Abstract
Purpose
Relentless placoid chorioretinitis (RPC) is a new disease concept that was proposed by Jones et al. in 2000. Some cases of RPC have been reported; however, a treatment strategy has not yet been established. We report herein four cases of patients diagnosed with RPC.
Observations
We experienced four cases of RPC in patients aged 24–51 years. All patients exhibited retinal lesions similar to that seen in acute posterior multifocal placoid pigment epitheliopathy or serpiginous choroiditis from the posterior pole to the surrounding region. Although patients underwent systemic prednisolone (PSL) therapy, recurrence was observed and the retinal scar formation was progressive; they were then diagnosed with RPC. In all cases, cyclosporine (CyA) was administered in addition to PSL, no recurrence was observed thereafter.
Conclusions and Importance
RPC is a rare disease, and a treatment strategy has not yet been established. CyA and PSL combination therapy is considered to be effective in the treatment of RPC.
Keywords: Relentless placoid chorioretinitis, APMPPE, Serpiginous choroiditis, Cyclosporine, Prednisolone
1. Introduction
Relentless placoid chorioretinitis (RPC) is a new clinical entity that was proposed by Jones BE et al. in 2000.1 RPC exhibits fundus and fluorescein angiography findings similar to acute posterior multifocal placoid pigment epitheliopathy (APMPPE) or serpiginous choroiditis (SC); however, its clinical manifestations differ in the following ways: 1) multifocal retinal activity results in the appearance of numerous (>50) lesions, 2) lesions are widespread anterior and posterior to the equator of the fundus, 3) healed lesions involve the superficial choroid, and 4) the clinical course is prolonged with recurrences months to years after initial onset.1 The term ampiginous choroiditis has been used to describe the conditions of such patients.2
The treatment strategy for RPC has not yet been established. Thus far, some cases of RPC have been reported,1,3, 4, 5, 6, 7, 8, 9, 10, 11, 12 most of which were refractory to prednisolone (PSL) administration and were recurrent. Only a few cases were reported as treated with cyclosporine (CyA)1 or mycophenolate mofetil,6 and the efficacy of these treatments is not known. Herein, we report four cases in which patients were diagnosed with RPC, and cyclosporine and prednisolone combination therapy was considered to be effective.
The study was a retrospective observational study and was approved by the ethics committee of Hokkaido University Hospital (approval number 015–0327) and carried out in accordance with the Declaration of Helsinki and Ethical Guideline for Clinical Studies stipulated by the Ministry of Health, Labor and Welfare, Japan.
2. Findings
2.1. Case 1
A 29-year-old man weighing 87.6 kg and suffering for 1 week from slight occipital headaches, blurred vision, and hyperemia in his right eye (OD) visited our hospital. The patient had no significant past medical history or drug allergies, and had no significant travel history. At the initial visit, best-corrected visual acuity (BCVA) was 0.2 OD and 1.2 in his left eye (OS). Slit-lamp examination showed trace flare and 2 + cells in the anterior chamber (AC) with keratic precipitates and anterior vitreous cells OD, whereas no inflammatory findings were seen OS in the anterior segment.
Funduscopic examination showed numerous placoid lesions that appeared to be mixed with fresh and old scar lesions in both eyes (OU). No obvious vitreous opacity was seen OU. Fresh lesions with multiple yellowish-white placoid exudates were scattered from the posterior pole to the periphery, and old scar lesions were also scattered with multiple granular and placoid scar lesions (Fig. 1a). Fresh lesions involved the fovea OD. Fluorescein angiography (FA) revealed hypofluorescence in the early phase and hyperfluorescence in the late phase, which were consistent with the fresh lesions (Fig. 1b and c). FA also showed hypofluorescence rimmed with hyperfluorescence, which was consistent with old scar lesions. In indocyanine green angiography (ICGA), areas corresponding to both fresh lesions and old scar lesions were hypofluorescence from early to late phase. Optical coherence tomography (OCT) revealed that the ellipsoid zone (EZ) and the interdigitation zone (IDZ) were not identified under either the old or fresh lesions and that they showed some small retinal pigment epithelium detachments. Blood examinations including syphilis lipid antigen (rapid plasma reagin; RPR) and treponema antigen (treponema pallidum Latex immuno Assay; TPLA) and QuantiFERON-TB Gold® were all negative. The examination of cerebrospinal fluid showed pleocytosis (22 cells/μl), but any extraocular symptoms were not observed.
Fig. 1.
Fundus of Case 1 OD. At the first visit numerous placoid lesions mixed with fresh lesions (white arrowhead) and old scar lesions were scattered from the posterior pole to the peripheral retina (a). In fluorescein angiography these fresh lesions were the hypofluorescence in the early phase (116 seconds) (b) and the hyperfluorescence in the late phase (406 seconds) (c) (white arrowhead). In contrast, scar lesions were the hypofluorescence surrounded by hyperfluorescence with no late leakage.
Although fundus and FA findings appeared similar to APMPPE or serpiginous choroiditis (SC), this case was atypical for these diseases in the following ways: 1) there was a large amount of exudate, 2) there was widely spread exudate, and 3) to some extent, the exudate was accompanied by anterior segment inflammation. With these findings, RPC (rather than APMPPE) was strongly suspected. Because fresh lesions involved macular area OD, steroid pulse therapy (3 days of 1000 mg/day methylprednisolone, followed by 60 mg/day PSL) was administered. Ten days later, fresh lesions were resolved, some of which changed to scar lesions, and BCVA was recovered to 0.4 OD (Fig. 2a). With the gradually tapering dose of PSL treatment, BCVA was improved to 0.6 OD 1 month later.
Fig. 2.
Fundus of Case 1 OD after steroid pulse therapy. Fresh lesions were resolved with steroid pulse therapy, and some of them changed to scar lesions (a). However, two months from the initial visit, recurrence was seen OD. New white retinal lesions appeared in the temporal macula OD (b).
However, recurrence was seen 2 months after the initial visit when the dose of PSL was decreased to 15mg/day. Whereas visual acuity was well recovered, BCVA was 1.2 OD and 1.5 OS, and inflammatory findings in the AC and anterior vitreous were not observed, new fresh retinal lesions appeared in the temporal macula OD (Fig. 2b). Forty mg of a sub-Tenon's injection of triamcinolone acetonide (STTA) were administered along with the oral PSL. These lesions disappeared 1 month later.
Eleven months after the initial visit, a second recurrence was seen when the dose of PSL was 7.5 mg/day. Along with the appearance of anterior vitreous cells, new retinal lesions appeared OS, scattered in the temporal macula. We administered CyA 250 mg/day along with PSL maintained at 7.5mg. Since then, slight recurrences with small peripheral retinal exudates were sometimes seen, however, no severe recurrences resulting in the enlargement of chorioretinal degeneration have not been seen for 48 months, and the dose of PSL and CYA could be reduced to 1 mg/day and 200 mg/day respectively. The patient has kept his BCVA at 1.0 OD and 1.2 OS.
2.2. Case 2
A 24-year-old man weighing 56 kg complained of blurred vision OU starting 4 days before his initial visit to our hospital. The patient had no significant past medical history or drug allergies, and had no significant travel history. At the initial visit, BCVA was found to be 0.3 OD and 0.1 OS. Slit-lamp examination demonstrated a clear AC. Funduscopic examination revealed scattered white placoid lesions, which seemed to be fresh, from the posterior pole to the peripheral fundus with numerous scattered scar lesions OU (Fig. 3). No obvious vitreous opacity was seen OU.
Fig. 3.
Fundus of Case 2 at the first visit. Multiple white placoid fresh lesions and scar lesions were seen OU at the first visit. They changed to scar lesions after the corticosteroid therapy.
FA revealed early hypofluorescence, followed by late hyperfluorescence consistent with the white lesions and hypofluorescence that was consistent with scar lesions. ICGA showed hypofluorescent dark areas from early to late phase. OCT revealed indistinct EZ and IDZ, which were consistent with the white placoid lesions, and the presence of a slight serous retinal detachment. The examination of cerebrospinal fluid showed slight pleocytosis (7 cells/μl). Blood examinations including syphilis lipid antigen (rapid plasma reagin; RPR) and treponema antigen (treponema pallidum Latex immuno Assay; TPLA) and QuantiFERON-TB Gold® were all negative.
RPC was considered in this case because of the numerous lesions that had spread widely from the posterior pole to the anterior retina. Because of the marked decrease in BCVA OU, steroid pulse therapy (3 days of 1000 mg/day methylprednisolone, followed by 60 mg/day PSL) was administered. Two weeks after the initial presentation, funduscopic examination revealed that placoid fresh lesions had resolved with the remaining scar formations, and BCVA had recovered to 0.9 OD and 0.3 OS. However, a recurrence was observed 3 weeks after the initial presentation when the dose of PSL was 30 mg/day. BCVA was 0.9 OD and 0.6 OS. Although AC was clear and no vitreous opacity was seen, 1 + anterior vitreous cells were observed OS. Fresh retinal lesions were observed in the peripheral fundi OU (with OD being worse than OS). With 40 mg of STTA OD and PSL to 40mg/day, these fresh lesions were resolved with scarring remaining.
Thereafter, during the decreasing dose of PSL, the patient showed the third and the fourth recurrence. The patient demonstrated fresh placoid retinal lesions within 2 months and required an increased dose of PSL each time. Therefore, CyA was initiated at a dose of 200 mg/day in addition to PSL. The patients showed slight recurrences with peripheral retinal exudates OS 8 months later, however, since then, no recurrences with retinal lesions have not been observed for 42 months. Dose of PSL could be reduced and be stopped, and dose of CyA also could be reduced to 125mg/day. Afterward, the patients showed only anterior segment inflammation OS once without posterior segment inflammation. The patient has kept his BCVA at 1.2 OD and 1.2 OS.
2.3. Case 3
A 43-year-old man weighing 85 kg had a history of uveitis showing iridocyclitis and PC scar like chorioretinal scar OD 3 years ago, and he showed relapse of iridocyclitis 2 year ago. He visited an eye clinic complained of redness of the eye OS and he was referred to our hospital with the treatment with 0.1% betamethasone eye drop. The patient had no significant past medical history or drug allergies, and had no significant travel history.
At the initial visit, BCVA was 1.2 OU. Slit-lamp examination demonstrated a trace flare & occasional cells OD and 1 + flare & 1 + cells OS in AC. Almost total posterior iris synechia was seen OD. Funduscopic examination revealed the presence of numerous scattered scar lesions accompanied with fresh white lesions without vitreous opacity OU. (Fig. 4a). FA demonstrated early hypofluorescence followed by late hyperfluorescence that was consistent with the white lesions. ICGA showed hypofluorescent dark areas from early to late phase. Blood examinations including RPR、TPLA and T-SPOT. TB® were all negative. These white lesions were seen in macular area OD, therefore, 40mg of STTA OD was performed, and administration of oral PSL 15mg/day was started. White lesions were resolved with scarring remaining.
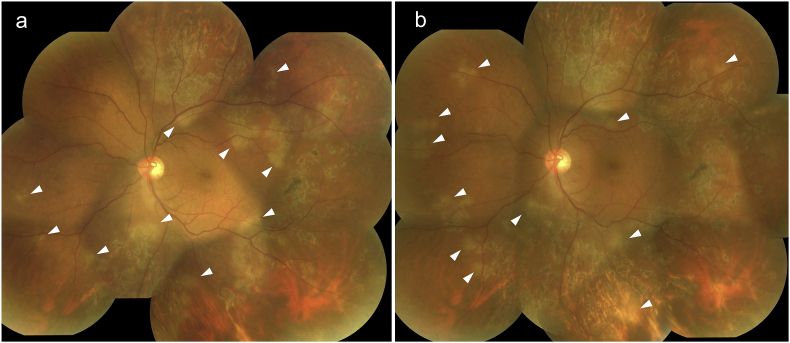
Fig. 4.
Fundus of Case 3 at the first visit. Numerous scattered scar lesions accompanied with fresh white lesions (white arrowhead) were seen at the initial visit OS (a). (Numerous scattered scar lesions accompanied with fresh white lesions were also seen OD, however, fundus photograph OD could not be taken due to the posterior iris synechia.) Two month later, new white chorioretinal lesions (white arrowhead) appeared in addition to old scar lesions OS (b).
Two month later, although he was not aware any changes in vision, new white chorioretinal lesions were seen in addition to old scar lesions OS (Fig. 4b).
Because numerous lesions that had spread widely in the ocular fundus were seen and he showed the recurrence rapidly even with systemic steroid therapy, RPC was considered.
Therefore, 250 mg/day of CyA was administered in addition to 30mg/day of PSL. For the past 8 months, no recurrences have been seen, and dose of PSL and CYA could be reduced to 10 mg/day and 200mg/day respectively. The patient has kept his BCVA at 1.2 OU.
2.4. Case 4
A 51-year-old woman weighing 60 kg complaining of ocular pain and hyperemia OU over a 2-day period visited our hospital. She had no medical history except for sudden hearing loss of her left ear, and had no significant travel history. At the initial visit, BCVA was 0.02 OD and hand motion OS. She showed severe AC inflammation with 3 + cells, hypopyon and fibrin formation along with partial posterior synechia OU (Fig. 5). Vitreous opacity was also observed OU. Numerous white placoid chorioretinal lesions were scattered from the macula to the mid-peripheral fundi OU.
Fig. 5.
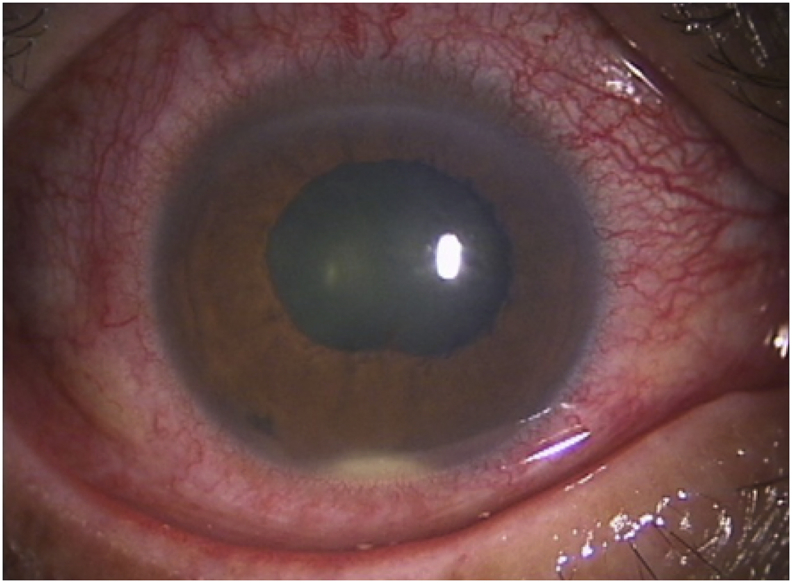
Slit-lamp image of Case 4 at the first visit. Hypopyon along with fibrin formation was seen in the anterior chamber OU (photo shows right eye).
FA demonstrated early hypofluorescence followed by late hyperfluorescence that was consistent with the white lesions. ICGA showed hypofluorescent dark areas from early to late phase. OCT revealed the presence of cystoid macular edema with a slight serous retinal detachment. Blood examinations including RPR、TPLA were all negative. The examination of cerebrospinal didn't show pleocytosis. With 60 mg/day of PSL, all inflammatory findings were resolved and most white placoid lesions disappeared OU. BCVA recovered to 1.0 OD and 0.8 OS.
Eight months after the initial presentation, when PSL doses were gradually decreased to 2.5 mg/day, the first recurrence was observed. BCVA was 1.0 OD and 0.5 OS. AC inflammation with 2 + cells were observed OU. Numerous white placoid chorioretinal lesions appeared again in the mid-to-peripheral fundus OU. OCT revealed the presence of serous retinal detachments in the macular area OU. With the dose of PSL increased to 30 mg/day, although scar formations remained, the white placoid chorioretinal lesions were resolved 2 weeks later.
Thereafter, the patient developed several recurrences when the dose of PSL decreased to 2.5–5.0 mg/day; the dose of PSL was increased to 30 mg/day in each recurrence. Consequently, orange color chorioretinal scar lesions were widely spread from the posterior pole to the peripheral retina (Fig. 6).
Fig. 6.
Fundus of Case 4 after several recurrences. Numerous orange color chorioretinal scars were widely spread from the posterior pole to peripheral retina OU. Right eye (a), Left eye (b).
In addition to the increased PSL dose (20 mg/day), 170 mg/day of CyA was initiated with the seventh recurrence. Since then, recurrences with chorioretinal lesions have not been observed for 44 months whereas 3 times of slight recurrences with anterior chamber cells and vitreous haze were observed in the period. The dose of PSL and CyA could be reduced to 7.5 mg/day and 150 mg/day respectively. The patient has kept her BCVA at 1.2 OU.
3. Results
Recurrences were seen in this series of 4 RPC cases when they were treated with PSL alone. In all cases, after CyA combined with PSL was administered no severe recurrences have been observed for 8–48 months, and the dose of PSL could be reduced.
4. Discussion
All four cases exhibited placoid chorioretinal white lesions scattering from the posterior pole to peripheral retina, and part of them changed to scar lesions similar to those seen in APMPPE or SC; however, because all cases were refractory to steroid therapy alone and showed recurrences resulting in expanding of retinal scar lesions, it is believed that the diagnosis of RPC in these cases were reasonable and proper.
Since Jones et al. proposed the concept of RPC in 2000, a number of cases have been reported1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11; however, the shape of chorioretinal infiltrates and the clinical course differed in each case. Therefore, RPC cannot be truly considered to have been established as a single disease concept.
Pathogenesis of this disease is still not clear. Two of our four cases presented with pleocytosis, indicating the presence of meningitis; however, fundus findings apparently differed from Vogt-Koyanagi-Harada (VKH) disease in which pleocytosis is associated with a high rate, and none of the extraocular findings that accompany VKH disease were observed in the subsequent course. It is possible that some types of viral infections related to the development of meningitis may relate to the onset of RPC. We examined laboratory work up for syphilis and tuberculosis in every cases, but we did not have the positive result.
As there is the term “relentless” in the name of RPC, this disease is difficult to be controlled with PSL alone. In previous reports, some additional medicine has been used in combination with PSL. CyA 100–150 mg/day was started and PSL could be tapered off without any recurrences in two cases.1 In other cases, mycophenolate mofetil 1000–2000 mg/day was administrated with PSL, and no recurrence was observed for 15–18 months.4,6
CyA is a most common T-cell-specific immunosuppressant and has been used for tissue transplantation and for autoimmune diseases all over the world. In this study CyA in combination with PSL was administered in all 4 cases that were refractory to PSL monotherapy, and after starting the combination therapy recurrence has not been observed and dose of PSL could be reduced successfully in all cases. CyA and PSL combination therapy is considered to be a potential therapeutic strategy for RPC. We examined only CyA this time, however, recently the efficacy of biologics including infliximab and adalimumab or other immunosuppressants including micofenorate mofetil for non-inflectious uveitis have been reported, and they may be good candidates as the therapeutic agents for RPC. The examination about them is the subject for future analysis.
5. Conclusions
RPC is a refractory disease to PSL monotherapy. CyA and PSL combination therapy is the considerable treatment for RPC showing recurrences.
6. Patients consent
Institutional review board approved this retrospective case report. Consent to publish the case report was not obtained. This report does not contain any personal information that could lead to the identification of the patient.
Conflicts of Interest
The following authors have no financial disclosures: KU, KN, KM, DI, SO, NK, SI.
7. Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Funding
No funding or grant support
Acknowledgements
None.
References
- 1.Jones B.E., Jampol L.M., Yannuzzi L.A. Relentless placoid chorioretinitis. Arch Ophthalmol. 2000;118(1):931–938. [PubMed] [Google Scholar]
- 2.Nussenblatt R., Whitcup S.P.A. second ed. 1996. Uveitis: Fundamentals and Clinical Practice. [Google Scholar]
- 3.Orihara T., Wakabayashi T., Okada A.A. A young Japanese man with relentless placoid chorioretinitis. Jpn J Ophthalmol. 2005;49:539–542. doi: 10.1007/s10384-005-0241-9. [DOI] [PubMed] [Google Scholar]
- 4.Amer R., Florescu T. Optical coherence tomography in relentless placoid chorioretinitis. Clin Exp Ophthalmol. 2008;36(4):388–390. doi: 10.1111/j.1442-9071.2008.01773.x. [DOI] [PubMed] [Google Scholar]
- 5.Chen E. Relentless placoid chorioretinitis. Ophthalmic Surg Laser Imag. 2008;40:87–88. doi: 10.3928/15428877-20090101-03. [DOI] [PubMed] [Google Scholar]
- 6.Yeh S., Lew J.C., Wong W.T., Nussenblatt R.B. Relentless placoid chorioretinitis associated with central nervous system lesions treated with mycophenolate mofetil. Arch Ophthalmol. 2009;127:341–343. doi: 10.1001/archophthalmol.2009.12. [DOI] [PubMed] [Google Scholar]
- 7.Jyotirmay B., Jafferji S.S., Sudharshan S. Clinical profile, treatment, and visual outcome of ampiginous choroiditis. Ocul Immunol Inflamm. 2010;18(1):46–51. doi: 10.3109/09273940903402637. [DOI] [PubMed] [Google Scholar]
- 8.Khalifa Y.M., Monahan P.M., Acharya N.R. Ampiginous choroiditis following quadrivalent human papilloma virus vaccine. Br J Ophthalmol. 2010;94(1):137–139. doi: 10.1136/bjo.2009.159293. [DOI] [PubMed] [Google Scholar]
- 9.Bhuibhar S.S., Biswas J. Nested PCR-positive tubercular ampiginous choroiditis: a case report. Ocul Immunol Inflamm. 2012;20(4):303–305. doi: 10.3109/09273948.2012.685684. [DOI] [PubMed] [Google Scholar]
- 10.Mirza R. Relentless placoid chorioretinitis. Int Ophthalmol Clin. 2012;52:237–242. doi: 10.1097/IIO.0b013e31826686a3. [DOI] [PubMed] [Google Scholar]
- 11.Patel M., Vavvas D.G. Fundus autofluorescence in ampiginous choroiditis. Ophthalmic Surg Lasers Imaging Retina. 2013;44(4):393–397. doi: 10.3928/23258160-20130715-10. [DOI] [PubMed] [Google Scholar]
- 12.Veronese C., Marcheggiani E.B., Tassi F. Early autofluorescence findings of relentless placoid chorioretinitis. Retina. 2014;34(3):625–627. doi: 10.1097/IAE.0b013e3182a487d5. [DOI] [PubMed] [Google Scholar]