Abstract
Symptomatic individuals suspected of having myocardial ischemia often have no obstructive atherosclerotic narrowing of epicardial coronary arteries. Abnormal coronary vascular reactivity, and in particular, coronary artery vasospasm (CAS), may be an explanation in a subset of these patients. Psychological factors play an important role in ischemic heart disease, but their role in CAS is not clear; autonomic dysfunction and increased inflammation are two prevailing pathophysiological mechanisms implicated in abnormal coronary reactivity resulting from mental health conditions. Interrelationships between psychological factors, abnormal coronary reactivity, and sex/gender differences are poorly defined in the etiology of CAS. In this issue of Psychosomatic Medicine, Hung et al. report a frequency of less than 0.1% of new onset CAS in the Taiwanese population, with higher occurrence in women and younger individuals. Patients with CAS had a higher prevalence of prior anxiety and depression compared to those with coronary artery disease and controls, with no sex differences. In this editorial comment, we discuss the potential reasons for underreporting of CAS and the challenges regarding the use of administrative health records for psychosomatic research. In this editorial, a model is presented to explain the association between emotional stressors and mental health factors with CAS, including the role of sympathetic nervous system activation, inflammation, oxidative stress, endothelial dysfunction, and smooth muscle cell dysregulation.
Keywords: coronary artery spasm, anxiety, depression, women, coronary artery disease
Patients with evidence of ischemia and no obstructive narrowing of the coronary arteries (INOCA) are increasingly recognized as having adverse cardiovascular morbidity and mortality, despite absence of flow-limiting epicardial stenosis and preserved ejection fraction (1). The pathophysiology of INOCA is incompletely understood, but abnormal coronary vascular reactivity has been implicated, due to epicardial and/or microvascular coronary dysfunction from endothelium dependent or independent mechanisms (2, 3). Coronary artery spasm (CAS) is part of the spectrum of abnormal vasomotion that may underlie the etiology of INOCA, but it remains under-diagnosed and under-reported, and thus its overall role in angina and myocardial ischemia remains uncertain. The Coronary Vasomotion Disorders International Study Group (COVADIS) has published diagnostic criteria for vasospastic angina, which include: (a) angina that responds to nitrates; (b) transient electrocardiogram (ECG) changes suggestive of myocardial ischemia; and (c) documented coronary artery spasm on angiography, spontaneously or with provocation testing (4). Despite this accepted definition, CAS remains a diagnostic challenge, because provocation testing is not routinely performed after the finding of unobstructive coronary artery disease (CAD) on angiography. Therefore, the true prevalence of CAS in the U.S. and other populations is unknown, although epidemiologic data suggest that there may be ethnic differences in CAS, with individuals who are Asian having a higher prevalence than individuals who are white (3). Whether there are sex differences in CAS also remains controversial (3, 5).
The exact mechanisms of CAS are unclear but appear multifactorial. Smooth muscle hyperactivity due to autonomic nervous system dysfunction with sympathetic predominance, inflammation and oxidative stress, have all been implicated (Figure). That these effects are mediated by the neuroendocrine and autonomic nervous system is suggested by emerging research linking psychological stress and myocardial ischemia to brain areas contributing to emotional regulation, autonomic outflow and vascular reactivity (6, 7). On the other hand, traditional cardiovascular risk factors have been inconsistently associated with CAS (8).
Figure.
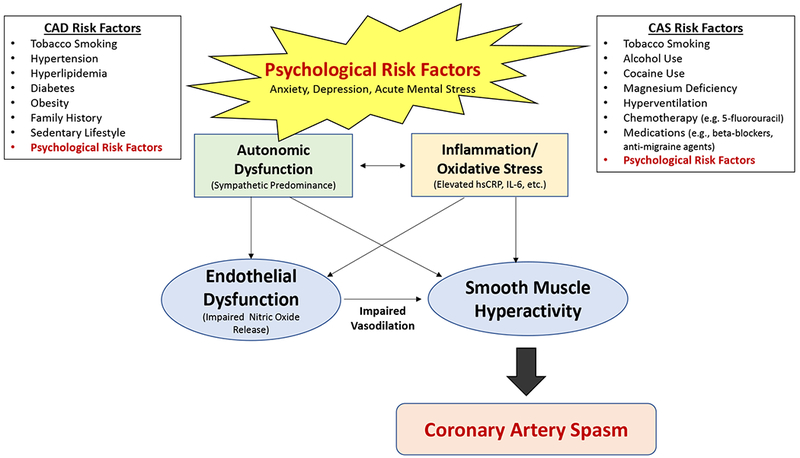
Psychological risk factors are implicated in ischemic heart disease due to atherosclerotic coronary artery disease (CAD) and coronary artery spasm (CAS). The prevailing mechanistic pathways of autonomic dysfunction with disruption of neuroendocrine axis, and inflammation/oxidative stress may lead to a state of altered smooth muscle reactivity that predisposes to CAS, irrespective of significant obstructive epicardial coronary artery disease.
Given the potential role of neurobiology, autonomic function and inflammation in CAS, it is reasonable to hypothesize that the psychosocial sphere, such as anxiety and depression, may play a role in this condition. A large body of literature implicates these psychosocial factors in the risk and outcome of cardiovascular disease, with autonomic dysfunction and inflammation as prevailing hypothesized mechanisms (9, 10). Additional studies have reported a higher prevalence of anxiety and depression in patients with INOCA compared to those with obstructive CAD (11), although a recent study found no difference in the prevalence of anxiety and depression when comparing myocardial infarction patients with and without obstructive CAD (12). Anxiety and depression are highly prevalent also in patients with chest pain, irrespective of CAD severity, and predict adverse outcomes (13, 14). In addition, mental stress can induce myocardial ischemia in susceptible patients with coronary disease (15, 16), and this phenomenon has been linked to depression (17, 18), as well as to angina in daily life (19) and microvascular reactivity, but not coronary occlusion, especially among women (20–23). Such observations suggest that emotional stressors and mental health factors may be involved in the etiology of INOCA due to CAS, possibly through sympathetic nervous system stimulation. However, little is known to date about the role of psychosocial factors in CAS.
In this issue of Psychosomatic Medicine, Hung et al. describe the association of anxiety and depression with CAS in a large retrospective cohort study based on the Taiwanese National Health Insurance Research Database (24). They used propensity score matching for the period between 2000 and 2012 to identify three groups: 10,473 patients with CAS; 10,473 patients with obstructive CAD; and 10,325 controls with no CAS and no obstructive CAD. The diagnosis of CAS was made in symptomatic patients with ECG changes whose symptoms were relieved by nitroglycerin, who were found not to have obstructive CAD on coronary angiography, and who had a positive provocative test with methylergonovine (unless there was ST-segment elevation during chest pain in the absence of obstructive CAD). Patients who had a concomitant diagnosis of obstructive CAD and CAS were excluded. A diagnosis of anxiety and depression was identified retrospectively in the preceding 3 years, and also going back to 1997.
New-onset CAS was a rare phenomenon in this Taiwanese population (<0.1%), which is much lower than previously reported in smaller studies (3). CAS was more common in women and younger individuals than new-onset obstructive CAD. When compared with the group with obstructive CAD, patients with new-onset CAS had a higher prevalence of a prior anxiety diagnosis (38.7% vs. 25.8%) and a prior depression diagnosis (2.3% vs. 1.5%), which corresponded to an adjusted odds ratio of 2.2 for the association between anxiety and CAS, and an adjusted odds ratio of 1.5 for the association between depression and CAS. When patients with new-onset CAS were compared with controls, the corresponding odds ratios were >5 for anxiety and about 2 for depression. The associations were similar in men and women.
The finding that patients with CAS were more often younger women is interesting, since this is also the group that is more likely to develop myocardial ischemia under laboratory-induced mental stress (21, 23). Furthermore, younger women more often present with myocardial infarction in the setting of nonobstructive CAD (2). However, the study by Hung et al. found no sex-differences in the association of anxiety and depression with CAS.
This study is convincing because of its large sample size, which is an advantage when studying a rare condition such as CAS. However, several limitations should be considered as well, some of which the authors have acknowledged. Misclassification, coding errors and missing values are inherent problems in research based on electronic health records. The authors used three outpatient diagnoses or one inpatient diagnosis to improve the accuracy of diagnostic classification, but substantial misclassification is likely to remain. The authors attempted to verify the CAS diagnostic code, and detailed data were required for this, including presence of chest pain with ECG changes with relief by nitroglycerin, presence and extent of obstructive CAD on coronary angiography, and results of provocative testing. These data may have been inadequately documented in the medical records, and we are not told how this information was retrieved and how complete it was. In addition, several patients may not have received the diagnosis of CAS because of incomplete testing. These issues might help explain the low frequency of CAS in this study. The diagnosis of psychiatric disorders through electronic billing codes is also likely to be misclassified or under-reported (25). Again, this may explain the low prevalence of anxiety and depression in the control group (5%-10% for anxiety and 0.6%-1% for depression, depending on the assessment time frame). The prevalence of depression was also low in the CAS and obstructive CAD groups (1%-2%). Misclassification of CAS and psychiatric diagnoses can affect study results also because of possible reverse causation, if the mental health conditions actually occurred after rather than before the onset of CAS, and were caused by CAS-related symptoms. Even though the authors attempted to obtain psychological measures before CAS, this concern remains. For example, because of the possible under-reporting or miscoding of CAS in the medical record data mentioned above, it can be difficult to establish the time of CAS onset with accuracy. Another potential problem with the use of electronic health records is the relative lack of data on potential confounding factors, such as socioeconomic and behavioral measures like education, smoking and substance abuse, as well as medication use, all factors that may affect CAS, coronary atherosclerosis or both. Under-detection of CAS and of psychological risk factors, and/or the presence of confounding factors could have resulted in either an underestimation or an overestimation of the true associations in this study, depending on the type of misclassification. If reverse causation were an issue, it would have resulted in an over-estimation of the true associations. Thus, although the authors should be commended for their detailed work in an attempt to improve accuracy of disease classifications in this large administrative database, limitations remain as for all studies that rely on electronic health record systems like this.
An additional important point to consider is that absence of obstructive CAD does not mean absence of coronary atherosclerosis. Some of the individuals in the CAS group may have had atherosclerotic plaques even if not obstructive, but information on angiographic CAD severity was not provided. The study also did not report whether CAS was focal or diffuse. These can be considered two different types of CAS, because focal spasm is more likely to occur near areas of plaque, while diffuse spasm more often is related to endothelial dysfunction (26). Finally, the definition of CAS varies among studies, with some considering a >75% vasoconstriction with provocative testing, while others considering a >90% vasoconstriction. In this study, we are not provided information related to percent vasoconstriction in those with CAS.
Does a diagnosis of anxiety and/or depression predict future CAS, and does sex/gender play a role? The study by Hung et al. brings needed attention to these issues but does not provide definite answers. The interrelationships among psychological factors and anginal chest pain, myocardial ischemia and infarction, as well as differences by sex/gender, remain poorly defined. An additional, broader question is whether electronic medical record systems are acceptable in psychosomatic research where accurate assessment of psychological/psychiatric conditions (and potential confounding factors) is paramount to valid results, since these factors ten to be incompletely documented in administrative health records. In the meantime, well-conducted studies are needed from large registries with accurate psychological or psychiatric assessments, as well as rigorous human mechanistic studies, in order to clarify if and how psychological factors contribute to CAS. Ultimately, clinical trials should address the impact of psychological treatments and other interventions on CAS-related outcomes in order to guide clinical care in this at-risk population.
Acknowledgments
Sources of funding: National Institutes of Health grants K23HL105787, R01 HL109413, R01 HL125246, R01 HL136205, and P01 HL101398.
Footnotes
Conflicts: Mehta: None; Thobani: None; Vaccarino: None
References
- 1.Bairey Merz CN, Pepine CJ, Walsh MN, Fleg JL. Ischemia and No Obstructive Coronary Artery Disease (INOCA): Developing Evidence-Based Therapies and Research Agenda for the Next Decade. Circulation. 2017;135:1075–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pasupathy S, Tavella R, Beltrame JF. The What, When, Who, Why, How and Where of Myocardial Infarction With Non-Obstructive Coronary Arteries (MINOCA). Circ J 2016;80:11–6. [DOI] [PubMed] [Google Scholar]
- 3.J. C. S. Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (Coronary Spastic Angina) (JCS 2013). Circulation journal : official journal of the Japanese Circulation Society. 2014;78:2779–801. [DOI] [PubMed] [Google Scholar]
- 4.Beltrame JF, Crea F, Kaski JC, Ogawa H, Ong P, Sechtem U, Shimokawa H, Bairey Merz CN, Coronary Vasomotion Disorders International Study G. International standardization of diagnostic criteria for vasospastic angina. European heart journal. 2017;38:2565–8. [DOI] [PubMed] [Google Scholar]
- 5.Aziz A, Hansen HS, Sechtem U, Prescott E, Ong P. Sex-Related Differences in Vasomotor Function in Patients With Angina and Unobstructed Coronary Arteries. J Am Coll Cardiol 2017;70:2349–58. [DOI] [PubMed] [Google Scholar]
- 6.Shah A, Chen C, Campanella C, Kasher N, Evans S, Reiff C, Mishra S, Hammadah M, Lima BB, Wilmot K, Al Mheid I, Alkhoder A, Isakadze N, Levantsevych O, Pimple PM, Garcia EV, Wittbrodt M, Nye J, Ward L, Lewis TT, Kutner M, Raggi P, Quyyumi A, Vaccarino V, Bremner JD. Brain correlates of stress-induced peripheral vasoconstriction in patients with cardiovascular disease. Psychophysiology. 2018:e13291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bremner JD, Campanella C, Khan Z, Shah M, Hammadah M, Wilmot K, Al Mheid I, Lima BB, Garcia EV, Nye J, Ward L, Kutner MH, Raggi P, Pearce BD, Shah AJ, Quyyumi AA, Vaccarino V. Brain Correlates of Mental Stress-Induced Myocardial Ischemia. Psychosom Med 2018;80:515–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Slavich M, Patel RS. Coronary artery spasm: Current knowledge and residual uncertainties. Int J Cardiol Heart Vasc 2016;10:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vogelzangs N, Beekman AT, de Jonge P, Penninx BW. Anxiety disorders and inflammation in a large adult cohort. Transl Psychiatry. 2013;3:e249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang M, Su S, Goldberg J, Miller AH, Levantsevych OM, Shallenberger L, Pimple P, Pearce B, Bremner JD, Vaccarino V. Longitudinal association of inflammation with depressive symptoms: A 7-year cross-lagged twin difference study. Brain Behav Immun 2019;75:200–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asbury EA, Creed F, Collins P. Distinct psychosocial differences between women with coronary heart disease and cardiac syndrome X. European heart journal. 2004;25:1695–701. [DOI] [PubMed] [Google Scholar]
- 12.Daniel M, Agewall S, Berglund F, Caidahl K, Collste O, Ekenback C, Frick M, Henareh L, Jernberg T, Malmqvist K, Schenck-Gustafsson K, Spaak J, Sundin O, Sorensson P, S YH, Hofman-Bang C, Tornvall P. Prevalence of Anxiety and Depression Symptoms in Patients with Myocardial Infarction with Non-Obstructive Coronary Arteries. Am J Med 2018;131:1118–24. [DOI] [PubMed] [Google Scholar]
- 13.Hayek SS, Ko YA, Awad M, Del Mar Soto A, Ahmed H, Patel K, Yuan M, Maddox S, Gray B, Hajjari J, Sperling L, Shah A, Vaccarino V, Quyyumi AA. Depression and chest pain in patients with coronary artery disease. Int J Cardiol 2017;230:420–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parashar S, Rumsfeld JS, Spertus JA, Reid KJ, Wenger NK, Krumholz HM, Amin A, Weintraub WS, Lichtman J, Dawood N, Vaccarino V. Time course of depression and outcome of myocardial infarction. Arch Intern Med 2006;166:2035–43. [DOI] [PubMed] [Google Scholar]
- 15.Burg MM, Soufer R. Psychological Stress and Induced Ischemic Syndromes. Current cardiovascular risk reports. 2014;8:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wei J, Rooks C, Ramadan R, Shah AJ, Bremner JD, Quyyumi AA, Kutner M, Vaccarino V. Meta-analysis of mental stress-induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease. Am J Cardiol 2014;114:187–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burg MM, Meadows J, Shimbo D, Davidson KW, Schwartz JE, Soufer R. Confluence of depression and acute psychological stress among patients with stable coronary heart disease: effects on myocardial perfusion. Journal of the American Heart Association. 2014;3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wei J, Pimple P, Shah AJ, Rooks C, Bremner JD, Nye JA, Ibeanu I, Murrah N, Shallenberger L, Raggi P, Vaccarino V. Depressive symptoms are associated with mental stress-induced myocardial ischemia after acute myocardial infarction. PloS one. 2014;9:e102986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pimple P, Hammadah M, Wilmot K, Ramadan R, Al Mheid I, Levantsevych O, Sullivan S, Garcia EV, Nye J, Shah AJ, Ward L, Mehta P, Raggi P, Bremner JD, Quyyumi AA, Vaccarino V. Chest Pain and Mental Stress-Induced Myocardial Ischemia: Sex Differences. Am J Med 2018;131:540–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sullivan S, Hammadah M, Al Mheid I, Wilmot K, Ramadan R, Alkhoder A, Isakadze N, Shah A, Levantsevych O, Pimple PM, Kutner M, Ward L, Garcia EV, Nye J, Mehta PK, Lewis TT, Bremner JD, Raggi P, Quyyumi AA, Vaccarino V. Sex differences in hemodynamic and microvascular mechanisms of myocardial ischemia induced by mental stress. Arterioscler Thromb Vasc Biol 2018;38:473–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaccarino V, Shah AJ, Rooks C, Ibeanu I, Nye JA, Pimple P, Salerno A, D’Marco L, Karohl C, Bremner JD, Raggi P. Sex differences in mental stress-induced myocardial ischemia in young survivors of an acute myocardial infarction. Psychosom Med 2014;76:171–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Almuwaqqat Z, Sullivan S, Hammadah M, Lima BB, Shah AJ, Abdelhadi N, Fan S, Wilmot K, Al Mheid I, Bremner DJ, Garcia E, Nye JA, Elon L, Li L, O’Neal WT, Raggi P, Quyyumi AA, Vaccaino V. Sex-specific association between coronary artery disease severity and myocardial ischemia induced by mental stress. Psychosom Med 2018;In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vaccarino V, Sullivan S, Hammadah M, Wilmot K, Al Mheid I, Ramadan R, Elon L, Pimple PM, Garcia EV, Nye J, Shah AJ, Alkhoder A, Levantsevych O, Gay H, Obideen M, Huang M, Lewis TT, Bremner JD, Quyyumi AA, Raggi P. Mental Stress-Induced-Myocardial Ischemia in Young Patients With Recent Myocardial Infarction: Sex Differences and Mechanisms. Circulation. 2018;137:794–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hung M, et al. Coronary Artery Spasm as Related to Anxiety and Depression: a Nationwide Population-Based Study. Psychosom Med (in press). [DOI] [PubMed] [Google Scholar]
- 25.Davis KA, Sudlow CL, Hotopf M. Can mental health diagnoses in administrative data be used for research? A systematic review of the accuracy of routinely collected diagnoses. BMC psychiatry. 2016;16:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bugiardini R, Cenko E. A Short History of Vasospastic Angina. J Am Coll Cardiol 2017;70:2359–62. [DOI] [PubMed] [Google Scholar]


