Abstract
Williams syndrome (WS) is a clinical condition, involving cognitive deficits and an uneven language profile, which has been the object of intense inquiry over the last decades. Although WS results from the hemideletion of around two dozen genes in chromosome 7, no gene has yet been probed to account for, or contribute significantly to, the language problems exhibited by the affected people. In this paper we have relied on gene expression profiles in the peripheral blood of WS patients obtained by microarray analysis and show that several robust candidates for language disorders and/or for language evolution in the species, all of them located outside the hemideleted region, are up- or downregulated in the blood of subjects with WS. Most of these genes play a role in the development and function of brain areas involved in language processing, which exhibit structural and functional anomalies in people with this condition. Overall, these genes emerge as robust candidates for language dysfunction in WS.
Keywords: Williams syndrome, blood transcriptional profile, language disorders, language evolution, candidate genes
Introduction
Williams syndrome (WS) is a clinical condition resulting from a hemizygous deletion of 1.5 to 1.8 Mb on 7q11.23, which encompasses nearly 30 genes (Korenberg et al., 2000; Pober et al., 2010). The affected people exhibit a distinctive behavioral and cognitive profile, with enhanced sociability, mental retardation, impaired spatial cognition, and spared musical abilities (Reilly et al., 1990; Udwin and Yule, 1991; Bellugi et al., 1999; Galaburda et al., 2002; Levitin et al., 2005). Language abilities are significantly preserved in people with WS compared to other neurodevelopmental disorders, to the extent that this syndrome has often been used to support the view that language can be teased apart from other aspects of cognition. Nonetheless, recent, fine-grained analyses of WS language have concluded that WS language is delayed or impaired across different levels compared to the neurotypical population (Karmiloff-Smith and Mills, 2006; Brock, 2007; Mervis and Becerra, 2007; Martens et al., 2008 for good reviews). Specifically, children with WS experience problems with irregular word forms and complex syntax; likewise, they have problems with word definitions, although they usually excel on expressive vocabulary (including semantic organization and fluency) (Volterra et al., 1996; Mervis et al., 1999; Purser et al., 2011; Van Den Heuvel et al., 2016; see Mervis and Becerra, 2007 for discussion). However, as with other aspects of the cognitive profile of this condition, no robust gene-to-phenotype associations have been established in the language domain. To date, the most promising candidates for language dysfunction in WS are GTF2I, BAZ1B, and LIMK1. In particular, GTF2I, which encodes a regulator of transcription, has been repeatedly related to the behavioral and cognitive disabilities that are typically found in this condition and that have an impact on language function (Morris et al., 2003; Tassabehji et al., 2005; Sakurai et al., 2011; Hoeft et al., 2014). Its adjacent paralog, GTF2IRD1, has been related to altered vocalizations among other features (Howard et al., 2012). Interestingly too, BAZ1B haploinsufficiency explains almost 50% of transcriptional dysregulation in WS neurons, with BAZ1B target genes being enriched in functions related to neurogenesis and neuron differentiation (Lalli et al., 2016). Regarding LIMK1, it regulates synaptic plasticity and long-term memory (Todorovski et al., 2015), and its hemideletion has been hypothesized to account for the observed deficits in spatial cognition in combination with other genes (Gray et al., 2006; Smith et al., 2009). Still, these potential links with aspects of language (dys)function seem quite vague, particularly if one considers our remarkable understanding of the genetic underpinnings of human language, language disorders, and language evolution (see Scharff and White, 2004; Li and Bartlett, 2012; Benítez-Burraco, 2013; Graham et al., 2015; Fisher, 2017; Murphy and Benítez-Burraco, 2017, 2018 for reviews). Examining how robust candidate genes for language disorders and language evolution behave in people with WS should help refine our view of the molecular causes of the language deficits attested in this condition. One general reason supporting this approach is the deep link that exists between evolution and (abnormal) development, in the spirit of evo-devo theories. One specific reason supporting this approach is that although in WS the number of hemideleted genes is small, changes in the dosage of hundreds, or even thousands, of other genes can be expected, with a potential impact on language abilities, in the spirit of omnigenic theories of complex diseases (Boyle et al., 2017; Peedicayil and Grayson, 2018). Recently Kimura et al. (2018) confirmed that the dysregulation of several co-expression modules involving dozens of genes outside of the 7q11.23 region seemingly accounts for the complex phenotypes observed in WS patients. Importantly, they found BCL11A, a gene associated with speech disorders, among the hub genes in the top WS-related modules.
In this paper we have conducted a more focused research on the potential dysregulation of genes related to language outside the WS region as a possible explanation of the distinctive language profile of the affected people. Similarly to Kimura et al. (2018), we have relied on gene expression profiles in peripheral blood of WS patients obtained by microarray analysis. We have found that significant differences exist in the blood of subjects with WS compared to neurotypical controls in the expression levels of robust candidates for language development, language evolution, and language impairment.
Methods
The list of core candidates for language (abnormal) development and language evolution (Supplementary Table S1) encompasses two subsets of genes. The first subset consists of strong candidates for language disorders, in particular, developmental dyslexia (DD) and specific language disorder (SLI), as listed by Paracchini et al. (2016), Pettigrew et al. (2016) and Chen et al. (2017). The second subset consists of strong candidates for language evolution, as compiled by Boeckx and Benítez-Burraco (2014a,b) and Benítez-Burraco and Boeckx (2015). These are genes involved in the globularization of the human skull/brain and the cognitive changes accounting for our species-specific ability to learn and use languages (aka our language- readiness). Overall, the genes comprising this second subset fulfill several criteria. First, they have changed (and/or interact with genes that have changed) after our split from Neanderthals/Denisovans, including changes in their coding regions and/or their epigenetic profile. Second, they play some known role in brain development, regionalization, wiring, and/or function. Third, they are candidates for language dysfunction in broad cognitive disorders, particularly, autism spectrum disorder (ASD) and schizophrenia (SZ) (see Benítez-Burraco and Murphy, 2016; Murphy and Benítez-Burraco, 2016, 2017 for details about their role in language processing).
The gene expression profiling data of peripheral blood were obtained from our previous study (Kimura et al., 2018), available at the Gene Expression Omnibus (GSE89594). Briefly, total RNA from 32 WS patients and 30 healthy controls were analyzed using an Agilent Human GE v2 8×60K Microarray (Agilent Technologies). After the normalization step, differentially expressed genes (DEG) were calculated using the Limma R package (Smyth, 2005). The Benjamini-Hochberg method was used to evaluate the false discovery rate (FDR) (Benjamini and Hochberg, 1995). DEG were defined as FDR < 0.05 and the |fold change (FC)| > 1.2. Gene list enrichment analysis was performed using Fisher’s exact test. All the expressed genes were used as the background gene list.
Results
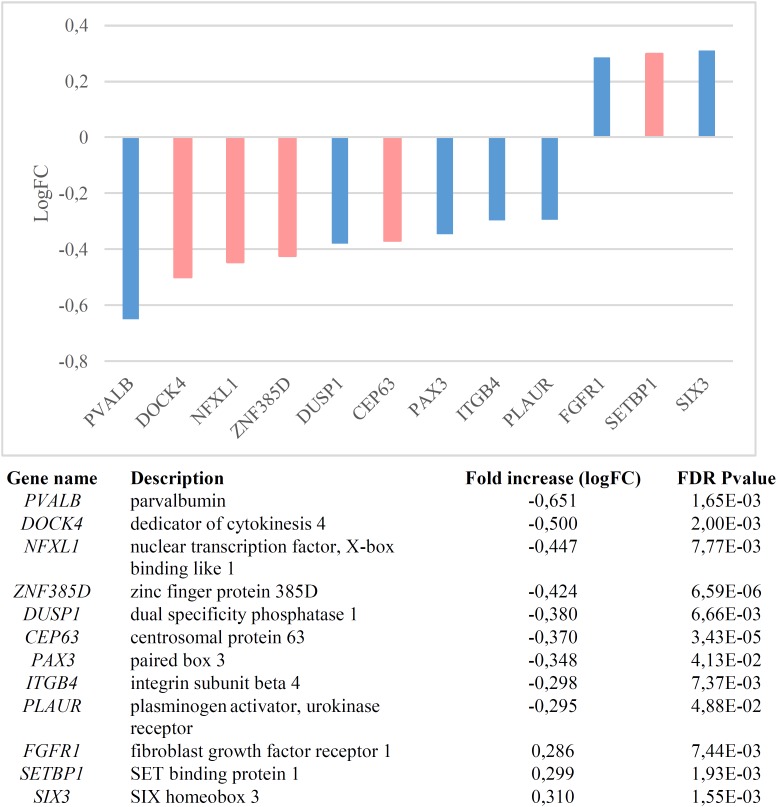
We found that candidates for language (abnormal) development and language evolution are significantly dysregulated in the blood of subjects with WS (p = 1.1e-7 by Fisher’s exact test). Figure 1 shows the genes that are significantly up- or down-regulated compared to controls (FDR < 0.05, |FC| > 1.2).
FIGURE 1.
Genes significantly dysregulated in the blood of subjects with WS (FDR < 0.05, |FC| > 1.2). Candidate genes for language disorders (SLI, DD) are displayed in light red, whereas candidates for language evolution are colored in light blue.
In order to check the specificity of this set of genes in relation to language we conducted a functional enrichment analysis with Enrichr (amp.pharm.mssm.edu/Enrichr; Chen et al., 2013; Kuleshov et al., 2016), which showed that they are significantly related to biological processes, molecular functions, and abnormal phenotypes of interest for language (Table 1). Finally, these genes were predicted to be preferentially expressed in body parts important for language processing or for language development, particularly, the cerebellum and the thalamus (Table 1 and Supplementary Table S2). We now provide a detailed discussion of our results.
Table 1.
Functional enrichment analysis according to Enrichr of the set of genes significantly dysregulated in the blood of subjects with WS.
| Index | Name | P-value | Adjusted p-value | Combined Z-score | score |
|---|---|---|---|---|---|
| GO Biological Process 2018 | |||||
| 1 | Regulation of endothelial cell chemotaxis to fibroblast growth factor (GO:2000544) | 0.004791 | 0.04609 | −3.72 | 19.88 |
| 2 | Regulation of mitotic spindle checkpoint (GO:1903504) | 0.004193 | 0.04609 | −3.57 | 19.54 |
| 3 | Positive regulation of vascular endothelial cell proliferation (GO: 1905564) | 0.005985 | 0.04609 | −3.47 | 17.74 |
| 4 | Negative regulation of meiotic cell cycle (GO:0051447) | 0.004193 | 0.04609 | −3.21 | 17.58 |
| 5 | Positive regulation of smooth muscle cell migration (GO:0014911) | 0.006582 | 0.04609 | −3.48 | 17.49 |
| 6 | Embryonic camera-type eye morphogenesis (GO:0048596) | 0.004193 | 0.04609 | −2.98 | 16.34 |
| 7 | Attachment of GPI anchor to protein (GO:0016255) | 0.004791 | 0.04609 | −2.95 | 15.76 |
| 8 | Regulation of MAP kinase activity (GO:0043405) | 0.001228 | 0.04609 | −2.13 | 14.28 |
| 9 | Regulation of neuroblast proliferation (GO: 1902692) | 0.006582 | 0.04609 | −2.83 | 14.20 |
| 10 | Mesodermal cell differentiation (GO:0048333) | 0.005985 | 0.04609 | −2.71 | 13.87 |
| GO Molecular Function 2018 | |||||
| 1 | MAP kinase tyrosine/serine/threonine phosphatase activity (GO:0017017) | 0.004791 | 0.07352 | −3.07 | 16.41 |
| 2 | MAP kinase phosphatase activity (GO:0033549) | 0.005985 | 0.07352 | −2.64 | 13.51 |
| 3 | Transcription corepressor binding (GO:0001222) | 0.007774 | 0.07352 | −2.38 | 11.56 |
| 4 | Insulin-like growth factor binding (GO:0005520) | 0.008965 | 0.07352 | −2.18 | 10.27 |
| 5 | Insulin-like growth factor I binding (GO:0031994) | 0.008370 | 0.07352 | −2.10 | 10.02 |
| 6 | Protein tyrosine kinase binding (GO: 1990782) | 0.02901 | 0.08271 | −2.70 | 9.55 |
| 7 | Transcription cofactor binding (GO:0001221) | 0.01549 | 0.08271 | −2.29 | 9.54 |
| 8 | Receptor tyrosine kinase binding (GO:0030971) | 0.02374 | 0.08271 | −2.35 | 8.80 |
| 9 | Phosphatidylinositol kinase activity (GO:0052742) | 0.03077 | 0.08271 | −2.28 | 7.93 |
| 10 | Fibroblast growth factor binding (GO:0017134) | 0.01372 | 0.08271 | −1.84 | 7.88 |
| GO Cellular Component 2018 | |||||
| 1 | Specific granule membrane (GO:0035579) | 0.05384 | 0.2061 | −1.87 | 5.47 |
| 2 | Spindle pole (GO:0000922) | 0.06293 | 0.2061 | −1.79 | 4.95 |
| 3 | Centriole (GO:0005814) | 0.05612 | 0.2061 | −1.53 | 4.40 |
| 4 | Nucleolus (GO:0005730) | 0.06032 | 0.2061 | −1.54 | 4.33 |
| 5 | Specific granule (GO:0042581) | 0.09246 | 0.2133 | −1.57 | 3.74 |
| 6 | Microtubule organizing center part (GO:0044450) | 0.07361 | 0.2061 | −1.40 | 3.64 |
| MGI Mammalian Phenotype 2017 | |||||
| 1 | MP:0002151_abnormal_neural_tube_morphology | 0.0001029 | 0.009725 | −3.34 | 30.71 |
| 2 | MP:0011089_perinatal_lethality,_complete_penetrance | 0.0002578 | 0.01392 | −3.68 | 30.40 |
| 3 | MP:0012138_decreased_forebrain_size | 0.00003942 | 0.007070 | −2.67 | 27.06 |
| 4 | MP:0002950_abnormal_neural_crest_cell_migration | 0.00003942 | 0.007070 | −2.48 | 25.10 |
| 5 | MP:0010378_increased_respiratory_quotient | 0.0002542 | 0.01392 | −2.77 | 22.94 |
| 6 | MP:0003864_abnormal_midbrain_development | 0.0001725 | 0.01304 | −2.45 | 21.19 |
| 7 | MP:0000733_abnormal_muscle_development | 0.00005611 | 0.007070 | −2.11 | 20.66 |
| 8 | MP:0005221_abnormal_rostral-caudal_axis_patterning | 0.0005171 | 0.02443 | −2.55 | 19.29 |
| 9 | MP:0005602_decreased_angiogenesis | 0.0006517 | 0.02463 | −2.56 | 18.75 |
| 10 | MP:0002111_abnormal_tail_morphology | 0.0006517 | 0.02463 | −2.47 | 18.08 |
| Human Phenotype Ontology | |||||
| 1 | Malar flattening (HP:0000272) | 0.00000345 5 | 0.0008259 | −2.42 | 30.38 |
| 2 | Midface retrusion (HP:0011800) | 0.00000611 8 | 0.0008259 | −2.02 | 24.26 |
| 3 | Camptodactyly of finger (HP:0100490) | 0.00004567 | 0.001761 | −2.26 | 22.60 |
| 4 | Choanal stenosis (HP:0000452) | 0.00003450 | 0.001553 | −2.15 | 22.14 |
| 5 | Shallow orbits (HP:0000586) | 0.00002171 | 0.001553 | −2.02 | 21.67 |
| 6 | Ureteral obstruction (HP:0006000) | 0.00003450 | 0.001553 | −2.08 | 21.39 |
| 7 | Short nose (HP:0003196) | 0.00007989 | 0.002546 | −2.26 | 21.32 |
| 8 | Ureteral stenosis (HP:0000071) | 0.00002991 | 0.001553 | −2.01 | 20.93 |
| 9 | Heterogeneous (HP:0001425) | 0.00008487 | 0.002546 | −2.14 | 20.06 |
| 10 | Depressed nasal bridge (HP:0005280) | 0.0002981 | 0.007161 | −2.37 | 19.20 |
| Jensen TISSUES | |||||
| 1 | Ectoderm | 0.00006469 | 0.005546 | −4.15 | 39.98 |
| 2 | Cranium | 0.00007203 | 0.005546 | −4.00 | 38.17 |
| 3 | Retina | 0.008991 | 0.09231 | −7.36 | 34.68 |
| 4 | Adult | 0.01554 | 0.09772 | −6.50 | 27.05 |
| 5 | Neural crest | 0.002981 | 0.06593 | −4.14 | 24.10 |
| 6 | Somite | 0.0005354 | 0.02749 | −3.08 | 23.19 |
| 7 | Bud | 0.001676 | 0.05163 | −3.59 | 22.95 |
| 8 | Mesenchyme | 0.01050 | 0.09772 | −5.01 | 22.84 |
| 9 | Myoblast | 0.001550 | 0.05163 | −3.53 | 22.83 |
| 10 | Immune system | 0.02200 | 0.1019 | −5.91 | 22.56 |
Only the top-10 functions have been included (whenever available). The p-value was computed using Fisher’s exact test. The adjusted p-value was computed using the Benjamini-Hochberg method for correction for multiple hypotheses testing. The z-score was computed using a modification to Fisher’s exact test and assess the deviation from the expected rank. Finally, the combined score is a combination of the p-value and z-score calculated by multiplying the two scores (combined score = ln(p-value) ∗ z-score). This combined score provides a compromise between both methods and it is claimed to report the best rankings when compared with the other scoring schemes. See http://amp.pharm.mssm.edu/Enrichr/help#background&q=5 for details.
Discussion
Functional Characterization of Individual Genes
Nearly one third of the language-related genes found downregulated in the blood of subjects with WS are candidates for DD (DOCK4, ZNF385D, and CEP63) and/or for SLI (DOCK4, NFXL1). As other members of the Dock family, DOCK4 regulates cytoskeleton assembly and cell adhesion and migration (Gadea and Blangy, 2014). Specifically, DOCK4 has been shown to be involved in neuronal migration and neurite differentiation (Ueda et al., 2008; Xiao et al., 2013), via interaction with the actin-binding protein cortactin (Ueda et al., 2013). Knockdown of Dock4 in mice abolishes commissural axon attraction by Shh (Makihara et al., 2018). The gene has been related to neuronal migration and neurite outgrowth anomalies linked to DD (Shao et al., 2016), although it is also associated with ASD (Pagnamenta et al., 2010) and SZ (Alkelai et al., 2012). GWAs have associated markers in ZNF385D to the co-occurrence of reading disability and language impairment (Eicher et al., 2013), but also to negative symptoms in SZ (Xu et al., 2013). CEP63 is required for normal spindle assembly, being involved in maintaining centriole number and establishing the order of events in centriole formation (Brown et al., 2013). Besides its association with DD (Einarsdottir et al., 2015), the gene is also a candidate for primary microcephaly (Marjanović et al., 2015), a feature that is commonly found in subjects with WS (Jernigan and Bellugi, 1990; Schmitt et al., 2001; Thompson et al., 2005; Jackowski et al., 2009). Finally, variants of NFXL1, which is predicted to encode a transcription factor, confer a risk for SLI (Villanueva et al., 2015). The gene is highly expressed in the cerebellum (Nudel, 2016).
Regarding the candidates for language evolution that we have found downregulated in the blood of subjects with WS, DUSP1 is involved in vocal learning in songbirds (Horita et al., 2010, 2012). PVALB encodes a calcium-binding protein that is structurally and functionally similar to calmodulin and that is involved in hippocampal plasticity, learning and memory (Donato et al., 2013). Interestingly enough, the inactivation of Pvalb-expressing interneurons in the auditory cortex alters response to sound, strengthening forward suppression and altering its frequency dependence (Phillips et al., 2017). Inhibition of PVALB-expressing GABAergic interneurons results in complex behavioral changes related to the behavioral phenotype of people with SZ (Brown et al., 2015). Importantly, some of the key changes that contributed to the emergence of our language-readiness involved GABAergic signaling (discussed in detail in Boeckx and Benítez-Burraco, 2014b), which are vital for oscillatory processes underlying language processing (Bae et al., 2010; see Murphy and Benítez-Burraco, 2018 for details). Reduction in PVALB expression in interneurons has also been found in mouse models of ASD (Filice et al., 2016), specifically, in the Cntnap2-/- model (Lauber et al., 2018). CNTNAP2 is a direct target of FOXP2, the renowned “language gene” (Vernes et al., 2008; Adam et al., 2017), and regulates language development in non-pathological populations too (Whitehouse et al., 2011; Whalley et al., 2011, Kos et al., 2012). Also mice lacking PLAUR have significantly fewer neocortical parvalbumin-containing GABAergic interneurons, with this reduction correlating with impaired social interactions (Bruneau and Szepetowski, 2011). PLAUR is a target of FOXP2 too (Roll et al., 2010), but also an effector of SRPX2, another of FOXP2’s targets (Royer-Zemmour et al., 2008) and a candidate for speech dyspraxia (Roll et al., 2006). Concerning PAX3, this gene is expressed in the neural crest and is a candidate for Waardenburg syndrome, a clinical condition entailing sensorineural hearing loss and developmental delay (Tassabehji et al., 1992; Chen et al., 2010). Finally, ITGB4 encodes the integrin beta 4 subunit, a receptor for the laminins, including FLNA (Travis et al., 2004), an actin-binding protein needed for cytoskeleton remodeling and neuronal migration (Fox et al., 1998) FLNA binds CMIP (Fox et al., 1998), a candidate for SLI (Newbury et al., 2009). Interestingly enough, ITGB4 is one of the proteins bearing fixed changes in humans compared to extinct hominins (Pääbo, 2014; Supplementary Table S1).
Lastly, among the genes found to be upregulated in the blood on WS subjects, we found the SLI candidate SETBP1, as well as FGFR1 and SIX3. SETBP1 is also a candidate for Schinzel-Giedion syndrome, a clinical condition entailing occasional epilepsy and severe developmental delay (Ko et al., 2013; Miyake et al., 2015). Mutations on this gene have been associated as well to behavioral and social deficits (Coe et al., 2014). The Integrative Nuclear FGFR1 Signaling (INFS) has been hypothesized to be one of the neurodevelopmental pathways on which multiple SZ candidates converge, regulating numerous neurotransmitter systems and neural circuits (Stachowiak et al., 2013). Finally, SIX3 contributes to regulate the relative size of the telencephalon versus the thalamus (Lavado et al., 2008; Sylvester et al., 2010). Interestingly, Six3 regulates Shh (Jeong et al., 2008), one robust candidate for microcephaly that has been positively selected in the human lineage (Dorus et al., 2004), but it also interacts with several genes relevant for our language-ready brain (Benítez-Burraco and Boeckx, 2015).
Functional Characterization of the Set of Dysregulated Genes
The results of our functional enrichment analyses (Table 1) show that the language-related genes that are dysregulated in the blood of people with WS mainly contribute to the cytoskeleton activity, being significantly involved in cell proliferation and migration, including neuroblast proliferation. Regarding their molecular function, they typically participate in protein modification, particularly via (tyrosine) kinase phosphatase and (tyrosine) kinase binding activities, but also in gene regulation, via transcription cofactor binding. Interestingly, these genes are significantly associated to aberrant processes impacting on brain development, like abnormal neural tube morphology and neural crest cell migration, as well as decreased forebrain size and abnormal midbrain development. Likewise, they are associated to clinical symptoms mostly impacting on craniofacial morphology, like malar flattening, midface retrusion, shallow orbits, or depressed nasal bridge. Finally, these genes are predicted to be preferentially expressed in the ectoderm, the cranium, the retina, and the neural crest. According to the Human Brain Transcriptome Database1 all these genes are expressed in the brain, particularly in the thalamus and the cerebellum (Supplementary Table S2). The thalamus functions as a sort of relay center to connect many brain areas involved in language processing (Wahl et al., 2008; Murdoch, 2010; David et al., 2011) and changes in the thalamus have been claimed to contribute to the evolutionary emergence of our language-ready brain (see Boeckx and Benítez-Burraco, 2014b for details). Similarly, the cerebellum plays a key role in language processing and is impaired in language-related pathologies (Vias and Dick, 2017; Mariën and Borgatti, 2018). People with WS exhibit cerebellar volume alterations that are seemingly associated with their cognitive, affective and motor distinctive features (Osório et al., 2014). In the same vein, the thalamus exhibits structural and functional differences with the neurotypical population, including disproportionately reduced volumes and decreased gray matter (Chiang et al., 2007; Campbell et al., 2009), as well as enhanced thalamic activity (Mobbs et al., 2007; Bódizs et al., 2012).
Conclusion
To conclude, it is true that deciphering the exact molecular causes of language dysfunction in WS is still pending, particularly, because at present none of the genes hemideleted in this condition has been demonstrated to play a central role in language processing. Nonetheless, in this paper we have shown that the genes that are dysregulated in subjects with WS are significantly enriched in core candidates for language disorders and language evolution. These genes emerge as robust candidates for language dysfunction in WS. Future research should try to delve into the expression patterns of these genes in the brain of people with WS, as well as into their role in neurotypical brain development. Likewise, altering these genes in animal models of WS should help gaining a better understanding of their biological role and ultimately, of their contribution to language dysfunction in WS.
Data Availability
Publicly available datasets were analyzed in this study. This data can be found here: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE89594.
Author Contributions
AB-B conceived and wrote the manuscript. RK conducted the expression studies and analyzed the data. Both authors contributed to manuscript revision, and read and approved the submitted version.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. This research was funded by the Spanish Ministry of Economy and Competitiveness [Grant FFI2016-78034-C2-2-P (AEI/FEDER, UE) to AB-B].
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2019.00258/full#supplementary-material
References
- Adam I., Mendoza E., Kobalz U., Wohlgemuth S., Scharff C. (2017). CNTNAP2 is a direct FoxP2 target in vitro and in vivo in zebra finches: complex regulation by age and activity. Genes Brain Behav. 16 635–642. 10.1111/gbb.12390 [DOI] [PubMed] [Google Scholar]
- Alkelai A., Lupoli S., Greenbaum L., Kohn Y., Kanyas-Sarner K., Ben-Asher E., et al. (2012). DOCK4 and CEACAM21 as novel schizophrenia candidate genes in the Jewish population. Int. J. Neuropsychopharmacol. 15 459–469. 10.1017/S1461145711000903 [DOI] [PubMed] [Google Scholar]
- Bae M. H., Bissonette G. B., Mars W. M., Michalopoulos G. K., Achim C. L., Depireux D. A., et al. (2010). Hepatocyte growth factor (HGF) modulates GABAergic inhibition and seizure susceptibility. Exp. Neurol. 221 129–135. 10.1016/j.expneurol.2009.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellugi U., Lichtenberger L., Mills D., Galaburda A., Korenberg J. R. (1999). Bridging cognition, the brain and molecular genetics: evidence from Williams syndrome. Trends Neurosci. 5 197–207. 10.1016/S0166-2236(99)01397-1 [DOI] [PubMed] [Google Scholar]
- Benítez-Burraco A. (2013). “Genetics of language: roots of specific language deficits,” in The Cambridge Handbook of Biolinguistics, eds Boeckx C., Grohmann K. K. (Cambridge: Cambridge University Press; ), 375–412. [Google Scholar]
- Benítez-Burraco A., Boeckx C. (2015). Possible functional links among brain- and skull-related genes selected in modern humans. Front. Psychol. 6:794. 10.3389/fpsyg.2015.00794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benítez-Burraco A., Murphy E. (2016). The oscillopathic nature of language deficits in autism: from genes to language evolution. Front. Hum. Neurosci. 10:120. 10.3389/fnhum.2016.00120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamini Y., Hochberg Y. (1995). Controlling the false discovery rate - a practical and powerful approach to multiple testing. J. R. Stat. Soc. Series B 57 289–300. 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- Bódizs R., Gombos F., Kovács I. (2012). Sleep EEG fingerprints reveal accelerated thalamocortical oscillatory dynamics in Williams syndrome. Res. Dev. Disabil. 33 153–164. 10.1016/j.ridd.2011.09.004 [DOI] [PubMed] [Google Scholar]
- Boeckx C., Benítez-Burraco A. (2014a). Globularity and language-readiness: generating new predictions by expanding the set of genes of interest. Front. Psychol. 5:1324. 10.3389/fpsyg.2014.01324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeckx C., Benítez-Burraco A. (2014b). The shape of the human language-ready brain. Front. Psychol. 5:282. 10.3389/fpsyg.2014.00282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle E. A., Li Y. I., Pritchard J. K. (2017). An expanded view of complex traits: from polygenic to omnigenic. Cell 169 1177–1186. 10.1016/j.cell.2017.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brock J. (2007). Language abilities in Williams syndrome: a critical review. Dev. Psychopathol. 19 97–127. 10.1017/S095457940707006X [DOI] [PubMed] [Google Scholar]
- Brown J. A., Ramikie T. S., Schmidt M. J., Báldi R., Garbett K., Everheart M. G., et al. (2015). Inhibition of parvalbumin-expressing interneurons results in complex behavioral changes. Mol. Psychiatry 20 1499–1507. 10.1038/mp.2014.192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown N. J., Marjanović M., Lüders J., Stracker T. H., Costanzo V. (2013). Cep63 and cep152 cooperate to ensure centriole duplication. PLoS One 8:e69986. 10.1371/journal.pone.0069986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruneau N., Szepetowski P. (2011). The role of the urokinase receptor in epilepsy, in disorders of language, cognition, communication and behavior, and in the central nervous system. Curr. Pharm. Des. 17 1914–1923. 10.2174/138161211796718198 [DOI] [PubMed] [Google Scholar]
- Campbell L. E., Daly E., Toal F., Stevens A., Azuma R., Karmiloff-Smith A., et al. (2009). Brain structural differences associated with the behavioural phenotype in children with Williams syndrome. Brain Res. 1258 96–107. 10.1016/j.brainres.2008.11.101 [DOI] [PubMed] [Google Scholar]
- Chen E. Y., Tan C. M., Kou Y., Duan Q., Wang Z., Meirelles G. V., et al. (2013). Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics 14:128. 10.1186/1471-2105-14-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H., Jiang L., Xie Z., Mei L., He C., Hu Z., et al. (2010). Novel mutations of PAX3, MITF, and SOX10 genes in Chinese patients with type I or type II Waardenburg syndrome. Biochem. Biophys. Res. Commun. 397 70–74. 10.1016/j.bbrc.2010.05.066 [DOI] [PubMed] [Google Scholar]
- Chen X. S., Reader R. H., Hoischen A., Veltman J. A., Simpson N. H., Francks C., et al. (2017). Next-generation sequencing identifies novel gene variants and pathways involved in specific language impairment. Sci. Rep. 7:46105. 10.1038/srep46105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiang M. C., Reiss A. L., Lee A. D., Bellugi U., Galaburda A. M., Korenberg J. R., et al. (2007). 3D pattern of brain abnormalities in Williams syndrome visualized using tensor-based morphometry. Neuroimage 36 1096–1109. 10.1016/j.neuroimage.2007.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe B. P., Witherspoon K., Rosenfeld J. A., van Bon B. W., Vulto-van Silfhout A. T., Bosco P., et al. (2014). Refining analyses of copy number variation identifies specific genes associated with developmental delay. Nat. Genet. 46 1063–1071. 10.1038/ng.3092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- David O., Maess B., Eckstein K., Friederici A. D. (2011). Dynamic causal modeling of subcortical connectivity of language. J. Neurosci. 31 2712–2717. 10.1523/JNEUROSCI.3433-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donato F., Rompani S. B., Caroni P. (2013). Parvalbumin-expressing basket-cell network plasticity induced by experience regulates adult learning. Nature 504 272–276. 10.1038/nature12866 [DOI] [PubMed] [Google Scholar]
- Dorus S., Vallender E. J., Evans P. D., Anderson J. R., Gilbert S. L., Mahowald M., et al. (2004). Accelerated evolution of nervous system genes in the origin of Homo sapiens. Cell 119 1027–1040. 10.1016/j.cell.2004.11.040 [DOI] [PubMed] [Google Scholar]
- Eicher J. D., Powers N. R., Miller L. L., Akshoomoff N., Amaral D. G., Bloss C. S., et al. (2013). Genome-wide association study of shared components of reading disability and language impairment. Genes Brain Behav. 12 792–801. 10.1111/gbb.12085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Einarsdottir E., Svensson I., Darki F., Peyrard-Janvid M., Lindvall J. M., Ameur A., et al. (2015). Mutation in CEP63 co-segregating with developmental dyslexia in a Swedish family. Hum. Genet. 134 1239–1248. 10.1007/s00439-015-1602-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filice F., Vörckel K. J., Sungur A. Ö., Wöhr M., Schwaller B. (2016). Reduction in parvalbumin expression not loss of the parvalbumin-expressing GABA interneuron subpopulation in genetic parvalbumin and shank mouse models of autism. Mol. Brain 9:10. 10.1186/s13041-016-0192-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher S. E. (2017). Evolution of language: lessons from the genome. Psychon. Bull. Rev. 24 34–40. 10.3758/s13423-016-1112-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J. W., Lamperti E. D., Eksioglu Y. Z., Hong S. E., Feng Y., Graham D. A., et al. (1998). Mutations in filamin 1 prevent migration of cerebral cortical neurons in human periventricular heterotopia. Neuron 21 1315–1325. 10.1016/S0896-6273(00)80651-0 [DOI] [PubMed] [Google Scholar]
- Gadea G., Blangy A. (2014). Dock-family exchange factors in cell migration and disease. Eur. J. Cell Biol. 93 466–477. 10.1016/j.ejcb.2014.06.003 [DOI] [PubMed] [Google Scholar]
- Galaburda A. M., Holinger D. P., Bellugi U., Sherman G. F. (2002). Williams syndromeneuronal size and neuronal-packing density in primary visual cortex. Arch. Neurol. 59 1461–1467. 10.1001/archneur.59.9.1461 [DOI] [PubMed] [Google Scholar]
- Graham S. A., Deriziotis P., Fisher S. E. (2015). Insights into the genetic foundations of human communication. Neuropsychol. Rev. 25 3–26. 10.1007/s11065-014-9277-2 [DOI] [PubMed] [Google Scholar]
- Gray V., Karmiloff-Smith A., Funnell E., Tassabehji M. (2006). In-depth analysis of spatial cognition in Williams syndrome: a critical assessment of the role of the LIMK1 gene. Neuropsychologia 44 679–685. 10.1016/j.neuropsychologia.2005.08.007 [DOI] [PubMed] [Google Scholar]
- Hoeft F., Dai L., Haas B. W., Sheau K., Mimura M., Mills D., et al. (2014). Mapping genetically controlled neural circuits of social behavior and visuo-motor integration by a preliminary examination of atypical deletions with Williams syndrome. PLoS One 9:e104088. 10.1371/journal.pone.0104088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horita H., Kobayashi M., Liu W. C., Oka K., Jarvis E. D., Wada K. (2012). Specialized motor-driven Dusp1 expression in the song systems of multiple lineages of vocal learning birds. PLoS One 7:e42173. 10.1371/journal.pone.0042173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horita H., Wada K., Rivas M. V., Hara E., Jarvis E. D. (2010). The dusp1 immediate early gene is regulated by natural stimuli predominantly in sensory input neurons. J. Comp. Neurol. 518 2873–2901. 10.1002/cne.22370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard M. L., Palmer S. J., Taylor K. M., Arthurson G. J., Spitzer M. W., Du X., et al. (2012). Mutation of Gtf2ird1 from the Williams-Beuren syndrome critical region results in facial dysplasia, motor dysfunction, and altered vocalisations. Neurobiol. Dis. 45 913–922. 10.1016/j.nbd.2011.12.010 [DOI] [PubMed] [Google Scholar]
- Jackowski A. P., Rando K., Maria de Araújo C., Del Cole C. G., Silva I., Tavares de Lacerda A. L. (2009). Brain abnormalities in Williams syndrome: a review of structural and functional magnetic resonance imaging findings. Eur. J. Paediatr. Neurol. 13 305–316. 10.1016/j.ejpn.2008.07.002 [DOI] [PubMed] [Google Scholar]
- Jeong Y., Leskow F. C., El-Jaick K., Roessler E., Muenke M., Yocum A., et al. (2008). Regulation of a remote Shh forebrain enhancer by the Six3 homeoprotein. Nat. Genet. 40 1348–1353. 10.1038/ng.230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan T. L., Bellugi U. (1990). Anomalous brain morphology on magnetic resonance images in Williams syndrome and Down syndrome. Arch. Neurol. 47 529–533. 10.1001/archneur.1990.00530050049011 [DOI] [PubMed] [Google Scholar]
- Karmiloff-Smith A., Mills D. L. (2006). “Williams Syndrome,” in Encyclopedia of Language and Linguistics, ed. Brown K. (Oxford: Elsevier; ) 585–589. 10.1016/B0-08-044854-2/04181-X [DOI] [Google Scholar]
- Kimura R., Swarup V., Tomiwa K., Gandal M. J., Parikshak N. N., Funabiki Y., et al. (2018). Integrative network analysis reveals biological pathways associated with Williams syndrome. J. Child Psychol. Psychiatry 10.1111/jcpp.12999 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko J. M., Lim B. C., Kim K. J., Hwang Y. S., Ryu H. W., Lee J. H., et al. (2013). Distinct neurological features in a patient with Schinzel-Giedion syndrome caused by a recurrent SETBP1 mutation. Childs Nerv. Syst 29 525–529. 10.1007/s00381-013-2047-2 [DOI] [PubMed] [Google Scholar]
- Korenberg J. R., Chen X. N., Hirota H., Lai Z., Bellugi U., Burian D., et al. (2000). Genome structure and cognitive map of Williams syndrome. J. Cogn. Neurosci. 12(Suppl. 1), 89–107. 10.1162/089892900562002 [DOI] [PubMed] [Google Scholar]
- Kos M., van den Brink D., Snijders T. M., Rijpkema M., Franke B., Fernandez G., et al. (2012). CNTNAP2 and language processing in healthy individuals as measured with ERPs. PLoS One 7:e46995. 10.1371/journal.pone.0046995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuleshov M. V., Jones M. R., Rouillard A. D., Fernandez N. F., Duan Q., Wang Z., et al. (2016). Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 44 W90–W97. 10.1093/nar/gkw377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalli M. A., Jang J., Park J. H., Wang Y., Guzman E., Zhou H., et al. (2016). Haploinsufficiency of BAZ1B contributes to Williams syndrome through transcriptional dysregulation of neurodevelopmental pathways. Hum. Mol. Genet. 25 1294–1306. 10.1093/hmg/ddw010 [DOI] [PubMed] [Google Scholar]
- Lauber E., Filice F., Schwaller B. (2018). Dysregulation of parvalbumin expression in the Cntnap2-/- mouse model of Autism spectrum disorder. Front. Mol. Neurosci. 11:262. 10.3389/fnmol.2018.00262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavado A., Lagutin O. V., Oliver G. (2008). Six3 inactivation causes progressive caudalization and aberrant patterning of the mammalian diencephalon. Development 135 441–450. 10.1242/dev.010082 [DOI] [PubMed] [Google Scholar]
- Levitin D. J., Cole K., Lincoln A., Bellugi U. (2005). Aversion, awareness, and attraction: investigating claims of hyperacusis in the Williamssyndrome phenotype. J. Child Psychol. Psychiatry 46 514–523. 10.1111/j.1469-7610.2004.00376.x [DOI] [PubMed] [Google Scholar]
- Li N., Bartlett C. W. (2012). Defining the genetic architecture of human developmental language impairment. Life Sci. 90 469–475. 10.1016/j.lfs.2012.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makihara S., Morin S., Ferent J., Côté J. F., Yam P. T., Charron F. (2018). Polarized dock activity drives Shh-mediated axon guidance. Dev. Cell 46:410-425.e7. 10.1016/j.devcel.2018.07.007 [DOI] [PubMed] [Google Scholar]
- Mariën P., Borgatti R. (2018). Language and the cerebellum. Handb. Clin. Neurol. 154 181–202. 10.1016/B978-0-444-63956-1.00011-4 [DOI] [PubMed] [Google Scholar]
- Marjanović M., Sánchez-Huertas C., Terré B., Gómez R., Scheel J. F., Pacheco S., et al. (2015). CEP63 deficiency promotes p53-dependent microcephaly and reveals a role for the centrosome in meiotic recombination. Nat. Commun. 6:7676. 10.1038/ncomms8676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens M. A., Wilson S. J., Reutens D. C. (2008). Research Review: Williams syndrome: acritical review of the cognitive, behavioral, and neuroanatomical phenotype. J. Child Psychol. Psychiatry 49 576–608. 10.1111/j.1469-7610.2008.01887.x [DOI] [PubMed] [Google Scholar]
- Mervis C. B., Becerra A. M. (2007). Language and communicative development in Williams syndrome. Ment. Retard. Dev. Disabil. Res. Rev. 13 3–15. [DOI] [PubMed] [Google Scholar]
- Mervis C. B., Morris C. A., Bertrand J., Robinson E. F. (1999). “Williams syndrome: findings from an integrated program of research,” in Neurodevelopmental Disorders, ed. Tager-Flusberg H. (Cambridge, MA: The MIT Press; ), 65–110. [Google Scholar]
- Miyake F., Kuroda Y., Naruto T., Ohashi I., Takano K., Kurosawa K. (2015). West syndrome in a patient with Schinzel-Giedion syndrome. J. Child Neurol. 30 932–936. 10.1177/0883073814541468 [DOI] [PubMed] [Google Scholar]
- Mobbs D., Eckert M. A., Menon V., Mills D., Korenberg J., Galaburda A. M., et al. (2007). Reduced parietal and visual cortical activation during global processing in Williams syndrome. Dev. Med. Child Neurol. 49 433–438. 10.1111/j.1469-8749.2007.00433.x [DOI] [PubMed] [Google Scholar]
- Morris C. A., Mervis C. B., Hobart H. H., Gregg R. G., Bertrand J., Ensing G. J., et al. (2003). GTF2I hemizygosity implicated in mental retardation in Williams syndrome: genotype-phenotype analysis of five families with deletions in the Williams syndrome region. Am. J. Med. Genet. 123A, 45–59. 10.1002/ajmg.a.20496 [DOI] [PubMed] [Google Scholar]
- Murdoch B. (2010). The cerebellum and language: historical perspective and review. Cortex 46 858–868. 10.1016/j.cortex.2009.07.018 [DOI] [PubMed] [Google Scholar]
- Murphy E., Benítez-Burraco A. (2016). Bridging the gap between genes and language deficits in schizophrenia: an oscillopathic approach. Front. Hum. Neurosci. 10:422. 10.3389/fnhum.2016.00422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy E., Benítez-Burraco A. (2017). Language deficits in schizophrenia and autism as related oscillatory connectomopathies: an evolutionary account. Neurosci. Biobehav. Rev. 83 742–764. 10.1016/j.neubiorev.2016.07.029 [DOI] [PubMed] [Google Scholar]
- Murphy E., Benítez-Burraco A. (2018). Toward the language oscillogenome. Front. Psychol. 9:1999. 10.3389/fpsyg.2018.01999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newbury D. F., Winchester L., Addis L., Paracchini S., Buckingham L. L., Clark A., et al. (2009). CMIP and ATP2C2 modulate phonological short-term memory in language impairment. Am. J. Hum. Genet. 85 264–72. 10.1016/j.ajhg.2009.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nudel R. (2016). An investigation of NFXL1, a gene implicated in a study of specific language impairment. J. Neurodev. Disord. 8:13. 10.1186/s11689-016-9146-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osório A., Soares J. M., Prieto M. F., Vasconcelos C., Fernandes C., Sousa S., et al. (2014). Cerebral and cerebellar MRI volumes in Williams syndrome. Res. Dev. Disabil. 35 922–928. 10.1016/j.ridd.2013.12.014 [DOI] [PubMed] [Google Scholar]
- Pääbo S. (2014). The human condition-a molecular approach. Cell 157 216–226. 10.1016/j.cell.2013.12.036 [DOI] [PubMed] [Google Scholar]
- Pagnamenta A. T., Bacchelli E., de Jonge M. V., Mirza G., Scerri T. S., Minopoli F., et al. (2010). Characterization of a family with rare deletions in CNTNAP5 and DOCK4 suggests novel risk loci for autism and dyslexia. Biol. Psychiatry 68 320–328. 10.1016/j.biopsych.2010.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paracchini S., Diaz R., Stein J. (2016). “Advances in dyslexia genetics—new insights into the role of brain asymmetries,” in Advances in Genetics 96, eds Friedmann T., Dunlap J. C., Goodwin S. F. (London: Academic Press; ),53–97. [DOI] [PubMed] [Google Scholar]
- Peedicayil J., Grayson D. R. (2018). An epigenetic basis for an omnigenic model of psychiatric disorders. J. Theor. Biol. 443 52–55. 10.1016/j.jtbi.2018.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettigrew K. A., Frinton E., Nudel R., Chan M. T., Thompson P., Hayiou-Thomas M. E., et al. (2016). Further evidence for a parent-of-origin effect at the NOP9 locus on language-related phenotypes. J. Neurodev. Disord. 8:24. 10.1186/s11689-016-9157-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips E. A. K., Schreiner C. E., Hasenstaub A. R. (2017). Cortical interneurons differentially regulate the effects of acoustic context. Cell Rep. 20 771–778. 10.1016/j.celrep.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pober B. R., Wang E., Caprio S., Petersen K. F., Brandt C., Stanley T., et al. (2010). High prevalence of diabetes and pre-diabetes in adults with Williams syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 154C, 291–298. 10.1002/ajmg.c.30261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purser H. R., Thomas M. S., Snoxall S., Mareschal D., Karmiloff-Smith A. (2011). Definitions versus categorization: assessing the development of lexico-semantic knowledge in Williams syndrome. Int. J. Lang. Commun. Disord. 46 361–373. 10.3109/13682822.2010.497531 [DOI] [PubMed] [Google Scholar]
- Reilly J., Klima E. S., Bellugi U. (1990). Once more with feeling: affect and language in atypical populations. Dev. Psychopathol. 2 367–391. 10.1017/S0954579400005782 [DOI] [Google Scholar]
- Roll P., Rudolf G., Pereira S., Royer B., Scheffer I. E., Massacrier A., et al. (2006). SRPX2 mutations in disorders of language cortex and cognition. Hum. Mol. Genet. 15 1195–1207. 10.1093/hmg/ddl035 [DOI] [PubMed] [Google Scholar]
- Roll P., Vernes S. C., Bruneau N., Cillario J., Ponsole-Lenfant M., Massacrier A., et al. (2010). Molecular networks implicated in speech-related disorders: FOXP2 regulates the SRPX2/uPAR complex. Hum. Mol. Genet. 19 4848–4860. 10.1093/hmg/ddq415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royer-Zemmour B., Ponsole-Lenfant M., Gara H., Roll P., Lévêque C., Massacrier A., et al. (2008). Epileptic and developmental disorders of the speech cortex: ligand/receptor interaction of wild-type and mutant SRPX2 with the plasminogen activator receptor uPAR. Hum. Mol. Genet. 17 3617–3630. 10.1093/hmg/ddn256 [DOI] [PubMed] [Google Scholar]
- Sakurai T., Dorr N. P., Takahashi N., McInnes L. A., Elder G. A., Buxbaum J. D. (2011). Haploinsufficiency of Gtf2i, a gene deleted in Williams Syndrome, leads to increases in social interactions. Autism Res. 4 28–39. 10.1002/aur.169 [DOI] [PubMed] [Google Scholar]
- Scharff C., White S. A. (2004). Genetic components of vocal learning. Ann. N. Y. Acad. Sci. 1016 325–347. 10.1196/annals.1298.032 [DOI] [PubMed] [Google Scholar]
- Schmitt J. E., Eliez S., Bellugi U., Reiss A. L. (2001). Analysis of cerebral shape in Williams syndrome. Arch. Neurol. 58 283–287. 10.1001/archneur.58.2.283 [DOI] [PubMed] [Google Scholar]
- Shao S., Kong R., Zou L., Zhong R., Lou J., Zhou J., et al. (2016). The roles of genes in the neuronal migration and neurite outgrowth network in developmental dyslexia: single- and multiple-risk genetic variants. Mol. Neurobiol. 53 3967–3975. 10.1007/s12035-015-9334-8 [DOI] [PubMed] [Google Scholar]
- Smith A. D., Gilchrist I. D., Hood B., Tassabehji M., Karmiloff-Smith A. (2009). Inefficient search of large-scale space in Williams syndrome: further insights on the role of LIMK1 deletion in deficits of spatial cognition. Perception 38 694–701. 10.1068/p6050 [DOI] [PubMed] [Google Scholar]
- Smyth G. K. (2005). “Limma: linear models for microarray data,” in Bioinformatics and Computational Biology Solutions Using R and Bioconductor, eds Gentleman R., Carey V., Dudoit S., Irizarry R., Huber W. (New York: Springer; ), 397–420. 10.1007/0-387-29362-0_23 [DOI] [Google Scholar]
- Stachowiak M. K., Kucinski A., Curl R., Syposs C., Yang Y., Narla S., et al. (2013). Schizophrenia: a neurodevelopmental disorder-integrative genomic hypothesis and therapeutic implications from a transgenic mouse model. Schizophr. Res. 143 367–376. 10.1016/j.schres.2012.11.004 [DOI] [PubMed] [Google Scholar]
- Sylvester J. B., Rich C. A., Loh Y. H., van Staaden M. J., Fraser G. J., Streelman J. T. (2010). Brain diversity evolves via differences in patterning. Proc. Natl. Acad. Sci. U.S.A. 107 9718–9723. 10.1073/pnas.1000395107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tassabehji M., Hammond P., Karmiloff-Smith A., Thompson P., Thorgeirsson S. S., Durkin M. E., et al. (2005). GTF2IRD1 in craniofacial development of humans and mice. Science 310 1184–1187. 10.1126/science.1116142 [DOI] [PubMed] [Google Scholar]
- Tassabehji M., Read A. P., Newton V. E., Harris R., Balling R., Gruss P., et al. (1992). Waardenburg’s syndrome patients have mutations in the human homologue of the Pax-3 paired box gene. Nature 355 635–636. 10.1038/355635a0 [DOI] [PubMed] [Google Scholar]
- Thompson P. M., Lee A. D., Dutton R. A., Geaga J. A., Hayashi K. M., Eckert M. A., et al. (2005). Abnormal cortical complexity and thickness profiles mapped in Williams syndrome. J. Neurosci. 25 4146–4158. 10.1523/JNEUROSCI.0165-05.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todorovski Z., Asrar S., Liu J., Saw N. M., Joshi K., Cortez M. A., et al. (2015). LIMK1 regulates long-term memory and synaptic plasticity via the transcriptional factor CREB. Mol. Cell. Biol. 35 1316–1328. 10.1128/MCB.01263-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis M. A., van der Flier A., Kammerer R. A., Mould A. P., Sonnenberg A., Humphries M. J. (2004). Interaction of filamin A with the integrin beta 7 cytoplasmic domain: role of alternative splicing and phosphorylation. FEBS Lett. 569 185–190. 10.1016/j.febslet.2004.04.099 [DOI] [PubMed] [Google Scholar]
- Udwin O., Yule W. (1991). A cognitive and behavioural phenotype in Williams syndrome. J. Clin. Exp. Neuropsychol. 13 232–244. 10.1080/01688639108401040 [DOI] [PubMed] [Google Scholar]
- Ueda S., Fujimoto S., Hiramoto K., Negishi M., Katoh H. (2008). Dock4 regulates dendritic development in hippocampal neurons. J. Neurosci. Res. 86 3052–3061. 10.1002/jnr.21763 [DOI] [PubMed] [Google Scholar]
- Ueda S., Negishi M., Katoh H. (2013). Rac GEF Dock4 interacts with cortactin to regulate dendritic spine formation. Mol. Biol. Cell 24 1602–1613. 10.1091/mbc.E12-11-0782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Heuvel E., Manders E., Swillen A., Zink I. (2016). Developmental trajectories of structural and pragmatic language skills in school-aged children with Williams syndrome. J. Intellect. Disabil. Res. 60 903–919. 10.1111/jir.12329 [DOI] [PubMed] [Google Scholar]
- Vernes S. C., Newbury D. F., Abrahams B. S., Winchester L., Nicod J., Groszer M., et al. (2008). A functional genetic link between distinct developmental language disorders. N. Engl. J. Med. 359:2337. 10.1056/NEJMoa0802828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vias C., Dick A. S. (2017). Cerebellar contributions to language in typical and atypical development: a review. Dev. Neuropsychol. 42 404–421. 10.1080/87565641.2017.1334783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villanueva P., Nudel R., Hoischen A., Fernández M. A., Simpson N. H., Gilissen C., et al. (2015). Exome sequencing in an admixed isolated population indicates NFXL1 variants confer a risk for specific language impairment. PLoS Genet. 11:e1004925. 10.1371/journal.pgen.1004925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volterra V., Capirci O., Pezzini G., Sabbadini L., Vicari S. (1996). Linguistic abilities in Italian children with Williams syndrome. Cortex 32 663–677. 10.1016/S0010-9452(96)80037-2 [DOI] [PubMed] [Google Scholar]
- Wahl M., Marzinzik F., Friederici A. D., Hahne A., Kupsch A., Schneider G. H., et al. (2008). The human thalamus processes syntactic and semantic language violations. Neuron 59 695–707. 10.1016/j.neuron.2008.07.011 [DOI] [PubMed] [Google Scholar]
- Whalley H. C., O’Connell G., Sussmann J. E., Peel A., Stanfield A. C., Hayiou-Thomas M. E., et al. (2011). Genetic variation in CNTNAP2 alters brain function during linguistic processing in healthy individuals. Am. J. Med. Genet. B Neuropsychiatr. Genet. 156B, 941–948. 10.1002/ajmg.b.31241 [DOI] [PubMed] [Google Scholar]
- Whitehouse A. J., Bishop D. V., Ang Q. W., Pennell C. E., Fisher S. E. (2011). CNTNAP2 variants affect early language development in the general population. Genes Brain Behav. 10 451–456. 10.1111/j.1601-183X.2011.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y., Peng Y., Wan J., Tang G., Chen Y., Tang J., et al. (2013). The atypical guanine nucleotide exchange factor Dock4 regulates neurite differentiation through modulation of Rac1 GTPase and actin dynamics. J. Biol. Chem. 288 20034–20045. 10.1074/jbc.M113.458612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu C., Aragam N., Li X., Villla E. C., Wang L., Briones D., et al. (2013). BCL9 and C9orf5 are associated with negative symptoms in schizophrenia: meta-analysis of two genome-wide association studies. PLoS One 8:e51674. 10.1371/journal.pone.0051674 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE89594.