Abstract
Traumatic brain injury (TBI) has become an economic and social burden for patients and their families. While acupuncture is an effective tool for promoting recovery of disorder of consciousness (DOC) following TBI, there have been no comprehensive meta-analyses and/or systematic reviews addressing this topic. The present systematic review and meta-analysis aimed to assess the therapeutic efficacy of acupuncture for DOC after TBI. All randomized controlled trials (RCTs) incorporating acupuncture, or acupuncture combined with other interventions for DOC after TBI, were included and assessed by two independent investigators. Six outcome indicators were assessed: Glasgow Coma Scale (GCS); Glasgow Outcome Scale (GOS); mortality; efficacy rate; activities of daily living (ADL); and functional comprehensive assessment. Direct comparisons were performed using RevMan 5.3.0 software, with results presented as mean difference (MD) for continuous outcomes and relative risk (RR) for binary outcomes. A total of 3511 patients from 49 trials were included. Pooled analyses indicated that acupuncture may have a superior effect on GCS score (MD=2.03, 95% CI :1.92 2.43, Z=16.54, and P<0.00001); GOS score (RR=1.23, 95%CI: 1.18 1.35, Z=6.65, and P<0.00001); efficacy rate (RR=1.48, 95%CI: 1.40 1.56, Z=13.49, and P<0.00001); ADL (MD=9.20, 95% CI:8.19 10.21, Z=17.84, and P<0.00001); and mortality (RR=0.50, 95% CI:0.38 0.67, Z=4.70, and P<0.00001). The results demonstrated that the acupuncture group fared better than the control group in the treatment of DOC after TBI. However, studies were generally of poor quality, and publication bias favoring positive studies was obvious. Therefore, rigorous evaluation standards and well-designed studies are necessary in future studies.
1. Introduction
Traumatic brain injury (TBI) is a global public health problem and one of the major causes of death and disability [1]. According to a survey by the World Health Organization, TBI will surpass many other factors as a main cause of death and disability by the year 2020 [2]. According to statistics, more than 50 million individuals experience TBI each year, and the total number of new TBI cases has been reported to approach 3.5 million per year in the United States [3], with 30-40% of deaths related to the injury. The mortality rate of TBI in China was 12.99/100,000 in 2013 and 17.1/100,000 in the United States, with traffic accidents and falls as the main causes [4–6]. TBI has become an enormous economic burden to families and society as a whole. TBI-related costs were estimated to be as high as €33 billion in Europe in 2010, of which indirect costs accounted for 59% and direct costs accounted for 41% [7, 8]. In the United States, it has been reported that aggregate direct and indirect costs increased from USD$60.4 billion in 2000 to USD$221 billion in 2009 [9].
The rapid development of emergency medicine and intensive care technology in recent years has clearly improved the survival of individuals who sustain TBI [10]. However, regarding severe brain damage, patients also experienced varying degrees of disorders of consciousness (DOC) after TBI, which seriously affects an individual's ability to perform the activities of daily living (ADL) and reduces the quality of life [11–13]. The early recovery of consciousness is closely associated with recovery in other functional domains, and the duration of DOC is an important prognostic factor in patients who experience TBI [13–15].
The annual cost for treatment and rehabilitation of TBI patients is nearly $400 billion, which is associated with tremendous inconvenience and economic pressure on patients, their families, and society [16, 17]. Therefore, studies investigating the recovery of patients' consciousness after TBI are important in the field of neurologic rehabilitation and have a great economic and social impact. There are many important treatment approaches for recovering consciousness, including pharmacological interventions, surgery, rehabilitation, and alternative medicine treatments such as acupuncture. Acupuncture has been shown to be an effective method when applied to traumatic injuries. A systematic review by Ma concluded that the use of acupuncture to treat spinal cord injury may have a beneficial effect on neurological and functional recovery. [18] Another review suggested that acupuncture is efficacious in acute TBI [19]. In China, acupuncture has been used for centuries to promote the recovery of consciousness after coma or other DOCs by increasing the excitability of nerve cells [20–22] and the supply of oxygen and blood flow in the traumatized area of the brain, which may be a potential mechanism for its rousing effects [23–25].
Although many studies investigating acupuncture for treatment of DOC after TBI have been published, they have not been systematically reviewed. Thus, the aim of the present systematic literature review was to assess the rousing effect of acupuncture on DOC after TBI.
2. Methods
2.1. Protocol and Registration
We had published a protocol of this systematic review in the PROSPERO database (identification number: CRD42018091226).
2.2. Data Source and Search Strategy
A systematic search of the literature was conducted in PubMed, Cochrane Library, Chinese Biomedical Literature Database (CBM), VIP, WanFang Database, and Chinese National Knowledge Infrastructure (CNKI) databases for articles published up to February 28, 2018. The searching terms include “coma”, “disorder of consciousness”, “minimally consciousness state”, “vegetative state”, “locked-in state”, “traumatic brain injury”, “brain injury”, “head injury”, “acupuncture”, and “electro-acupuncture”. The search was limited to studies published in Chinese and English.
2.3. Inclusion Criteria
All trials in which the intervention involved acupuncture or electroacupuncture separately, or acupuncture combined with other interventions, such as hyperbaric oxygen (HPO), traditional Chinese medicine (TCM) rehabilitation, and electrical stimulation, were included. There was no distinction for acupoints, manipulation, stimulation intensity, or the course of treatment. It is available for basic treatment or combined with rehabilitation training in the control group. The trials' outcome indicators had to include at least one of the following: Glasgow Coma Scale (GCS) or Glasgow Outcome Scale (GOS).
2.4. Exclusion Criteria
Trials that used transcutaneous electrical nerve stimulation and/or manual acupressure and DOC results from nontraumatic diseases, such as cerebrovascular disease, tumor, or toxicosis, were excluded. In addition, trials without a nonacupuncture group were also excluded.
2.5. Data Extraction
Data were extracted independently by two authors (LT and LZ) using a specifically designed data extraction form. Disagreements were resolved by assistance from the third author (NW). Data extracted from each study were summarized in a data extraction table. Items noted included the following: first author and year of publication; type of intervention; sample size; sex ratios; years; TBI's degree, duration of treatment, and main outcome indicators in each trial. For studies in which outcomes were assessed at several different time points, the measurement after the final treatment was selected. Meanwhile, if the duration of treatment described as applying according to the condition of disease, we attributed it to an unclear duration of treatment.
2.6. Quality Assessment
Two authors (MJD and TIM) evaluated the quality of included trials. The risk of bias was assessed using the risk of bias tool from the Cochrane Handbook of Systematic Reviews of Interventions [26] according to the following criteria: random sequence generation allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; and other biases and descriptions of the risk of bias.
2.7. Data Analysis
RevMan 5.3 software was used for data analysis and Stata version 13.0 (StataCorp LP, College Station, TX, USA) was used for sensitivity analysis. Different outcome indicators were classified and analyzed. Relative risk (RR) was evaluated for dichotomous outcomes, while mean difference (MD) was used for continuous outcomes with 95% confidence interval (CI). Because there was significant clinical heterogeneity among the trials (P<0.1), a random-effects model was used in the meta-analysis, and a fixed-effects model was used for those with low heterogeneity (P>0.1). Potential publication bias was assessed using funnel plots.
3. Results
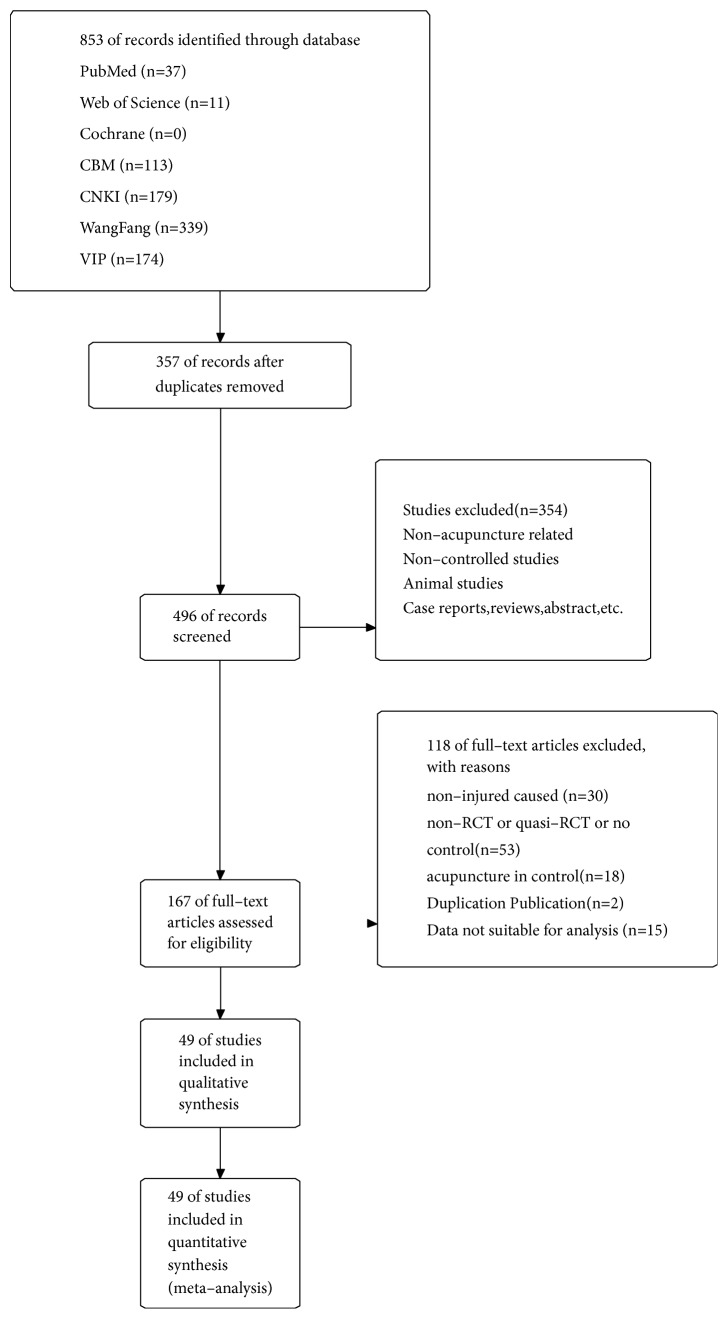
A flowchart depicting the search process and study selection is shown in Figure 1. Forty-nine studies including 3511 patients were ultimately included. There were 1800 participants in the acupuncture group and 1711 in the control group.
Figure 1.
The screening flow diagram.
3.1. The Basic Characteristics
All trials were conducted in China and published in Chinese. The acupuncture and control groups were compared statistically according to sex, age, duration, and level of consciousness; baseline data were comparable. Regarding the intervention in the treatment groups, acupuncture was applied in 18 RCTs, electroacupuncture in 16, acupuncture combined with HPO in 6, acupuncture combined with TCM in 7, electroacupuncture combined TCM and HPO in 1, and acupuncture combined TCM and laser intravascular irradiation in 1. Thirty-seven studies reported GCS data before treatment, with sample sizes ranging from 29 to 126. Only 10 RCTs enrolled patients and reported the duration of TBI. The characteristics of the included trials are summarized in Table 1.
Table 1.
The basic characteristic of the included studies.
| Studies | Simple Size (T/C)(M/F) |
Mean age (T/C) |
Intervention (T/C) |
GCS before treatment (T/C) (GCS Scores/number) |
TBI's Degree | Duration of Treatment | Outcome measure |
|---|---|---|---|---|---|---|---|
| Fu 2009 | 16(12/4)/16(14/3) | 41.8±18.5/36.8±18.5 | EA/BT | 4.06±1.06/3.87±1.02 | S | 30 D | GCS |
| He 2012 | 30/20 | NR | EA/BT | NR | S | 1 M | GOS |
| Yu 2010 | 34/34 | NR | A/BT | 5.60±2.25/5.81±2.23 | S | 1 M | GCS |
| Yu 2012 | 30/30 | 33.38±12.65 | A/BT | 5.63±1.69/5.80±1.79 | S | 1 M | GCS |
| Feng 2005 | 44(29/15)/40(29/15) | 39±15/36±13 | A/BT | (3-5/9,6-8/35)/(3-5/3,6-8/32) | S | 1 M | GCS/GOS |
| Liu 2015 | 43/42 | NR | A/BT | NR | S | 1 M | GOS |
| Liu 2010 | 15(9/6)/14(9/6) | 32.6±15.3/31.9±15.8 | EA/BT | (5/3,6/4,7/3,8/5)/(5/3,6/3,7/4,8/4) | S | U | GOS |
| Liu 2016 | 43(30/12)/42(29/14) | 38.61±4.65/36.92±4.87 | A/BT | 3-5/22,6-8/35,9-11/17,12-15/11 | S/Mo/Mi | 30 D | GOS |
| Liu 2006 | 50(34/16)/50(32/18) | NR | EA/BT | (3-5/12,6-8/38)/(3-5/11,6-8/39) | S | 30 D | GOS |
| Liu et.al. 2006 | 60(44/16)/60(42/18) | 32.5/32 | A+HO+LII/BT | (8/19,7/36,≤6/5)/(8/18,7/36,≤6/6) | S | 30 D | GCS |
| Lu 2015 | 37(22/15)/37(22/15) | 39.6±1.5/30.21±1.8 | EA/BT | NR | S | 30 D | GOS |
| Gu 2010 | 61(42/19)/61(41/20) | 45±12.11/43.1±11.12 | A+TCM/BT | (3-5/23,6-8/38)/(3-5/24,6-8/37) | S | 1 W | GOS |
| Lv 2013 | 43(23/20)/42(25/17) | 42.5±12.7/41.7±13.2 | EA/BT | 3.9±1.1/4.01±1.06 | S | 30 D | GCS/GOS |
| Tang 2016 | 15(11/4)/15(11/3) | 49.53±15.73/52.14±11.36 | EA/BT | 5.80±1.47/5.57±1.22 | S | 4 W | GCS/GOS |
| Lou 2013 | 25/25 | NR | A+HO/BT | NR | S | U | GOS |
| Sun 2009 | 30(22/8)/30(20/10) | 45.2/39.8 | A/BT | (3-5/9,6-8/21)/(3-5/8,6-8/22) | S | 2 M | GOS |
| Song 2007 | 30/20 | NR | EA/BT | NR | S | 1 M | GOS |
| Zhang 2013 | 30(19/11)/30(21/9) | 37.1±9.1/37.2±10.1 | EA/BT | (3-5/13,6-8/17)/(3-5/12,6-8/18) | S | 1 M | GOS |
| Zhang 2011 | 22(19/3)/20(14/6) | 43.50±1.27/46.25±1.31 | A/BT | 6.41±1.47/6.45±1.47 | S | 30 D | GCS |
| Peng 2010 | 29(20/9)/27(20/7) | 39.1±12.2/40.2±9.8 | EA/BT | 5.08±1.47/5.10±2.11 | S | 1 M | GOS |
| Cheng 2016 | 28/29 | NR | EA/BT | 5.42±1.29/5.68±1.54 | S | U | GCS |
| Li 2003 | 40(29/11)/40(27/13) | 39±15/36±14 | A+TCM/BT | (3-5/9,6-8/31)/(3-5/8,6-8/32) | S | 1 M | GOS |
| Li 2010 | 16(12/4)/14(10/4) | 45.6/46.4 | A+TCM/BT | (3-5/4,6-8/12)/(3-5/4,6-8/10) | S | 1 M | GOS |
| Yang 2011 | 15(11/4)/15(10/5) | 37.4/35.1 | A+HO/BT | 5.7/5.9 | S | 30 D | GCS |
| Yang 2007 | 20(11/9)/20(12/8) | 40.25±0.36/42.06±0.28 | EA/BT | 6.5±1.471/6.6±1.04 | S | 7 D | GCS |
| Yang 2016 | 50/40 | NR | A/BT | NR | S | 60 D | GOS |
| Jiang 2009a | 33(25/8)/30(26/4) | NR | A+HO/BT | NR | S | U | GOS |
| jiang 2009b | 76(53/12)/58(48/10) | 28.1/27.4 | A/BT | 5.3±1.18/5.1±1.21 | S | U | GOS |
| You 2013 | 16(12/4)/15(10/5) | 34.7±9.9/35.2±8.7 | A/BT | 6.2±1.7/5.9±1.4 | S | 4 W | GCS |
| Wang 2012 | 50(42/8)/50(40/10) | NR | A/BT | 4.04±1.06/4.08±1.02 | NR | 1 M | GCS |
| Wang 2013 | 50/50 | NR | EA+HO+TCM/BT | NR | S | 2 W | GOS |
| Wang 2016 | 50(37/13)/50(37/13) | 42.36±16.11/43.10±15.33 | A/BT | 5.90±1.53/5.98±1.60 | S | 3 W | GCS |
| Ge 2014 | 23(13/10)/23(15/8) | 32.06±3.18/31.26±4.25 | EA/BT | NR | S | 1 M | GOS |
| Xie 2016 | 32(24/8)/32(25/7) | 39.5/36.9 | A/BT | 4.92±1.17/4.81±1.55 | S | 1 M | GCS |
| Guo 2016 | 30(18/12)/30(20/10) | 35.2±8.43/33.7±7.56 | EA/BT | 6.53±1.18/6.87±7.56 | S | 30 D | GCS |
| Chen 2013 | 39(25/14)/38(26/12) | 31.47±3.88/31.52±3.82 | A+HO/BT | NR | S | U | GOS |
| Chen 2011 | 36/34 | NR | A+HO/BT | NR | S | 1 M | GOS |
| Chen 2006 | 54(36/18)/51(37/14) | 34±11/36±112 | A+TCM/BT | (3-5/15,6-8/39)/(3-5/14,6-8/37) | S | 8 W | GCS/GOS |
| Chen 2009 | 46(38/8)/46(35/11) | 47±2.13/47±2.37 | EA/BT | 4.03±1.05/4.07±1.02 | S/Mo | U | GCS |
| Lu 2014 | 20(12/8)/20(11/9) | 34±116/33±16 | A/BT | (5/6,6/7,7/3,8/4)/(5/5,6/6,7/4,8/5) | S | 30 D | GOS |
| Tu 2010 | 51(35/16)/51(37/14) | 42.5±11.4/41.1±11.2 | A/BT | (3-5/16,6-8/35)/(3-5/17,6-8/34) | S | 30 D | GOS |
| Yan 2018 | 50(32/18)/50(30/20) | 35.2±11.8/34.5±10.3 | EA/BT | 4.6±1.15/4.5±1.44 | S | 1 M | GCS |
| Xue 2017 | 36(25/13)/38(24/12) | 38.15±5.26/39.75±6.18 | A+TCM/BT | 5.75±2.26/6.13±2.27 | S/Mo | 8 W | GCS/GOS |
| Xu 2015 | 30(19/12)/30(18/11) | 39.75±17.86/9.06±2.03 | A/BT | 6.0±1.80/5.9±1.70 | S | 14 D | GCS/GOS |
| Xing 2007 | 20/20 | NR | A/BT | 5.9±0.85/5.00±1.17 | S | 4 W | GCS |
| Wang et al 2016 | 39(22/17)/39(21/18) | 53.5±2.4/53.4±2.5 | A+HO/BT | 6.3±1.36/6.4±1.14 | NR | 3 M | GCS |
| Ding 2015 | 40(24/16)/40(22/18) | 35.8±4.3/35.4±4.3 | A+TCM/BT | 5.7±1.06/10.05±1.3 | NR | U | GCS |
| Zhang 2014 | 80(82/44)/46 | 27.7 | A+TCM/BT | NR | S | 2 M | GOS |
| Tian 2012 | 58(85/31)/58 | 43.5 | A/BT | 8.5±3.01/8.46±3.22 | S/Mo | 14 D | GCS/GOS |
NR: not report; A: acupuncture; EA: electroacupuncture; TCM: traditional Chinese medicine; HO: hyperbaric oxygen; BT: basic treatment; Mi: mild TBI; Mo: moderate TBI; S: severe TBI; M: month; W: week; D: day; U: unclear; GCS: Glasgow Coma Scale; GOS: Glasgow Outcome Scale.
3.2. Quality Evaluation
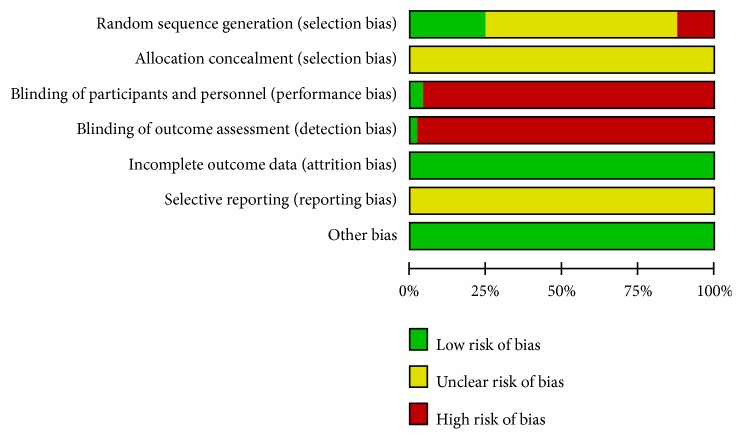
The majority of the included studies were assessed to be of generally poor methodological quality according to the Cochrane Handbook of Systematic Reviews of Interventions. Although “random allocation” was mentioned in all studies, only 12 RCTs reported the details of random sequence generation using a random numbers table. [21–23, 27–35]. There was no clear information regarding allocation concealment, and only 2 RCTs reported the blinding method [22, 32]. For incomplete outcome data, 1 study reported drop-out and exit of patients without any effect on the results, and 1 reported transfer from one hospital to another [29, 32]. Selective reporting was generally unclear due to inaccessibility of trial protocols. Only 7 trials reported funding support [25, 30, 32, 34–37]. The methodological quality of the included RCTs is shown in Figures 2 and 3.
Figure 2.
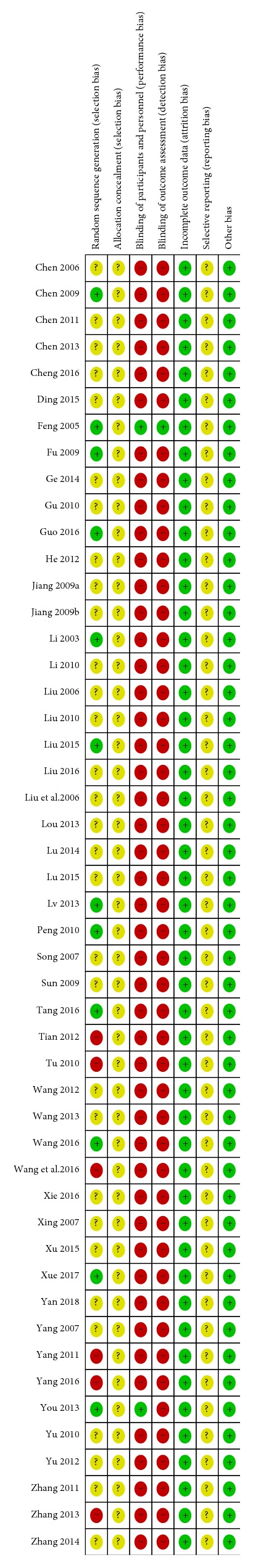
The bias of each study.
Figure 3.
The summary of bias evaluation for the studies.
3.3. Glasgow Coma Scale (GCS)
Thirty-seven trials reported the level of consciousness (according to GCS) before treatment [20–23, 25, 27–30, 32–58], and GCS score was used in 28 studies as the outcome measure [20–23, 25, 27–30, 32, 33, 35–39, 41, 42, 44–48, 54–56, 58]. Twenty-two studies used continuous data, and the statistic used was the difference in GCS score before and after treatment [20, 21, 23, 27–30, 32, 33, 36–39, 41, 42, 44–46, 48, 54, 55]. The GCS results showed high heterogeneity (I2=72%), so we did a subgroup analysis according to the treatment duration, TBI's degree (we define the GCS score between 3 and 8 as severe TBI, 8 and 12 as moderate TBI, and 13 and 15 as mild TBI), and intervention. From Table 2, results of subgroup of unclear treatment course [36, 42, 54] in treatment duration are the main source of heterogeneity (I2=96%) and show that there is no difference between acupuncture group and control (MD=1.34, 95%CI -0.24 2.92). Also, there were no differences between treatment group and control for results of subgroup of unclear degree of TBI patients in TBI's degree (MD=2.03, 95%CI: -0.06 4.12) and subgroup of acupuncture plus TCM in intervention (MD=0.83, 95%CI: -0.49 2.15). Test for overall effect demonstrates that the acupuncture could improve the GCS score (MD=2.03, 95%CI 1.54—2.52, Z=8.17, and P<0.00001) (Table 2).
Table 2.
Results of subgroup analysis of GCS by treatment duration, TBI's degree, and intervention.
| Variables | Numbers of studies | Numbers of patient(T/C) | MD(95%CI) | Heterogeneity(I2) | Z-value | P-value | |
|---|---|---|---|---|---|---|---|
| Treatment duration | 7d | 1 | 20/20 | 2.20 [1.28, 3.12] | Not applicable | 4.71 | P < 0.00001 |
| 14d | 2 | 89/87 | 2.42 [1.56, 3.29] | 0% | 5.48 | P < 0.00001 | |
| 3W | 1 | 50/50 | 2.42 [1.29, 3.55] | Not applicable | 4.18 | P < 0.00001 | |
| 4W or 30d or 1M | 12 | 358/354 | 2.20 [1.80, 2.59] | 2% | 10.9 | P < 0.00001 | |
| 8W | 2 | 91/91 | 2.13 [0.93, 3.33] | 67% | 3.47 | P < 0.00001 | |
| 3M | 1 | 39/39 | 3.20 [2.31, 4.09] | Not applicable | 7.07 | P < 0.00001 | |
| Unclear | 3 | 144/127 | 1.34 [-0.24, 2.92] | 96% | 2.02 | P=0.04 | |
| Test for subgroup differences | 85.8% | P < 0.00001 | |||||
| TBI's Degree | Severe | 17 | 560/548 | 2.00 [1.49, 2.51] | 68% | 7.69 | P < 0.00001 |
| Severe/Moderate | 2 | 91/91 | 2.13 [0.93, 3.33] | 67% | 3.47 | P = 0.0005 | |
| Unclear | 3 | 129/129 | 2.03 [-0.06, 4.12] | 95% | 1.91 | P=0.06 | |
| Test for subgroup differences | 0% | P = 0.98 | |||||
| Intervention | A | 12 | 425/415 | 2.22 [1.47, 2.96] | 83% | 6.07 | P < 0.00001 |
| EA | 8 | 248/248 | 2.13 [1.59, 2.68] | 29% | 7.71 | P < 0.00001 | |
| A plus TCM | 2 | 85/85 | 0.83 [-0.49, 2.15] | 84% | 1.23 | P = 0.22 | |
| Test for subgroup differences | 43.4% | P = 0.17 | |||||
| Total | 22 | 780/768 | 2.03 [1.54, 2.52] | 78% | 8.17 | P < 0.00001 | |
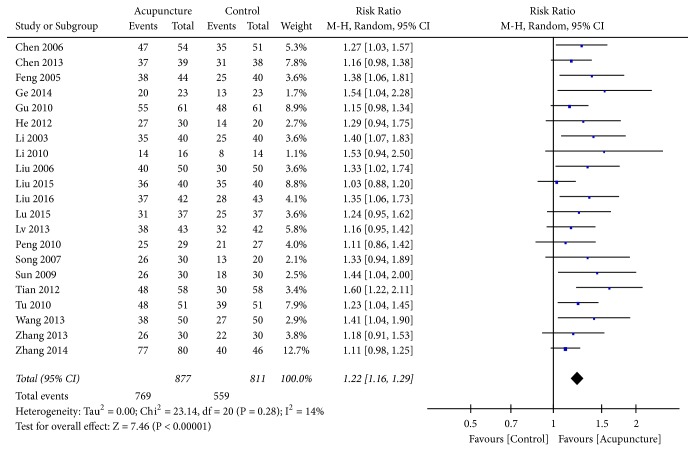
3.4. Glasgow Outcome Scale (GOS)
The GOS was used in 28 trials, 25 of which used dichotomous data [22, 25, 31, 33–35, 40, 43, 45, 49–53, 57–66], and 2 were excluded because outcome times were unclear [50, 63]. Outcome was defined as good conscious state (GOS score ≥ 3/5) or poor (GOS score 1-2) as a simplified measure of level of consciousness outcome after TBI. The RR was selected to represent the count data. Low heterogeneity (I2 = 14%, P=0.28) was found after pooling the data; hence, a random-effects model was applied. The rectangle was on the right of the equivalence line, which indicated that acupuncture could improve the level of consciousness after TBI (RR=1.23, 95%CI 1.20 1.33], Z=8.88, and P<0.00001) (Figure 4).
Figure 4.
Forest plot of GOS.
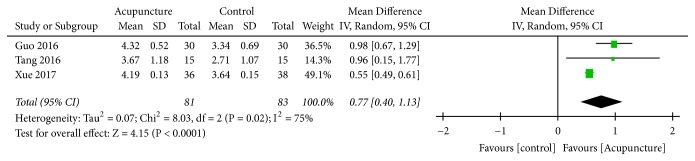
Three trials [27, 29, 30] used continuous data with MD. The results indicated high heterogeneity (I2 = 75%, P=0.02); therefore, a random-effect model was applied. Pooled analysis revealed that acupuncture improved GOS score (MD= 0.77, 95% CI: 0.40 1.13, Z=4.15, and P=0.01) (Figure 5).
Figure 5.
Forest plot of GOS.
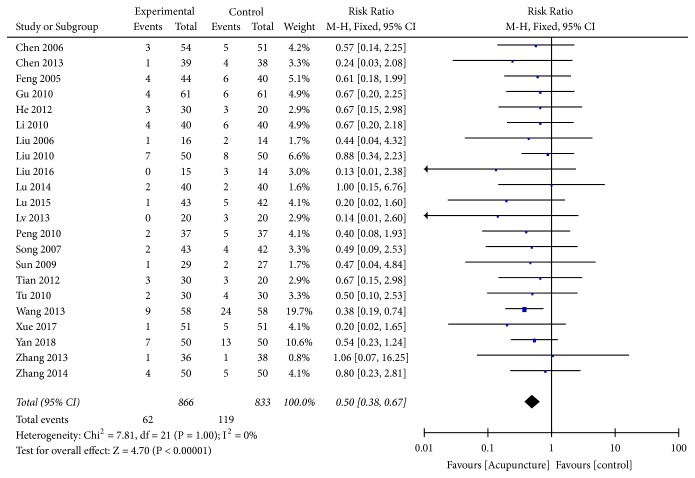
3.5. Mortality
Among the included studies, 24 [20, 22, 25, 27, 31, 33–35, 40, 43, 45, 49–53, 57–60, 62, 64–66] reported mortality data after acupuncture treatment. Due to low statistical heterogeneity (I2 = 0%, P=1.0), a fixed-effects model was applied, which revealed that mortality rates between the acupuncture and the control groups were significantly different (RR=0.50, 95%CI: 0.38 0.67, Z=4.70, and P<0.00001) (Figure 6).
Figure 6.
Forest plot of mortality.
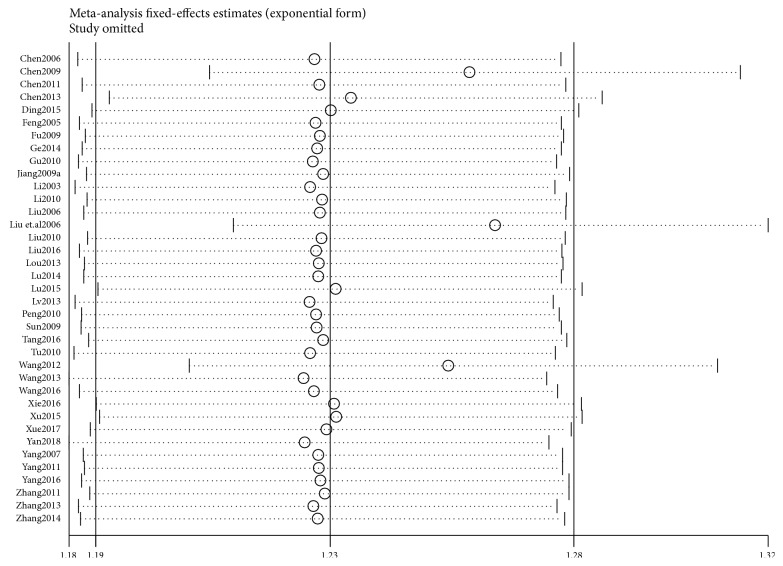
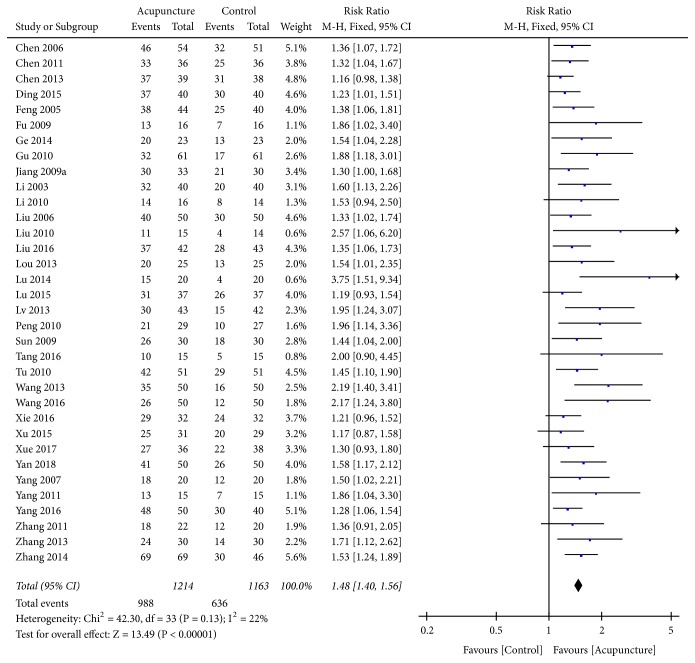
3.6. Efficacy Rate
In 37 trials [20–23, 25, 27–29, 33–35, 38, 40–44, 46, 47, 49–53, 55–64, 67–69], the clinical efficacy rate was used as the evaluation indicator with dichotomous data; therefore, RR was used to express the results. After combining the data, high heterogeneity (I2 = 69%, P<0.00001) was found; therefore, a sensitivity analysis was applied. The funnel plot revealed that 3 trials [21, 44, 56] deviated from the center line (Figure 7), which had significant influence on combined effect due to high sensitivity. The curative effect in the acupuncture group was found significantly higher than that of the control group. After high-sensitivity studies were removed, low heterogeneity was found after remerging (I2 = 22%, P=0.13); therefore, a fixed-effects model was used for analysis. The results revealed there was a statistically significant difference between the acupuncture and the control groups (RR=1.48, 95%CI: 1.40 1.56, Z=13.49, and P<0.00001) (Figure 8). The funnel plot demonstrated asymmetry, indicating publication bias (Figure 9).
Figure 7.
Sensitivity analysis.
Figure 8.
Forest plot of efficacy rate.
Figure 9.
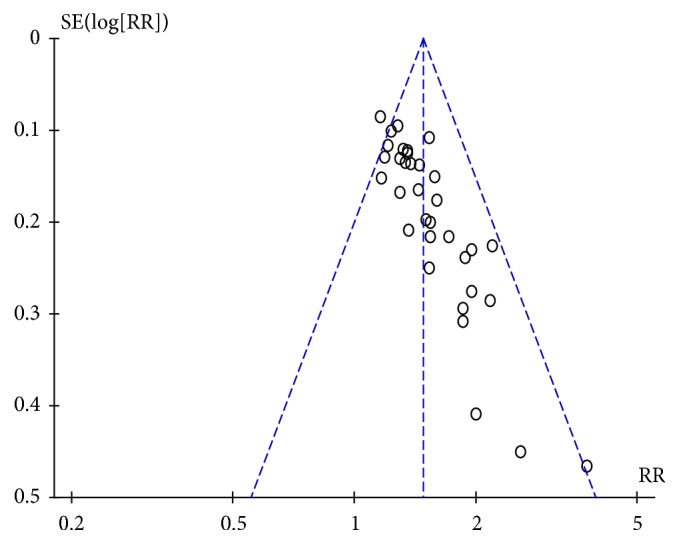
Funnel plot of efficacy rate.
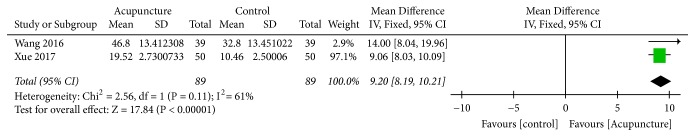
3.7. ADL
Two trials [27, 39] used ADL to assess the curative effect and the continuous data were analyzed. Meta-analysis revealed that the acupuncture group demonstrated significantly improved ADL, with moderate heterogeneity (I2= 61%, P=0.11). The results indicated that improvement of ADL was 9.20 times higher than the control group (MD=9.20, 95% CI: 8.19 10.21, Z=17.84, and P<0.00001) (Figure 10).
Figure 10.
Forest plot of ADL.
3.8. Functional Comprehensive Assessment(FCA)
Among all included studies, FCA was used as an evaluation of neural function recovery in 2 investigations [23, 42]. Both demonstrated a better effect in the acupuncture group compared with the control group; however, the effect was not combined with high heterogeneity (I2 = 97%, P<0.00001).
4. Discussion
The results of the present review suggest that acupuncture may have a beneficial effect on the recovery of consciousness after TBI. According to these findings, acupuncture may improve consciousness levels evaluated using GCS or GOS scores, clinical efficacy, and lower mortality after TBI. Acupuncture may also help in rehabilitation. The mechanism for the beneficial effects of acupuncture in promoting arousal in TBI patients has been investigated in many animal experiments [70–72]. Cheng et al. [36] found that lowering the level of plasma D-dimer may be one of the therapeutic mechanisms of electroacupuncture in recovering consciousness.
However, these positive findings should be interpreted cautiously due to the high risk of bias in all of the included studies, the quality of which was poor overall. Among the 49 studies, the method of randomization was completely described in only 12 trials and incompletely described in 6, whereas the remainder merely only mentioned that “patients were randomized into two groups”. Without appropriate randomization, there is a strong possibility that some of these studies were not actually RCTs. Of all RCTs, only 2 reported blinding and none of allocation, which demonstrated exaggerated treatment effects and limited the reliability of the study results. In addition, only 2 trials reported dropouts and some trials did not report the missing data that led to the exaggerated treatment effects of acupuncture.
Despite the positive results, there were several obvious problems with the trials we analyzed. First, the sample size in many of the studies was too small to draw firm conclusions, and none of the included RCTs reported calculation of sample size. Second, treatment in the control groups could be a major source of bias, especially for clinical efficacy rate, which was subjective. All RCTs compared acupuncture versus basic treatment, and no sham acupuncture or placebo was used; moreover, the patients in these studies were not blinded as to whether they were receiving acupuncture or nonacupuncture. If participants had a preference for acupuncture relative to control treatment, it may have resulted in a greater placebo effect than basic treatment. Third, some trials used acupuncture combined with other interventions in the control group, which resulted in mixed effects and, in turn, made it difficult to evaluate the correlation between differences in acupuncture treatment and its therapeutic effectiveness. Thus, analysis of acupuncture alone or combined with other interventions in the control or experimental groups may increase reliability. Meanwhile, the duration and frequency of acupuncture, acupoint selection and stimulation parameters, and time of electroacupuncture varied among the RCTs, which may have contributed to the heterogeneity among the included trials. Fourth, the duration and grade of TBIs were different in the included trials and not reported in many RCTs, which may have led to different outcomes in clinical efficacy rate, GOS score, and mortality and was an additional source of heterogeneity in the meta-analysis. It has been established that high GCS scores are likely to result in good outcomes, and patients with DOC may regain consciousness more quickly. Fifth, the funnel plot demonstrated asymmetry, indicating potential publication bias against “negative” studies due to journal' preferences for positive research. Moreover, it is difficult to judge whether there were unreported negative research results given the inaccessibility of the study protocols. Adverse events and safety profiles of acupuncture were not reported.
5. Conclusion
To our knowledge, this was the first systematic review and meta-analysis to investigate acupuncture for DOC after TBI. Although the results suggest that acupuncture produced superior effects on the recovery of consciousness in the included trials, the above limitations make this effect questionable and difficult in drawing definitive conclusions. In the future, there is a need for more high-quality studies designed to investigate the rousing effect of acupuncture on patients with TBI. In particular, more effort and attention should be dedicated to improving the quality of studies to enhance internal validity. For example, inclusion criteria, sufficient sample size, truly randomized methods and adequate concealment of allocation, blinding of investigators and participants, and outcome assessors should be unified to minimize performance and assessment bias. Moreover, widely recognized and standardized outcome measurements, such as GCS and GOS, should be adopted to ensure reliability, comparability, and validity and to present results clearly in sufficient detail. Additionally, study protocols and clinical trial registration are an essential part of research. Researchers should be encouraged to devote special attention to monitoring and reporting adverse events regarding acupuncture intervention, quality of life, long-term efficacy, and objective outcomes (such as electroencephalography and functional magnetic resonance imaging). Even if acupuncture demonstrated an effect superior to control in our study, more evidence as to whether it has significant advantages over sham acupuncture at the same acupoints is needed.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (No. 81373800).
Data Availability
The data supporting this systematic review are from previous studies and datasets, which have been cited. The processed data are available from the corresponding author upon request.
Conflicts of Interest
No financial conflicts of interest exist.
References
- 1.Feigin V. L., Theadom A., Barker-Collo S., et al. Incidence of traumatic brain injury in New Zealand: a population-based study. The Lancet Neurology. 2013;12(1):53–64. doi: 10.1016/S1474-4422(12)70262-4. [DOI] [PubMed] [Google Scholar]
- 2.GBD Disease. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Vol. 390. London, England: Lancet; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronado V. G., McGuire L. C., Sarmiento K., et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995-2009. Journal of Safety Research. 2012;43(4):299–307. doi: 10.1016/j.jsr.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Cheng P., Yin P., Ning P., et al. Trends in traumatic brain injury mortality in China, 2006–2013: A population-based longitudinal study. PLoS Medicine. 2017;14(7) doi: 10.1371/journal.pmed.1002332.e1002332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jiang J. Head trauma in China. Injury. 2013;44(11):1453–1457. doi: 10.1016/j.injury.2012.08.045. [DOI] [PubMed] [Google Scholar]
- 6.Taylor C. A., Bell J. M., Breiding M. J., Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveillance Summaries. 2017;66(9):1–16. doi: 10.15585/mmwr.ss6609a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gustavsson A., Svensson M., Jacobi F., et al. Cost of disorders of the brain in Europe 2010. European Neuropsychopharmacology. 2011;21(10):718–779. doi: 10.1016/j.euroneuro.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Olesen J., Gustavsson A., Svensson M., et al. The economic cost of brain disorders in Europe. European Journal of Neurology. 2012;19(1):155–162. doi: 10.1111/j.1468-1331.2011.03590.x. [DOI] [PubMed] [Google Scholar]
- 9.Corso P., Finkelstein E., Miller T., Fiebelkorn I., Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Injury Prevention. 2006;12(4):212–218. doi: 10.1136/ip.2005.010983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stocchetti N., Carbonara M., Citerio G., et al. Severe traumatic brain injury: targeted management in the intensive care unit. The Lancet Neurology. 2017;16(6):452–464. doi: 10.1016/S1474-4422(17)30118-7. [DOI] [PubMed] [Google Scholar]
- 11.Boly M., Massimini M., Garrido M. I., et al. Brain connectivity in disorders of consciousness. Brain Connectivity. 2012;2(1):1–10. doi: 10.1089/brain.2011.0049. [DOI] [PubMed] [Google Scholar]
- 12.Fu T. S., Jing R., Fu W. W., Cusimano M. D., Alexander S. Epidemiological trends of traumatic brain injury identified in the emergency department in a publicly-insured population, 2002-2010. PLoS ONE. 2016;11(1) doi: 10.1371/journal.pone.0145469.e0145469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andriessen T. M. J. C., Horn J., Franschman G., et al. Epidemiology, severity classification, and outcome of moderate and severe traumatic brain injury: a prospective multicenter study. Journal of Neurotrauma. 2011;28(10):2019–2031. doi: 10.1089/neu.2011.2034. [DOI] [PubMed] [Google Scholar]
- 14.Giacino J. T., Fins J. J., Laureys S., Schiff N. D. Disorders of consciousness after acquired brain injury: the state of the science. Nature Reviews Neurology. 2014;10:99–114. doi: 10.1038/nrneurol.2013.279. [DOI] [PubMed] [Google Scholar]
- 15.Gómez P. A., De-La-Cruz J., Lora D., et al. Validation of a prognostic score for early mortality in severe head injury cases. Journal of Neurosurgery. 2014;121(6):1314–1322. doi: 10.3171/2014.7.JNS131874. [DOI] [PubMed] [Google Scholar]
- 16.Ponsford J. L., Spitz G., Cromarty F., Gifford D., Attwood D. Costs of care after traumatic brain injury. Journal of Neurotrauma. 2013;30(17):1498–1505. doi: 10.1089/neu.2012.2843. [DOI] [PubMed] [Google Scholar]
- 17.Spitz G., McKenzie D., Attwood D., Ponsford J. L. Cost prediction following traumatic brain injury: Model development and validation. Journal of Neurology, Neurosurgery & Psychiatry. 2016;87(2):173–180. doi: 10.1136/jnnp-2014-309479. [DOI] [PubMed] [Google Scholar]
- 18.Ma R., Liu X., Clark J., Williams G. M., Doi S. A. The impact of acupuncture on neurological recovery in spinal cord injury: A systematic review and meta-analysis. Journal of Neurotrauma. 2015;32(24):1943–1957. doi: 10.1089/neu.2014.3866. [DOI] [PubMed] [Google Scholar]
- 19.Wong V., Cheuk D. K. L., Lee S., Chu V. Acupuncture for acute management and rehabilitation of traumatic brain injury. Cochrane Database of Systematic Reviews. 2013;3 doi: 10.1002/14651858.CD007700.pub3.CD007700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bin Y., Yan Z. Clinical effect of electroacupuncture on promoting coma in patients with severe craniocerebral injury. Clinical Research. 2018;26:174–175. [Google Scholar]
- 21.Chen X.-Y., Zhu Y., Huang X.-S. Effect of strong stimulation of acupuncture at twelve Jing-well points as main for neurosurgery patients with disorder of consciousness. Zhongguo Zhen Jiu = Chinese Acupuncture & Moxibustion. 2009;29(8):619–622. [PubMed] [Google Scholar]
- 22.Feng R. Xingnao Kai Qiao acupuncture theray combined with stimulative rehabilitation therapy. Chinese Journal of Tissue Engineering Research. 2005;9:172–172. [Google Scholar]
- 23.Fu Y., Cao S., Zhuang J., Hu L., Chen D., Gu F. Observation on electroacupuncture combined with routine western medicine therapy for promoting consciousness of the patient with coma caused by craniocerebral trauma. Chinese Acupuncture Moxibustion. 2009;29:107–110. [PubMed] [Google Scholar]
- 24.Feng B., Zhang X. Study on t-test, analysis of variance and multiple comparisons. Journal of Taiyuan Normal University (Natural Science Edition) 2012;11(4):46–49. [Google Scholar]
- 25.Zhang Y., Chen A., Tang C., Yin H., Chen S. Clinical observation of electroacupuncture for arousing consciousness of comatose patients with severe traumatic brain injury. Acupuncture Research. 2013;38:158–162. [PubMed] [Google Scholar]
- 26.Steinmann H. W. Succinimide und Krampferregbarkeit. Naunyn-Schmiedeberg's Archiv für Experimentelle Pathologie und Pharmakologie. 1964;247(4):316–317. doi: 10.1007/BF02308410. [DOI] [Google Scholar]
- 27.Guangtuan X., Bingcang Y. Clinical observation of acupuncture combined with medicine in the treatment of traumatic brain injury after convalescence Shandong. Journal of Traditional Chinese Medicine. 2017;36:113–115. [Google Scholar]
- 28.Wang Z., Liu Z., Peng X. Arousal effect of needling acupuncture on coma patients with severe traumatic brain injury. Journal of Emergency in Traditional Chinese Medicine. 2016;25:1791–1793. [Google Scholar]
- 29.Tang J. The Clinial Study of Electroacupuncture At Optimal Selection Of Acupoints Combined With Five Sensory Stimulation In Coma After Traumatic Brain Injury. Nanjing University of Chinese Medicine; 2016. [Google Scholar]
- 30.Vos P. E., Diaz-Arrastia R. Traumatic Brain Injury. Chichester, UK: John Wiley & Sons, Ltd; 2014. [DOI] [Google Scholar]
- 31.Zhang B., Wang J., Liu Z., et al. Meta-analysis of the efficacy and safety of therapeutic hypothermia in children with acute traumatic brain injury. World Neurosurgery. 2015;83(4):567–573. doi: 10.1016/j.wneu.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 32.You G., Liao L., Liang H. Effectiveness of comprehensive rehabilitation treatment on the coma patients after traumatic brain injury randomized controlled trial. China Medicine and Pharmacy. 2013;3:12–13. [Google Scholar]
- 33.Zhao H., Yang D., Shi M., Liang J., Yang X., Jin S. Clinical efficacy and safety of Traditional Chinese Medicine combined with Western Medicine in patients with diabetic acute ischemic stroke. Journal of Traditional Chinese Medicine. 2014;34(2):145–149. doi: 10.1016/S0254-6272(14)60068-6. [DOI] [PubMed] [Google Scholar]
- 34.Peng F., Chen Z.-Q., Luo J.-K. Clinical observation on continuous electroacupuncture at Neiguan (PC 6) for arousing consciousness of comatose patients with severe craniocerebral trauma. Zhongguo Zhen Jiu = Chinese Acupuncture & Moxibustion. 2010;30(6):465–468. [PubMed] [Google Scholar]
- 35.Li Z., Sun X., Zhang X., Cao R., Qi B., Liu S. Observation on therapeutic effect of integrated treatment of traditional chinese medicine and western medicine in promoting revival of coma for the patient of severe craniocerebral trauma. Chinese Acupuncture Moxibustion. 2003;23:380–382. [Google Scholar]
- 36.Cheng J. The effects and mechanisms of electroacupuncture on coma degree in patients with severe traumatic brain injury. Shandong Medical Journal. 2016;56:61–62. [Google Scholar]
- 37.Yu M., Liu J., Zhou Y., Song Y. Clinical Observation of Xingnao Kai Qiao acupuncture on coma after traumatic brain injury. Chinese Journal of Integrative Medicine on Cardio-/Cerebrovascular Disease. 2012;10:1471–1473. [Google Scholar]
- 38.Xie X., Cong W., Xu H., Cheng S. The observation on effects of acupuncture on coma patients with traumatic brain injury. Chinese Journal of Traditional Medical Science and Technology. 2016;23:720–721. [Google Scholar]
- 39.Min W. Effects of acupuncture combined with hyperbaric oxygen on patients after traumatic brain injury. Guide of China Medicine. 2016;14:189–190. [Google Scholar]
- 40.Calabria K. E. Battlefield acupuncture effect on chronic sequelae of severe traumatic brain injury. Medical Acupuncture. 2016;28(5):278–282. doi: 10.1089/acu.2016.1200. [DOI] [Google Scholar]
- 41.Jianxia X., Zhihua X., Wei H., Weiping L. Effect of Xingnao Kaiqiao acupuncture on plasma MBP and GFAP levels in patients with severe craniocerebral injury. Modern Journal of Integrated Traditional Chinese and Western Medicine. 2015;24 [Google Scholar]
- 42.Dong D. The Effect of Acupuncture Combined with Chinese Medicine on Rehabilitation in Patients with Traumatic Brain Injury Operation. Anhui University of Traditional Chinese Medicine; 2015. [Google Scholar]
- 43.Zhang X., Wang X. Clinical observation on 78 cases of insomnia from Uganda treated by scalp acupuncture. World Journal of Acupuncture - Moxibustion. 2014;24(1):63–67. doi: 10.1016/S1003-5257(14)60046-5. [DOI] [Google Scholar]
- 44.Wang J., Shi Z. Acupuncture combined with western medicine in the treatment of 50 cases of disorder of consciousness after traumatic brain injury. Chinese Journal of Integrated Traditional and Western Medicine in Intensive and Critical Care. 2012;19:119–119. [Google Scholar]
- 45.Bin T., Yongsheng P., Jiyong S. Observation of acupuncture in the treatment of acute craniocerebral injury. Medical Innovation of China. 2012;09:42–43. [Google Scholar]
- 46.Dan Z., Li H., He X., Wang J., Chen Z. Clinical observation on Xingnao Kaiqiao acupuncture combined with repetitive transcranial magnetic stimulation for post-stroke speech dysfunction. Rehabilitation Medicine. 2017;27(6):p. 15. doi: 10.3724/SP.J.1329.2017.06015. [DOI] [Google Scholar]
- 47.Yang B., Teng J., Huang C. Efficacy observation on hyperbaric oxygen combined with acupuncture treating patients with coma inducd by severe head injury. Modern Diagnosis and Treatment. 2011;22:23–24. [Google Scholar]
- 48.Yu M., Zheng X. Treatment of coma post-severe cerebral trauma by acupuncture and rehabilitation training. Chinese Journal of Neurosurgical Disease Research. 2010;29:p. 6. [Google Scholar]
- 49.Tu X., He Z., Fu X., Chen Y., Kang S. Brain arousal dysfunction in severe craniocerebral injury treated with acupuncture. Chinese Acupuncture Moxibustion. 2010;21:974–976. [PubMed] [Google Scholar]
- 50.Liu J., Yang Z., Wang S., Shi R., Zhu B. Observation on therapeutic effect of electroacupuncture therapy for promoting consciousness of patients with coma. Chinese Acupuncture & Moxibustion. 2010;30:206–208. [PubMed] [Google Scholar]
- 51.Li J. Clinical study of acupuncture combined with Xingnao Kai Qiao. Chinese Journal of Ethnomedicine and Ethnopharmacy. 2010;19:134–134. [Google Scholar]
- 52.Gu Q., Mao Q., Zhang X., Wang S. Effect of compound cuixing liquid combined with brain-resusciatating acupuncture. Journal of Emergency in Traditional Chinese Medicine. 2010;19:1832–1832. [Google Scholar]
- 53.Sun X., Liu S., Li Z. Analysis to the therapeutic efiect of acupuncture for restoring consciousness and inducing resuscitation in promoting revival of coma for the patient of diffuse axonal lnjury. International Journal of Traditional Chinese Medicine. 2009;31:341–342. [Google Scholar]
- 54.Ni G. F., Zhejiang Experimental study on anti-tumor activity of different extracts from Panax japonicus in vitro. Journal of Traditional Chinese Medicine. 2007;42(4):230–231. [Google Scholar]
- 55.Yang X. The clinical research of eieotro-acupuncture treatment on the patients with acute craniocerebrai injury and com. Guangzhou University of Chinese Medecine. 2007 [Google Scholar]
- 56.Liu S., Wang L., Wu Y., Liu Y., Liu J. Clinical study of comprehensive rehabilitation therapy on coma patients with severe craniocerebral injury. Laser Journal. 2006;27:87–87. [Google Scholar]
- 57.Liu S., Tang Y., Guo Q., Luo L., Liu X. The applying of brain resuscitation and enlighten with acupuncture treatment on the further revive of patients with craniocerebral injury and coma. Practical Clinical Medicine. 2006;7:93–95. [Google Scholar]
- 58.Chen Y., Huang L., Chen Y. Clinical research on treatment of severe traumatic brain injury coma by activating blood circulation and inducing resuscitation and refreshing spirit. Journal of Guangxi Medical University. 2006;23:942–944. [Google Scholar]
- 59.Zha X. X., Zuo Y., Liu L. Analysis of mechanical properties of container structure under earthquake action. Journal of South China University of Technology (Natural Science Edition) 2015;7:92–99. [Google Scholar]
- 60.Yuchao Z. Cinical effect of itegrated traditional chinese and western medicine in treating 126 cases of coma after brain injury. China Foreign Medical Treatment. 2014;33:117–118. [Google Scholar]
- 61.Yang X., Ye R.-G., Pei C.-C., Liu G.-X., Li Y.-J. Observational study of Lang Chuang Fang and immunosuppressants in the treatment of lupus nephritis. Chinese Medicine. 2000;35(6):45–46. [Google Scholar]
- 62.Wang X. P. The effect of Angong Niuhuang Pill combined with head electroacupuncture and hyperbaric oxygen therapy on coma patients. Clinical Medicine. 2013;33(4):120–121. [Google Scholar]
- 63.lou M., Luo Y. Effects of acupuncture combined with hyperbaric oxygen on arousal in patients with severe wraniocerebral injury coma. Contemporary Medicine. 2013;19:159–160. [Google Scholar]
- 64.Chen L., Zhu Y., Zhou J., Li C. 39 cases of coma patients with traumatic brain injury treated with combination of traditional chinese and western medicine. Chinese Medicine Modern Distance Education of China. 2013;11:62–63. [Google Scholar]
- 65.He X., Li X. Clinical observation of xingnao kai qiao acupuncture on coma after traumatic brain injury. Chinese Journal of Integratee Chinese and foreign health abstractd Traditional and Western Medicine. 2012;71-72 [Google Scholar]
- 66.Song Y., Zhang L., Zhou Y. Observations on the efficacy of electroacupuncture-assisted treatment for resuscitating coma patients with serious brain trauma. Shanghai Journal of Acupuncture and Moxibustion. 2007;26:11–12. [Google Scholar]
- 67.Yang P., Zhan J. Acupuncture combined with hyperbaric oxygen in the treatment of coma. Chinese Journal of Neurosurgical Disease Research. 2016;15:369–371. [Google Scholar]
- 68.Chen Q. Clinical Observation of the Awakening Effects of Xingnao Kaiqiao Acupuncture Combined with Hyperbaric Oxygen in Coma Patients with Traumatic Brain Injury. Journal Article. 2011;32:1696–1696. [Google Scholar]
- 69.Dongmei Y. The risk model of inventory financing and the system implementation based on Internet of things. Journal of Nanjing University. 2009;5:17–20. [Google Scholar]
- 70.Yao W.-P., Wang S., Han L., Ma J.-Q., Shen Y. Effects of electro-acupuncture at Shuigou (DU26) point on motor evoked potential in rats with cerebral infarction. Journal of Chinese Integrative Medicine. 2010;8(10):979–984. doi: 10.3736/jcim20101011. [DOI] [PubMed] [Google Scholar]
- 71.Chen K., Hu f. Effect of electroacupuncture on Shuigou on expression of excitatory amino acid transporter 1 and γ-amion-butyric acid transporter1 in brian tissue of coma rats model. Shanxi Medical Journal. 2013;42:501–503. [Google Scholar]
- 72.Fu L., Shi H., Chang W., et al. Study on electroacupuncture at Shuigou (GV 26) for treatment of mild and moderate shock :a multicentral and randomized control led trial. Chinese Acupuncture Moxibustion. 2008;28:473–476. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting this systematic review are from previous studies and datasets, which have been cited. The processed data are available from the corresponding author upon request.