Abstract
The diagnosis of infective endocarditis is based on modified Duke's criteria, which includes clinical, biological, and echocardiographic findings. However, computed tomography (CT) has not been mentioned as a diagnostic tool in the criteria. We report a case of infective endocarditis confirmed by cardiac CT in which we could identify vegetations and perivalvular abscess not on transthoracic echocardiography and transesophageal echocardiography. Cardiac CT was feasible imaging modality for evaluating and diagnosing infective endocarditis. Cardiac CT should be recommended in patients with clinical suspicion of infective endocarditis even when transthoracic echocardiography and transesophageal echocardiography is negative for infective endocarditis.
Keywords: Cardiac computed tomography, Infective endocarditis
Introduction
The diagnosis of infective endocarditis is based on modified Duke's criteria, which include clinical, biological, and echocardiographic findings, cardiac computed tomography (CT) has not been mentioned as a diagnostic tool in the criteria. We report a case of infective endocarditis confirmed by cardiac CT in which we could identify vegetations and perivalvular abscess, but not on transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE).
Case report
A 69-year-old man with moderate aortic valve stenosis, hypertension, and diabetes was admitted to our hospital with a temperature of 37.8°C and acute back pain. On admission, his consciousness was clear, blood pressure was 102/65 mmHg, and heart rate was at 86 bpm. He demonstrated Systolic heart murmur was auscultated on examination. The other physical findings were unremarkable.
Laboratory data on admission showed marked elevations in C-reactive protein (31.4 mg/dL), white blood cell counts (124,600/µL) and brain natriuretic peptide (246.1 pg/ml). Platelet count (85,000/µL) were slightly low. Initial electrocardiogram revealed sinus tachycardia and right bundle branch block. Chest X-ray did not show any visible of cardiac valvular calcifications, otherwise it was unremarkable. Infectious diseases were suspected and performed chest-abdomen-pelvis CT and echocardiography were performed to search for the source of infection at admission. There was no finding to suggest infection and inflammation on CT. Echocardiography showed aortic valve stenosis with calcification, but vegetations were not identified. He was admitted to our hospital for a fever of unknown origin.
Although there was no evidence of systemic infection, we initiated empirical antibiotic therapy with carbapenem and vancomycin as serious infectious disease was suspected on admission. Mild pyogenic spondylitis was suspected as the cause of his back pain on lumber magnetic resonance imaging on the third day of admission. His body temperature showed marked elevation at 40.6°C with shaking chill on the fourth day. On the fifth day, ventricle fibrillation occurred and he was resuscitated. We performed coronary angiography to evaluate coronary artery disease. Coronary angiography showed normal coronary arteries. Two sets of blood cultures obtained before antibiotic therapy showed Staphylococcus aureus on the fifth day. We suspected infective endocarditis and performed TEE, however we could not identify vegetations (Fig. 1). Although we also performed bed side TTE several times after blood cultures revealed S. aureus, we could not detect vegetations. We continued antibiotic therapy with cefazolin according to antibiotic sensitivity, and the C-reactive protein level decreased gradually. We obtained blood cultures again to evaluate the therapeutic effectiveness, which showed negative results. On the 10th day, the consciousness level of him is deteriorated, and CT showed cerebral hemorrhage. On the 12th day, electrocardiogram showed complete atrioventricular (AV) block with a wide ventricular escape rhythm and prolonged QT interval. Therefore, we suspected perivalvular abscess associated with infective endocarditis and performed cardiac CT after a temporary transvenous pacemaker was placed. CT revealed perivalvular abscess which involved the region of atrioventricular node and vegetations in all cusps of aortic valve, which allowed us to confirm infective endocarditis (Fig. 2). Surgery was performed, and intraoperative findings showed bicuspid aortic valve with heavy calcifications, vegetations in all cusps, perivalvular abscess extending to aortomitral continuity. Aortic valve replacement was performed. AV conduction did not recover after surgery; therefore a dual-chamber permanent pacemaker was implanted. He was discharged with good postoperative course.
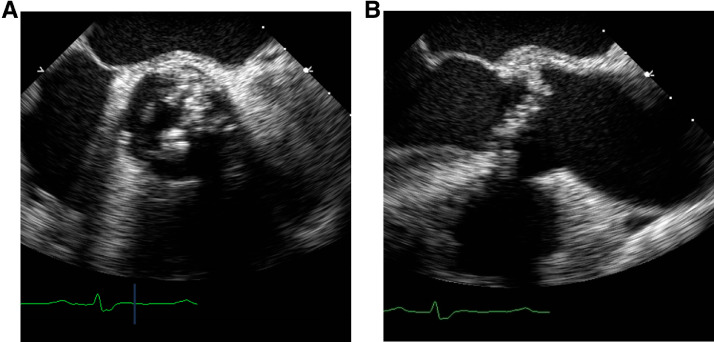
Fig. 1.
Transesophageal echocardiography midesophageal aortic valve short axis view (A) and Midesophageal aortic valve long axis view (B) on the fifth day showed heavy calcifications in aortic valve. The vegetations could not be identified.
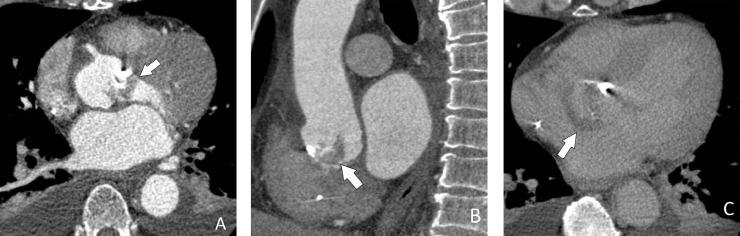
Fig. 2.
Cardiac CT (iCT, Philips, the Netherlands) was performed in double phase scan with the initial arterial phase and second delayed phase scan on the 12th day. Scan parameters were: slice collimation, 128 × 0.625 mm; gantry rotation time, 270 milliseconds (SDFlash) or 330 milliseconds (SD); pitch, 0.2; tube voltage, 120 kVp and tube current, 400 mAs. Cardiac CT axial (A, C) and sagittal (B) image showed vegetations in aortic valve (arrow (A), (B)), and perivalvular abscess which involved in the region of atrioventricular node (arrow (C)).
Discussion
We identified vegetations and perivalvular abscess on cardiac CT but not on TTE and TEE, to diagnose infective endocarditis. We found out 2 clinical issues. First, CT was feasible imaging modality for detecting vegetations and perivalvular abscess to diagnose infective endocarditis. Second, CT could complement echocardiography for evaluating and diagnosing infective endocarditis when repeated echocardiography resulted in negative study for suspected infective endocarditis.
CT was feasible imaging modality for detecting vegetations and perivalvular abscess to diagnose infective endocarditis. The diagnosis of infective endocarditis is based on modified Duke's criteria, including echocardiography result as imaging modality. CT has not been mentioned as a diagnostic tool in the criteria. Previous study showed that the sensitivity and specificity of CT in detecting leaflet vegetation and pseudoaneurysm was comparable to TEE, using intraoperative surgical findings as a standard of reference [1], [2]. Other study showed that CT provided more accurate anatomic information regarding perivalvular extent of abscess, and pseudoaneurysms than TEE [3], [4]. The European Society of Cardiology guidelines mentions CT for the detection of vegetations in prosthetic valve and the evaluation of complications associated with infective endocarditis including perivalvular involvement and extracardiac lesions, and highly detectability of peripheral embolic events. Although the guidelines mainly consider CT accessory role for the evaluation of infective endocarditis, it does not mention clearly CT as a viable tool for diagnosis of infective endocarditis [5]. We could detect vegetations as well as perivalvular abscess on cardiac CT but not on repeated echocardiography. To our knowledge, this is the first case report where infective endocarditis was diagnosed on cardiac CT but not on echocardiography.
CT could complement echocardiography for evaluating and diagnosing infective endocarditis when repeated echocardiography resulted in negative study for suspected infective endocarditis. Echocardiography is regarded as optimal tool in the assessment of infective endocarditis [6]. Performing initial TTE is usually recommended, and first-line TEE is recommend when TTE is not going to be diagnostic. However, atypical findings are frequent, and echocardiography may be falsely negative in 15% of infective endocarditis, particularly in cases of pre-existent severe lesions such as mitral valve prolapse, degenerative lesions, and prosthetic valves [7]. Echocardiography is limited in its diagnostic ability due to its dependence on the individual patient's morphology, instrumental settings, transducer position, operator, and artifacts from heavy valve calcifications and metallic prosthetic valves through acoustic shadowing. On the other hand, CT allows observation from multiple directions by reconstructing images of any section regardless of such factors including patient morphology or operator skill. Transesophageal echocardiography is a semi-invasive technique, usually performed with the use of conscious sedation. The recognized complication occurrence rate during TEE examination is 0.88% and includes bleeding, perforation, conscious sedation/anesthesia-related events, hypotension, cardiac arrhythmia, and death [8]. On the other hand, CT is a safe, noninvasive modality, requiring minimal patient cooperation and allows rapid scanning. CT also has the capacity to assess anatomy of coronary artery and to diagnose peripheral embolic events in a single examination. Precise, rapid assessment of cardiac and extracardiac lesions in infective endocarditis has an impact on the choice of treatment. Thus, CT is an imaging modality that assessed valvular and perivalvular involvement, extracardiac lesions, and noninvasive evaluation of anatomy of coronary artery, simultaneously.
In general, CT misses some small vegetations and valve leaflet perforations for infective endocarditis and is not suitable for evaluating hemodynamics and function, but echocardiography does allow visualization of the blood, so the 2 modalities might be used as complementary techniques. In this case, we cannot precisely refer to superiority in detectability of infective endocarditis lesions between TEE and CT because we did not perform TEE and CT on the same day. However, cardiac CT could be a feasible choice for the evaluation of infective endocarditis because of its low invasiveness and ability to detect vegetations and perivalvular complications if repeated echocardiography resulted in negative study for suspected infective endocarditis.
In conclusion, CT was a feasible imaging modality in detecting vegetations and perivalvular abscess to diagnose infective endocarditis. Cardiac CT could complement echocardiography for evaluating and diagnosing infective endocarditis when repeated echocardiography resulted in negative study for suspected infective endocarditis. CT should be recommended in patients with clinical suspicion of infective endocarditis even when TTE and TEE is not diagnostic.
Acknowledgment
The authors would like to show my greatest appreciation to Reina Kawakami, the clinical fellow of The Jikei University School of Medicine, for insightful comments and suggestions.
Footnotes
The authors have no conflict of interest directly relevant to the content of this article.
Our institutional review board approved the study, and we obtained written informed consent from the patient.
References
- 1.Feuchtner G.M., Stolzmann P., Dichtl W., Schertler T., Bonatti J., Scheffel H. Multislice computed tomography in infective endocarditis: comparison with transesophageal echocardiography and intraoperative findings. J Am Coll Cardiol. 2009;53:436–444. doi: 10.1016/j.jacc.2008.01.077. [DOI] [PubMed] [Google Scholar]
- 2.Ouchi K., Sakuma T., Ojiri H. Cardiac computed tomography as a viable alternative to echocardiography to detect vegetations and perivalvular complications in patients with infective endocarditis. Jpn J Radiol. 2018;36:421–428. doi: 10.1007/s11604-018-0740-5. [DOI] [PubMed] [Google Scholar]
- 3.Bruun N.E., Habib G., Thuny F., Sogaard P. Cardiac imaging in infectious endocarditis. Eur Heart J. 2014;35:624–632. doi: 10.1093/eurheartj/eht274. [DOI] [PubMed] [Google Scholar]
- 4.Fagman E., Perrotta S., Bech-Hanssen O., Flinck A., Lamm C., Olaison L., Svensson G. ECG-gated computed tomography: a new role for patients with suspected aortic prosthetic valve endocarditis. Eur Radiol. 2012;22:2407–2414. doi: 10.1007/s00330-012-2491-5. [DOI] [PubMed] [Google Scholar]
- 5.Habib G., Lancellotti P., Antunes M.J., Bongiorni M.G., Casalta J.P., Del Zotti F. ESC Guidelines for the management of infective endocarditis. The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC) Eur Heart J. 2015;36:3075–3128. doi: 10.1093/eurheartj/ehv319. [DOI] [PubMed] [Google Scholar]
- 6.Li J.S., Sexton D.J., Mick N., Nettles R., Fowler V.G.Jr., Ryan T. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 7.Sachev M., Peterson G.E., Jollis J.G. Imaging techniques for diagnosis of infective endocarditis. Cardiol Clin. 2003;21:185–195. doi: 10.1016/s0733-8651(03)00026-2. [DOI] [PubMed] [Google Scholar]
- 8.Daniel W.G., Erbel R., Kasper W., Visser C.A., Engberding R., Sutherland G.R. Safety of transesophageal echocardiography: a multicenter survey of 10,419 examinations. Circulation. 1991;83:817–821. doi: 10.1161/01.cir.83.3.817. [DOI] [PubMed] [Google Scholar]