Abstract
Background:
In an effort to reduce medication discrepancies during transitions-of-care and improve accuracy of the patient’s medication list, AU Health conducted a study to identify a comprehensive set of issues related to EHR Medication Reconciliation (MedRec) from the perspective of practitioners directly involved in the EHR MedRec process.
Methods:
An exploratory mixed-method design was used. The two-round study included 15 individual interviews, followed by a survey of 200 practitioners, i.e., physicians, nurses, and pharmacists, based in the outpatient and inpatient medicine service at AU Health.
Results:
Thematic analysis of interview data identified 55 issue-items related to EHR MedRec under 9 issue-categories. The survey sought practitioners’ importance-rating of all issue-items identified from interviews. A total of 127 (63%) survey responses were received. Factor analysis served to validate the following 6 of the 9 issue-categories, all of which, were rated “Important” or higher (on average), by over 70% of all respondents: 1) Care-Coordination (CCI); 2) Patient-Education (PEI); 3) Ownership-and-Accountability (OAI); 4) Processes-of-Care (PCI); 5) IT-Related (ITRI); and 6) Workforce-Training (WTI). Significance-testing of importance-rating by professional affiliation revealed no statistically significant differences for CCI and PEI; and some statistically significant differences for OAI, PCI, ITRI, and WTI.
Conclusion:
There were two key gleanings from the issues related to EHR MedRec unearthed by this study: 1) there was an absence of shared understanding among practitioners, of the value of EHR MedRec in promoting patient safety, which contributed to workarounds, and suboptimal use of the EHR MedRec system; and 2) there was a socio-technical dimension to many of the issues, creating an added layer of complexity. These gleanings in turn, provide insights into best practices for managing both: 1) clinical transitions-of-care in the EHR MedRec process; and 2) socio-technical challenges encountered in EHR MedRec implementation.
Keywords: Electronic Health Records, Medication Reconciliation, Patient Safety, Transitions-of-Care, Change Implementation, Quality Improvement
Background
Healthcare delivery and payment reform efforts are increasingly focused on improving quality and safety during transitions of care, when patients are most vulnerable to medical errors [1]. Medication errors in particular, are common at hospital admission and discharge, and are a major contributor to adverse patient outcomes and increased spending associated with transitions of care [2, 3]. The risk of medication errors is heightened during care transitions because, clinicians, and in some cases, patients, do not have access to accurate up-to-date medication lists. This can result in the inadvertent addition, omission or duplication of medications, resulting in “unintended discrepancies” between what patients should be prescribed, and what they are actually prescribed. [4–6].
To help prevent medication errors and discrepancies during transitions of care, patient safety advocates have promoted the use of Medication Reconciliation or “MedRec” [7, 8]. MedRec refers to the process of creating the most complete and accurate list of a patient’s current medications, comparing the list to those in the patient’s records, and communicating the final up-to-date list to the patient, family, caregivers, and the next providers of care. Since 2005, MedRec has been part of the Joint Commission’s hospital accreditation program, and more recently, it has become part of the “EHR Meaningful Use” requirements [9, 10].
Despite the regulatory impetus towards EHR MedRec, hospital adherence has lagged for one chief reason; low physician engagement, which in part, stems from lack of professional consensus about which physician (e.g., hospital vs. community physician) is responsible for managing a patient’s medication list, and the value of MedRec as a clinical tool for improving quality of care [11–15]. Moreover, within the hospital context, the assignment of MedRec responsibilities among provider subgroups—multiple physicians, nurses, and pharmacists,—is often unclear, leading to inefficiency and potential for error [16–18]. Not surprisingly therefore, a recent national study found that although hospital EHR vendors have been enhancing MedRec functionality over time, more than a third of the hospitals still use partially paper-based processes at admission, discharge, or both [13].
Purpose of the study
The Augusta University Health System, AU Health, has invested in certified EHR technology throughout its system, which includes an academic medical center and over 80 satellite outpatient clinics. Similar to issues faced by other hospitals, there is consensus among AU Health administrators that a key challenge being encountered at the institution is that physicians who did not originally order the drugs in question, are resistant to discontinuing those medications at discharge, leading to frustrated patients with incomplete and inaccurate medication lists. The EHR system requires clinicians to mark MedRec as “complete” with the press of a radio-button before patients can be officially discharged from the facility. However, in 2016, AU Health leadership estimated MedRec to be accurately completed, i.e., free of discrepancies between patient’s home and hospital medication lists in regard to drugs, dosages, and frequencies, for less than 25% of discharged cases. During the same period, the average monthly patient satisfaction score for medication instructions (“medications and care at home were explained to me in a way I could understand”) was at the 25th percentile for outpatient visits, 40th percentile for inpatient discharges, and 2nd percentile for the ED.
In an effort to reduce medication discrepancies during care transitions, and improve accuracy of the patient’s active medication list, AU Health recently conducted a study to identify a comprehensive set of issues related to EHR MedRec from the perspective of various practitioner groups (physicians, nurses, and pharmacists) directly involved in the EHR MedRec process. Such an effort was deemed as an essential first step for understanding the problem, and laying a foundation for identifying effective strategies to address the problem. This paper seeks to describe the methods and results of this study.
Design/Approach
The study began after Institutional Review Board (IRB) approval was obtained from Augusta University. An exploratory mixed-method approach was used for data collection and analysis [19]. The study included two rounds of data collection in 2017. Round 1 consisted of individual interviews with a small group of physicians, nurses, and pharmacists; while Round 2 consisted of a survey of a larger group of physicians, nurses, and pharmacists, based in the inpatient and outpatient medicine service at AU Health.
Study setting & participants
Based in Augusta, Georgia, AU Health is a health system offering comprehensive primary, specialty and subspecialty care in the region. Facilities include a 478-bed AU Medical Center, more than 80 outpatient practice sites, a Critical Care Center housing a regional trauma center and a 154-bed Children’s Hospital. AU Health uses certified EHR technology (powered by Cerner Inc.), throughout its health system. By definition, the level of EHR implementation at AU Health is “comprehensive” (HIMSS Level 6). As part of the EHR, providers can electronically prescribe medications through SureScripts™, which enables them to view patients’ medication history, including prescriptions filled at participating pharmacies.
The population-of-interest for this study was all physicians, nurses, and pharmacists in the inpatient medicine and outpatient medicine service of AU Health, including Internal Medicine, Family Medicine, Hospitalist, and Cardiology services, with Cardiology being the only medicine subspecialty included in the study. There were a total of 215 practitioners (including physicians, nurses, and pharmacists) in the population of interest, and all were included in the study, with 15 included in Round 1 and 200 included in Round 2.
Round 1 Approach
Round 1 consisted of 15 individual open-ended interviews with practitioners based in inpatient and outpatient medicine units, including 3 Internal Medicine Physicians; 3 Cardiology Physicians; 3 Hospitalists; 3 Staff Nurses; and 3 Pharmacists. Participants were asked one question: “What are the key issues you have encountered with EHR MedRec at your institution?” Interviews lasted ~30 minutes each, and were audio-recorded, with permission of participants.
Audio-recordings from the 15 interviews were transcribed to text, to facilitate Thematic Analysis using an emergent manual coding process. The Thematic Analysis team consisted of four researchers, including one MD in Internal Medicine, one PhD in Health Management, and two PhD students in biomedical sciences, hereafter referred to as Coders 1–4, respectively. To begin with, two coders (Coders 1 & 2) completed all key phases of Thematic Analysis, to develop an initial coding scheme for identifying key themes and concepts. This included: 1) data familiarization; 2) manual generation of initial codes; 3) searching for themes; 4) reviewing themes; and 5) defining and naming themes [20–22]. The initial coding scheme was used by two other coders (Coders 3 & 4) to code approximately 33% of the interview data, i.e., data from 5 of the 15 interviews. Analysis of initial inter-coder agreement amongst the four coders, revealed a 75% match. Follow-up discussions among the four coders resulted in further refinements to the coding scheme. The revised coding scheme in turn, was used by all four coders to recode 100% the interview data. This iterative process of coding, evaluation, discussion, and refinements to the coding scheme was repeated until final inter-coder agreement amongst the four coders was over 95%.
The Thematic Analysis process resulted identifying a total of 55 individual issue-items related to EHR MedRec, grouped into 9 issue-categories (themes), including: 1) Care Coordination Issues (CCI); 2) Patient Education Issues (PEI); 3) Ownership-and-Accountability Issues (OAI) 4) Process-of-Care Issues (PCI); 5) IT-Related Issues (ITRI); 6) Workforce-Training Issues (WTI); 7) Workflow Issues (WI); 8) Resources Issues (RI); and 9) Documentation Issues (DI). A full listing of the 55 issue-items grouped into 9 issue-categories, is provided in Table 1.
Table 1.
EHR Medication Reconciliation: Issue-Items and Issue-Categories
| # | Issue-Item Code | Issue-Item Description |
|---|---|---|
| Care Coordination Issues (CCI) | ||
| 1 | CCI-1 | The medication list is not complete when patient returns to the clinic after being discharged from the hospital (even if the system shows discharge reconciliation as complete). |
| 2 | CCI-2 | The current process of “discharge -then-pharmacy scripts,” rushes the process, making it difficult for pharmacy to meet patients as they transition into the community. Several opportunities for patient education (e.g. affordable options for drug substitutes etc.) are missed, as a result. |
| 3 | CCI-3 | No arrangements have been made for post-discharge follow-up with the patient’s clinic to monitor interactions of new medicines with the patient’s existing medication. |
| 4 | CCI-4 | Good medication management in the hospital alone is not sufficient. Patients are not in control after they have transitioned to the community and/or their usual customary care, which in turn, creates the risk for readmission. |
| 5 | CCI-5 | Sometimes, chronic disease poly-pharmacy patients on 15 or more medications do not have a primary care physician designated in the system. |
| 6 | CCI-6 | We do not have a process in place for identifying people who do not have a primary care physician in our EHR, and designating one from within our health system, to ensure care coordination. |
| 7 | CCI-7 | Some patients may have multiple pharmacies and multiple sub-specialist physicians. This is a challenge, since we currently does not have a reliable interface between pharmacies, specialty clinics, and primary care clinics. |
| Patient Education Issues (PEI) | ||
| 8 | PEI-1 | Patients do not understand when they need to stop taking a previous prescription and start taking the updated one. |
| 9 | PEI-2 | Patient insurance issues are not addressed at discharge. |
| 10 | PEI-3 | Patients are not educated to take control of their medication management following discharge. |
| 11 | PEI-4 | Often, patients do not have their medication lists or pill bottles with them, which makes it difficult to verify what they are actually taking. |
| 12 | PEI-5 | Patient needs to understand why they are taking each drug, e.g., Infection Drug, Diabetes Drug, and BP drug; to ensure that they stick with the regimen. This is an area for improvement. |
| 13 | PEI-6 | We do not have a standardized system for educating patients that they need to bring in their pill bottles each time they visit the clinic or ED. |
| 14 | PEI-7 | We do not have a user-friendly form or template for patients/families to list their medications while they are waiting to be seen. |
| 15 | PEI-8 | Patients are not receiving discharge instructions on which medicines to continue taking; which to stop; and why. |
| 16 | PEI-9 | Sometime patients end up taking both an earlier prescription and a replacement prescription since they have not been properly educated. |
| Ownership & Accountability Issues (OAI) | ||
| 17 | OAI-1 | Since several practitioner groups are involved in medication reconciliation, without a shared understanding of each other’s responsibilities, multiple medication lists (with varying drug information) exist for a single patient, instead of a Master List. |
| 18 | OAI-2 | There is no provision to indicate patient is “not taking” a medication on the active medication list. Nurses’ documentation of “not taking” in the medical record may be missed by the doctor, which in turn, may prevent meds from being discontinued in a timely fashion. |
| 19 | OAI-3 | A patient may have a beta-blocker drug that is on hospital formulary ordered, to replace the home beta-blocker drug, during the hospital stay, but the former may not be discontinued at discharge, allowing both formulary and home (i.e., duplicate) prescriptions of the beta-blocker to be continued on the patient’s active medication list. |
| 20 | OAI-4 | Doctors generally prefer not to discontinue a medication from the list, if they did not originally order it, or are unfamiliar with the drugs in question. |
| 21 | OAI-5 | At {the study institution}, pharmacy technicians are not being utilized to collect medication history in the ED, prior to admission, even for poly-pharmacy patients. |
| 22 | OAI-6 | Medication reconciliation has not been heavily emphasized for Nursing, so the responsibility falls upon all groups involved in patient care delivery to capture medication history. |
| 23 | OAI-7 | Medication reconciliation is not as heavily emphasized for subspecialists as it is for primary care physicians. |
| 24 | OAI-8 | In some instances, hospital personnel who notice their peers inputting incorrect information, also take time to report them, which could become a cycle of blame shifting. |
| 25 | OAI-9 | Sometimes patients experience frustration towards hospital personnel, since their medication list, which they are asked about multiple times, is not viewable by all hospital personnel. |
| 26 | OAI-10 | The quality of medication information captured varies between triage providers, hospitalists, and nurses on the floor. |
| Process of Care Issues (PCI) | ||
| 27 | PCI-1 | We do not have processes in place to ensure comprehensive medication history at the front-end (admission), which makes it difficult for medication reconciliation to be completed at the back-end (discharge). |
| 28 | PCI-2 | Both on the outpatient and inpatient side, the process of obtaining medication history from pharmacies and primary care physicians, is cumbersome and inefficient. |
| 29 | PCI-3 | Patients may not always be aware of the medications they are on, making the process of compiling a complete and accurate medication list, a challenging one for hospital providers. |
| 30 | PCI-4 | Medication reconciliation is performed only at admission and discharge; and not during the hospital stay, to supplement data gathered at admission; which in turn, affects the accuracy of reconciliation at discharge. |
| 31 | PCI-5 | During hospital stay, patients are not in regular contact with pharmacists, who are in the best position to update patients’ medication history and the active medication list. |
| 32 | PCI-6 | The medication list needs to be dynamic, not static. Often, the Admission H&P is not amended while the patient is in the hospital, even if new information is provided by patient/family. |
| IT-Related Issues (ITRI) | ||
| 33 | ITRI-1 | Some of our patients have primary care physicians outside of our system, and we are often unable to access their medication reconciliation on the EHR. |
| 34 | ITRI-2 | Patients are portable. However, even within our local community, there are many hospital EHRs that are not accessible to physicians in our system. |
| 35 | ITRI-3 | While we can retrieve External Rx Histories from various local pharmacies through the EHR, the medication history from our own outpatient pharmacy is not retrievable on the EHR. |
| 36 | ITRI-4 | Our EHR system does not include enough clinical decision support for clinical guidelines like Core Measures, although we do have support for drug-allergy alerts and drug-to-drug interactions. |
| 37 | ITRI-5 | For statin prescriptions (among MI patients), the medication label automatically prints out that it is “FOR CHOLESTEROL” which may be confusing for patients who don’t have cholesterol. |
| 38 | ITRI-6 | Sometimes on the EHR, orders for certain medications tend to pre-populate the dosages inaccurately, e.g., Valium and Vitamin D. |
| 39 | ITRI-7 | The EHR is fairly slow. Some controlled substances cannot be printed in the same room; so providers need to go to a different room, which can slow things down. |
| 40 | ITRI-8 | A check box against discharge medication reconciliation does not mean it is done. Providers understand that the button needs to be checked to bill for the patient, but they also know that the discharge medication list may be inaccurate or incomplete. |
| 41 | ITRI-9 | Users of the software system need to figure out how they can work with the configurations within the EHR system, as opposed to “working around” or against it. |
| Workforce Training Issues (WTI) | ||
| 42 | WTI-1 | Often times, house staff do not understand the importance of comprehensively documenting the medication history and continuously updating the medication list, to facilitate smooth discharge and prevent readmissions. |
| 43 | WTI-2 | The importance of medication reconciliation needs to be emphasized during resident orientation and training. |
| 44 | WTI-3 | Pharmacists could play a key role in educating hospital residents on selecting the right drug & dose; improving drug documentation; and identifying substitutes when patients cannot afford the drugs prescribed. This is an area for improvement. |
| 45 | WTI-4 | Medical Assistants, who are responsible for taking the medication inventory and entering it in the system, may not have had any pharmacological training. |
| 46 | WTI-5 | Medical Assistants in Orthopedics may be completely unfamiliar with cardiac medications. For example, in Orthopedics, they dose medicines in pounds, whereas in Cardiology, they are dosed in kilograms. |
| 47 | WTI-6 | Nursing personnel need training on how to effectively utilize limited time and resources to gather medication history so as to improve the workflow, rather than lose time working against the system. |
| Workflow Issues (WI) | ||
| 48 | WI-1 | When our ED or clinics are busy, medication history is not being obtained & recorded comprehensively. |
| 49 | WI-2 | For attending physicians, logging back into the computer to approve the final medication list after the nurse has prepared it can produce a delay, which can create a back-log of patients on a busy day. |
| 50 | WI-3 | Due to time constraints, especially during triage, medication reconciliation becomes a heavy burden on providers rushing to help the next patient; this often leads to incomplete and inaccurate information for medications inputted into the EHR. |
| Resources Issues (RI) | ||
| 51 | RI-1 | In the ED, nurses are already stretched with documentation responsibility, so some form of supplemental staffing (e.g., pharmacy techs) may be necessary for medication history. |
| 52 | RI-2 | On the outpatient side, medication reconciliation proceeds smoothly when nurses have the time and resources they need to complete medication history. |
| 53 | RI-3 | On the inpatient side, if a patient is incapacitated; we do not have a provision to leverage patient navigators in obtaining medication histories by engaging families during the hospital stay. |
| Documentation Issues (DI) | ||
| 54 | DI-1 | The specific details related to medications names, types, and dosages are not well-documented on the discharge medication list. For example, “sustained release” vs. “controlled release” dosing is not documented well. |
| 55 | DI-2 | Primary care physicians should prepare the medication list from scratch, each time the patient undergoes a change in care, by re-documenting the whole list. The physician’s notes in turn, should provide information on the patient’s updated medication list to all other providers of care. This is an area for improvement. |
Round 2 Approach
Round 2 consisted of a survey administered to the larger population of interest, i.e., 200 practitioners, including 50 nurses, 50 pharmacists, and 100 physicians (including residents, hospitalists, and physicians from internal medicine, family medicine, and cardiology services), based in inpatient and outpatient medicine units at AU Health. To ensure a fair assessment and validation of the issues in Round 2, the 15 individuals who completed the interviews in Round 1, were excluded from the survey (Round 2). The survey was conducted electronically, and contained three sections:
Section 1 captured participants’ demographic characteristics, including age, gender, race, unit affiliation, professional affiliation, and length of tenure at AU Health;
Section 2 captured participants’ importance-rating (on a 7-point Likert scale) of the 55 issue-items related to EHR MedRec (grouped into 9 “issue-categories”), identified in Round 1 interviews.
Section 3 was open-ended, and captured comments & suggestions from participants.
The survey received a total of 127 responses, translating to a 63% response rate. The STATA 14 software package was used for analysis. A variety of descriptive analyses were conducted to evaluate respondents’ importance-ratings and demographic characteristics, with the latter including unit affiliation and professional affiliation.
Unit Affiliation consisted of the following five categories for analysis: 1) Inpatient; 2) Outpatient Subspecialty; 3) Outpatient Primary Care; 4) Emergency Department; and 5) Outpatient Pharmacy.
Professional Affiliation consisted of the following six categories for analysis: 1) Internal Medicine Physician; 2) Family Medicine Physician; 3) Cardiology Physician; 4) Hospitalist; 5) Pharmacist; and 6) Nurse. The first three physician categories included residents and attending faculty members.
Next, Factor Analysis was used to validate the issue categories and generate an index for the validated issue categories, to facilitate assessment of differences in importance-rating by unit and professional affiliation. Factor Analysis served the purpose of assessing if issue-items grouped under each issue category, were correlated or loading on to a single common factor. This involved generating a Principal Factors output, including the eigenvalue for each factor [23]. An eigenvalue >1 (for a factor) means that the variables (issue-items) are meaningfully correlated with that particular factor. If the eigenvalue indicates that the variables are loading on to a single factor, the next step is to calculate the Cronbach’s Alpha (α) to assess whether all issue items included in a single issue category are sufficiently related to one another to be considered part of a single index. The common rule is that the Cronbach’s α should be at least 0.70, with many analysts seeking 0.75 or higher before the set of items is accepted as being related to a single latent factor [24, 25]. Once the factor loadings were verified through eigenvalue and Cronbach’s α, the next decision to make was whether or not to generate an index. An index was created if the eigenvalue >1 and Cronbach’s α was >0.75. The creation of indexes in turn, enabled significance-testing of differences in importance-rating by unit and professional affiliation for each index, using the ANOVA technique. Finally, the open-ended comments section was reviewed to ensure that no additional issue items related to EHR MedRec (not included in the survey) were reported by participants.
Results
Round 1 Results
The Thematic Analysis of interviews helped identify 55 issue-items related to EHR MedRec, which were in turn, grouped into 9 issue categories or themes. To begin with, participants discussed issues related to care coordination across multiple settings, e.g., across the hospital, the outpatient cardiology clinic, and the primary care clinic. For example, one cardiologist commented that “no arrangements are made for post-discharge follow-up with the patient’s clinic to monitor interactions of new medicines with the patient’s existing medications. It is not sufficient if medications are managed well during the hospital stay alone. It is more important for patients to be in control after they have transitioned to the community and their usual customary care.” A pharmacist discussed how the “current process of ‘discharge-then-scripts,’ poses a serious time constraint, which results in pharmacy not being able to meet many discharged patients before they leave the facility, at the most crucial point of transition, before they return to the community. Several opportunities for reconciliation (related to insurance, drug brand etc.) and patient education are missed by pharmacy, as a result.”
Participants from all groups also discussed several issues related to patient education. One cardiologist mentioned that “Patients do not understand when a medication is being replaced by another one, i.e., that they need to stop taking a previous prescription and start taking the more updated one; this is particularly an issue with beta-blockers and ACE inhibitors.” Similarly, within the hospital setting, hospitalists, nurse, and pharmacists commented on how patients’ lack of awareness of the medications they are on, can result in providers being unable to compile a complete and accurate medication list.
Participants also discussed concerns related to ownership & accountability. For example, a cardiologist mentioned that “a patient may have a beta-blocker drug that is on hospital formulary ordered to replace the home beta-blocker drug, during the hospital stay, but the former may not be discontinued at discharge, allowing both formulary and home (i.e., duplicate) prescriptions of the beta-blocker to be continued on the patient medication list, creating room for confusion for the patient/family and the next provider of care.” A nurse mentioned that “since you cannot indicate on the medication list that a patient is ‘not taking’ a medication, without removing it from the list; these notes are usually made by nurses within the medical record for the attending doctor to review and discontinue medications as appropriate. However, these notes are often missed by doctors.” Correspondingly, several drugs that that patient is ‘not taking’ and should be discontinued remain on the list even after discharge, causing potential for error at the next level of care.” Similarly, a pharmacist discussed how the “lack of role clarity prompts multiple practitioners (nurses, pharmacists, residents) to go through the throes of reconciliation, and yet, nobody takes full responsibility for inputting accurate information related to drug names, frequency, and dosages. This problem in turn, results in multiple medication lists for one patient, which affects not only patient safety, but also patient satisfaction during hospital stay.”
There were also a number of issues related to process of care expressed by participants. For example, an Internal Medicine physician mentioned that “MedRec is often performed only at admission or discharge; and not during the hospital stay, to supplement data gathered at admission, based on new information from family; which in turn, affects the accuracy of reconciliation at discharge.” Participants from all practitioner groups also described how the lack of a comprehensive medication history at the time of admission (front-end), could result in duplication of work, confusion related to the regimen, and an inaccurate or incomplete medication list at the time of discharge (back-end).
Several interviews also revealed concerns with IT-related issues. For example, an Internal Medicine physician commented that “patients are highly portable; however, there is considerable lack of EHR interoperability among hospitals within the local community.” Importantly, participants from all groups commented on providers’ unanimous recognition of the need for workarounds with the EHR MedRec system; “simply having a check box against discharge reconciliation does not mean it’s done. We understand that the button needs to be checked for us to bill for it, but we also know that the medication list is likely to be inaccurate or incomplete.”
Participants also spoke of workforce training issues: An Internal Medicine physician mentioned that “often times, residents do not understand the importance of continuously updating the medication list even while the patient is in the facility, to facilitate smooth discharge and prevent readmissions.” A pharmacist mentioned that “pharmacy could play a key role in educating residents on selecting the right drug and dose; improving drug documentation; and identifying substitutes when patients cannot afford the drugs prescribed.”
Participants from all groups also spoke of workflow issues. For example, a nurse mentioned that “in a busy clinic or ED, data on medication history may not be recorded comprehensively, which in turn leads to incomplete and sometimes false medication information inputted into a patient’s EHR.” Finally, yet importantly, practitioners commented on resource issues and documentation issues. In regard to the former, a hospitalist physician and a pharmacist commented on the “need for a supplemental staffing in the ED (e.g., pharmacy techs) to assist with MedRec during triage,” and in regard to the latter, a pharmacist mentioned the need for better documentation on “details related to medications names, types, and dosages on the discharge medication list.”
Round 2 Results
Results from the interviews provided a foundation for conducting a survey of a larger group of 200 practitioners (physicians, nurses, and pharmacists) based in inpatient and outpatient medicine units at AU Health. The survey received a total of 127 responses, translating to a 63% response rate. Table 2 summarizes the demographic characteristics of respondents.
Table 2.
Demographic Characteristics of Survey Respondents N=127
| Characteristic | # | % |
|---|---|---|
| Age | ||
| <25 years | 41 | 32% |
| 25–34 years | 33 | 26% |
| 35–44 years | 26 | 20% |
| 45–54 years | 27 | 21% |
| Gender | ||
| Male | 53 | 42% |
| Female | 74 | 58% |
| Race | ||
| Caucasian | 92 | 72% |
| African-American | 13 | 10% |
| Hispanic | 3 | 2% |
| Asian/Pacific Islander | 16 | 13% |
| Other | 3 | 2% |
| Length of Tenure at Facility | ||
| <1 year | 18 | 14% |
| 1-<3years | 30 | 24% |
| 3-<5 years | 13 | 10% |
| 5-<10 years | 19 | 15% |
| >=10 years | 47 | 37% |
| Professional Affiliation | ||
| Internal Medicine Physician | 23 | 18% |
| Family Physician | 22 | 17% |
| Cardiology Physician | 10 | 8% |
| Hospitalist Physician | 11 | 9% |
| Pharmacist | 35 | 28% |
| Nurse | 26 | 20% |
| Unit Affiliation | ||
| Inpatient | 76 | 60% |
| Outpatient Subspecialty | 28 | 22% |
| Outpatient Primary Care | 50 | 39% |
| Emergency Department | 7 | 6% |
| Outpatient Pharmacy | 7 | 6% |
While Professional Affiliation includes mutually exclusive categories, Unit Affiliation does not, since several physician participants practiced in both inpatient and outpatient settings.
Descriptive analysis of importance-ratings by respondents revealed that all 55 issue-items related to EHR MedRec were rated as “Important” or “Extremely Important” (i.e., “6” or “7” respectively, on a 7-point Likert Scale), by at least 70% of all respondents. Figure 1 shows the average importance-rating of issue-items within each of the nine issue-categories.
Issue-Category Average Importance-Rating
• CCI: Care Coordination Issues
• PEI: Patient Education Issues
• PCI: Process of Care Issues
• ITRI: IT-Related Issues
• WTI: Workforce Training Issues
• OAI: Ownership & Accountability Issues
• WI: Workflow Issues
• RI: Resource Issues
• DI: Documentation Issues
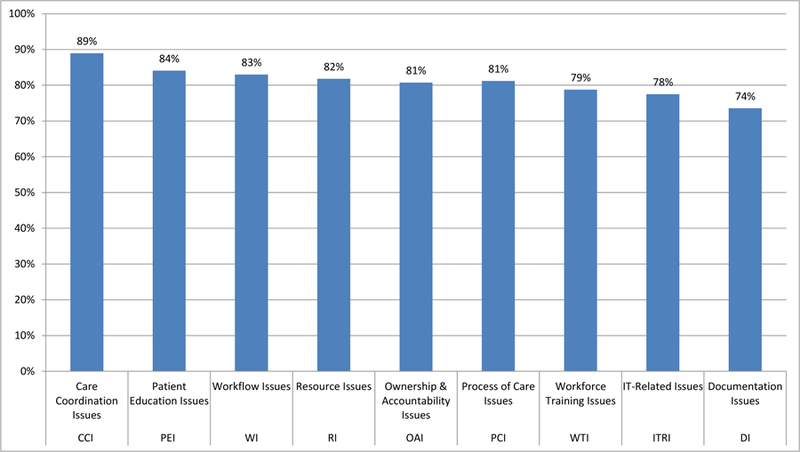
• Bars represent the average proportion of respondents who rated issue-items within each issue-category as “Important” or “Extremely Important”
Table 3 shows results of Factor Analysis for the 9 sets of issue-items (or issue-categories). The second column shows the eigenvalue generated by Factor Analysis for the first factor for each set of issue-items. For example, for CCI, the eigenvalue for the first factor generated from the issue-items was 2.41. No other factor from the output had an eigenvalue greater than 1.00, so the rest were disregarded. This suggested that the issue-items were all loading on to a single common underlying concept. As indicated in Table 3, all sets of issue-items, except DI and RI, had an eigenvalue >1. The next step was to calculate the Cronbach’s α test for all set of issue-items, to assess inter-item covariance. As indicated in Table 3, three of the nine issue-categories did not meet the minimum cutoff for Cronbach’s α of 0.75, including DI, RI, and WI. For the remaining 6 out of the original 9 issue categories, the Cronbach’s α of >0.75 suggested that these sets of issue-items were strongest in capturing a single latent concept. The next step was to generate indexes for these 6 validated issue categories, which in turn, enabled assessment of differences in importance-rating by unit and professional affiliation, for each index, through the ANOVA technique.
Table 3.
Factor Analysis Output
| Issue Category | Eigenvalue (Factor 1) | No. of Obs | No. of Items on Scale | Cronbach’s Alpha |
|---|---|---|---|---|
| Care Coordination Issues (CCI) | 2.41 | 97 | 7 | 0.80 |
| Patient Education Issues (PEI) | 3.82 | 94 | 9 | 0.87 |
| Ownership & Accountability Issues (OAI) | 2.77 | 103 | 10 | 0.77 |
| Process of Care Issues (PCI) | 2.59 | 101 | 6 | 0.81 |
| IT-Related Issues (ITRI) | 4.39 | 96 | 9 | 0.88 |
| Workforce Training Issues (WTI) | 3.21 | 91 | 6 | 0.86 |
| Workflow Issues (WI) | 1.32 | 94 | 3 | 0.71 |
| Resource Issues (RI) | 0.88 | 97 | 3 | 0.56 |
| Documentation Issues (DI) | 0.87 | 92 | 2 | 0.65 |
Table 4A shows results of the Index ANOVA Analysis by unit and professional affiliation. The results showed no statistically significant differences (at the 5% significance level), in importance-rating by unit affiliation for any of the 6 indexes. However, the results were mixed by professional affiliation. While there were no statistically significant differences, in importance-rating by professional affiliation, for two indexes, CCI and PEI; there were some statistically significant differences for the four remaining indexes, OAI, PCI, ITRI, and WTI.
Table 4A.
Index ANOVA Analysis by Unit Affiliation and Professional Affiliation
| CCI-Index | PEI-Index | OAI-Index | PCI-Index | ITRI-Index | WTI-Index | |
|---|---|---|---|---|---|---|
| Index by Unit Affiliation (UA) | ||||||
| Number of observations | 93 | 92 | 100 | 96 | 91 | 87 |
| F-Statistic | 1.74 | 0.82 | 2.13 | 1.00 | 0.60 | 1.46 |
| P-value | 0.15 | 0.52 | 0.14 | 0.41 | 0.66 | 0.22 |
| Degrees of Freedom | 4 | 4 | 4 | 4 | 4 | 4 |
| Index by Professional Affiliation (PA) | ||||||
| Number of observations | 97 | 94 | 102 | 101 | 96 | 91 |
| F-Statistic | 1.90 | 0.71 | 2.83 | 2.56 | 3.72 | 3.36 |
| P-value | 0.12 | 0.62 | 0.02* | 0.03* | 0.00* | 0.01* |
| Degrees of Freedom | 5 | 5 | 5 | 5 | 5 | 5 |
Statistically Significant at 5% Level
Table 4B shows the results of Post-ANOVA regression analysis for the four significant indexes by professional affiliation. These results help understand which practitioner groups differed significantly from the base category of Internal Medicine Physicians. For example, results for OAI-index indicate that nurses and pharmacists rated issues with higher importance compared to Internal Medicine physicians, whereas, results for ITRI-index indicate that Family Medicine and Hospitalist physicians rated issues with lower importance compared to Internal Medicine physicians; and for the WTI-index, Family Medicine physicians rated issues with lower importance compared to Internal Medicine physicians.
Table 4B.
Post-ANOVA Regression Analysis of Significant Indexes by Professional Affiliation
| Coef. | Std. Err. | t | P-value | ||
|---|---|---|---|---|---|
| OAI Index | |||||
| Family Medicine Physician | 0.06 | 0.31 | 0.18 | 0.86 | |
| Cardiology Physician | 0.30 | 0.37 | 0.81 | 0.42 | |
| Hospitalist Physician | 0.04 | 0.36 | 0.11 | 0.92 | |
| Nursing | 0.77 | 0.28 | 2.74 | 0.01* | |
| Pharmacy | 0.59 | 0.29 | 1.98 | 0.05* | |
| Cons | −0.39 | 0.23 | −1.67 | 0.10 | |
| R-square | 0.1283 | ||||
| PCI Index | |||||
| Family Medicine Physician | −0.35 | 0.32 | −1.11 | 0.27 | |
| Cardiology Physician | 0.15 | 0.36 | 0.43 | 0.67 | |
| Hospitalist Physician | −0.43 | 0.36 | −1.19 | 0.24 | |
| Nursing | 0.45 | 0.28 | 1.61 | 0.11 | |
| Pharmacy | −0.05 | 0.30 | −0.17 | 0.87 | |
| Cons | −0.04 | 0.23 | −0.16 | 0.87 | |
| R-square | 0.1186 | ||||
| ITRI-Index | |||||
| Family Medicine Physician | −1.06 | 0.34 | −2.15 | 0.01* | |
| Cardiology Physician | −0.15 | 0.39 | −0.40 | 0.69 | |
| Hospitalist Physician | −0.76 | 0.37 | −2.03 | 0.04* | |
| Nursing | −0.17 | 0.30 | −0.58 | 0.56 | |
| Pharmacy | 0.02 | 0.32 | 0.06 | 0.95 | |
| Cons | 0.31 | 0.25 | 1.25 | 0.22 | |
| R-square | 0.1714 | ||||
| WTI-Index | |||||
| Family Medicine Physician | −0.74 | 0.35 | −2.12 | 0.04* | |
| Cardiology Physician | −0.05 | 0.39 | −0.12 | 0.91 | |
| Hospitalist Physician | −0.20 | 0.38 | −0.52 | 0.61 | |
| Nursing | 0.30 | 0.31 | 0.97 | 0.34 | |
| Pharmacy | 0.39 | 0.33 | 1.19 | 0.24 | |
| Cons | −0.03 | 0.26 | −0.11 | 0.91 | |
| R-square | 0.1652 | ||||
Statistically Significant at 5% Level
Professional Affiliation Base (Excluded) Category: Internal Medicine Physician
To identify the specific issue-items within the indexes where these differences occurred, we performed an ANOVA analysis by issue-item for the four indexes. This analysis revealed a total of 7 issue-items showing significant differences by professional affiliation, including two in the OAI issue-category (OAI-1 and OAI-4); one in PCI (PCI-6); two in ITRI (ITRI-4 and ITRI-6); and one in WTI (WTI-2 and WTI-3). Further analysis of the actual importance-ratings for these issue-items revealed that nurses and pharmacists had a higher proportion of respondents rating the two OAI issues as “Extremely Important” compared to a higher proportion of Internal Medicine physicians rating them as “Important.” Similarly, for the ITRI and WTI issue-items, the differences boiled down to a higher proportion of Hospitalists and/or Family Medicine physicians rating these issues as “Important” compared to a higher proportion of Internal Medicine physicians rating them as “Extremely Important.” In summary, although the rating differences by professional affiliation were statistically significant for a small number of issue-items, they were not practically meaningful.
The analysis of survey results concluded with a review of open-ended comments received from respondents. We received several comments that served to corroborate the various issue-items related to EHR MedRec included on the survey. Importantly, the comments helped to verify that no additional issue items related to EHR MedRec (not included on the survey), were identified by respondents. This in turn, served to reinforce the gleaning that the mixed-method approach had indeed served the purpose of identifying a comprehensive set of issues related to EHR MedRec encountered by multiple practitioner groups at AU Health.
Discussion
The issues identified in this study related to EHR MedRec, shed light on not only the complexities inherent in clinical transitions-of-care in the MedRec process, but also the complexities arising from practitioners’ interaction with the EHR system, or socio-technical challenges in implementing EHR MedRec at the study institution. In regard to the latter, the results suggest that socio-technical challenges may be a “cross-cutting” theme across a majority of issue-categories. To provide an example of an issue-item under the core issue category of “Ownership & Accountability” with an added socio-technical dimension, it would be useful to consider the issue of “not taking” meds not being discontinued at discharge (OAI-2). Currently, the socio-technical dimension to the issue is that the “not taking” information is not visible on the active medication list within the EHR system. However, even if this issue were to be addressed through EHR system redesign (to facilitate provider access to this information on the active medication list), the core issue of “Ownership & Accountability” could persist on the part of the treatment provider, in deciding whether or not to use the information to modify the medication list. There may be resistance on the part of providers to discontinue a “not taking” medication, simply because they did not originally order it. This helps illustrate how socio-technical challenges could create an added layer of complexity to issues related to EHR MedRec unearthed by this study, making it a cross-cutting theme across several issue categories.
Additionally, regardless of whether or not there were statistically significant differences in importance-rating by professional affiliation, the full stock of issues related to EHR MedRec unearthed by this study, are reflective of a central theme, i.e., the absence of shared understanding across multiple practitioner groups, including:
Absence of shared understanding of what the responsibilities are of each practitioner group in the MedRec process. For example, admitting providers are not clear on who does what in in the medication history and admission process.
Absence of shared understanding of how the EHR MedRec system is being used by other clinicians. For example, outpatient subspecialists are not convinced that MedRec marked as complete in the system at the time of hospital discharge translates to a complete and accurate medication list.
Absence of shared understanding of the why, i.e., the value of EHR MedRec in preventing discrepancies and promoting patient safety. For example, outpatient providers expressed the concern that inpatient clinicians may not realize the importance of ensuring a medication list that is free of discrepancies at discharge, to enable patients to effectively transition into the community.
Practice Implications
The results of this study provide substantive implications for practice by providing insight into:
Best practices for managing clinical transitions of care in the EHR MedRec process; and
Best practices for managing socio-technical challenges in EHR MedRec implementation.
In regard to the former, the study suggests that clinical transitions-of-care in the EHR MedRec process could be effectively managed by creating shared understanding of the process for MedRec and responsibilities for each step of the process among all practitioner (stakeholder) groups involved in the EHR MedRec process. Additionally, it would be important to create shared understanding of the value and importance of EHR MedRec in generating an accurate medication list to promote patient safety.
In regard to best practices for managing socio-technical challenges encountered in EHR MedRec implementation, the study helps understand the importance of concurrent attention to workflow redesign and EHR system redesign for addressing issues related to EHR MedRec. For example, one issue that surfaced under “Ownership & Accountability” was that physicians need to review nurses’ notes on compliance status to know whether a patient is “not taking” a medication, to decide whether or not to discontinue the medication at the time of discharge. This issue could be resolved by physicians and nurses taking ownership in redesigning the patient care workflow to include a compliance status check prior to completing MedRec. Likewise, the issue could also be addressed by redesigning the system to enable compliance status to be accessed within the medication list. However, even after system redesign, the “Ownership & Accountability” issue might persist, for example, a physician may resist discontinuing a “not taking” medication if they did not previously order it. Nevertheless, this example highlights how improvements could be made through redesign of the workflow and/or the EHR system. It also suggests that improvements to both patient care workflow and the EHR system may need to go hand-in-hand to facilitate meaningful use and successful implementation of EHR MedRec.
Conclusion
This paper describes the results of a study that sought to identify a comprehensive set of issues related to EHR MedRec from multiple practitioner groups at a health system. There were two key lessons learned from the study: 1) there was a socio-technical dimension to all issues related to EHR MedRec unearthed by the study, creating an added layer of complexity; and 2) there was an absence of shared understanding among practitioners in regard to the value of EHR MedRec in promoting patient safety, which in turn, led to workarounds and suboptimal use of the EHR MedRec system. Results provide insights into best practices for managing both: 1) clinical transitions-of-care in the EHR MedRec process; and 2) socio-technical challenges encountered in EHR MedRec implementation. Taken together, the results suggest that strategies and interventions seeking to concurrently: 1) enable shared understanding of the value of EHR MedRec across practitioner groups; and 2) address socio-technical challenges through workflow and system redesign, by way of practitioner/stakeholder engagement, may be most effective for promoting meaningful use and successful implementation of EHR MedRec in healthcare organizations.
Acknowledgements:
The authors wish to thank the senior leadership, staff, and clinicians at AU Health for their support & collaboration in enabling the research team to conduct this study. We are also grateful to AHRQ for providing funding support for this project.
Funding support: This study was supported by grant number R21HS024335 from the Agency for Healthcare Research and Quality (AHRQ).
Source of Funding: The authors’ study institution (Augusta University) received funding for this project from AHRQ as indicated on the Title Page. Other than institutional receipt of funding for this project
Footnotes
IRB approval: The study was approved by the Institutional Review Board (IRB) at Augusta University. IRB approval was obtained prior to data collection.
Conflict-of-Interest the authors have no conflicts-of-interest to declare. Below is a COI summary for all authors listed on this study.
1. Pavani Rangachari None
2. Kevin C. Dellsperger None
3. David Fallaw None
4. Ian Davis None
5. Michael Sumner None
6. Walter Ray None
7. Shashana Fiedler None
8. Tran Nguyen None
9. R. Karl Rethemeyer None
References
- 1.AHRQ, Agency for Healthcare Research and Quality (2016). Patient safety primer: medication reconciliation https://psnet.ahrq.gov/primers/primer/1/medication-reconciliation; Accessed: October 15, 2016.
- 2.IOM, Institute of Medicine Committee on Identifying and Preventing Medication Errors, Aspden P, Wolcott J, Bootman JL, Cronenwett LR, eds. (2007). Preventing Medication Errors: Quality Chasm Series Washington, DC: The National Academies Press. [Google Scholar]
- 3.Mueller SK, Sponsler KC, Kripalani S, Schnipper JL (2012). Hospital-based medication reconciliation practices: a systematic review. Archives of Internal Medicine, 172:1057–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burton R (2012). Health Policy Brief: Improving Care Transitions,” Health Affairs http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=76.
- 5.Coleman EA (2003). Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs; Journal of the American Geriatrics Society, 51(4): 549–55. [DOI] [PubMed] [Google Scholar]
- 6.Pronovost P, Weast B, Schwarz M, Wyskiel RM, Prow D, Dorman T, Lipsett P (2003). Medication reconciliation: a practical tool to reduce the risk of medication errors. Journal of Critical Care, 18:201–205. [DOI] [PubMed] [Google Scholar]
- 7.Barnsteiner JH (2008). Medication Reconciliation. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Clinicians Rockville (MD): Agency for Healthcare Research and Quality (US); Chapter 38 Available from: http://www.ncbi.nlm.nih.gov/books/NBK2648/ [PubMed] [Google Scholar]
- 8.Greenwald JL, Halasyamani L, Greene J, LaCivitta C, Stucky E, Benjamin B, Reid W, Griffin FA, Vaida AJ, Williams MV. (2010). Making inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. Journal of Hospital Medicine, 5(8):477–485. [DOI] [PubMed] [Google Scholar]
- 9.CMS Centers for Medicare and Medicaid Services (2012). Stage 2 Eligible Professional Meaningful Use Core Measures Measure 14 of 17 https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/Stage2_EPCore_14_MedicationReconciliation.pdf
- 10.HealthIT.Gov. (2014). Achieving Meaningful Use Stage 2: Medication Reconciliation; https://www.healthit.gov/providers-professionals/achieve-meaningful-use/core-measures-2/medication-reconciliation
- 11.Boockvar KS, Santos SL, Kushniruk A, Johnson C, Nebeker JR (2011). Medication reconciliation: barriers and facilitators from the perspectives of physicians and pharmacists. Journal of Hospital Medicine, 6:329–337. [DOI] [PubMed] [Google Scholar]
- 12.Sanchez HS, Sadie SS, Santos SL, Boockvar K (2014). Implementing medication reconciliation from the planner’s perspective: a qualitative study. BMC Health Services Research, 14:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grossman J, Gourevitch R, Cross DA (2014). Hospital experiences using electronic health records to support medication reconciliation. National Institute for Healthcare Reform (NIHCR) Research Brief Number 17
- 14.Rangachari P (2010). Overcoming the Unintended Adverse Consequences of Implementing Health IT through Human Resource and Knowledge Management. In Blair JD, Fottler MD, and Savage GT (Eds.), Strategic Human Resource Management in Health Care, Advances in Health Care Management, Volume 9, pp. 163–194. Bingley, UK: Emerald. [Google Scholar]
- 15.Rangachari P (2016). Role of Social Knowledge Networking Technology in facilitating meaningful use of Electronic Health Record medication reconciliation. Journal of Hospital Administration, 5(3): 98–106. 10.5430/jha.v5n3p98.PMCID:5690564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clay BJ, Halasyamani L, Stucky ER, Greenwald JL, Williams MV (2008). Results of a medication reconciliation survey from the 2006 Society of Hospital Medicine National Meeting. Journal of Hospital Medicine, 3(6):465–472. [DOI] [PubMed] [Google Scholar]
- 17.Rose AJ, Fischer SH, Pasche-Orlow MK (2017). Beyond Medication Reconciliation: The Correct Medication List. Journal of the American Medical Association; 317(20):2057–2058. doi: 10.1001/jama.2017.4628. [DOI] [PubMed] [Google Scholar]
- 18.Van Sluisveld N, Zegers M, Natsch S, Wollersheim H (2012). Medication reconciliation at hospital admission and discharge: insufficient knowledge, unclear task reallocation and lack of collaboration as major barriers to medication safety. BMC Health Services Research, 12:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Creswell J (2015). A Concise Introduction to Mixed-Methods Research; SAGE Publications Inc., Thousand Oaks, CA: ISBN: 9781483359045. [Google Scholar]
- 20.Braun V and Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology, 3 (2). pp. 77–101. [Google Scholar]
- 21.Elo S, Kyngas H (2007). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107Y115. [DOI] [PubMed] [Google Scholar]
- 22.Pope C, Ziebland S,Mays N (2000). Qualitative research in health care: Analyzing qualitative data. British Medical Journal, 320, 114Y116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schneeweiss H, Mathes H (1995). Factor analysis and principal components; Journal of Multivariate Analysis; 55: 105–124. [Google Scholar]
- 24.DeVellis RF (2012). Scale development: Theory and applications Los Angeles: SAGE; pp. 109–110. [Google Scholar]
- 25.Cortina JM (1993). What is coefficient alpha? An examination of theory and applications. Journal of Applied Psychology; 78: 98–104. [Google Scholar]


