Abstract
We herein report a sporadic Creutzfeldt-Jakob disease (sCJD) patient followed from the presymptomatic phase to death. A 67-year-old woman had abnormal hyperintense cortical lesions on diffusion-weighted magnetic resonance imaging (MRI) one year before the onset. The levels of 14-3-3 protein and total tau protein, and findings from a real-time quaking-induced conversion test were normal at first but became abnormal after disease onset. Although there are four reports of presymptomatic sCJD identified by MRI, this is the first case report in which all three biomarkers had been assessed before and after the disease onset. MRI might be the most sensitive modality for detecting presymptomatic sCJD patients.
Keywords: sporadic Creutzfeldt-Jakob disease, presymptomatic, MRI, RT-QuIC
Introduction
The presymptomatic detection of Creutzfeldt-Jakob disease (CJD) is very important in carriers of pathogenic prion genes or candidates of variant CJD. Various tests using cerebrospinal fluid (CSF) or urine have been proposed (1). However, it is quite difficult to identify patients before the disease onset in cases of sporadic CJD (sCJD).
We herein report a sCJD patient followed from the presymptomatic phase to the disease onset. Cortical hyperintensity on diffusion-weighted imaging (DWI) was more sensitive than the levels of 14-3-3 protein or total tau protein (t-tau) and findings of a real-time quaking-induced conversion (RT-QuIC) test in this case.
Case Report
A 67-year-old woman presented with abnormalities on magnetic resonance imaging (MRI) of her brain. She was a care worker who underwent MRI (1.5T) for a health check. She had no neurological symptoms at that time. She had no history of brain surgery or traveling abroad and no family members with neurological diseases. She was alert.
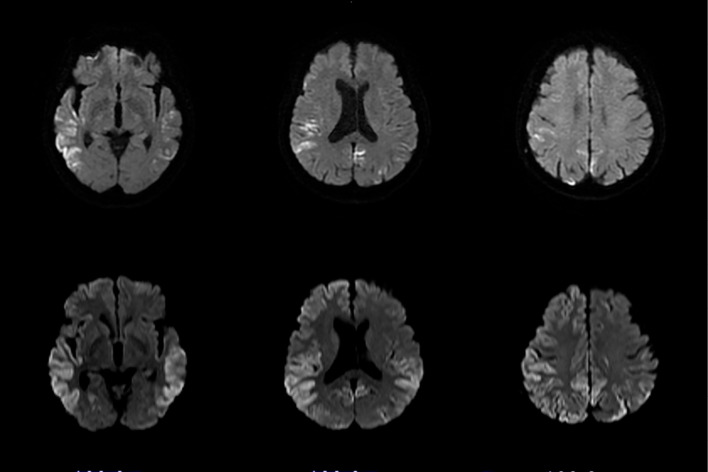
The findings of a neurological examination were normal. Cortical hyperintensity was found in the bilateral temporo-occipital cortices on DWI (Figure, upper row), and these lesions had apparent diffusion coefficient hypointensity. There was no pleocytosis in the CSF. The levels of 14-3-3 protein (2,3) (3,442 AU/mL; cut-off value >20,000) and t-tau (4) (257 pg/mL, cut-off value >1,300) in the CSF did not meet the cut-off levels for the diagnosis of CJD. The findings of semi-quantitative RT-QuIC (5) were also normal. Her electroencephalogram (EEG) was normal. Single-photon emission computed tomography using 99mTc-ethyl cysteinate dimer showed decreased cerebral blood flow in the regions corresponding to cortical hyperintensity on DWI. Her scores on the Wechsler Adult Intelligence Scale (third edition) and standard language test of aphasia were normal. A genetic analysis of her prion gene revealed homozygosity for methionine in codon 129, and no pathogenic mutation of the prion gene was detected.
Figure.
Diffusion-weighted magnetic resonance imaging scans in the presymptomatic phase (upper row) and just at the disease onset (lower row).
She showed no symptoms, even after six months. However, her area of cortical hyperintensity was enlarged. One year after her first MRI scan, she presented with difficulty walking and amnesia. The area of cortical hyperintensity (Figure, lower row) was further expanded compared to six months earlier, and slow waves were prominent on EEG. Pleocytosis was still not detected in the CSF. The levels of 14-3-3 protein and t-tau had changed to 323,276 AU/mL and 4,385 pg/mL, respectively, and the findings on RT-QuIC had become positive. Three weeks after her admission, she could not speak or stand up. Myoclonus was observed at this time. Periodic synchronized discharges were observed on EEG. Her basal ganglia became hyperintense on DWI. She developed akinetic mutism one month later and died six months after the disease onset. An autopsy was not permitted by her family.
Discussion
The clinical course after the disease onset in the present patient was compatible with probable MM1 sCJD. The most striking feature was the detection of cortical hyperintensity on DWI before the disease onset. It is very rare that a sCJD patient is encountered in the presymptomatic phase, and only four sCJD patients have been reported to have abnormal MRI findings prior to the symptom onset (Table) (6-9). Three of these patients had definite sCJD (6,8,9), and one had probable sCJD (7). The preclinical duration was 3 to 14 months. Among these patients, the levels of 14-3-3 protein and t-tau in the CSF before and after the disease onset were examined in only one (6). In that patient, these markers changed from negative to positive for the diagnosis of CJD. The RT-QuIC findings in these presymptomatic patients were not reported. In the present case, the markers of 14-3-3and t-tau as well as the RT-QuIC were negative for the diagnosis of CJD before the disease onset. The reported sensitivity and specificity of RT-QuIC are 80% and 100%, respectively (10). Considering the biochemical results of these presymptomatic CJD patients, cortical hyperintensity on DWI may be the most sensitive clinical finding for sCJD patients.
Table.
Summary of SCJD Patients Identified before Disease Onset.
| Case | Before or after onset | Age (years) | Sex | Presymptomatic duration (months) | 14-3-3 | t-tau | RT-QuIC | Cortical hyperintensity on DWI | Ref. No |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Before | 68 | M | 3 | (-) | (-) | NE | (+) | 6 |
| After | (-) | (+) | NE | (+) | |||||
| 2 | Before | 65 | F | 12 | NE | NE | NE | (+) | 7 |
| After | (+) | (+) | (+) | (+) | |||||
| 3 | Before | 74 | F | 14 | NE | NE | NE | (+) | 8 |
| After | (+) | (+) | (+) | (+) | |||||
| 4 | Before | 77 | M | 8 | NE | NE | NE | (+) | 9 |
| After | (+) | (+) | NE | (+) | |||||
| 5 | Before | 67 | F | 12 | (-) | (-) | (-) | (+) | This case |
| After | (+) | (+) | (+) | (+) |
RT-QuIC: real-time quaking-induced conversion, DWI: diffusion-weighted imaging, NE: not examined, Ref. No: Reference number
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We thank Professor Tetsuyuki Kitamoto of Tohoku University for performing the prion gene analysis.
References
- 1. Al-Ansari A, Robertson NP. Creutzfeldt-Jacob disease: new directions in diagnosis and therapeutics. J Neurol 264: 1029-1031, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Satoh K, Tobiume M, Matsui Y, et al. Establishment of a standard 14-3-3 protein assay of cerebrospinal fluid as a diagnosis tool for Creutzfeldt-Jakob disease. Lab Invest 90: 1637-1644, 2010. [DOI] [PubMed] [Google Scholar]
- 3. Schmitz M, Ebert E, Stoeck K, et al. Validation of 14-3-3 protein as a marker in sporadic Creutzfeldt-Jakob disease diagnostic. Mol Neurobiol 53: 2189-2199, 2016. [DOI] [PubMed] [Google Scholar]
- 4. Satoh K, Shirabe S, Tsujino A, et al. Total tau protein in cerebrospinal fluid and diffusion-weighted MRI as an early diagnostic marker for Creutzfeldt-Jakob disease. Dement Geriatr Cogn Disord 24: 207-212, 2007. [DOI] [PubMed] [Google Scholar]
- 5. Schmitz M, Cramm M, Llorens F, et al. The real-time quaking-induced conversion assay for detection of human prion disease and study of other protein misfolding diseases. Nat Protoc 11: 2233-2242, 2016. [DOI] [PubMed] [Google Scholar]
- 6. Satoh K, Nakaoke R, Nishiura Y, et al. Early detection of sporadic CJD by diffusion-weighted MRI before the onset of symptoms. J Neurol Neurosurg Psychiatry 82: 942-943, 2011. [DOI] [PubMed] [Google Scholar]
- 7. Verde F, Ticozzi N, Messina S, et al. MRI abnormalities found 1 year prior to symptom onset in a case of Creutzfeldt-Jakob disease. J Neurol 263: 597-599, 2016. [DOI] [PubMed] [Google Scholar]
- 8. Zanusso G, Camporese G, Ferrrari S, et al. Long-term preclinical magnetic resonance imaging alterations in sporadic Creutzfeldt-Jakob disease. Ann Neurol 80: 629-632, 2016. [DOI] [PubMed] [Google Scholar]
- 9. Iwasaki Y, Mori K, Ito M, Mimuro M, Kitamoto T, Yoshida M. An autopsied case of MM1+MM2-cortical with thalamic-type sporadic Creutzfeldt-Jakob disease presenting with hyperintensities on diffusion-weighted MRI before clinical onset. Neuropathology 37: 78-85, 2017. [DOI] [PubMed] [Google Scholar]
- 10. Atarashi R, Satoh K, Sano K, et al. Ultrasensitive human prion detection in cerebrospinal fluid by real-time quaking-induced conversion. Nat Med 17: 175-178, 2011. [DOI] [PubMed] [Google Scholar]