Highlights
-
•
A rapid response EEG system is tested in comparison to two conventional EEG systems.
-
•
The rapid response EEG provides quality equivalent or better than conventional EEG.
-
•
The rapid response EEG has less 60 Hz noise compared to conventional EEG.
Keywords: Electroencephalography, Easy EEG, Rapid response EEG, Concordance
Abstract
Objectives
To compare the quality of electroencephalography (EEG) signals recorded with a rapid response EEG system and the signals recorded with conventional clinical EEG recordings.
Methods
We studied the differences between EEG recordings taken with a rapid response EEG system (Ceribell) compared to conventional EEG through two separate set of studies. First, we conducted simultaneous recording on a healthy subject in an experimental laboratory setting where the rapid response EEG and two conventional EEG recording systems (Nihon Kohden and Natus) were used at the same time on the same subject using separate but adjacently placed electrodes. The rapid response EEG was applied by a user without prior training in EEG set up while two separate sets of conventional EEG electrodes were placed by a trained EEG technologist. The correlation between each of the recordings was calculated and quantitatively compared. In the second study, we performed a set of consecutive recordings on 22 patients in an ICU environment. The rapid response EEG system was applied by clinical ICU fellows without prior training in EEG set up while waiting for the conventional EEG system to arrive, after which the rapid response EEG was stopped and the conventional EEG was applied by a trained EEG technologist. We measured and compared several metrics of EEG quality using comparative metrics.
Results
For the simultaneous recording performed in a laboratory environment, the tested rapid response EEG and conventional EEG recordings showed agreement when aligned and visually compared in the time domain, all EEG waveform features were distinguishable in both recordings. The correlation between each pair of recordings also showed that the correlation between the rapid response EEG recording and each of the two conventional recordings was statistically the same as the correlation between the two conventional recordings. For the consecutive recordings performed in real life clinical ICU environment, Hjorth parameters, spike count, baseline wander, and kurtosis measures were statistically similar (p > 0.05, Wilcoxon signed rank test) for the rapid response EEG and conventional clinical EEG recordings. The rapid response EEG data had significantly lower 60 Hz noise compared to recordings made with the conventional systems both in laboratory and ICU settings. Lastly, the clinical information obtained with the rapid response EEG system was concordant with the diagnostic information obtained with the conventional EEG recordings in the ICU setting.
Conclusions
Our findings show that the tested rapid response EEG system provides EEG recording quality that is equivalent to conventional EEG systems and even better when it comes to 60 Hz noise level. The concordance between the rapid response EEG and conventional EEG systems was demonstrated both in a controlled laboratory environment as well as in the noisy environment of a hospital ICU on patients with altered mental status.
Significance
Our findings clearly confirm that the tested rapid response EEG system provides EEG data that is equivalent in quality to the recordings made using conventional EEG systems despite the fact that the rapid response system can be applied within few minutes and with no reliance on specialized technologists. This can be important for urgent situations where the use of conventional EEG systems is hindered by the lengthy setup time and limited availability of EEG technologists.
1. Introduction
Obtaining stat EEG in emergency departments (EDs) or intensive care units (ICUs) for high-risk patients can enhance the accuracy and speed of diagnosis of neurological disorders, while reducing time until treatment. Currently the use of EEGs in urgent situations is limited by lengthy setup time as well as the availability of specialized EEG technologists. The average delay between when an EEG is ordered and when the recording is initiated can be several hours or more (Gururangan et al., 2016). This makes it difficult or impossible for most hospitals to meet recent guidelines which state that EEG should be initiated within 60 min in urgent situations, such as when status epilepticus is suspected (Brophy et al., 2012).
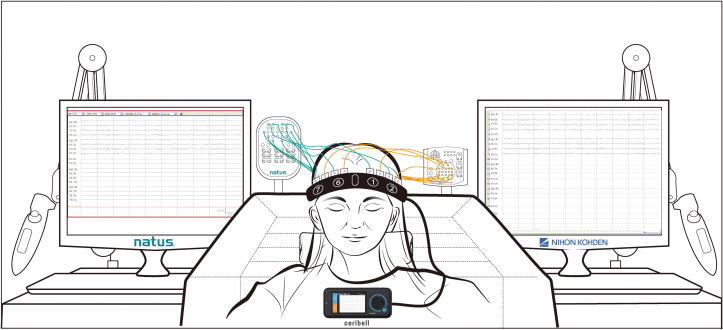
In this study, a rapid response EEG system is tested that addresses the limitations of conventional EEG systems, particularly in urgent situations when non-convulsive and subclinical seizures are suspected. The tested rapid response EEG system consists of a portable EEG recorder that records, displays, and transmits EEG waveforms, and a single use, disposable EEG headband (Fig. 1).
Fig. 1.
The rapid response EEG system consisting of a portable EEG recorder and a disposable electrode headband.
Since the tested rapid response EEG system can be applied in few minutes by users who do not need to have any prior background in EEG set up, a question that may be raised is to what extent it provides the same quality of EEG recordings as the conventional EEG systems that requires a certified EEG technologist to set up. The purpose of this study was to address the question by evaluating the signal quality of EEG waveforms acquired with the tested rapid response EEG system in comparison to conventional clinical EEG systems in laboratory as well as clinical ICU settings.
2. Methods
This study was performed in two separate settings:
-
•
Experimental Setting: Simultaneous recording of the rapid response EEG system and two conventional EEG systems on a healthy human subject in a laboratory environment during various conditions.
-
•
Real life Clinical ICU Setting: Consecutive recordings with the rapid response EEG system and then conventional EEG systems on 22 patients admitted to ICU with altered mental status
2.1. Simultaneous recording in healthy subject
In this test, a full system comparison was made with simultaneous recordings on a healthy adult female subject with usual hair volume (Fig. 2). This test was conducted as part of a healthy subject study overseen and approved by the Western Institutional Review Board (WIRB), WIRB protocol 20161422. Informed consent was obtained from the subject, and the subject was not affiliated with Ceribell in any way. The rapid response EEG recorder and disposable headband were connected to the subject, and simultaneously two conventional EEG recording systems (described below) and conventional cup electrodes were connected to the same subject. The conventional electrodes were prepped and applied by a qualified EEG technologist while a trained user of the rapid response EEG system applied the disposable EEG headband. The electrodes used for both conventional EEG systems were 10 mm Ag/AgCl disposable EEG cup electrodes (Model DAGD152600, Rhythmlink International, Columbia, SC). The skin was first prepared with EEG skin prep gel (Nuprep gel, Weaver and Co., Aurora, CO), then secured to the scalp with EEG electrode paste (Ten20 paste, Weaver and Co., Aurora, CO) and collodion.
Fig. 2.
Simultaneous recordings in a single subject with three EEG systems: rapid response EEG, conventional EEG #1, and conventional EEG #2.
The rapid response EEG headband electrodes and corresponding conventional electrodes were positioned to be as close as possible, but the electrodes were not touching and there was no overlap of conductive gel; this ensured that there were no electrical shorts between the rapid response EEG and conventional EEG electrodes. The simultaneous recording session was approximately 37 min in duration and the subject was asked to perform different activities during EEG recording. The activities included: resting with eyes closed, blinking, eyes open, clenching jaw, talking, walking, and talking on a cellphone (connected to charger).
All EEG recordings were then pre-processed with a 4th order Butterworth bandpass filter with [1–70 Hz] passband, resampled if necessary, and were compared visually for the entire recording by aligning the recordings and overlaying the waveforms in the time-domain. Since the electrodes are placed close together and the recordings from all 3 systems are from the same subject and simultaneous, the waveforms are expected to match each other. But since the electrodes are not at identical locations, some differences are unavoidable. The goal was to show that the difference between the rapid response EEG waveform and either of the two conventional recordings is not greater that the difference between the two conventional recordings.
In addition to visual alignment and comparison, the correlation between each pair of EEG recordings was calculated and compared (rapid response EEG to conventional EEG #1, rapid response EEG to conventional EEG #2, and conventional EEG #1 to conventional EEG #2). The correlation was calculated as the Pearson correlation coefficient for each pair of recordings A and B:
where μ and σ are the mean and standard deviations of each recording.
2.1.1. EEG systems
Conventional EEG #1 (Neurofax EEG-1200, Nihon Kohden Co., Tokyo, Japan) is a conventional EEG recording system that acquires EEG data from electrodes with a common reference channel, with a frequency response of 0.016–300 Hz. The sampling rate is configurable from 200 to 1000 Hz. In this study, Conventional EEG #1 data was acquired at a sampling rate of 500 Hz, then downsampled to 250 Hz to match the rapid response EEG. Conventional EEG #2 (NicoletOne, Natus Medical Inc., Pleasanton, CA) is a conventional EEG system that acquires EEG data from electrodes with a common reference channel, with a frequency response of 0.1–500 Hz. The sampling rate is configurable from 128 to 1024 Hz. In this study, Conventional EEG #2 data was acquired at a sampling rate of 256 Hz, then downsampled to 250 Hz to match the rapid response EEG.
The tested rapid response EEG system includes a portable EEG recorder (Ceribell Model C100, Ceribell Inc., Mountain View, CA), a pocket-sized device that records, displays, and transmits EEG waveforms. The system also includes a disposable EEG headband (Ceribell Model C152, Ceribell Inc., Mountain View, CA). The EEG headband consists of a stretchable band that contains ten integrated Ag/AgCl electrode assemblies. Each electrode assembly also comprises skin preparing features and is pre-loaded with conductive gel. The electrode assemblies are round and 19.8 mm in diameter.
The rapid response EEG system records 8 channels of data from a bipolar array of 10 electrodes (Fig. 1). The data is acquired as digital samples at a rate of 250 Hz, with a frequency response of 0.5–100 Hz. During recordings, the rapid response EEG recorder automatically measures electrode impedances at regular intervals so that disconnected electrodes can be detected and fixed.
The rapid response EEG system records EEG waveforms using 10 electrodes configured in a bipolar montage with 4 electrode pairs on each hemisphere (Table 1). The fixed bipolar configuration of the rapid response EEG system means that the EEG recordings cannot be re-montaged during subsequent review. The rapid response EEG channels are: Left: Fp1-F7, F7-T3, T3-T5, T5-O1; Right: Fp2-F8, F8-T4, T4-T6, T6-O2. For the comparisons performed in this study, the EEG recordings from the conventional EEG systems were configured to match the rapid response EEG electrode pairs.
Table 1.
The tested rapid response EEG system’s electrode pairs.
| Rapid response EEG system channels | Corresponding conventional EEG channels | Rapid response EEG system channels | Corresponding conventional EEG channels |
|---|---|---|---|
| 1–2 | Fp1-F7 | 6–7 | Fp2-F8 |
| 2–3 | F7-T3 | 7–8 | F8-T4 |
| 3–4 | T3-T5 | 8–9 | T4-T6 |
| 4–5 | T5-O1 | 9–10 | T6-O2 |
The rapid response EEG system automatically uploads EEG data to a cloud-hosted server. Using a web browser interface, neurologists are able to log in and review EEG sessions in real-time or retrospectively. The review software provides the ability to make annotations and comments, adjust gain/scale settings, select different high and low pass filter options, and select a powerline (60 Hz) notch filter. The review software also displays notes and tags that were made at the bedside on the rapid response EEG recorder.
2.2. Consecutive recordings of ICU patients
Simultaneous or side-by-side comparison tests are only possible in a controlled laboratory environment. To evaluate the performance of the tested rapid response EEG system under real use conditions in a hospital, a study was performed in a clinical ICU setting at the Stanford University Medical Center neuro-ICU. This study was overseen and approved by the Stanford University institutional Review Board, protocol number 38555. Informed consent was obtained from the patients’ surrogate decision makers as the patients were of altered mental status and unable to consent for themselves. Further details of the conduct of the study can be found in (Hobbs et al., 2018).
Patients enrolled in this study presented with altered mental status and suspicion of seizure requiring EEG for diagnosis. For each subject, EEG data was first recorded with the rapid response EEG system while awaiting the arrival of an EEG technologist and the conventional EEG system. The rapid response EEG system was applied by a neuro-ICU fellow. After the arrival of the EEG technologist and conventional EEG system, the rapid response EEG system was removed and the EEG technologist applied the conventional EEG electrodes and initiated an EEG recording with the conventional EEG system. The conventional EEG systems used in this study were the same make and model as Conventional EEG #1 described in Section 2.1.1.
A total of 22 subjects had EEG recordings with both the rapid response EEG and conventional EEG systems. These patients were studied as part of a prospective observational clinical trial (Hobbs et al., 2018). Patients were admitted to intensive care units at Stanford Medical Center and suffered from various neurological diagnoses. Since the recordings were not simultaneous, signals were not expected to closely match in the time domain but given that they were obtained from the same patients and the conditions of the patients were likely to be similar at the time of both recordings, they were expected to have the same overall characteristics. To assess that, we performed the following analysis.
The recorded EEG data from both the rapid response EEG and conventional EEG systems were pre-processed with a 4th order Butterworth bandpass filter with [1–70 Hz] passband. After filtering, the first 5 min (after skipping the first minute) of both rapid response EEG and conventional EEG systems were used for evaluation. The first minute was skipped because for the conventional EEG system, the first minute often included artifacts from the EEG setup. The first 5 min was selected as the evaluation period to provide the most consistent comparison between EEG recordings as the total recording length for both the rapid response EEG and conventional EEG recordings varied between patients. The following metrics were calculated on both sets of data to characterize concordance and to demonstrate that for each metric pair, there isn’t any statistical difference between the rapid response EEG and conventional recording. The metrics used for this analysis are: Hjorth parameters, spike count, baseline wander, power of 60 Hz noise and kurtosis. All metrics are described in Section 2.2.1. All metrics were calculated for all channels on segments of 10 s duration. The metrics from all 8 channels were then averaged to have one value per each 10 s of data, and these values were subsequently averaged over all 10 s segments for the evaluation period, resulting in a feature vector which was statistically compared between the rapid response EEG and conventional EEG.
2.2.1. Metrics
2.2.1.1. Hjorth parameters
Hjorth parameters – Activity, Mobility and Complexity – are indicators of statistical properties of a signal and are commonly used in the analysis of EEG signals. Activity is defined as:
where y(t) represents the time domain signal.
Mobility is defined as below and is a representative of the mean frequency and proportional to standard deviation of power spectrum.
Complexity, indicates the signal’s similarity to sine waves and converges to one if the signal is a pure sine wave.
2.2.1.2. Artifact spike count
In our study, artifact spike count is defined as number of datapoints outside of mean ± 6 standard deviation of the signal segment (note that each artifact spike usually consists of multiple datapoints so the actual number of real artifact spikes is less than the artifact spike count metric but since we only use this metric for comparison this definition provides a consistent comparison).
2.2.1.3. Baseline wander
Baseline wander is where the base axis of the signal appears to “wander” or drift up and down rather than being straight. In this study, it is defined as the absolute value of the change in the average of the signal from one segment to the other.
2.2.1.4. Power of 60 Hz noise
This metric calculates the average power of the signal around 60 Hz frequency to measure the power line interference on EEG channels (which is at 60 Hz in north America).
2.2.1.5. Kurtosis
Kurtosis is the fourth moment of the signal defined as:
where y is the time-domain signal, µ is the mean of y and σ is its standard deviation. Kurtosis is a measure of outliers in the signal or the “tailedness” of its probability distribution.
3. Results
3.1. Simultaneous recording of healthy subject
The simultaneous recordings taken with the rapid response EEG and two conventional EEG systems were time-domain aligned and visually compared for the entire duration of the recording. As shown in Fig. 3, the visual comparison showed good agreement between rapid response EEG and each of the two conventional EEG systems.
Fig. 3.
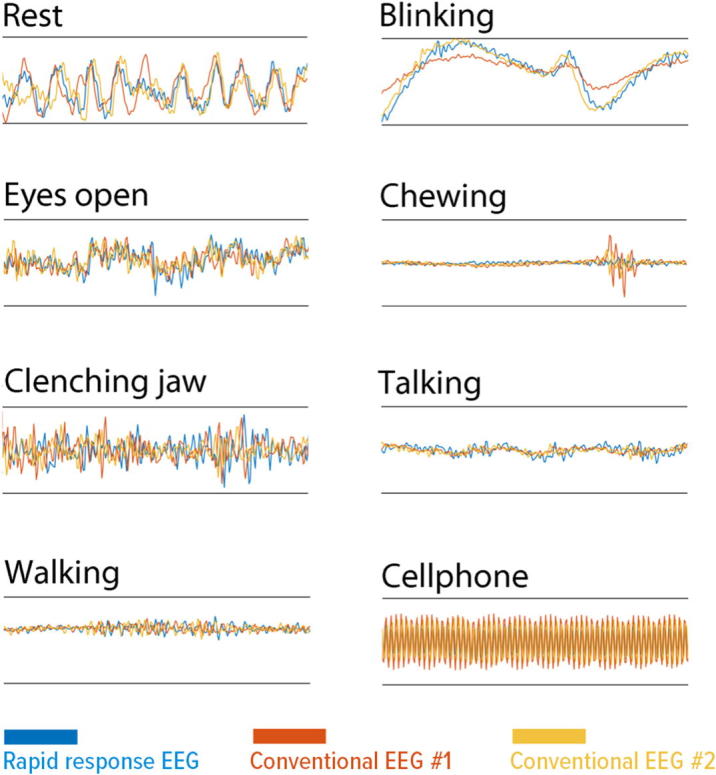
Comparison of epochs of interest showing the EEG waveforms captured by the tested rapid response EEG (blue traces), Conventional EEG #1 (orange traces), and Conventional EEG #2 (yellow traces).
The three recording systems captured signals that were not at the identical locations; the electrodes for each system were separated by approximately 2 cm to prevent shorting through the conductive gel. Therefore, small point by point differences are expected between each recording.
To offer a quantitative validation, we calculated the correlation between each pair of EEG recordings (rapid response EEG to conventional EEG #1, rapid response EEG to conventional EEG #2, and conventional EEG #1 to conventional EEG #2). The calculated correlations were: rapid response EEG to conventional EEG #1 = 0.34, rapid response EEG to conventional EEG #2 = 0.31, and conventional EEG #1 to conventional EEG #2 = 0.31. This correlation results show that the comparison between the rapid response EEG recording to each conventional EEG recording is equivalent to the comparison between the two conventional EEG recordings.
3.2. Consecutive recordings of ICU patients
Unlike the simultaneous recording described above, the ICU comparison recordings cannot be time-domain aligned as the rapid response EEG and conventional EEG recordings were taken at different times. Comparison of these recordings can only be made through calculated parameters. The parameters used for comparison were Hjorth activity, Hjorth mobility, Hjorth complexity, artifact spike count, baseline wander, power of 60 Hz noise, and kurtosis.
After all metrics were calculated for both the rapid response EEG and conventional EEG data, the Wilcoxon signed-rank test was run on each metric pair to assess whether there is a statistically significant difference between the metrics calculated for the rapid response EEG recordings vs conventional recordings. The test is performed at 5% significance level under the null hypothesis that the metrics' distributions are similar for the rapid response EEG and conventional EEG recordings. For p-values greater than 0.05, the test is considered to “pass,” meaning the rapid response EEG and conventional EEG recordings are found to be equivalent. For p-values less than 0.05, the test is considered to “fail,” meaning the rapid response EEG and conventional EEG recordings are found to have a statistically significant difference.
The p-values calculated for each metric are as follows: Hjorth Activity = 0.4264, Hjorth Mobility = 0.0883, Hjorth Complexity = 0.4264, Artifact Spike Count = 0.2912, Baseline Wander = 0.1579, Power of 60 Hz Noise = 0.0005, Kurtosis = 0.4455. The results of the Wilcoxon signed-rank test confirmed a lack of statistically significant difference between the rapid response EEG and conventional EEG signals (i.e., p > 0.05) in all except one of the selected metrics (Table 2). The power of 60 Hz noise failed the comparison with a p value of 0.0005. For power of 60 Hz noise, the conventional system recordings have significantly higher 60 Hz noise. For reference, the average power of 60 Hz noise across all subjects and all channels on the conventional recordings was 764.98 compared to 16.55 microvolt2 for the rapid response EEG recordings. The full table of calculated metrics for all of the patients is shown in Table 3.
Table 2.
Wilcoxon signed-rank test analysis of calculated parameters for ICU study of 22 subjects with non-simultaneous EEG recordings with the rapid response EEG and conventional EEG systems.
| Metric | Hjorth Activity | Hjorth Mobility | Hjorth Complexity | Artifact Spike count | Baseline wander | Power of 60 Hz noise | Kurtosis |
|---|---|---|---|---|---|---|---|
| P-value | 0.4264 | 0.0883 | 0.4264 | 0.2912 | 0.1579 | 0.0005 | 0.4455 |
Table 3.
Calculated metrics for all 22 patients recorded consecutively with the rapid response EEG (rapid resp.) and conventional EEG (con.) systems in an ICU environment.
| Hjorth Activity |
Hjorth Mobility |
Hjorth Complexity |
Artifact SpikeCount |
Baseline Wander |
Power of 60 Hz Noise |
Kurtosis |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subj. | Rapid resp. | Con. | Rapid resp. | Con. | Rapid resp. | Con. | Rapid resp. | Con. | Rapid resp. | Con. | Rapid resp. | Con. | Rapid resp. | Con. |
| 1 | 144 | 270 | 0.60 | 0.47 | 3.15 | 3.58 | 0 | 0.04 | 0.22 | 0.36 | 2.19 | 9.15 | 3.53 | 10.15 |
| 2 | 137 | 3008 | 0.46 | 0.68 | 3.46 | 3.23 | 0.02 | 0.02 | 0.15 | 0.73 | 0.45 | 101.66 | 13.05 | 9.32 |
| 3 | 26 | 2648 | 0.49 | 1.34 | 3.05 | 1.24 | 0.01 | 0.01 | 0.15 | 0.17 | 0.28 | 2197.8 | 3.87 | 4.96 |
| 4 | 1501 | 280 | 0.65 | 1.21 | 3.53 | 1.45 | 0 | 0 | 0.39 | 0.2 | 0.04 | 236.42 | 2.94 | 3.14 |
| 5 | 286 | 106 | 1.01 | 0.59 | 1.60 | 4.32 | 0 | 0 | 0.16 | 0.22 | 0.1 | 52.02 | 2.79 | 2.78 |
| 6 | 483 | 46,925 | 0.43 | 0.59 | 3.99 | 2.86 | 0.01 | 0.01 | 0.33 | 0.69 | 1.17 | 5356.6 | 4.65 | 4.67 |
| 7 | 257 | 310 | 0.87 | 0.81 | 1.92 | 2.45 | 0.02 | 0.01 | 0.3 | 0.34 | 3.31 | 19.38 | 7 | 8.22 |
| 8 | 2071 | 3221 | 0.59 | 0.47 | 3.01 | 5.74 | 0.01 | 0.01 | 1.06 | 1.99 | 11.31 | 4.99 | 4.84 | 6.81 |
| 9 | 40 | 1229 | 0.46 | 1.39 | 3.74 | 1.20 | 0.01 | 0.01 | 0.1 | 0.2 | 0.35 | 1518 | 4.16 | 5.89 |
| 10 | 91 | 14,076 | 0.67 | 1.14 | 2.41 | 1.80 | 0.02 | 0.02 | 0.19 | 1.11 | 9.65 | 6232.4 | 6.23 | 7.09 |
| 11 | 5559 | 3241 | 0.98 | 1.09 | 1.38 | 1.30 | 0.15 | 0.02 | 0.39 | 0.26 | 312.52 | 242.38 | 19.98 | 16.58 |
| 12 | 26,782 | 549 | 0.31 | 0.76 | 4.72 | 2.63 | 0.07 | 0.01 | 0.16 | 0.26 | 0.76 | 118.74 | 9.39 | 4.76 |
| 13 | 38 | 52 | 0.15 | 0.47 | 9.58 | 4.26 | 0 | 0 | 0.19 | 0.21 | 0.01 | 6.86 | 3.6 | 3.07 |
| 14 | 159 | 82 | 0.69 | 0.44 | 2.17 | 3.29 | 0.01 | 0 | 0.32 | 0.25 | 2.53 | 1.43 | 4.37 | 3.36 |
| 15 | 88 | 84 | 0.55 | 0.51 | 2.88 | 3.54 | 0 | 0 | 0.19 | 0.21 | 0.57 | 14.18 | 3.23 | 2.95 |
| 16 | 18 | 57 | 0.50 | 0.95 | 3.04 | 2.33 | 0.01 | 0 | 0.08 | 0.09 | 0.06 | 41.4 | 3.56 | 2.57 |
| 17 | 152 | 3563 | 0.40 | 0.33 | 4.70 | 5.39 | 0.01 | 0.02 | 0.55 | 1.09 | 1.12 | 15.65 | 3.35 | 6.6 |
| 18 | 404 | 336 | 1.03 | 0.33 | 1.56 | 4.75 | 0 | 0.01 | 0.23 | 0.3 | 2.22 | 86.27 | 3.53 | 6.52 |
| 19 | 78 | 379 | 0.65 | 0.71 | 2.34 | 2.18 | 0.01 | 0.01 | 0.19 | 0.14 | 2.86 | 38.48 | 3.88 | 9.12 |
| 20 | 1,205,052 | 592 | 0.81 | 1.01 | 2.42 | 1.52 | 0.02 | 0 | 19.83 | 0.29 | 11.8 | 502.66 | 5.15 | 2.92 |
| 21 | 20 | 106 | 0.30 | 0.57 | 5.58 | 3.35 | 0 | 0.01 | 0.12 | 0.15 | 0.16 | 32.52 | 3.59 | 9.51 |
| 22 | 227 | 67 | 0.42 | 0.31 | 4.56 | 4.71 | 0 | 0 | 0.5 | 0.17 | 0.74 | 0.47 | 5.1 | 3.91 |
| Median | 1927 | 1710 | 0.59 | 0.72 | 3.19 | 3.01 | 0.012 | 0.009 | 0.29 | 0.37 | 2.58 | 529.84 | 4.95 | 5.79 |
*Used trim mean 5% (trimmed mean of the values in X is the mean of X, excluding the highest and lowest K data values, where K = N*(PERCENT(=5)/100)/2 and where N is the number of values in X. Values reported for each subject is the average value of the metric over all 8 channels and entire recording.
Lastly, as shown in Table 4, the clinical information obtained with rapid response EEG system was to large extent concordant with the information revealed by conventional EEG recordings. The clinical interpretation was performed by three EEG trained epileptologists (from three different institutions) who were blinded to the patient identification. It should be noted that the two recordings were not performed simultaneously, and as per clinical study protocol, the rapid response EEG recordings had to be stopped when the conventional EEG system arrived at the bedside.
Table 4.
Concordance of clinical information obtained with the rapid response EEG and conventional EEG.
| Time* (mins) | Rapid response EEG Finding | Conventional EEG Finding | |
|---|---|---|---|
| 1 | 21 | Focal seizure in the right occipital region (7 min 23 s into recording) |
Moderate diffuse slowing. Generalized rhythmic delta activity with frontal intermittent rhythmic delta activity. |
| 2 | 43 | Focal right hemispheric seizure (12 min 04 s into recording) | Moderate to severe diffuse slowing. Patient was loaded with Keppra 1000 mg prior to conventional EEG. |
| 3 | 134 | Diffuse slowing | Diffuse slowing |
| 4 | 47 | Diffuse slowing, missing data from electrode 8 (on bandage) | Diffuse slowing |
| 5 | 8 | Diffuse slowing | Diffuse slowing |
| 6 | 7 | Diffuse slowing | Diffuse slowing with left frontal epileptiform discharges and 4 electrographic left frontal seizures |
| 7 | 21 | Excessive beta, otherwise mildly slow | Normal awake and asleep EEG |
| 8 | 74 | Slow bilaterally but with excessive movement artifact especially in the posterior channels | Moderate to severe slowing with bifrontal sharply contoured transients |
| 9 | 81 | Diffuse slowing | Diffuse slowing |
| 10 | 115 | Diffuse slowing | Diffuse slowing with Generalized Periodic Discharges |
| 11 | 44 | Generalized periodic discharges on suppressed background with excessive muscle artifact | Myoclonic status epilepticus with intervening burst suppression |
| 12 | 2 | Diffuse slowing | Diffuse slowing |
| 13 | 90 | Diffuse slowing | Diffuse slowing |
| 14 | 25 | Diffuse slowing | Diffuse slowing with additional right fronto-parietal slowing and suppression |
| 15 | 92 | Diffuse slowing | Diffuse slowing |
| 16 | 25 | Diffuse slowing with GPDs | Diffuse slowing with episodes of generalized rhythmic slowing (GRDA), and rare runs of non-specific generalized periodic discharges (GPDs) |
| 17 | 76 | Diffuse slowing | Intermittent epileptiform discharges over the left and right frontal regions, less frequently over the bitemporal regions, and sometimes in the form of lateralized periodic discharges, mild to moderate diffuse slowing with additional intermittent focal slowing over the right |
| 18 | 70 | Diffuse slowing with GPDs | Diffuse slowing, including rhythmic slow patterns with additional intermittent rhythmic slowing and nonspecific periodic discharges over the left frontal region |
| 19 | 76 | Right > left slow and stimulus induced rhythmic activity | Diffuse slowing with stimulus induced rhythmic waveforms upon noxious stimulation |
| 20 | 115 | Diffuse slowing with sharply contoured waveforms (L > R) | Diffuse slowing with brief periods of discontinuities and non-specific blunted generalized discharges, occasionally in runs (Generalized Periodic Discharges) |
| 21 | 33 | Diffuse slowing | Diffuse slowing |
| 22 | 117 | Diffuse slowing | Occasional runs of Generalized Periodic Discharges (GPDs) upon stimulation with diffuse slowing |
Time = duration of rapid response EEG recording.
4. Discussion
The simultaneous recordings taken with the rapid response EEG and two conventional EEG systems were found to match for the entire duration of the recording when aligned and inspected in the time domain. The rapid response EEG and conventional EEG recordings were visually equivalent, and all EEG waveform features were distinguishable in the recordings from the two systems. Since it is impossible to place all three electrodes at the exact same location, small differences were expected and acceptable. The correlation analysis showed that the difference between the rapid response EEG and each of the conventional EEG recordings was not greater that the difference between the two conventional recordings.
While the simultaneous recording clearly shows equivalence between the rapid response EEG and conventional EEG systems, it is also important to evaluate performance under real use conditions in a hospital. However, simultaneous recordings on patients in the ICU are not practical, so the systems were evaluated based on consecutive recordings. As a result, for the consecutive recordings, EEG quality metrics were evaluated rather than coherence between the recordings. A Wilcoxon signed-rank test was used to demonstrate equivalence between the rapid response EEG recording and the conventional recording for each of the EEG quality metrics. All of the EEG quality metrics were found to be equivalent, except for the metric related to 60 Hz AC line noise in which the rapid response EEG recordings were found to have significantly less 60 Hz noise compared to the conventional recordings.
As for the diagnostic utility of the tested rapid response EEG versus conventional EEG recordings, it should be noted that recordings with rapid response EEG system were obtained as part of an industry sponsored study and as part of the study design, the rapid response EEG recordings lasted only until the conventional EEG technicians arrived at the bedside. In some instances, the procedure of obtaining informed consent from the patients’ kin was time consuming and shortly after the rapid response EEG was set up, the recording had to be stopped to allow conventional EEG monitoring to be performed. Therefore, our findings are limited by an asymmetric duration of the EEG recordings by the rapid response EEG and the hospital’s own conventional EEG system. While in a few cases seizures were detected by the rapid response EEG but not by conventional system (partly because the patients were treated with antiepileptic medications before the arrival of conventional EEG), and in some cases seizures were captured with longer recordings. Despite this limitation, it is remarkable that the rapid response EEG and conventional recordings revealed a remarkable concordance in their diagnostic utility.
With respect to the quantitative analysis of the consecutive recordings, the Hjorth parameters (activity, mobility, and complexity) are commonly used metrics of the statistical properties of EEG signals. For all three Hjorth parameters, the rapid response EEG and conventional EEG recordings were found to be statistically equivalent across the 22 ICU patients. Baseline wander, artifact spike count, and kurtosis are all metrics relating to EEG waveform artifacts. Baseline wander is indicative of signal drift over time, while artifact spike count and kurtosis are indicative of signal outliers (e.g. electrode movement artifact). For all three of these artifact related metrics, the rapid response EEG and conventional EEG recordings were again found to be statistically equivalent across the 22 ICU patients.
In the case of 60 Hz noise, the conventional EEG was found to have significantly worse 60 Hz noise compared to the rapid response EEG. The rapid response EEG system is battery powered and therefore completely isolated from any AC powered devices. For the conventional EEG system, the EEG amplifier is connected to a PC computer which is AC powered. Additionally, the rapid response EEG electrode headband uses a shielded cable whereas standard EEG electrode wires are unshielded.
Finally, we acknowledge that the technical and clinical diagnostic concordance between the rapid response EEG and conventional EEG systems does not mean that the systems are identical in their diagnostic utility. One of the major limitations of the tested rapid response system in that it contains 10 electrodes. Any EEG pattern, finding, or localization that requires electrodes in the parasagittal region cannot be measured.
5. Conclusion
The results of both parts of this study show that the tested rapid response EEG system is able to provide EEG recording quality equivalent to conventional EEG systems. This was demonstrated both in a controlled laboratory environment as well as in real life environment of a hospital ICU on patients with altered mental status. In the ICU comparison of non-simultaneous recordings, it was found that the conventional system had significantly higher 60 Hz noise compared to the rapid response EEG system. This difference may not be observable in all environments due the variation in external sources of electrical noise. Hospital rooms, and in particular ICUs and emergency departments, are typically full of a multitude of electrical monitoring and treatment equipment that may be operating simultaneously during an EEG recording. Therefore, the improved 60 Hz noise performance of the rapid response EEG system compared to the conventional EEG system is a significant advantage for busy hospital environments.
Declaration of interest
All of the authors are current full-time employees of Ceribell and were also involved in the design of the studies, analysis of data, and preparation of this manuscript.
References
- Brophy G.M., Bell R., Claassen J., Alldredge B., Bleck T.P., Glauser T. Guidelines for the evaluation and management of status epilepticus. Neurocrit. Care. 2012;17:3–23. doi: 10.1007/s12028-012-9695-z. [DOI] [PubMed] [Google Scholar]
- Gururangan K., Razavi B., Parvizi J. Utility of electroencephalography: Experience from a U.S. tertiary care medical center. Clin. Neurophysiol. 2016;127:3335–3340. doi: 10.1016/j.clinph.2016.08.013. [DOI] [PubMed] [Google Scholar]
- Hobbs K., Krishnamohan P., Legault C., Goodman S., Parvizi J., Gururangan K. Rapid Bedside Evaluation of Seizures in the ICU by Listening to the Sound of Brainwaves: A Prospective Observational Clinical Trial of Ceribell's Brain Stethoscope Function. Neurocrit. Care. 2018;29:302–312. doi: 10.1007/s12028-018-0543-7. [DOI] [PubMed] [Google Scholar]