale structure and items Alpha: 0.85 Content Validity: • Evaluated the original ISEL for language and cultural adaption in Venezuela using in-depth interviews |
|
Medical Outcomes Study – Social
Support Survey • Evaluates social support in individuals with chronic illness Subscales (Kim et al., 2017; Saddiki et al., 2017): Emotional/information; Tangible support; Positive social interaction; Affectionate support Subscales (Yu et al., 2015) Social-emotional support; Tangible support |
HIV+ adults who are incarcerated (Kim et al., 2017) HIV+ patients undergoing follow-up at infectious disease clinic in Malaysia (Saddiki et al., 2017) HIV+ adults living in Mainland China (Yu et al., 2015) |
Language: English # Items: 19 Factor Analysis: Confirmed scale structure and items using Rasch model Alpha: 0.90 Construct Validity: • Assessed validity using Rasch item hierarchy provided by the item difficulty estimates • Compared the level of social support between men and women using differential item functioning (DIF) and found no difference [known-group] Language: Malay # Items: 19 Factor Analysis: Confirmed scale structure and items Alpha: 0.96 Test-retest: 0.88 Content Validity: The translated to Malay version of the MOS-SSS and assessed the equivalence of the translated version to the original English version based on semantic equivalence, idiomatic equivalence, experiential equivalence, and conceptual equivalence. Scale was piloted with convenient sample of HIV patients. Construct Validity • Compared social support scores for each social support subscale and the overall functional social support between married and non-married patients Language: Mandarin # Items: 19 Factor Analysis: Confirmed scale structure and items Alpha: 0.91 – 0.96 Criterion-related Validity: • Concurrent validity of MOS-SSS tested using Person product-moment correlations with the Beck Depression Inventory Revised (BDI-II) (r = −0.41, p < 0.01), the Self-rating Anxiety Scale (SAS) (r = −0.27, p < 0.01), Perceived Stress Scale (PSS-10) (r = −0.30, p <0.01), and WHOQOL-BREF (r = 0.61, p <0.01) Construct Validity: • Scale assessed using correlation between each item and its respective subscale (item-own subscale). Correlations ranged 0.66 – 0.86. [convergent validity] • Scale assessed using correlation between item-own subscale correlation with the other item-other subscale correlations. Correlations ranged 0.53 – 0.69. [discriminant] |
|
Perceived Social Support Scale
• Evaluates perceived tangible support from family and friends Subscale: Tangible support |
HIV+ adult women (Hudson et al., 2001) |
Language: English # Items: 5 Alpha: 0.72 Content Validity: Examined items of against the domains of social support theory |
|
Scale of Perceived Social Support in HIV (PSS-HIV)
• Evaluates HIV/AIDS-related perceived social support Subscales: Belonging, Esteem, Self-development |
HIV+ and HIV− adults in the United Kingdom (Cortes et al., 2014) HIV+ and HIV− adults in Chile (Cortes et al., 2014) |
Language: English # Items: 12 Factor Analysis: Confirmed scale structure and items Alpha: 0.91 Content Validity: Literature review conducted to develop items, experts reviewed for item suitability, and scale was piloted in a sample of PLWH Construct Validity: • Compared the correlation between scale and the Hospital Anxiety Depression Scale (HADS). PSS-HIV negatively correlated with anxiety (r= −0.875, p< 0.01) and depression (r= −0.917, p< 0.01) [discriminant] • Subscale scores showed high correlations between each other and the full scale (r> 0.76, p< 0.01) [convergent] • Compared mean scores between HIV+ and HIV− samples in the UK (t = −4.13, p< 0.001) [known-group] Language: Spanish # Items: 12 Factor Analysis: Confirmed scale structure and items Alpha: 0.93 Content Validity: Translated from Spanish to English and assessed for semantic equivalence. Scale was pilot tested in HIV− and HIV+ samples Construct Validity: • Compared the correlation between scale and the Hospital Anxiety and Depression Scale (HADS). PSS-HIV negatively correlated with anxiety (r= −0.758, p< 0.01) and depression (r= −0.688, p< 0.01) [discriminant] • Subscale scores showed high correlations between each other and the full scale (r> 0.76, p<0.01) [convergent] • Compared mean scores between HIV+ and HIV− samples in Chile (t= 1.98, p< 0.049) [known-group] |
|
Social Support for PLWH
• Assesses available social support related to HIV and antiretroviral medications Subscales: Emotional/informational; Adherence support; Instrumental support |
Adults living with HIV (Dima et al., 2014) |
Language: Kiswahili # Items: 12 Factor Analysis: Alpha: 0.80 Content Validity: Used MOS-SSS items, qualitative work, and clinical experts to develop items, then piloted scale with convenient target sample Construct validity: • Voluntary disclosure was positively correlated with the emotional/information support subscale (T = .12, p< 0.05), instrumental support was positively correlated with disclosure to spouse/partner (T = .16, p< 0.05) but negatively correlated with disclosure to close family (T= −.14, p< 0.05). Adherence support was uncorrelated with disclosure. [convergent] |
|
Social Support Inventory for People Who are HIV Positive or Have AIDS
• Assesses 3 types of received social support for HIV+ individuals Subscales: Instrumental; Informational; Emotional Within each subscale the following was assessed: Have or whether support is received; Want or whether in individual wants the support; Satisfaction or how satisfied the individual is with support received; Source or who provides support (qualitative) |
Adults with HIV/AIDS recruited from clinics in Toronto, Canada (Renwick et al., 1999) |
Language: English # Items: 17 Factor Analysis: Confirmed scale structure and items Alpha: 0.38 – 0.89 Content Validity: Conducted a literature review, consulted with experts and persons living with HIV, conducted a thematic analysis of qualitative interviews with target group to identify supportive behaviors Construct validity: • Scores for the Have domains for each factor of support were correlated with the Instrument Support Evaluation List (ISEL) for correlations (r > 0.26; p < 0.01) [criterion-related] |
|
Social Support Questionnaire – Short Form (SSQ-6)
• Assesses available social support Subscales (Prado et al., 2004): Social support Subscale (Robbins et al., 2003): Social network size; Social support satisfaction |
HIV+ African American mothers (Prado et al, 2004) HIV+ African American women (Robbins et al., 2003) |
Language: English # Items: 6 Factor Analysis: Confirmed scale structure and items Alpha: 0.84 Language: English # Items: 6 Factor Analysis: Confirmed scale structure and items Alpha: 0.67 |
|
UCLA Social Support Inventory (UCLA-SSI)
• Assesses received social support Subscales: Types of support – Advice; Assistance; Reassurance; Listening Sources of support – Friends; Relatives; Partners; Groups |
Gay and bisexual men participating in research study (Schwarzer et al., 1994) |
Language: English # Items: 24 Factor Analysis: Confirmed scale structure and items Alpha: 0.77 – 0.80 Test-Retest: 0.47 Construct validity: • Four types of social support were strongly correlated (r > .71) [convergent] • Four source factors were weakly interrelated [discriminant] |
|
Unsupportive Social Interactions Inventory
• Evaluates unsupportive behavior related to specific stressor, in this case having HIV Subscales: • Insensitivity; Disconnecting; Forced Optimism; Blaming |
Adults living with HIV recruited through university medical center clinics (Ingram et al. 1999) |
Language: English # Items: 24 Factor Analysis: Confirmed subscales and items Alpha 0.81 – 0.89 Criterion Validity: Only one significant correlation with Social Support Questionnaire (Sarason et al., 1987) indicating unsupportive social interactions distinct from general support Construct Validity: • Depression (CES-D) and negative affectivity (PANAS) correlated with higher scores on Insensitivity, Disconnecting and Blaming subscales [convergent] • After control for physical functioning and general social support (Social Support Questionnaire), USII-18 accounted for 15% of variance in depression (CES-D) (p < 0.001) |
Populations
Of the 17 studies that were included in the final review, 10 studies were conducted in the United States, and seven were conducted in other countries. The similarities and differences between U.S.-based studies and global studies are presented below.
Domestic Populations
Geographic location of the 10 domestic studies ranged from California to the East Coast region; two studies were conducted in California (37, 38), three in New York City (8, 26, 39), two in the Southeast (12, 40), and three in multiple locations across the United States (9, 35, 41). All domestic studies used non-probability sampling methods to recruit study populations, and recruitment site type varied. Three studies recruited eligible study participants through health clinics (9, 37, 39), four recruited through community organizations (8, 26, 35, 40), and one recruited participants through prisons (41). Study sample sizes ranged from 38 (12) to 1,615 (39), with 8 of 10 studies reporting sample sizes between 100 to 600 participants.
Six of the 10 studies focused solely on people with HIV (8, 9, 12, 37, 40, 41). Three of those studies focused explicitly on female populations (12, 37, 40), including one study of African American mothers living with HIV (40). Two of the six studies recruited samples of gay or bisexual men only (35, 38), one study involved a sample of PWID (26), and one study targeted recently incarcerated individuals living with HIV (41). Average age of the study populations, when reported, ranged from 35 years (40) to 58 years (39).
Of the remaining studies, three involved HIV+ and HIV− negative populations. These studies included patients with advanced chronic conditions (including HIV) (39), populations that are HIV-affected such as PWID (26), and gay and bisexual men (38). The study by Darbes & Lewis (35) examined behaviors of gay couples but did not report on their HIV status.
Global Populations
Study locations of the seven global studies were Canada, Venezuela, Chile, the United Kingdom, Rwanda, China, Tanzania, and Malaysia (14, 34, 36, 42-45). Six studies employed non-probability sampling methods to recruit study participants, all six of which recruited participants from clinical settings; Bastardo et al. (14) also recruited participants through community support groups. Saddki et al. (44) used random sampling of patients at a hospital Infectious Disease Unit in Malaysia to generate the study sample. Five studies focused on adult patients already living with HIV, and one included both HIV-infected and HIV-negative adults. None of the global studies targeted only one gender, and the percent of the samples that were male ranged from 38% to 90% across all seven studies (36, 43). Two global studies utilized English-language scales (34, 36) and two utilized Spanish scales (14, 34). The remaining study scale languages included Kinyarwanda (43), Mandarin Chinese (45), Malay (44), and Kiswahili (42).
Social Support Scales
As shown in Table III, the number of items ranged from 5 – 40 for each scale. For two of the 19 scales, studies did not present information on the number of factors or dimensions underlying each scales (35). Of those that did, the range of dimensions assessed was 1 –4. Scales were coded as to the dimensions of social support they included: emotional support (8 scales), tangible/instrumental support (7 scales), general social support (4 scales), informational support (3 scales), and appraisal/esteem support (3 scales). Most of the studies that were evaluated used scales that assessed perceived social support (14 scales) compared to received social support (3 scales), with only one scale measuring unsupportive behaviors such as insensitivity and blaming. There was little overlap between the identified, validated scales regardless of if the scale assessed general social support or a specific domain of social support.
The internal-consistency reliability assessed using Cronbach’s alpha, for the overall scales ranged from 0.67-0.97. At the lower end of this range was the Social Support Questionnaire Short Form, which examines social support network size and support satisfaction (12). At the higher end of the range was the Mandarin version of the Medical Outcome Study-Social Support Survey (45). Overall, in this review 18 of 19 scales had achieved “acceptable” internal consistency, generally accepted as alphas greater than or equal to 0.70. Seven of 19 scales achieved excellent internal consistency at alphas greater than or less 0.90 (46). Test-re-test reliability was less commonly reported, with only 4 of the 19 scales reporting test-retest.
The most common forms of validation reported for these scales were content-related validity (12/19 scales) and convergent validity (10/19). For example, Ingram et al. (9) reported construct validity in assessing the correlation between the Unsupportive Social Interactions Inventory (USII) and depression (measured using CES-D), psychological distress (measured using the PANAS). The remaining construct-validity categories were reported in fewer studies, specifically discriminant validity was reported in 6 of 19 scales and known-group validity was reported in 7 of 19 scales. Criterion-related validity was reported for five scales. For example, Yu et al. (45) assessed concurrent validity, a form of criterion-related validity, between the Chinese Version of the Medical Outcomes Study Social Support Survey and the Beck Depression Inventory Revised, as well as the Perceived Stress Scale. No individual study we evaluated assessed all five validity attributes of interest. However, the Spanish and English versions of the Scale of Perceived Social Support in HIV did report on all validity attributes except for criterion-related validity. Of the 19 scales, 7 reported 3 out of 5 validity attributes (see Table III).
While we identified 19 different validated social support scales that were used throughout the 17studies of HIV-infected and at-risk populations reviewed, two legacy scales were used more often and therefore are described in detail below. These were the Medical Outcomes Study-Social Support Survey and the Social Support Scale-Short Form.
Medical Outcomes Study (MOS)-Social Support Survey
The Medical Outcomes Study (MOS)-Social Support Survey was originally developed and validated in patients with chronic conditions by Sherbourne & Stewart (47) for use in patients with chronic illnesses who were enrolled in the Medical Outcome Study in Boston, Chicago, and Los Angeles. The scale in its original form consists of 19 items that cover four dimensions of perceived social support: emotional/informational support, tangible support, positive social interaction, and affectionate support (47). Responses are measured on a 5-point scale, with response categories ranging from “none of the time” to “all of the time” (47). The scale was initially validated through comparison with scales of other constructs related to social support, including loneliness, emotional ties, family functioning, marital functioning, and mental health; tests of convergent validity with these concepts revealed high correlations between the MOS-Social Support Survey and these other scales. Cronbach’s alpha for the scale subscales and total scale in Sherbourne & Stewart’s (47) original study ranged from 0.91-0.97.
The MOS-Social Support Survey, either in its original form or slightly modified, was subsequently used to measure perceived social support among women living with HIV in Canada (48), adults receiving ART in Tanzania (49), patients with HIV in the Netherlands (50), psychiatric outpatients at risk of HIV in the Northeastern U.S. (51), and patients with HIV in South Africa (52); however, these studies did not validate the survey in these populations and are therefore not included as part of our review (see Table IV).
Three studies included in our final full review adapted the MOS-Social Support Survey and validated it for use in new populations using construct validity and confirming the factor structure of the scale (41, 44, 45). Yu et al. (45) translated the scale into Mandarin for use among people living with HIV in China (details of full adaption described below). A factor analysis conducted by the authors resulted in a two-factor solution with the same 19-item scale rather than the original four-factor solution; the two dimensions found were tangible support (i.e., material aid, service) and social-emotional support (i.e., affection, empathy, encouragement, advice, guidance) (45). Reliability of the adapted scale was high at 0.97 (45). Saddki et al. (44) adapted the original scale into Malay for use in Malaysian patients with HIV, and reported a four-factor solution with a Cronbach’s alpha of 0.96 and an ICC test-retest reliability score of 0.88 (see full adaption description below). Kim et al. (41) validated the full survey in prison populations in the U.S.; while the study reported high reliability of the scale in this population (0.90), the authors found floor and ceiling effects among prisoners. These results suggest that the MOS-Social Support Survey may not be entirely suitable for that study population, in that it does not provide sufficient variation to measure the full range of social support (41).
Social Support Scale/Social Support Scale-Short Form (SSQ-6)
The Social Support Scale was originally developed (item development and testing) and validated by Sarason et al. (53) in multiple cohorts of undergraduate students at the same institution, with the goal of measuring perceived social support. Validation included item analysis to systematically reduce the number of items to the 27 that best fit the data. Participants were asked to list individuals to whom they would turn for support or upon whom they felt that they could rely (in a series of different hypothetical circumstances), and were then asked to indicate how satisfied they were, in general, with each of these individuals using a scale of 1 – 6 (“very dissatisfied” to “very satisfied”) (53). Cronbach’s alpha for the original 27-item scale was 0.97 (53). A six-item short form of the scale was later developed and validated, again in undergraduate samples in the United States (Social Support Scale-Short Form/SSQ6) (54).
The Social Support Scale or the SSQ-6 was later used in HIV-infected or HIV-affected populations, including young gay and bisexual males at risk of contracting HIV in the eastern U.S. (55) and mothers living with HIV (56). Reliability of the scale ranged from 0.82 to 0.89 in these populations; however, these studies provided no validity information and where therefore not included in our review (55, 56) (see Table IV).
Two studies included in the final review validated the factor structure of the SSQ-6 in new populations (12, 40). Robbins et al. (12) administered the SSQ-6 to HIV+ African American women in the Southeastern region of the United States; reliability of the scale was 0.67 and two factors (social network size and social support satisfaction) were reported. Prado et al. (40) also used the short form scale with HIV+ African American women in South Florida; however, the authors reported a single social support construct in contrast to a two-factor structure. Reliability of the scale was 0.84 (40).
Unsupportive Social Support Inventory
While most of the social support scales reviewed measured the presence of positive social support, one scale assessed the presence of perceived unsupportive behaviors among people living with HIV. Ingram et al. (57) developed the Unsupportive Social Support Inventory to assess the interpersonal interactions between the subject of a stressful life event and those in their social network responding to the stressful circumstances (57). Ingram et al. (9) then tested this scale for individuals with HIV specifically to reflect on the unsupportive or upsetting responses that a person with HIV receives from others in their network. The study also examined construct validity using correlations between perception and receipt of unsupportive behaviors and depression existed among adults living with HIV. The unsupportive behaviors subscales (e.g., insensitivity, disconnecting, blaming) were positively correlated with depression (r= 0.70 – 0.76). Ingram et al. (9) developed a 24-item scale that produced a four-factor solution. The four factors were forced optimism, insensitivity, disconnecting, and blaming, with scale alpha of 0.88. Participants responded to each item by indicating how much of each type of behavior they received, and response categories ranged from 0 (“none”) to 4 (“a lot”) (9). Hutton et al. (58) also used the Unsupportive Social Support Inventory in a population of patients living with HIV in Australia and reported a Cronbach’s alpha of 0.95 (58); however, Hutton et al. did not report validation.
Cultural Adaptation of Social Support Scales
Several of the included studies utilized a translated and/or culturally adapted version of a social support scale and provided details about the adaptation process. As mentioned above, Saddki et al. (44) adapted the Medical Outcomes Social Support Survey for use among people living with HIV in Malaysia. The research team enlisted two translators to independently translate the original English-language scale into Malay; these two translations were then critiqued by a team of researchers, translators, and health professionals. The preliminary Malay version was then independently back translated into English by the same two bilingual speakers. The Malay version was subsequently assessed for content validity. Semantic equivalence, idiomatic equivalence, experiential equivalence, and conceptual equivalence between the Malay version and the original English version were confirmed. Following this preliminary adaptation, the Malay version was tested on a convenience sample of 30 patients living with HIV, and patient feedback was collected to ensure that the survey was easy to understand. Cronbach’s alpha was also calculated and reported to be 0.70 or above for each subscale. Following this translation and preliminary testing procedure, the final scale was used in the main study (44).
A similar process of back translation was used by Bastardo et al. (14) to produce a Spanish version of the Interpersonal Support Evaluation List to be implemented in Venezuela. A Venezuelan individual initially translated the original English scale into Spanish, while attempting to preserve the meaning and wording of the scale. This Spanish version was then independently back translated into English by three bilingual individuals, two of whom were Venezuelan. Discrepancies were resolved by the research team, and the final scale was then tested in the study population. Cronbach’s alpha was 0.85, and no ceiling or floor effects of the Spanish scale were reported by the research team (14).
Reliability-only studies
Beyond the 17 studies previously reported, we identified a total of 37 unique social support scales, across 58 studies, used in HIV infected or-affected populations. These scales were developed and validated in other populations; however, in these 58 studies only alpha values were reported in HIV-infected or HIV-affected populations. For these studies, we extracted the name of the scale, alpha value, and the population examined in the study to take note of the range of populations in which each measure was used. The most often used measures were the Interpersonal Relationships Inventory Scale (3), UCLA Social Support Inventory (3), Multidimensional Scale of Perceived Social Support (4), Social Provisions Scale (4), Medical Outcomes Social Support Survey (5), and the Social Support Questionnaire (6). Approximately 64% of reliability-only studies were conducted in the United States. For those that took place outside of the United States, they were conducted in North America, sub-Saharan Africa, East Asia, Southeast Asia, Europe, and the Middle East. Studies are listed in Table IV.
DISCUSSION
The current review found 19 social support scales that met the inclusion criteria, primarily that they were validated in HIV-infected or affected populations. Although they met the standards for inclusion, the majority underwent limited or minimal psychometric testing. This review did not analyze the quality of the psychometric testing, but instead focused on identifying and describing the studies that did conduct psychometric testing
A growing body of research has highlighted social support as a key protective factor for the prevention and management of HIV/AIDS (14-16, 24). However, as social support is a theoretical construct that is not directly observable, our understanding of its effects is only as strong as the scales used to assess it. Without a collective knowledge of the psychometric functioning of these scales among HIV-affected populations, the mechanisms underlying these critical findings remain unclear. Social support measures differ by the content and format of their items as well as the dimensions they aim to capture (27). Moreover, broad conceptualizations of social support as a construct differ by the various behavioral, psychological, and interpersonal aims, as well as the research questions investigators seek to address. Many of the studies of the impact of social support on outcomes systematically reviewed by Qiao et al. (27) garnered empirical evidence for the protective associations of social support; however, this evidence was inconsistent across key at-risk populations (i.e., drug users, MSM, adolescents). As such, the authors suggested social support as a protective factor for HIV/AIDS may in part be attributable to these measurement differences. Therefore, the systematic review in the manuscript herein sought to not only identify and describe available scales of social support for studying HIV-infected and affected adults (see Table II), but also to report their psychometric properties and specify the various dimensions represented by these scales (see Table III).
Table II.
Characteristics of 17 studies included in the review of validated social support instruments use among HIV-affected populations
| First Author |
Study Sampling Method |
Study Population (N) |
Age Mean (SD) | % Men | %HIV+ |
Description of Population |
Geographic Location(s) |
Recruitment Location |
|---|---|---|---|---|---|---|---|---|
| Bastardo, 2000 | Nonrandom Sample | 118 | 36 (10.6) | 87.3 | 100 | HIV+ Venezuelan adults | Caracas, Venezuela | Community support groups & clinics |
| Cortes, 2014 | Nonrandom Sample | 406 | Chile: 30.5 (5.0) UK: 23.4 (4.3) |
Chile: 0 UK: 38.3 |
15.3 | HIV+ and HIV− adults | Chile & United Kingdom | Volunteers at university clinics |
| Darbes, 2005 | Random Sample | 120 (60-dyads) | 37 (NR) | 100 | NR | Gay couples over the age of 18 | United States | Gay men's community and university organizations; ads and announcements in gay and AIDS social service organizations |
| Dima, 2014 | Nonrandom Sample | 158 | 43.8 (10.3) | 30.4 | 100 | HIV+ Tanzanian adults | Tanzania | Rural anti-retroviral therapy clinics in the Kilimanjaro region |
| Epino, 2012 | Random Sample | 610 | 38 (10) | 38 | 100 | HIV+ Rwandan adults | Rwanda | Clinics serving HIV+ adults |
| Hudson, 2001 | Nonrandom Sample | 104 | 38.3 (7.8) | 0 | 100 | HIV+ women | Bay Area, California | Residential group home for seropositive women |
| Ingram, 1999 | Nonrandom Sample | 271 | 36.5 (8) | 75 | 100 | HIV+ adults | Columbus, OH; Richmond, VA |
Ohio State & Virginia Commonwealth Universities infectious disease clinics |
| Kim, 2017 | Nonrandom Sample | 411 | 4.9 (NR) | 62.3 | 100 | HIV+, recently incarcerated adults | Chicago, IL; Cleveland, OH; Columbia, SC; New Haven, CT; Philadelphia, PA |
Prison programs |
| Prado, 2004 | Random Sample | 252 | 35.3 (8.5) | 0 | 100 | HIV+ African American mothers | South Florida, USA | Urban, low-income HIV-seropositive African American mothers |
| Renwick, 1999 | Nonrandom Sample | 120 | 36.9 (8.1) | 89.2 | 100 | HIV+ adults | Toronto, Canada | Hospital and community clinics treating adults with HIV |
| Robbins, 2003 | Nonrandom Sample | 38 | 26.9 (5.6) | 0 | 100 | HIV+ African American women | Southeastern, USA | NR |
| Saddiki, 2017 | Random Sample | 120 | NR | 62.5 | 100 | HIV+ Malaysian adults | Kelantan, Malaysia | Infectious disease unit |
| Saracino, 2015 | Nonrandom Sample | 1615 | 57.5 (15) | 61.7 | 28.2 | Patients with advance chronic conditions, including HIV | New York, New York | Palliative care hospital & tertiary care center |
| Schwarzer, 1994 | Nonrandom Sample | 587 | 36.8 (6.8) | 100 | Wave 1:44 Wave 2:46 |
Cohort of gay and bisexual men participating in the MACS study | Los Angeles, CA | MACS Study Site |
| Varzan, 2012 | Random Sample | 62 | 35.5 (n/r) | 64.5 | 8 | Injection drug users | New York, New York | Centers providing services for injection drug users |
| Waddell, 2006 | Random Sample | 459 | NR | 60 | 100 | Community health advisory and information network participants | New York, New York | Sampled from NYC Health and Social Services departments that had HIV caseloads |
| Yu, 2015 | Nonrandom Sample | 200 | NR | 81 | 100 | HIV+ Chinese adults | Beijing, China | Ditan hospital, treatment center for infectious diseases in China |
Notes: NR = not reported
Our research team identified a relatively large number of studies (N=56) that used 37 unique social support scales, yet the psychometric information many of them reported was restricted to internal consistency reliability findings. Despite its importance, such findings only tell us how internally consistent a set of items is – not whether the scale is accurately assessing the underlying theoretical construct it was purported to measure (33).
While internal consistency reliability was prominently reported, test-retest was not. Four of the 19 scales were evaluated for test-retest reliability. In general, understanding how a scale performs over time is desirable; however, test-retest may not be the most desirable reliability indicator when accounting for the evolution of individuals’ HIV management and reactions of themselves and others (4). In other words, test-retest reliability is a measure of a scales consistency; however, social support might be expected to change over time, thereby nullifying this type of reliability testing.
This review revealed that reliable and valid social support scales have largely been used with HIV-positive and at-risk adult populations in historically and emerging high HIV prevalence regions throughout the United States (59). Missing are studies assessing social support in other high prevalence locations, particularly in Sub-Saharan Africa where more than half of all people living with HIV reside (60). Other than the study conducted by Epino et al. (43), this review revealed a dearth of studies implementing reliable and valid social support scales with populations living with or at risk of HIV in this densely affected location.
We advise researchers to take care, however, when considering which social support measure to select for their unique study populations. First, nearly all studies in this review employed nonprobability sampling. Though convenience sampling or purposive sampling is often utilized when resources are limited and is an efficient way to identify the hardly reached populations who engage in high risk behavior, nonprobability sampling inherently limits studies’ external generalizability and potentially threaten internal validity for estimates of the target population (61). Second, most studies in this review adapted existing scales for use with new populations, rather than developing their own. While this is useful, it is also important to note that scales developed for use in one population may not be effective for measuring social support in another population. To illustrate, the Medical Outcomes Study (MOS) – Social Support Survey is well validated and its various modified or adapted versions have demonstrated good psychometric functioning in U.S. and international populations. However, Kim et al. (41) noted its limitations with regard to capturing incarcerated populations’ range of experiences of social support. Thus, we encourage researchers wishing to implement a previously validated scale in broader populations conduct additional psychometric tests with their unique populations of interest.
Researchers should also consider the implications for their study objectives when selecting a scale to measure social support. Though emotional support, tangible support and satisfaction with support are the dimensions that have most often been assessed, researchers have identified and assessed a wide variety of social support dimensions which researchers may find more applicable to meeting their study objectives (see Table 2). For example, although most studies in this review assessed social support by measuring its presence—a natural fit for researching its protective associations – some researchers may be interested in examining the negative stressors and experiences potentially driven by unsupportive behaviors. If this is the case, they may be best served by the Unsupportive Social Support Inventory used by Ingram et al. (9) with HIV positive individuals in the US.
There are several limitations with this review. First, we only included studies that were written in English, which could have failed to identify additional scale development and or adaptation studies published in other languages. This may have also contributed to the fact that the majority of the studies we identified were conducted in western countries. Second, we only included studies conducted with adult populations; however, this was a decision based on empirical evidence that social support among adolescent populations is fundamentally different than that among adult populations (62). Separate reviews should be conducted to assess the use of social support scales with adolescents and children who are living with or at risk of HIV. Finally, many of the studies evaluated were cross-sectional and did not provide estimated effect sizes, thereby limiting our ability to assess the quality of studies and overall risk of bias assessment.
Despite these limitations, this study also has a number of strengths. This systematic review followed the PRISMA guidelines, with research assistants working in tandem with university librarians to identify a universe of possible inclusion studies. Second, trained research assistants worked collaboratively to ensure all studies were critiqued by two separate individuals to maintain fidelity. And finally, the study team leveraged the unique expertise of members of the HIV and social and behavioral science team. Collectively, these efforts enhance credibility of the study findings.
CONCLUSIONS AND FUTURE RESEARCH
We have synthesized a number of reliable and valid scales for use by HIV researchers with diverse adult populations living with and affected by HIV. While the existence of scales that tap into a variety of social support dimensions is a positive feature of this literature, the limited degree of overlap of scales used across studies make cross-study comparisons difficult to draw. Researchers should critically assess whether existing social support scales are appropriate for their study samples. Where necessary, existing scales should be adapted and validity-tested or new valid scales developed. Finally, to augment our understanding of social support as it relates to HIV/AIDS, researchers should report clearly the psychometric properties of both reliability and validity whenever possible.
Future studies should consider assessing a broader range of validity attributes. Conducting a variety of validity assessments is critical to strengthen the evidence of the performance of a scale (33). Researchers should consider assessing valid and reliable social support measures in more global contexts, particularly those with high HIV prevalence estimates. Studies validating such measures in these regions are sorely needed.
Acknowledgements:
We thank Angela Bardeen, University of North Carolina at Chapel Hill librarian for her guidance in the development of the systematic review. We also thank Camille McGirt, MPH, and Catherine Grodensky, MPH for their assistance in the conceptualization and review of the articles.
Funding: This study was funded by the National Institute of Allergy and Infectious Disease (P30-AI50410). Ms. Wallace was supported by a National Research Service Award Predoctoral Traineeship from AHRQ (T32-HS000032).
Footnotes
Conflict of Interest: Deshira D. Wallace declares that she has no conflict of interest. Allison Pack declares that she has no conflict of interest. Breana Uhrig Castonguay declares that she has no conflict of interest. J.L. Stewart declares that she has no conflict of interest. Christine Schalkoff declares that she has no conflict of interest. Sruthi Cherkur declares that she has no conflict of interest. Margot Schein declares that she has no conflict of interest. Matthew Go declares that he has no conflict of interest. Jackson Devadas declares that he has no conflict of interest. Edwin B. Fisher declares that he has no conflict of interest. Carol E. Golin declares that she has no conflict of interest.
Ethical approval: This article does not contain any studies with human participants performed by any of the authors.
REFERENCES
- 1.Uchino BN, Bowen K, Carlisle M, Birmingham W. Psychological pathways linking social support to health outcomes: A visit with the “ghosts” of research past, present, and future. Social Science & Medicine. 2012;74:949–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cassel J The contribution of the social environment to host resistance, the Fourth Wade Hampton Frost Lecture. American Journal of Epidemiology. 1976;104:107–23. [DOI] [PubMed] [Google Scholar]
- 3.Moritsugu J, Vera E, Wong FY, Duffy KG. Community psychology: Psychology Press; 2015 2015. [Google Scholar]
- 4.Uchino BN. Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspectives on Psychological Science. 2009;4:236–55. [DOI] [PubMed] [Google Scholar]
- 5.Cohen S, Syme SL. Social support and health.: Academic Press; 1985 1985. [Google Scholar]
- 6.Canty-Mitchell J, Zimet GD. Psychometric properties of the Multidimensional Scale of Perceived Social Support in urban adolescents. American Journal of Community Psychology. 2000;28:391–400. [DOI] [PubMed] [Google Scholar]
- 7.Wandersman L, Wandersman A, Kahn S. Social support in the transition to parenthood. Journal of Community Psychology. 1980;8:332–42. [Google Scholar]
- 8.Waddell EN, Messeri PA. Social support, disclosure, and use of antiretroviral therapy. AIDS and Behavior. 2006;10:263–72. [DOI] [PubMed] [Google Scholar]
- 9.Ingram KM, Jones DA, Fass RJ, Neidig JL, Song YS. Social support and unsupportive social interactions: Their association with depression among people living with HIV. AIDS Care. 1999;11:313–29. [DOI] [PubMed] [Google Scholar]
- 10.Russell D, Cutrona CE. Development and evolution of the UCLA Loneliness Scale Unpublished manuscript, Center for Health Services Research, College of Medicine, University of Iowa; 1988. [Google Scholar]
- 11.Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29:377–87. [DOI] [PubMed] [Google Scholar]
- 12.Robbins M, Szapocznik J, Tejeda M, Samuels D, Ironson G, Antoni M. The protective role of the family and social support network in a sample of HIV-positive African American women: Results of a pilot study. Journal of Black Psychology. 2003;29:17–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer social support is associated with recent HIV testing among young black men who have sex with men. AIDS and Behavior. 2014;18:913–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bastardo Y, Kimberlin C. Relationship between quality of life, social support and disease-related factors in HIV-infected persons in Venezuela. AIDS Care. 2000;12:673–84. [DOI] [PubMed] [Google Scholar]
- 15.Pakenham KI, Dadds MR, Terry DJ. Relationship between adjustment to HIV and both social support and coping. Journal of Consulting and Clinical Psychology. 1994;62:1194. [DOI] [PubMed] [Google Scholar]
- 16.Vandehey MA, Shuff IM, Diekhoff GM. Stage of HIV-Infection and social support networks: Gay and bisexual men's embeddedness, with family, friends, and partners. Journal of HIV/AIDS & Social Services. 2004;2:21–40. [Google Scholar]
- 17.Lackner JB, Joseph JG, Ostrow DG, Eshleman S. The effects of social support on Hopkins Symptom Checklist-assessed depression and distress in a cohort of human immunodeficiency virus-positive and-negative gay men: A longitudinal study at six time points. The Journal of Nervous and Mental Disease. 1993;181:632–8. [DOI] [PubMed] [Google Scholar]
- 18.Stowe A, Ross MW, Wodak A, Thomas GV, Larson SA. Significant relationships and social supports of injecting drug users and their implications for HIV/AIDS services. AIDS Care. 1993;5:23–33. [DOI] [PubMed] [Google Scholar]
- 19.Leserman J, Petitto JM, Golden RN, Gaynes BN, Gu H, Perkins DO, et al. Impact of stressful life events, depression, social support, coping, and cortisol on progression to AIDS. American Journal of Psychiatry. 2000;157:1221–8. [DOI] [PubMed] [Google Scholar]
- 20.Vyavaharkar M, Moneyham L, Tavakoli A, Phillips KD, Murdaugh C, Jackson K, et al. Social support, coping, and medication adherence among HIV-positive women with depression living in rural areas of the southeastern United States. AIDS Patient Care and STDs. 2007;21:667–80. [DOI] [PubMed] [Google Scholar]
- 21.Iob E, Kirschbaum C, Steptoe A. Positive and negative social support and HPA-axis hyperactivity: Evidence from glucocorticoids in human hair. Psychoneuroendocrinology. 2018;96:100–8. [DOI] [PubMed] [Google Scholar]
- 22.Lincoln KD. Social support, negative social interactions, and psychological well-being. Social Service Review. 2000;74(2):231–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell MM, Maragh-Bass AC, Nguyen TQ, Isenberg S. The role of chronic pain and current substance use in predicting negative social support among disadvantaged persons living with HIV/AIDS. AIDS Care. 2016;28(10):1280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kapadia F, Siconolfi D, Barton S, Olivieri B, Lombardo L, Halkitis P. Social support network characteristics and sexual risk taking among a racially/ethnically diverse sample of young, urban men who have sex with men. AIDS and Behavior. 2013;17:1819–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC. HIV among African American gay and bisexual men. Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 26.Vazan P, Mateu-Gelabert P, Cleland CM, Sandoval M, Friedman SR. Correlates of staying safe behaviors among long-term injection drug users: psychometric evaluation of the staying safe questionnaire. AIDS and Behavior. 2012;16:1472–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qiao S, Li X, Stanton B. Social support and HIV-related risk behaviors: A systematic review of the global literature. AIDS and Behavior. 2014;18:419–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Brien K, Wortman CB, Kessler RC, Joseph JG. Social relationships of men at risk for AIDS. Social Science & Medicine. 1993;36:1161–7. [DOI] [PubMed] [Google Scholar]
- 29.Kalichman SC, DiMarco M, Austin J, Luke W, DiFonzo K. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine. 2003;26:315–32. [DOI] [PubMed] [Google Scholar]
- 30.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bearman KJ, La Greca AM. Assessing friend support of adolescents' diabetes care: the diabetes social support questionnaire-friends version. Journal of Pediatric Psychology. 2002;27:417–28. [DOI] [PubMed] [Google Scholar]
- 32.Lohr KN. Assessing health status and quality-of-life instruments: attributes and review criteria. Quality of Life Research. 2002;11:193–205. [DOI] [PubMed] [Google Scholar]
- 33.DeVellis RF. Scale development: Theory and applications: Sage publications; 2016 2016. [Google Scholar]
- 34.Cortes A, Hunt N, McHale S. Development of the scale of perceived social support in HIV (PSS-HIV). AIDS and Behavior. 2014;18:2274–84. [DOI] [PubMed] [Google Scholar]
- 35.Darbes LA, Lewis MA. HIV-specific social support predicts less sexual risk behavior in gay male couples. Health Psychology. 2005;24:617. [DOI] [PubMed] [Google Scholar]
- 36.Renwick R, Halpen T, Rudman D, Friedland J. Description and validation of a measure of received support specific to HIV. Psychological Reports. 1999;84:663–73. [DOI] [PubMed] [Google Scholar]
- 37.Hudson AL, Lee KA, Miramontes H, Portillo CJ. Social interactions, perceived support, and level of distress in HIV-positive women. Journal of the Association of Nurses in AIDS Care. 2001;12:68–76. [DOI] [PubMed] [Google Scholar]
- 38.Schwarzer R, Dunkel-Schetter C, Kemeny M. The multidimensional nature of received social support in gay men at risk of HIV infection and AIDS. American Journal of Community Psychology. 1994;22:319–39. [DOI] [PubMed] [Google Scholar]
- 39.Saracino R, Kolva E, Rosenfeld B, Breitbart W. Measuring social support in patients with advanced medical illnesses: An analysis of the Duke-UNC Functional Social Support Questionnaire. Palliative & Supportive Care. 2015;13:1153–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Prado G, Feaster DJ, Schwartz SJ, Pratt IA, Smith L, Szapocznik J. Religious involvement, coping, social support, and psychological distress in HIV-seropositive African American mothers. AIDS and Behavior. 2004;8:221–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim S, Ouellet LJ, Mazza J, Spaulding AC. Rasch Analysis and Differential Item Functioning of a Social Support Measure in Jail Inmates With HIV Infection. Evaluation & The Health Professions. 2017;40:33–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dima AL, Stutterheim SE, Lyimo R, de Bruin M. Advancing methodology in the study of HIV status disclosure: The importance of considering disclosure target and intent. Social Science & Medicine. 2014;108:166–74. [DOI] [PubMed] [Google Scholar]
- 43.Epino HM, Rich ML, Kaigamba F, Hakizamungu M, Socci AR, Bagiruwigize E, et al. Reliability and construct validity of three health-related self-report scales in HIV-positive adults in rural Rwanda. AIDS Care. 2012;24:1576–83. [DOI] [PubMed] [Google Scholar]
- 44.Saddki N, Sulaiman Z, Abdullah S, Zakaria N, Mohamad N, Ab Razak A, et al. Psychometric properties of the Malay version of the Medical Outcomes Study Social Support Survey (MOS-SSS) in a sample of patients with HIV. Journal of HIV/AIDS & Social Services. 2017;16:60–74. [Google Scholar]
- 45.Yu Y, Yang JP, Shiu C-S, Simoni JM, Xiao S, Chen W-t, et al. Psychometric testing of the Chinese version of the Medical Outcomes Study Social Support Survey among people living with HIV/AIDS in China. Applied Nursing Research. 2015;28:328–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nunnally J, Bernstein I. Psychometric theory. 3rd ed. New York: Mc-Graw-Hill; 1994 1994. [Google Scholar]
- 47.Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine. 1991;32:705–14. [DOI] [PubMed] [Google Scholar]
- 48.Beaulieu M, Otis J, Blais M, Godin G, Cox JJ, Côté J, et al. A model of quality of life of women living with HIV. Journal of HIV/AIDS & Social Services. 2012;11:210–32. [Google Scholar]
- 49.Watt MH, Maman S, Golin CE, Earp JA, Eng E, Bangdiwala SI, et al. Factors associated with self-reported adherence to antiretroviral therapy in a Tanzanian setting. AIDS Care. 2010;22:381–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hinnen C, Schreuder I, Jong E, van Duijn M, Dahmen R, van Gorp EC. The contribution of adult attachment and perceived social support to depressive symptoms in patients with HIV. AIDS Care. 2012;24:1535–42. [DOI] [PubMed] [Google Scholar]
- 51.Meade CS, Sikkema KJ. Voluntary HIV testing among adults with severe mental illness: frequency and associated factors. AIDS and Behavior. 2005;9:465–73. [DOI] [PubMed] [Google Scholar]
- 52.McInerney PA, Ncama BP, Wantland D, Bhengu BR, McGibbon C, Davis SM, et al. Quality of life and physical functioning in HIV-infected individuals receiving antiretroviral therapy in KwaZulu-Natal, South Africa. Nursing & Health Sciences. 2008;10:266–72. [DOI] [PubMed] [Google Scholar]
- 53.Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: the social support questionnaire. Journal of Personality and Social Psychology. 1983;44:127. [Google Scholar]
- 54.Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: Practical and theoretical implications. Journal of Social and Personal Relationships. 1987;4:497–510. [Google Scholar]
- 55.Hart TA, Heimberg RG. Social anxiety as a risk factor for unprotected intercourse among gay and bisexual male youth. AIDS and Behavior. 2005;9:505–12. [DOI] [PubMed] [Google Scholar]
- 56.Wyatt AS. Prediction of hopelessness among HIV positive mothers: Evidence for the social support buffering and diathesis-stress models: The Chicago Medical School; 1997. [Google Scholar]
- 57.Ingram KM, Betz NE, Mindes EJ, Schmitt MM, Smith NG. Unsupportive responses from others concerning a stressful life event: Development of the Unsupportive Social Interactions Inventory. Journal of Social and Clinical Psychology. 2001;20:173–207. [Google Scholar]
- 58.Hutton VE. Companion animals and wellbeing when living with HIV in Australia. Anthrozoos. 2014;27:407–21. [Google Scholar]
- 59.CDC. HIV surveillance report, 2013. Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 60.UNAIDS. Global AIDS update 2016. United Nations Program on HIV/AIDS; 2016. 2016. [Google Scholar]
- 61.Watters JK, Biernacki P. Targeted sampling: options for the study of hidden populations. Social Problems. 1989;36:416–30. [Google Scholar]
- 62.Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. The Lancet. 2012;379:1641–52. [DOI] [PubMed] [Google Scholar]
- 63.Luszczynska A, Sarkar Y, Knoll N. Received social support, self-efficacy, and finding benefits in disease as predictors of physical functioning and adherence to antiretroviral therapy. Patient Education and Counseling. 2007;66:37–42. [DOI] [PubMed] [Google Scholar]
- 64.Rzeszutek M, Oniszczenko W, Żebrowska M, Firląg-Burkacka E. HIV infection duration, social support and the level of trauma symptoms in a sample of HIV-positive Polish individuals. AIDS Care. 2015;27:363–9. [DOI] [PubMed] [Google Scholar]
- 65.Schulz U, Schwarzer R. Long-term effects of spousal support on coping with cancer after surgery. Journal of Social and Clinical Psychology. 2004;23:716–32. [Google Scholar]
- 66.Hong Y, Fang X, Li X, Liu Y, Li M. Environmental support and HIV prevention behaviors among female sex workers in China. Sexually Transmitted Diseases. 2008;35:662–7. [DOI] [PubMed] [Google Scholar]
- 67.Qiao S, Li X, Zhou Y, Shen Z, Tang Z. AIDS impact special issue 2015: interpersonal factors associated with HIV partner disclosure among HIV-infected people in China. AIDS Care. 2016;28:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Siegel K, Raveis VH, Karus D. Psychological well-being of gay men with AIDS: Contribution of positve and negative illness-related network interactions to depressive mood. Social Science & Medicine. 1994;39:1555–63. [DOI] [PubMed] [Google Scholar]
- 69.Tate DC, Berg JJVD, Hansen NB, Kochman A, Sikkema KJ. Race, Social Support, and Coping Strategies among HIV-Positive Gay and Bisexual Men. Culture, Health & Sexuality. 2006;8:235–49. [DOI] [PubMed] [Google Scholar]
- 70.Gray JR, Beard MT. Uncertainty and spirituality in women with HIV/AIDS. Journal of Theory Construction & Testing. 1999;3:55. [Google Scholar]
- 71.Gray J Racial/ethnic differences in psychosocial factors among persons living with HIV/AIDS. Journal of Multicultural Nursing & Health. 2002;8:50. [Google Scholar]
- 72.Shannon M, Lee KA. HIV-infected mothers’ perceptions of uncertainty, stress, depression and social support during HIV viral testing of their infants. Archives of Women's Mental Health. 2008;11:259. [DOI] [PubMed] [Google Scholar]
- 73.Burrage J, Demi A. Buddy Programs for People Infected With HIV. Journal of the Association of Nurses in AIDS Care. 2003;14:52–62. [DOI] [PubMed] [Google Scholar]
- 74.Emlet CA. A comparison of HIV stigma and disclosure patterns between older and younger adults living with HIV/AIDS. AIDS Patient Care & STDs. 2006;20:350–8. [DOI] [PubMed] [Google Scholar]
- 75.Goodman ML, Serag H, Gitari S, Keiser PH, Dacso M, Raimer BG. Exploring Pathways Between HIV+ Status and Excellent Overall Health Among Kenyan Women: Family Functioning, Meaningfulness of Life, Seroconcordance, Social Support and Considering the Need for Integrated Care. Journal of Community Health. 2016;41:989–97. [DOI] [PubMed] [Google Scholar]
- 76.Li L, Lee S-J, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21:1007–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nyamathi A, Flaskerud J, Leake B, Chen S. Impoverished women at risk for AIDS: Social support variables. Journal of psychosocial nursing and mental health services. 1996;34:31–9. [DOI] [PubMed] [Google Scholar]
- 78.Sajjadi M, Rassouli M, Bahri N, Mohammadipoor F. The correlation between perceived social support and illness uncertainty in people with human immunodeficiency virus/acquired immune deficiency syndrome in Iran. Indian Journal of Palliative Care. 2015;21:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Clingerman EM. Participation in physical activity by persons living with HIV disease. Journal of the Association of Nurses in AIDS Care. 2003;14:59–70. [DOI] [PubMed] [Google Scholar]
- 80.Kipp AM, Audet CM, Earnshaw VA, Owens J, McGowan CC, Wallston KA. Re-validation of the Van Rie HIV/AIDS-related stigma scale for use with people living with HIV in the United States. PloS One. 2015;10:e0118836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rodgers AY. The relationship between changes in social social support and adjustment to AIDS in gay males. Social Work in Health Care. 1995;20:37–49. [DOI] [PubMed] [Google Scholar]
- 82.Serovich JM, Kimberly J, Mosack K, Lewis T. The role of family and friend social support in reducing emotional distress among HIV-positive women. AIDS Care. 2001;13:335–41. [DOI] [PubMed] [Google Scholar]
- 83.Chibnall JT, Videen SD, Duckro PN, Miller DK. Psychosocial— spiritual correlates of death distress in patients with life-threatening medical conditions. Palliative Medicine. 2002;16:331–8. [DOI] [PubMed] [Google Scholar]
- 84.Su X, Lau JTf, Mak WWs, Chen L, Choi KC, Song J, et al. Perceived discrimination, social support, and perceived stress among people living with HIV/AIDS in China. AIDS Care. 2013;25:239–48. [DOI] [PubMed] [Google Scholar]
- 85.Fleishman JA, Fogel B. Coping and depressive symptoms among young people with AIDS. Health Psychology. 1994;13:156–69. [DOI] [PubMed] [Google Scholar]
- 86.Chen ML, Deng SL, Chang HK. A comparison of the health locus of control and perceived social support between cancer and AIDS patients. Scandinavian Journal of Caring Sciences. 2001;15:92–8. [Google Scholar]
- 87.Tangkawanich T, Yunibhand J, Thanasilp S, Magilvy K. Causal model of health: Health-related quality of life in people living with HIV/AIDS in the northern region of Thailand. Nursing & Health Sciences. 2008;10:216–21. [DOI] [PubMed] [Google Scholar]
- 88.Heckman TG, Somlai AM, Sikkema KJ, Kelly JA, Franzoi SL. Psychosocial predictors of life satisfaction among persons living with HIV infection and AIDS. Journal of the Association of Nurses in AIDS Care. 1997;8:21–30. [DOI] [PubMed] [Google Scholar]
- 89.Kyle RD, Sachs LG. Perceptions of control and social support in relation to psychosocial adjustment to HIV/AIDS. AIDS Patient Care. 1994;8:322–7. [Google Scholar]
- 90.Shah K, McMahon JM, Trabold N, Aidala AA, Chen M, Pouget ER, et al. Determinants of physical and global functioning in adult HIV-positive heterosexual men. AIDS Care. 2015;27:1079–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Diaz RM, Ayala G, Bein E, Henne J, Marin BV. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: findings from 3 US cities. American Journal of Public Health. 2001;91:927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Organista KC, Kubo A. Pilot survey of HIV risk and contextual problems and issues in Mexican/Latino migrant day laborers. Journal of Immigrant and Minority Health. 2005;7:269–81. [DOI] [PubMed] [Google Scholar]
- 93.Blaney NT, Goodkin K, Feaster D, Morgan R, Millon C, Szapocznik J, et al. A psychosocial model of distress over time in early HIV-1 infection: The role of life stressors, social support and coping. Psychology & Health. 1997;12:633–53. [Google Scholar]
- 94.Murphy DA, Lu MC, Martin D, Hoffman D, Marelich WD. Results of a pilot intervention trial to improve antiretroviral adherence among HIV-positive patients. Journal of the Association of Nurses in AIDS Care. 2002;13:57–69. [DOI] [PubMed] [Google Scholar]
- 95.Toth M, Messer LC, Quinlivan EB. Barriers to HIV care for women of color living in the Southeastern US are associated with physical symptoms, social environment, and self-determination. AIDS Patient Care & STDs. 2013;27:613–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rongkavilit C, Wright K, Chen X, Naar-King S, Chuenyam T, Phanuphak P. HIV stigma, disclosure and psychosocial distress among Thai youth living with HIV. International Journal of STD & AIDS. 2010;21:126–32. [DOI] [PubMed] [Google Scholar]
- 97.Persons E, Kershaw T, Sikkema KJ, Hansen NB. The impact of shame on health-related quality of life among HIV-positive adults with a history of childhood sexual abuse. AIDS Patient Care & STDs. 2010;24:571–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Turner-Cobb JM, Gore-Felton C, Marouf F, Koopman C, Kim P, Israelski D, et al. Coping, social support, and attachment style as psychosocial correlates of adjustment in men and women with HIV/AIDS. Journal of Behavioral Medicine. 2002;25:337–53. [DOI] [PubMed] [Google Scholar]
- 99.Pinto RM, McKay MM. Do age and gender of social supports matter for low-income African-American women attending an HIV prevention program? Journal of HIV/AIDS & Social Services. 2005;3:5–25. [Google Scholar]
- 100.John T, Ndebbio M. Perceived psychosocial needs, social support, quality of life and adjustment in subjects with HIV/AIDS. Africa Journal of Nursing and Midwifery. 2002;4:59–62. [Google Scholar]
- 101.Sethosa E, Peltzer K. Evaluation of HIV counselling and testing, self-disclosure, social support and sexual behaviour change among a rural sample of HIV reactive patients in South Africa. Curationis. 2005;28:29–41. [DOI] [PubMed] [Google Scholar]
- 102.Prado G, Szapocznik J, Mitrani VB, Mauer MH, Smith L, Feaster DJ. Factors influencing engagement into interventions for adaptation to HIV in African American women. AIDS and Behavior. 2002;6:141–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ma W, Kang D, Song Y, Wei C, Marley G, Ma W. Social support and HIV/STDs infections among a probability-based sample of rural married migrant women in Shandong Province, China. BMC Public Health. 2015;15:1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gore-Felton C, Koopman C, Turner-Cobb J, Durán R, Israelski D, Spiegel D. The influence of social support, coping and mood on sexual risk behavior among HIV-positive men and women. Journal of Health Psychology. 2002;7:713–22. [DOI] [PubMed] [Google Scholar]
- 105.Gore-Felton C, Power R, Duran R, Sarlati S, Palmer L, Koopman C, et al. Psychosocial factors associated with disclosure of HIV positive serostatus: Understanding the influence of depression and social support. Journal of HIV/AIDS & Social Services. 2008;7:83–98. [Google Scholar]
- 106.Simoni JM, Demas P, Mason HR, Drossman JA, Davis ML. HIV disclosure among women of African descent: Associations with coping, social support, and psychological adaptation. AIDS and Behavior. 2000;4:147–58. [Google Scholar]
- 107.Simoni JM, Frick PA, Huang B. A longitudinal evaluation of a social support model of medication adherence among HIV-positive men and women osn antiretroviral therapy. Health Psychology. 2006;25:74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]