Abstract
Health care-associated infections (HAIs) and antimicrobial resistance constitute a major public health challenge. The aim of this study was to assess the prevalence rate of HAIs and antimicrobial use in acute care hospitals in Kosovo. A multicenter study was performed in all hospitals in Kosovo. The standardized protocol for Point Prevalence Survey (PPS) on HAIs and antimicrobial use developed by European Center for Disease Control and Prevention (ECDC) was used for this survey. A total of 915 patients were included in PPS. Countrywide prevalence rate of HAIs was 4.9%. The highest rate was noticed in tertiary care level in University Clinical Centre of Kosovo (UCCK) (7.2%). The most common type of HAI was surgical site infection, representing 35.5% of all reported HAIs. Prevalence of HAIs was highest in surgical departments (46.6%). The median length of stay before onset of HAI was 11 days (range: 3-27 days). Gram negative bacteria were the predominant microorganisms (61% of cases). From all patients, 520 (56.8%) of them were using at least one antibiotic. Ceftriaxone was the most prescribed antibiotic with 40.3%. Antibiotics were administered mainly through parenteral route (93.8%). Empiric treatment was the physician’s choice for prescribing in 87.1%. The main reason for antibiotic treatment was pneumonia (19.8%). Medical prophylaxis was reported in 10% of antibiotic prescriptions. Key recommendations driven by this study are to improve surveillance systems of HAI and antibiotic use, enhance infection prevention and control and establish antimicrobial stewardship program.
Key words: Health care-associated infections, antibiotic use, point prevalence survey, Kosovo
Introduction
Health care-associated infections (HCAIs) and antimicrobial resistance constitute a major public health problem worldwide. They result in high morbidity and mortality, prolonged hospital stays, increased use of antibiotics and increased costs.1,2 In developing countries this challenge is more prevalent because disease prevention and control policies are either absent, poorly adapted or insufficiently funded by governments.3
Kosovo, with a population of 1.7 million inhabitants is located in the south-east of Europe in the Western Balkans region. Health care in Kosovo underwent important reforms in the last decade facing many challenges, of which the most important are lack of political commitment and limited resources.4 The budget for the healthcare system in Kosovo for the year 2015 was only 160 million Euro (80 Euro/per capita).5
Infection control in Kosovo is still at the beginning of its journey. As in other developing countries, common problems in the field of infection control in Kosovo are lack of financial support, lack of political commitment, inadequate number of trained personnel working in infection control, overcrowded wards, and insufficient equipment and supplies.6 This can result in inappropriate infection control and a high HCAI rate. The first descriptive prevalence study on HCAIs in targeted high-risk areas in the University Clinical Centre of Kosovo (UCCK) conducted during 2003 with 167 patients surveyed, showed an overall prevalence rate of 17.4%.7 Patients with HCAIs had on average 13.2-22 extra days of stay at hospital. Other Point Prevalence Surveys (PPS) in central intensive care unit (ICU) within UCCK were conducted three times during 2006, 2008 and 2009. On the last survey, of 16 patients surveyed, 11 patients had a total of 18 HCAI, of which ventilator associated pneumonia was diagnosed in 8 patients.8
Antimicrobial resistance is another challenge closely related to HCAIs. Inappropriate use of antimicrobials is the most important cause of the emergence and spread of resistant microorganisms in the community and hospitals.9,10 Consumption and resistance are tending towards escalation in many countries of Europe, particularly in Eastern and Central Europe. Kosovo ranks high in the total consumption of antibiotics in Europe, with a wholesale level of 26.3 DDD (Defined Daily Doses/1000 inhabitants/day); holds sixth place for cephalosporin consumption (DDD 4.0) and is the European champion with the highest proportional total parenteral use of ceftriaxone.11,12 The resistance rates of all microorganisms to antibiotics tested in susceptibility testing in Kosovo is 2-5 fold higher compared to average rates in the European Antimicrobial Resistance Surveillance Network (EARS-Net), except for vancomycin resistant Enterococci.12 Finally, no evidence-based guidelines for the treatment of infectious diseases are yet available in Kosovo.
Point-prevalence surveys have been used to provide information about the burden of HCAIs and antimicrobial use. They represent a simple and feasible way to collect data on HCAIs and antimicrobial use at hospital level and have been successfully implemented in many countries worldwide.13-16
The objectives of this study were to estimate the prevalence rates and main features of HCAIs and antimicrobial use in acute care hospitals in Kosovo and to identify the main targets for quality improvements.
Materials and Methods
Settings
Surveillance was performed in all 7 hospitals in Kosovo during 2016. Patients were surveyed in 6 regional hospitals and in UCCK, which is the only referral tertiary care center with approximately 90,000 admissions per year. The 7 participating hospitals had a total of 4031 beds (mean, 575 beds; range, 75-2032 beds). One hospital was a tertiary care hospital with 2032 beds and 6 were secondary care hospitals with 2299 beds in total.
Data collection: Point prevalence survey
The standardized protocol for a combined Point Prevalence Survey (PPS) on healthcare-associated infections (HCAIs) and antimicrobial use developed by European center for Disease Control and Prevention (ECDC) was used for this survey.17
All patients registered on the ward before 8:00 a.m. and not discharged from the ward at the time of the survey were assessed. All acute care units were included, whereas long-term care units, emergency departments, patients admitted to same-day treatment or surgery, the outpatient departments and dialysis were excluded from the survey.
Data were collected in a single day for each ward/unit. This was a single day point prevalence survey that occurred in all hospitals in Kosovo. However, due to some delays collecting data in the university hospital in Prishtina, collection took place over a three days period.
Two data collection protocols were used by participating hospitals. The first one was patient-based and covered denominator data, including risk factors for each individual patient no matter if the patient had a HCAI and/or received antimicrobials. The patient form for this protocol also included more detailed information, such as the presence of invasive devices, the specialty area of the patient’s disease or consultant in charge of the patient and the McCabe score that classifies the severity of underlying medical conditions.
The second protocol was unit-based, where the denominator data were aggregated at ward level, and a patient form was used only for patients with a HCAI and/or receiving antimicrobials. For both protocols, data were also collected at both ward level (ward name and specialty) and hospital level, including hospital type, size and whether or not any wards were excluded from the survey. Alcohol hand rub consumption was reported as the number of liters per 1000 patient-days.
Data collection was carried out by staff experienced in reading patient charts/notes and in identification of HAIs’ (two infection control nurses, one clinical microbiologist, one surgeon, two anesthesiologists and two epidemiologists). Data collectors were previously trained over two days by the national PPS coordinators to become familiar with protocol and case definition. They also collaborated with the clinical team in charge of patient care in each ward. The competency of data collectors was assessed during the training and after the data collection through the random reevaluation of the completed forms.
Data were collected for patients showing an active HAI on the day of the survey. An HCAI was defined as active when: signs and symptoms fulfilled the survey definitions of HCAI and were present on the survey date or signs and symptoms fulfilling the survey definitions of HCAI had been present in the past and the patient was still receiving treatment on the survey date.17
The antimicrobial-related information was only collected if the patient was receiving antimicrobials at the time of the survey or alternatively had an active HCAI. The drugs included the Anatomical Therapeutic Chemical (ATC) classes J01 (antibacterials), J02 (antifungals) and J04 (anti-mycobacterials). The route of administration was also recorded. The usage of systemic antimicrobials was noted for the following infections: community-acquired infection, acute hospital acquired infection, surgical prophylaxis (any single dose of an antimicrobial agent given within the 24hour period before 8:00 am on the day of the survey), medical prophylaxis, other indications and unknown indication/reason assessed during PPS. Dosage and timing for antimicrobials were not collected. Antiviral agents and antimicrobials for the treatment of tuberculosis were not included.
The study was conducted after ethical approval with Decision No 2257, date 17.11.2015 by the Management Board of the Hospital and University Clinical Service of Kosovo.
Results
A total of 915 patients were included in PPS. Fifty-eight patients were infants aged 0-10 months and 498 (54.4%) were females. Overall, forty-five patients had one HCAI; the countrywide prevalence rate of HCAIs was 4.9%. The highest rate was noticed in tertiary care level in UCCK (7.2%), followed by regional hospitals in Peja (5.6%) and Gjakova (2.4%). No cases of HCAI were registered in the smallest hospitals – Ferizaj and Mitrovica. The prevalence of HCAIs in regional hospitals was 2.1%.
Table 1 shows that more than half of patients enrolled in the survey came from Prishtina (54.3%), followed by Prizren and Gjilan, (each representing 10.6%) and Peja (9.6%). The smallest hospital participating in survey was Ferizaj hospital and the largest one UCCK in Prishtina. Overall bed occupancy rate during the year 2015 in Kosovo hospitals was 60%. At the UCCK it was 65.7% and in all other hospitals 53.3%. The lowest rate was noticed in Ferizaj-41.6%.
Table 1.
Point prevalence survey (PPS) of healthcare associated infections (HAI) in Kosovo. Results by hospital.
| Hospital | Surveyed patients | Patients with HAI | ||
|---|---|---|---|---|
| N. | % | N. | % | |
| Prishtina | 497 | 54.32 | 36 | 7.2 |
| Peja | 88 | 9.61 | 5 | 5.6 |
| Gjakova | 81 | 8.85 | 2 | 2.4 |
| Gjilan | 97 | 10.6 | 1 | 1 |
| Prizren | 97 | 10.6 | 1 | 1 |
| Ferizaj | 16 | 1.74 | 0 | 0 |
| Mitrovica | 39 | 4.26 | 0 | 0 |
| Total | 915 | 100 | 45 | 4.9 |
Fifty hundred and fifty-one patients were hospitalized in medical wards (60.2%), 326 in surgical wards(35.6%) and 38 (4.1 %) in intensive care units (ICUs). The prevalence of HCAIs was highest in surgical wards (21 patients- 46.6%), followed by 15 patients in ICUs (33.3%) and medical wards, in which nine cases were registered (20%).
The most common type of HCAI was surgical site infection, accounting for 35.5% of all reported HCAIs (Table 2). The second most frequently reported type of HCAI was bloodstream infection (33.3%), followed by urinary tract infection (20%). Three patients had ventilator associated pneumonia and two of them gastrointestinal infections.
Table 2.
Distribution of microorganisms isolated in healthcare-associated infections (HAI), by main type of infection.
| All types, n. (%) | Pneumonia/other respiratory tract | Infection Surgical site | Urinary tract | Blood stream | Gastrointestinal | |
|---|---|---|---|---|---|---|
| HAIs and microorganisms | ||||||
| HAIs, total | 45 (4.9) | 3 | 16 | 9 | 15 | 2 |
| HAIs with microorganisms | 33 (3.6) | 3 | 11 | 7 | 11 | 1 |
| Microorganisms | ||||||
| Escherichia coli | 6 (19.3) | 0 | 2 | 2 | 2 | 0 |
| Pseudomonas aeruginosa | 2 (6.4) | 0 | 1 | 1 | 0 | 0 |
| Citrobacter | 1 (3.2) | 0 | 0 | 0 | 1 | 0 |
| Acinetobacter | 5 (16.1) | 0 | 1 | 0 | 4 | 0 |
| Klebsiella | 7 (22.5) | 3 | 1 | 0 | 3 | 0 |
| Proteus mirabilis | 1 (3.2) | 0 | 1 | 0 | 0 | 0 |
| Enterococcus fecalis | 3 (9.6) | 0 | 1 | 2 | 0 | 0 |
| Staphylococcus aureus | 5 (16.1) | 0 | 4 | 1 | 0 | 0 |
| Staphylococcus spp. | 1 (3.2) | 0 | 0 | 0 | 0 | 1 |
| Staphylococcus epidermidis | 1 (3.2) | 0 | 0 | 1 | 0 | 0 |
| Staphylococcus pneumoniae | 1 (3.2) | 0 | 0 | 0 | 1 | 0 |
The median length of stay of patients with an HAI was 11 days until onset of infection (range 3-27 days) and 15 days until the time of the survey, whereas the median length of stay until survey date for patients without an HAI was six days.
Positive microbiology results were available in 33 HCAI cases (73.3%). Gram negative bacteria were the predominant microorganisms isolated in 61% of cases. Overall, the most commonly isolated microorganism was Klebsiella pneumoniae (22.5% overall, and predominant in VAP), followed by Escherichia coli (19.3%, equally represented in UTI, SSI and BSI) and S.aureus (16.1%, mainly in surgical site infections).
A peripheral vascular catheter was present in 70.6% of patients, ranging between 6.2% in Ferizaj and 63.9% in Prishtina. Urinary tract catheters were present in 15% of patients, ranging from 12.3% in Prizren to 28.4% in Peja. Only 1.5% of patients were on mechanical ventilation and 1.3% had central vascular catheters at the time of the survey and all were hospitalized at the UCCK. All UTIs were occurring in patients with urinary catheter and all patients with BSIs had at least one invasive device in situ within for at least 48-hours.
Alcohol hand rub consumption data were provided by 6 hospitals. The total annual consumption was 10524.5 liters, varying from 265.5 liters in Gjilan to 6180 liters in Prishtina. The median alcohol hand rub consumption was 11.9 liters per 1000 patient-days. It was highest in UCCK - 12.5 liters per 1000 patient-days and lowest in Gjilan hospital with only 4.1 liters per 1000 patient-days.
In the field of antimicrobial consumption, from 915 patients included in the survey, 520 (56.8%) were using at least one antibiotic on the day of survey. Among the patients receiving at least one antibiotic, 339 (65.2%) out of 520 were given a single antibiotic agent, 156 patients (30%) received two antibiotic agents and 25 (4.8%) received three antibiotics. A large variation among hospitals is seen in antibiotic consumption, ranging from 34.7% in Gjilan and 56.4% in Peja hospital. In UCCK 34.8% of surveyed patients received antibiotics.
Ceftriaxone was the most prescribed antibiotic (40.3%), followed by oral metronidazole (11.9%) and gentamicin (11.6%). Other antibiotics were prescribed in smaller percentages (Figure 1).
Figure 1.
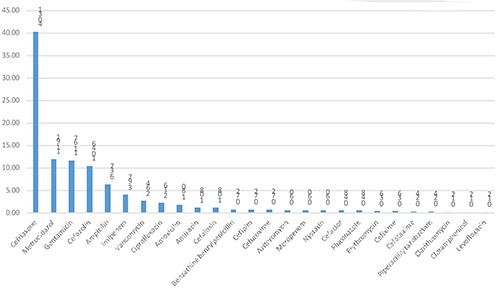
Overall antimicrobial usage percentage in Kosovo hospitals.
Two main indications reported for antibiotic prescription were community acquired infection (36% of cases) and surgical prophylaxis (32% of cases). Duration of surgical prophylaxis was more than one day in all recorded cases (range 2-4 days). Medical prophylaxis was reported in 10% of cases and other indications were reported in very small percentages.
Third generation cephalosporins were the most prescribed antibiotics for empiric treatment (34.6%), surgical prophylaxis (43.1%) and medical prophylaxis (54.1%), followed by aminoglycosides (Table 3).
Table 3.
Indications for antibiotic use.
| Antimicrobial agents, total | Indications, n (%) | Treatment, n (%) | Surgical prophylaxis, n (%) |
Medical prophylaxis, n (%) |
|---|---|---|---|---|
| Top antimicrobial agents at ATC 4th level | 835(100) | 393(100) | 322(100) | 120(100) |
| Third-generation cephalosporins (J01DD) | 340 (40.71) | 136 (34.60) | 139 (43.16) | 65 (54.16) |
| Aminoglycosides (J01GB) | 106 (12.69) | 43 (10.94) | 50 (15.52) | 13 (10.83) |
| Nitroimidazole derivates (P01AB) | 99 (11.85) | 49 (12.46) | 50 (15.52) | / |
| First-generation cephalosporins (J01DB) | 96 (11.49) | 43 (10.94) | 46 (14.28) | 7 (5.83) |
| Combinations of penicillins, incl.β-lactamase inhibitors (J01CR) | 70 (8.38) | 43 (10.94) | 13 (4.03) | 14 (11.66) |
| Carbapenems (J01DH) | 38 (4.55) | 26 (6.61) | 6 (1.86) | 6 (5.0) |
| Glycopeptide antibacterials (J01XA) | 22 (2.63) | 15 (3.81) | 5 (1.55) | 2 (1.66) |
| Fluoroquinolones (J01MA) | 18 (2.15) | 10 (2.54) | 5 (1.55) | 3 (2.5) |
| Penicillins, extended spectrum without anti-pseudomonal activity (J01CA) | 10 (1.19) | 7 (1.78) | / | 3 (2.5) |
| Macrolides (J01FA) | 9 (1.07) | 4 (1.01) | / | 5 (4.16) |
| Antidiarrheals, intestinal anti-inflammatory/anti-infective agents (A07AA) | / | / | / | / |
| Triazole derivates (J02AC) | / | / | / | / |
| Tetracyclines (J01AA) | / | / | / | / |
| Other antibacterials (J01XX) | 27 (3.23) | 17 (4.32) | 8 (2.48) | 2 (1.66) |
Antibiotics were administered mainly through the parenteral route (93.8%). Empiric treatment was the main physicians’ choice for prescribing (87.1%). The main reasons for treatment with an antibiotic were pneumonia (19.8%) and bronchitis (15.8%). On the other side, the most common indications for treatment among adult patients were respiratory tract infection in 23.4%, followed by antibiotic surgical prophylaxis in gynecology and obstetrics (17.6%). In 12.1% of cases antibiotics were prescribed to patients with an undefined site of infection and with no systemic inflammation.
Discussion and Conclusions
This is the first nationwide PPS of HCAI in Kosovo conducted in accordance with the ECDC protocol and represents the second, following the survey conducted in Croatia within the 2011-2012 global ECDC PPS,13 carried out in the Western Balkan countries. The overall prevalence rate of HAIs in Kosovo was 4.9%, lower than expected; indeed, the ECDC 2011-12 survey showed an average prevalence of 6%, ranging from 2.3% in Latvia to 10.8% in Portugal.13
A possible explanation was the case mix and complexity of inpatients and the lack of diagnostic capabilities in small hospitals of the country. Indeed, in UCCK, where more complex and severe patients are admitted, the prevalence was 7.2%. Eighty percent of cases with HCAI were indeed registered in UCCK. There were no registered cases in regional hospitals in Ferizaj and Mitrovica. These are the smallest hospitals in the country and the hospital in Mitrovica is currently operating in a very difficult financial and political context. Another explanation was HCAI underreporting; in our survey 73.3% of HCAI had a microbiological assay positive, that is much higher compared with the average 59.1% in the ECDC survey and does not reflect a better microbiological capability than in other European countries. It is likely that in our survey some infections without microbiological results were not registered as HCAI. Finally, in some small and peripheral hospital underreporting could also contribute to the lower prevalence rate, most likely due to difficulties in communication with the referral center.
The healthcare system in Kosovo suffers from a lack of accountability, corruption, misuse of existing resources, difficulty in communication and poor-quality assurance capacities. There is no health insurance in place and the Health Information System is not yet fully functional. Very often, patients and their families are required to provide health care materials by themselves. Households’ out-of-pocket spending on health is around 40% of total expenditures on health care.18 Infection prevention and control in Kosovo are facing common problems with other countries which have limited resources. These activities are limited to passive monitoring and usually actions are only initiated as a response to late stages of outbreaks. Outside UCCK and few other regional hospitals, hospital infection control committees existed solely on paper.
In our survey, the median duration of hospital stay until onset of the HCAI was 11 days, which was similar to the ECDC survey, i.e. 12 days. In European Union (EU) hospitals, HCAI prevalence was highest among patients admitted to ICU (19.5%), whereas in our survey surgical departments had the highest rate (35.5%). Of note, together with the possible limitations above mentioned, it should be considered that the total number of ICU beds in Kosovo is only 95. In our study 70% of patients had a peripheral device on the day of the survey and all UTIs occurred in patients with a urinary catheter. Results for UTI could be biased as a result of the very low sample size (only 7 patients with UTIs). In ECDC study 1694 (59.5%) patients had urinary catheter within 7 days before the HCAI onset. A peripheral vascular catheter was present in 46.7% of patients, varying between 30.6% in France and 70.6% in Greece.13
The HCAI etiologies in our study did not differ from those reported from other studies.19-23 The most frequently isolated microorganisms in HCAIs in the ECDC PPS study were, in decreasing order, Escherichia coli (15.9%), Staphylococcus aureus (12.3%), Enterococcus spp. (9.6%); in our survey Klebsiella pneumoniae, Escherichia coli and S. aureus accounted for 22.5%,19.3% and 16.1% of all HCAI, respectively.
High rates of antibiotic usage, particularly broad-spectrum antibiotics, were observed in our study as already evidenced in a previous survey.12 Ceftriaxone remains the most prescribed antibiotic.
In ECDC study the route of administration of antimicrobials was parenteral in 70.9% of cases and varied from less than 50% in UK-Wales, Sweden and UK-Scotland to more than 90% in Greece and Romania.13 In Kosovo this number was 93.8%, which is close to the Balkan countries, where parenteral route is preferred by clinicians.
Empiric treatment remains predominant in Kosovo acute care facilities. In Mitrovica hospital no patient received a targeted treatment based on susceptibility assays. In UCCK only 7.8% of patients received treatment for any infection, either community acquired or HCAI based on susceptibility results. The highest rate of targeted antibiotic treatment was registered in Peja hospital (23.8%), because this is the only center with clinical microbiology services inside the hospital. All other clinical microbiology laboratories are placed outside the hospital administration, i.e. within the Institutes of Public Health, which represent separate administrative institutions from the hospitals sometimes with communication difficulties. The challenges of the limited usage of routine antibiotic susceptibility testing is caused by the underutilization of microbiological diagnostics in clinical practice by clinicians. The results of our survey showed also that surgical prophylaxis is a significant area of misuse of antibiotics.
Antibiotic misuse and resistance present a challenge for the health care system in Kosovo. For many years all antimicrobials have been available in Kosovo’s outpatient pharmacies without a physician’s prescription, although this is illegal. There are no written antibiotic policy guidelines or basic recommendations, such as for antimicrobial prophylaxis in surgery, at governmental level and within hospitals. Other challenges are represented by aggressive promotion policies by pharmaceutical companies, the low level of awareness and education of the population and, last but not least, corruption.
Our PPS provided also data on alcohol-based hand-rub consumption as indicator of hand hygiene. The usage of alcoholic hand-rub in Kosovo hospitals was low, most likely due to budget constraints, and perhaps fear of skin damage by healthcare workers. Indeed, in Kosovo hospitals hand hygiene is mainly practiced by using plant soap or liquid soap. The median alcohol hand rub consumption in Kosovo was 11.9 liters per 1000 patient-days. In ECDC survey the median hospital alcohol hand rub consumption varied greatly between countries, from less than 10 L/1000 patient-days in Bulgaria, Hungary, Lithuania, Italy, Romania and Slovakia to more than 50 L/1000 patient-days in Denmark, Greece, Norway, Malta and Sweden.13 In both studies the use of alcohol hand rub was based on volumes dispensed by the hospital pharmacy and purchased during one-year period, but not necessarily used by the healthcare workers in the same year. This indicator didn’t include consumption of other hand hygiene agents.
Data representativeness was one of the limitations of our study. Low sensitivity (false negatives, or underreporting) of HAI is a frequent issue in the national HCAI surveillance systems. The protocol used did not collect indicators of the frequency of diagnostic testing, such as the denominator for blood cultures taken.
In conclusion, the HCAI prevalence rate detected in Kosovo is below the average infection rate in the EU, even though this is likely to be an underestimate. On the other hand, antimicrobial prescribing is very high in Kosovo hospitals, especially cephalosporins. Gathered data will be an important tool to identify targets for quality improvement in Kosovo and will support the preparation of guidelines and protocols for prudent use of antibiotics. A working group by the Ministry of Health is already established with a mandate to prepare restrictions in usage of antibiotics in all levels of health care. Key recommendations driven by this study are to improve surveillance systems of HCAI and antibiotic use and enhance infection prevention and control in all level of health care.
Acknowledgements
The authors would thank Prof. Steve Bristow for critical reading and correction of the manuscript.
Funding Statement
Funding: This study was financially supported by the Italian Agency for International Cooperation and Italian Embassy in Kosovo, within the project “Support to Health System in Kosovo”.
References
- 1.Morris K. Global control of health-care associated infections. Lancet 2008;372:1941-42. [DOI] [PubMed] [Google Scholar]
- 2.Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 2011;377:228-41. [DOI] [PubMed] [Google Scholar]
- 3.Pittet D, Allegranzi B, Storr J, et al. Infection control as a major World Health Organization priority for developing countries. J Hosp Infect 2008;68:285-92. [DOI] [PubMed] [Google Scholar]
- 4.Raka L. Lowbury lecture- Infection control and limited resources: Searching for the best solutions. J Hosp Infect 2009;72:292-8. [DOI] [PubMed] [Google Scholar]
- 5.Jakupi A. Report: Drug consumption in Kosovo 2011-2013. Kosovo Medicines Agency – Prishtina, 2014. [Google Scholar]
- 6.Licker M, Baditoiu L, Lungeanu D, et al. Infection control capacity building in European countries with limited resources: issues and priorities. J Hosp Infect 2017;96:85-8. [DOI] [PubMed] [Google Scholar]
- 7.Raka L, Zoutman D, Mulliqi G, et al. Prevalence of Nosocomial Infections in High-Risk Units in the University Clinical Center of Kosovo. Infect Control Hosp Epidemiol 2006;27:421-3. [DOI] [PubMed] [Google Scholar]
- 8.Spahija G, Mulliqi G, Raka L, et al. Prevalence of nosocomial infections in adult intensive care units at Kosovo teaching hospital. Infect Control Hosp Epidemiol 2008;29:475. [DOI] [PubMed] [Google Scholar]
- 9.Laxminarayan R, Duse A, Wattal C, et al. Antibiotic resistance – the need for global solutions. Lancet Infect Dis 2013;13:1057-98. [DOI] [PubMed] [Google Scholar]
- 10.Harbarth S, Balkhy H, Goossens H, et al. Antimicrobial resistance: one world, one fight. Antimicrob Resist Infect Control 2015;4:49 [Google Scholar]
- 11.Versporten A, Bolokhovets G, Ghazaryan L, et al. Antibiotic use in eastern Europe: a cross-national database study in coordination with the WHO Regional Office for Europe. Lancet Infect Dis 2014;14:381-7. [DOI] [PubMed] [Google Scholar]
- 12.Raka L, Goosens H, Mulliqi G, et al. Capacity building to implement state of the art surveillance systems for antibiotic consumption and resistance in Kosovo: results of European Union research project in Kosovo. Antimicrob Resist Infect Control 2015;4:P178. [Google Scholar]
- 13.Zarb P, Coignard B, Griskeviciene J, et al. The European Centre for Disease Prevention and Control (ECDC) pilot point prevalence survey of healthcare-associated infections and antimicrobial use. Euro Surveill 2012;17:20316. [DOI] [PubMed] [Google Scholar]
- 14.Gravel D, Taylor G, Ofner M, et al. Point prevalence survey for healthcare-associated infections within Canadian adult acute-care hospitals. J Hosp Infect 2007;66:243-8. [DOI] [PubMed] [Google Scholar]
- 15.Reilly JS, Price L, Godwin J, et al. A pilot validation in 10 European Union Member States of a point prevalence survey of healthcare-associated infections and antimicrobial use in acute hospitals in Europe, 2011. Euro Surveill 2015;20:21045. [DOI] [PubMed] [Google Scholar]
- 16.Versporten A, Bielicki J, Drapier N, et al. The Worldwide Antibiotic Resistance and Prescribing in European Children (ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J Antimicrob Chemother 2016;1-12. [DOI] [PubMed] [Google Scholar]
- 17.European Centre for Disease Prevention and Control (ECDC). Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals. Protocol version 4.3. Full scale survey and codebook. Stockholm: ECDC: 2012. Available from: http://www.ecdc.europa.eu/en [DOI] [PubMed] [Google Scholar]
- 18.The World Bank Group in Kosovo Country snapshot, April. 2015, accessed Jan 2017. available on http://www.worldbank.org/content/dam/Worldbank/document/eca/Kosovo-Snapshot.pdf). Accessed 21 Dec 2016 [Google Scholar]
- 19.European Centre for Disease Prevention and Control. Annual epidemiological report 2014. Antimicrobial resistance and healthcare associated infections. ECDC, Stockholm. 2015. Available from: http://ecdc.europa.eu/en/publications/Publications/antimicrobial-resistance-annualepidemiologicalreport.pdf. Accessed 21 Dec 2016 [Google Scholar]
- 20.Magill SS, Hellinger W, Cohen J, et al. Prevalence of healthcare-associated infections in acute care hospitals in Jacksonville, Florida. Infect Control Hosp Epidemiol 2012;33:283-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sinatra I, Carubia L, Marchese V, et al. Prevalence survey of healthcare-associated infections and antimicrobial use at the University Hospital “Paolo Giaccone”, Palermo, Italy. J Prev Med Hyg 2013;54:200-4. [PMC free article] [PubMed] [Google Scholar]
- 22.Hajdu A, Samodova OV, Carlsson TR, et al. A point prevalence survey of hospital-acquired infections and antimicrobial use in a paediatric hospital in northwestern Russia. J Hosp Infect 2007;66: 378-84. [DOI] [PubMed] [Google Scholar]
- 23.Askarian M, Yadollahi M, Assadian O. Point prevalence and risk factors of hospital acquired infections in a cluster of university-affiliated hospitals in Shiraz, Iran. J Infect Public Health 2012;5:169-76. [DOI] [PubMed] [Google Scholar]


