Abstract
Background. Vaccine hesitancy has increased worldwide with a subsequent decreasing of vaccination rates and outbreaks of vaccine-preventable diseases (i.e. measles, poliomyelitis and pertussis) in several developed countries, including Italy.
Design and Methods. We conducted a survey to investigate the attitudes of a parents’ sample about vaccinations by the distribution of questionnaires in six lower secondary schools of the Italian city of Messina.
Results. Regarding vaccinations carried out on children, the declared vaccination coverage rates ranged widely between good coverage percentages for some vaccinations (Measles-Mumps-Rubella, Diphtheria-Tetanus-Pertussis), and very low coverage rates for others, especially for “new” vaccinations (HPV, meningococcal, pneumococcal). The vaccinations carried out correlated negatively with both parents’ age and their level of education. Moreover, a favourable parents’ opinion was strongly influenced by a favourable opinion of the physician, while an unfavourable parents’ opinion seemed conditioned by a direct or indirect knowledge of people harmed by vaccines. In addition, our data show that parents do not often know or partially know the real composition of the vaccines and the diseases prevented by vaccinations.
Conclusions. Data analysis shows that parents are, theoretically, favourable towards vaccinations but have little knowledge of such practices, sometimes not being unaware of the types of vaccines administrated to their children. Health education and communication of correct information are certainly the cornerstones to improve the situation and to fight the widespread and non-grounded fears about vaccines.
Significance for public health.
The argument of the vaccine hesitancy is particularly important for public health because, due to the parents’ refusal to vaccine their children, we have assisted in last years to the recruitment of vaccine preventable diseases in many countries. This refusal is due especially to an unjustified fear about potential side effects of vaccines. However, many studies have shown that vaccines are sure and efficacies. Health education of parents is the cornerstone on which the public health should build the fight to the vaccine hesitancy and improve the vaccination coverages.
Key words: Vaccines, Hesitancy, Prevention, Health Education
Introduction
Background
In two centuries, vaccination programmes have led to the worldwide eradication of smallpox, the disappearance of poliomyelitis in the most world countries and the decline in the mortality and morbidity of several infectious diseases.1 To maintain these goals, a high rate of vaccination coverage (equal to at least the 95% for the most part of vaccinations) is necessary. In most developed countries, the rate of childhood vaccination coverage is high enough, indicating that vaccinations remain a widely accepted public health measures.2 Despite this, there are groups of under-vaccinated or non-vaccinated subjects representing a threat to public health because they hinder the achievement of the herd immunity, essential to protect the entire community.3 Recent studies estimate that approximately 1 in 8 children <2 years old in the United States are under-vaccinated, due to parental choice, and a majority of physicians reports at least one vaccine refusal per month.4,5
In Italy, the national vaccination calendar was modified over the years. Particularly, the current calendar includes, already for several years, a hexavalent vaccination, administered in 3 doses in the first year of age at third, fifth and eleventh months respectively. This vaccination protects against Diphtheria, Tetanus, Poliomyelitis and Hepatitis B, that are mandatory already for several decades, and Pertussis and Haemophilus influenzae b that became mandatory from last year. In the same vaccination sessions, with the hexavalent, the strongly recommended conjugated pneumococcal vaccine can be administered. Moreover, Meningococcal C, administered in only one dose at 13th-15th months, and the newest Meningococcal B, available only recently and administered in four doses during the first year of age, are strongly recommended. Always at 13th-15th months, it is now mandatory (from 2017) the first dose of trivalent Measles-Mumps-Rubella (MMR) or tetravalent MMR+Varicella (MMRV), a vaccination that was always only strongly recommended and of which the second dose is administered at 5th-6th years of age together with the first booster dose of Diphteria-Tetanus-Pertussis-Poliomyelitis. From 12th year of age is, also, free offered the Papillomavirus (HPV) vaccination to both females and males 6. In Sicily the regional adopted calendar is the same to that national.
The Italian childhood vaccination coverage rates for various vaccine-preventable diseases have been decreasing since 2013. In 2016, the vaccination coverage rate for poliomyelitis in children at 24 months of age was 93,3% compared to 95,7 of 2013. Moreover, in the same year, the vaccination coverage rate for measles in children at 24 months of age was dangerously low, accounting only for 87.3%.7,8 In Sicily, vaccination coverage rates both for mandatory and recommended are often under the national average.9 The hazard is highlighted by the recent outbreaks of vaccine-preventable diseases (VPDs), including measles,10 poliomyelitis and pertussis.11,12 In Italy, a large measles outbreak occurred in 2017, with more than 4,885 cases reported from January to December 2017.13 Sicily was one of the more affected Italian regions with 410 reported cases at December 2017. In particular, the whole territory of Messina reported 63 cases (10% of Sicilian cases).10
Vaccine hesitancy refers to delay in acceptance or refusal of vaccines despite availability of vaccination services and it is an individual behaviour influenced by a range of factors, such as knowledge or past experiences. This refusal is also linked to historical, political and socio-cultural contexts.14-16
Vaccine-hesitant individuals are a rather heterogeneous group, some refuse certain vaccines (i.e. influenza vaccination) but agree to others.14 Particularly, newer vaccines, usually generate more hesitancy.17,18 Many scientific studies have highlighted the negative influence of traditional (i.e. TV and newspapers) and newest (i.e. internet and social) media misinformation on vaccine acceptance.19-21 On the other hand, an important role is played by healthcare professionals. Several studies have demonstrated the importance of health professionals’ knowledge and attitudes about vaccines, particularly their intention to recommend the vaccinations to their patients, in the decision-making process regarding vaccination.22,23
Objectives
Because there are sub-optimal vaccine coverage rates in Sicily, we decided to carry out this research to investigate the attitudes of a parents’ sample about vaccinations in general and regarding the specific types of vaccines given to children. We decided to choose this category of individuals because the children’s vaccination coverages are strictly dependent on the level of knowledge and past experiences of parents. Therefore, as parents are the decision makers of their own children health we considered that this was the most appropriated target of our investigation.
We evaluated, in particular, their degree of vaccine acceptance, highlighting the role played by various sources of information in their decision whether or not to allow their children to undergo vaccination practices.
Design and Methods
Study design
We conducted a survey on opinions about vaccination of a parents’ sample. Particularly, we considered only parents of pupils of 13-14 years old. We chose this target population because, in Italy, according to the national vaccination calendar, all vaccinations are completed at this age, including HPV vaccine that is offered from 12 years old. Indeed, we thought that the information about HPV vaccination was very important to evaluate considering the extremely low coverage rates in our territory.
Setting
The survey was carried out from January to June 2017 in six lower secondary schools of the Sicilian city of Messina. Specifically, we used a questionnaire listing some questions about vaccinations. In each school, we organized a first meeting with parents after we obtained the favourable opinion of the head teacher. In this meeting, we explained the study and distributed the questionnaires, one for each family nucleus of the child.
After 20 days, we returned to school to collect the filled questionnaires delivered by participating parents. We initially distributed 1,300 questionnaires, and received – 1,093 (84%). Each questionnaire consisted of the following questions (Supplementary material):
Age and parents’ education;
Personal opinions about vaccinations;
Vaccines carried out on children;
Booster doses made;
Opinions of the physicians [paediatricians and family doctors];
Information received by the physicians;
Sources of information that convinced parents not to vaccinate their children;
Reasons why they are opposed to vaccinations;
Specific questions about personal views on meningococcal and pneumococcal vaccinations and information received from their physician about the importance of these vaccines;
Specific questions about their personal views regarding HPV vaccination and information received from their physician about the importance of this vaccine;
Direct or indirect knowledge of people harmed by vaccines.
Statistical analyses
All the obtained data were collected and analysed with Prism 4.0 software. Descriptive statistics were used to find the percentages and the 95% Confidence Interval (CI). To assess the data distribution patterns, the collected values of each parameter were evaluated using the Lilliefors and Shapiro-Wilk normality tests that were in most cases no significant. Correlations were determined using the Pearson test while χ2 was used for inter-group comparison. Significance was assessed at the P<0.05 level.
Results
The information about age and level of parents’ education are shown in Table 1.
Table 1.
Age and level of parents’ education.
| Mean age | Elementary and lower secondary school diploma | Upper secondary school diploma | University degree | |
|---|---|---|---|---|
| Father | 45.3 | 36.4% (95%CI: 31.5-41.2) | 42.6% (95%CI: 38.0-47.1) | 21.0% (95%CI: 15.7–26.4) |
| Mother | 42.2 | 30.0% (95%CI: 25.0-35.0) | 45.7% (95%CI: 41.3-50.1) | 24.3% (95%CI: 19.1-29.6) |
About personal opinion on vaccinations, parents answered “favourable” 86% (95%CI: 83.8-88.2), “indifferent” 6.6% (95%CI: 0.9-12.3), “contrary” 7.4% (95%CI: 1.7-13.1).
The vaccinations carried out correlated negatively with both the parents’ age (P<0.0001) and their level of education (P<0.0001). When asked about vaccinations carried out on their children, the results, shown in Figure 1A, highlighted a not homogeneous adherence to the various vaccinations. The self-reported coverage rates ranged widely between good coverage percentage (MMR and DTP vaccinations) and very low coverage rates, far from those advised in the international guidelines (pneumococcal, meningococcal, HPV and Hib vaccinations). By dividing the sample into those favourable and opposed to vaccinations, we observed significant differences in the vaccination coverages that however were very variable depending on the specific vaccinations. As reported in Figure 1B the most significant differences were observed for meningococcal C and HPV vaccines with only 26.7 and 8.3% of vaccination coverages in the children of opposing parents (P<0.01). When asked about booster doses of vaccines, parents’ response was 90.2% (95%CI: 88.4-92.1) “Yes” and 9.8% (95%CI: 4.1-15.5) “No”. Stratifying the sample in favourable and opposing to vaccinations these percentages were 91 and 61.7 respectively (P<0.0001). Moreover, when asked about the position of their physician with regard to vaccinations, they answered: “favourable” 79.5% (95%CI: 76.8-82.2), “favourable only for compulsory vaccinations” 18.1% (95%CI: 12.7-23.5), “unfavourable” 2.4% (95%CI: -3.5-8.3). By dividing our sample according to what was stated by the parents about the opinion expressed by the physician (favourable, favourable only to compulsory vaccinations, unfavourable), we observed that the presence of a favourable physician correlates positively with the number of fully vaccinated children (P=0.0063 to Pearson test), the percentage of vaccinations carried out (P<0.0001), both compulsory and recommended, as well as with vaccine booster doses (P=0.0081), information received by physician (P=0.0074) and the personal opinion of parents (P=0.0032) (Figure 2). The key role of the physician in influencing parents’ opinion on the usefulness of vaccinations was also confirmed by comparing the percentages of favourable physician in the two parent’s groups favourable and opposing to vaccinations. While in the former the percentage was 83.5 in the latter was 51.7 (P<0.0001).
Figure 1.
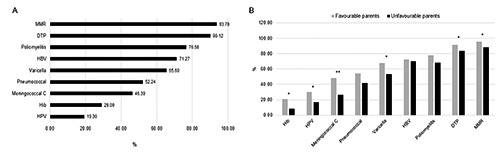
Vaccinations carried out on children (A) and vaccination percentages obtained comparing opposed parents versus favourable parents (B).
Figure 2.
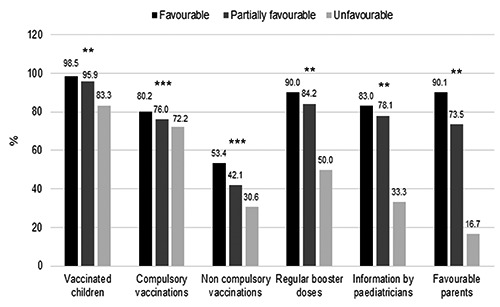
Percentage of vaccination coverages according to the physician’s position (Favourable, partially favourable and unfavourable) and results of Pearson test (**P <0.001; ***P <0.0001).
Concerning the degree of satisfaction regarding the information received from their physician about the vaccination schedule and the effectiveness of vaccinations, the results were as follows: “a lot” 26.7% (95%CI: 21.7-31.7), “enough” 56.3% (95%CI: 52.4-60.2), “a little bit” 10% (95%CI: 4.3-15.7), “not at all” 7.0% (95%CI: -1.2-12.8). About sources of contrary information regarding vaccination, paradoxically, physicians were the most important source of contrary information (41%, 95%CI: 24.0-57.5), followed by the internet/TV (32%, 95%CI: 14.2-50.0) and other sources (friends/relatives, books/journals) (27%, 95%CI: 8.6-45.7). Moreover, about reason why they did not get vaccinations for their children, the fear of collateral effects was the motivation reported by the almost parents (91.5%, 95%CI: 83.2-99.8).
Concerning the meningococcal and pneumococcal vaccinations, 81.1% (95%CI: 78.3-84.0) of parents were favourable towards them, while 18,9% (95%CI: 13.0-24.8) answered that these vaccinations are unnecessary. The explanation given by the opposing parents was the fear of side effects for 44.4% (95%CI: 40.8-48.0), poor information received for 30.3% (95%CI: 23.4-37.2) and doubts about the actual efficacy of these vaccines by 13.1% (95%CI: 8.4-17.8). In addition, 53.7% (95%CI: 49.5-57.9) said they had received information on these vaccinations, and the main sources of information were physicians for 82% (95%CI: 77.8-86.2). Among the respondents, 46.3% (95%CI: 41.8-50.8) answered that they had received no information on these vaccinations. Moreover, concerning vaccination against HPV, 74.8% (95%CI: 71.5-78.8) of parents were favourable towards it, while 25.2% (95%CI: 19.5-30.9) were contrary. The reasons given by the hesitant parents was poor information for 32.2% (95%CI: 18.7-45.7), fear of side effects for 26.6% (95%CI: 12.6-40.6) and doubts about the actual efficacy of the vaccine by 17.5% (95%CI: 2.6-32.4). In addition, 58.5% (95%CI:54.5-62.5) said they received information, while, 41.5% (95%CI: 36.8-46.2) responded that they did not receive any information. The information was given mainly by physicians (52.8%, 95%CI: 46.4-59.2), followed by the media/internet (13.3%, 95%CI: 4.6-22.0) and school (10.2%, 95%CI: 1.4-19.0).
Finally, about the knowledge of people damaged by vaccinations, the following answers were received: 14.4% (95%CI: 8.8-20.0) “yes personally”, 30.5% (95%CI: 25.5-35.5) “yes but indirectly”, 55.1% (95%CI: 51.0-59.1) “no”.
The likely factors influencing parents’ opinions on vaccinations were a favourable opinion of the physician and knowledge of people harmed by vaccines. In particular, as shown by Pearson test, the favourable opinion of the parents was strongly influenced by the favourable opinion of the physician (P<0.0001), while the unfavourable opinion of parents seemed conditioned by direct or indirect knowledge of people harmed by vaccines (P<0.0001). These results were confirmed by χ2 test that highlighted very significant differences in the percentages of favorable and opposed physicians, as stated by parents, in the two parent groups.
Discussion
The lack of knowledge and perception about the benefits of vaccination, associated with the misleading information on internet and strong anti-vaccination movement, may influence parents’ decision to not vaccinate their children.24,25 Therefore, it is important to understand what the perceptions are related to vaccination practices in order to improve parental knowledge of them and consequently to increase immunization coverage.
This study investigates the knowledge, attitudes and practices of parents towards vaccinations. The data show a general confidence by parents regarding vaccination as demonstrated by the percentage of vaccinated children. In particular, younger parents with a lower level of education were more likely to vaccinate their children. This is in agreement with the data from international literature highlighting that the level of parental education has also been implicated in contributing to vaccine hesitancy.5 Opel et al. found that parents with higher levels of education were nearly four times as likely to be concerned about the safety of vaccines than those with lower education levels.26,27 Similarly, Smith et al. found that refusal of all childhood vaccines was more common among college-educated parents than those with lower levels of education.28
Surely, some answers to the vaccinations and the booster doses administered to children are distorted. The most frequent vaccination was MMR, compared to the lower percentages of mandatory vaccination. Indeed, the polio and HBV vaccinations were only at third (76.6%) and fourth place (71.3%), respectively, while the Hib vaccine, which for a long time is contained in the hexavalent vaccine, and whose administration is favourably affected by this vaccination, is inexplicably only at eighth place (29.1%) of the responses. The cause of these findings probably lies in the lack of knowledge of these vaccines by parents who, paradoxically, know much more about diseases such as measles and rubella instead of polio or hepatitis B, or those caused by Hib. In addition, it is equally likely that parents do not know the exact composition of the hexavalent vaccine and, therefore, against what diseases this vaccination protects their children. Moreover, parents do not perceive some VPDs as significant health threats because they think that the disease no longer exists and/or that there is no need for their children to be vaccinated, assuming the children will benefit from herd immunity.29
In our study, vaccine hesitancy did not involve all vaccinations but only some of them, particularly the HPV and meningococcal vaccines. Indeed, vaccine hesitancy can take several forms. At its most severe, parents refuse all vaccines. However, this stance is relatively rare, adopted by only 1-2% of parents.17,18,30 Instead, delay or refusal of one or more specific vaccines is much more common. Among the parents opposed to vaccinations, the main cause was, by far, the fear of possible side effects. Indeed, different factors – past experiences with health services, family histories, feelings of control and conversations with friends, among others – can influence the decision-making process regarding vaccination. Vaccination has been the subject of many false myths, such as the association between the hepatitis B vaccine and multiple sclerosis or between the MMR vaccination and autism. Fear of autism is still a frequently reported vaccine safety concern among parents.21,31 Some factors that play a key role in the apparent increase of this phenomenon in the developed world are the roles of the media and communication, of public health and vaccine policies, and of health professionals. When asked about sources of information that oppose vaccines, parents said that the main source was physicians, followed by the internet and, thirdly, by friends or relatives against vaccinations. This result highlights a considerable reluctance still present in a fairly large number of healthcare workers. The datum is extremely significant because parents often rely entirely on physicians to care for their children, and hence a contrary opinion expressed by a doctor translates into a total mistrust of vaccine. Indeed, one of the main predictors of acceptance of a vaccine is a recommendation for vaccination by a health care professional.31 Many studies have shown that a parent’s decision to vaccinate his or her child was often based on what is compulsory or following recommendations, rather than based on specific knowledge about vaccines or VPDs.29,32 Physicians who share vaccine-related concerns or place less importance on vaccines may transmit these beliefs to their patients and families. Health professionals are generally strong supporters of vaccination. However, some of them could be categorized as vaccine hesitant.33,34 Vaccine hesitancy among health professionals is also well-illustrated by the reluctance of a significant proportion of healthcare workers to receive the flu vaccine despite strong recommendations to do so and free vaccines available at the workplace in many countries.35 The different health professionals (general practitioner, paediatrician, public health physicians) play a key role in the field of communication with parents.36 As stated by parents, 18% of physicians were favourable only to strongly recommended vaccinations and this alarming data must certainly be verified, also considering that among parents opposed to vaccines, 47.5% said that it was the physician who convinced them not to vaccinate their child.
However, the parents stated that the greatest share (79.5%) of physicians were favourable to vaccinations and provided general vaccine information that was good or satisfactory in 83% of cases; of these, only 27% of parents were completely satisfied with the information received by the physicians about the vaccine calendar. Specifically, misinformation was involved with vaccines for HPV, meningococcal C and pneumococcal. Regarding the HPV vaccination, although 60% of parents were favourable towards it, it was performed only in 19.3% of cases; this result shows that the knowledge of HPV is still very poor and it is in line with the local vaccine coverage rate that, at 2017, was about 30% for the cohort 2005.37 HPV has been implicated as the cause of many cancers in several tissues and recent studies on healthy subjects have even found a prevalence of high-risk HPV strains.38,39 These data are very important considering that the targeted population for this vaccine is the same to which the questionnaire was administered (last year of lower secondary school). This highlights the need to educate teenagers and their parents to implement the number of vaccinations.40 Compared to the HPV vaccination, the meningococcal C and pneumococcal vaccinations received more attention by parents. Indeed, on the base of the parents’ declaration, these vaccinations were performed in 52.2% and 46.4% of cases, respectively, compared to the percentage of 66.6% who were favourable towards them. This finding is probably due to the recent news about outbreaks of meningitis in some Italian regions. Moreover, most of those who received the pneumococcal vaccination did so because it was administered with others that are compulsory.
Finally, the results regarding the knowledge of people harmed by vaccines is very important. Indeed, in our study, the relative percentage was 43.3%, although only 13.9% stated that they directly knew such a person. This finding suggests that the idea of vaccines being harmful is present in public opinion and easily transferable to others, since indirect knowledge accounted for 29.4%.
Our results show that parents are theoretically favourable towards vaccinations but have little knowledge of such practices, sometimes lacking knowledge of the types of vaccines administrated to their children. Health education and communication are certainly the cornerstones to improving the situation and combatting the fears about vaccines. At the same time, it is important to communicate the necessity to carry out vaccinations correctly, following accurately the schedule (number of doses and times of administration) in order to reach the best result, as highlighted by previous studies.41
The role of health professionals is crucial in sustaining the success of vaccination programmes. It is necessary to improve their knowledge about vaccinations and stimulate them to promote vaccination practises to their patients. This goal can be reached especially by organizing information meetings between experts in vaccinations and paediatrics and family doctors aimed to make them conscious of their crucial role in promoting vaccination practises and improving vaccine coverages.
We think that the recent innovative and cost effective National Immunization Plan (PNPV 2017-2019)42 and the law 119/2017 extending in Italy the compulsory vaccinations from 4 (Diphteria-Tetanus-Poliomyelitis-HBV) to 10 (Diphteria-Tetanus-Pertussis-Poliomyelitis-HBV-Haemophylus influanzae b-MMRV) will improve over time the vaccination coverage rates for these vaccinations.43 Moreover, in Italy since 2004 is active the National Elimination Plan for Measles and Congenital Rubella (PNEMoRC) that aims to eliminate these diseases from all territory.44 However, the strongly recommended vaccinations (meningococcal B and C, pneumococcal and HPV) could continue to report low coverage rate.
Implication for practice
The argument of the vaccine hesitancy is particularly important for public health because, due to the parents’ refusal to vaccine their children, we have assisted in last years to the recruitment of VPDs in many countries. This refusal is due especially to a fear about potential side effects of vaccines. However, many studies have shown that vaccines are sure and efficacies. Health education of parents is the cornerstone on which the public health should build the fight to the vaccine hesitancy and improve the vaccination coverages.
Limit of the study
The results obtained in the study are based on self-reported data, so we will deepen the analysis comparing these data with the ones reported on the immunization registry to assess any discrepancies. These are due to the parents’ poor knowledge as well as they could be influenced by the memories. This is clearly confirmed by the data relating to the Hib, which are decidedly not corresponding to the actual situation. The use of a not-validate questionnaire could also represent a limit of the study while the physicians’ opinion, as stated by parents, could be the effect of a misunderstanding of the advices given by physicians.
Funding Statement
Funding: none.
References
- 1.Centers for Disease Control and Prevention. Ten great public health achievements-United States, 1900-1999. MMWR Morb Mortal Wkly Rep 1999;48:241-3. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/00056796.htm. [PubMed] [Google Scholar]
- 2.World Health Organization. Immunization summary - A statistical reference containing data through. 2013. Available from: http://www.who.int/immunization/monitoring_surveillance/Immunization_Summary_2013.pdf [Google Scholar]
- 3.Omer SB, Salmon DA, Orenstein WA, et al. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med 2009;360:1981-8. [DOI] [PubMed] [Google Scholar]
- 4.Glanz JM, Newcomer SR, Narwaney KJ, et al. A population-based cohort study of undervaccination in 8 managed care organizations across the United States. JAMA Pediatr 2013;167:274-81. [DOI] [PubMed] [Google Scholar]
- 5.Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine hesitancy. Hum Vaccin Immunother 2013;9:1755-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ministero della Salute. Calendario Vaccinale. Available from: http://www.salute.gov.it/portale/vaccinazioni/dettaglioContenutiVaccinazioni.jsp?lingua=italiano&id=4829&area=vaccinazioni&menu=vuoto. [Google Scholar]
- 7.Ministero della Salute. Coperture Vaccinali Pediatriche, i dati 2015. Available from: <http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?menu=notizie&p=dalministero&id=2718>. [Google Scholar]
- 8.Signorelli C, Odone A, Cella P, et al. Infant immunization coverage in Italy (2000-2016). Ann Ist Super San 2017;53:231-7. [DOI] [PubMed] [Google Scholar]
- 9.Epicentro. Vaccinazioni. Available from: http://www.epicentro.iss.it/temi/vaccinazioni/. [Google Scholar]
- 10.Palamara MA, Visalli G, Picerno I, et al. Measles outbreak from February to August 2017 in Messina, Italy. J Prev Med Hyg 2018;59:E8-E13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yakovenko ML, Gmyl AP, Ivanova OE, et al. The 2010 outbreak of poliomyelitis in Tajikistan: epidemiology and lessons learnt. Euro Surveill 2014;20;19:20706. [DOI] [PubMed] [Google Scholar]
- 12.Sealey KL, Belcher T, Preston A. Bordetella pertussis epidemiology and evolution in the light of pertussis resurgence. Infect Genet Evol 2016;40;136-43. [DOI] [PubMed] [Google Scholar]
- 13.Istituto Superiore di Sanità. Measles in Italy: weekly bullettin. Update as of 12 December 2017. Available from: http://www.epicentro.iss.it/problemi/morbillo/bollettino/Measles_WeeklyReport_N35eng.pdf [Google Scholar]
- 14.Dubé E, Laberge C, Guay M, et al. Vaccine hesitancy: an overview. Hum Vaccin Immunother 2013;9:1763-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gilkey MB, McRee AL, Magnus BE, et al. Vaccination Confidence and Parental Refusal/Delay of Early Childhood Vaccines. PLoS One 2016;11:e0159087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McClure CC, Cataldi JR, O'Leary ST. Vaccine Hesitancy: Where We Are and Where We Are Going. Clin Ther 2017;39:1550-62. [DOI] [PubMed] [Google Scholar]
- 17.Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics 2008;122:718-25. [DOI] [PubMed] [Google Scholar]
- 18.Freed GL, Clark SJ, Butchart AT, et al. Parental vaccine safety concerns in 2009. Pediatrics 2010;125:654-9. [DOI] [PubMed] [Google Scholar]
- 19.Mnookin S. The Panic Virus: A True Story of Medicine, Science, and Fear. Simon & Schuster: New York; 2011. [Google Scholar]
- 20.Smith A, Yarwood J, Salisbury DM. Tracking mothers’ attitudes to MMR immunisation 1996-2006. Vaccine 2007;25:3996-4002. [DOI] [PubMed] [Google Scholar]
- 21.Poland GA, Spier R. Fear, misinformation, and innumerates: how the Wakefield paper, the press, and advocacy groups damaged the public health. Vaccine 2010;28:2361-2. [DOI] [PubMed] [Google Scholar]
- 22.Katz-Sidlow RJ, Sidlow R. A look at the pediatrician as parent: experiences with the introduction of varicella vaccine. Clin Pediatr (Phila) 2003;42:635-40. [DOI] [PubMed] [Google Scholar]
- 23.Posfay-Barbe KM, Heininger U, Aebi C, et al. How do physicians immunize their own children? Differences among pediatricians and nonpediatricians. Pediatrics 2005;116:e623-33. [DOI] [PubMed] [Google Scholar]
- 24.Vrdelja M, Kraigher A, Vercic D, Kropivnik S. The growing vaccine hesitancy: exploring the influence of the internet. Eur J Public Health 2018;28:934-9. [DOI] [PubMed] [Google Scholar]
- 25.Vezzosi L, Santagati G, Angelillo IF. Knowledge, attitudes, and behaviors of parents towards varicella and its vaccination. BMC Infect Dis 2017;27;17:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Opel DJ, Taylor JA, Mangione-Smith R, et al. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine 2011;29:6598-605. [DOI] [PubMed] [Google Scholar]
- 27.Giambi C, Fabiani M, D'Ancona F, et al. Parental vaccine hesitancy in Italy. Result from a National survey. Vaccine 2018;36:779-87. [DOI] [PubMed] [Google Scholar]
- 28.Smith PJ, Chu SY, Barker LE. Children who have received no vaccines: who are they and where do they live? Pediatrics 2004;114:187-95. [DOI] [PubMed] [Google Scholar]
- 29.Benin AL, Wisler-Scher DJ, Colson E, et al. Qualitative analysis of mothers’ decision-making about vaccines for infants: the importance of trust. Pediatrics 2006;117:1532-41. [DOI] [PubMed] [Google Scholar]
- 30.Dempsey AF, Schaffer S, Singer D, et al. Alternative vaccination schedule preferences among parents of young children. Pediatrics 2011;128:848-56. [DOI] [PubMed] [Google Scholar]
- 31.Stefanoff P, Mamelund SE, Robinson M, et al. VACSATC working group on standardization of attitudinal studies in Europe. Tracking parental attitudes on vaccination across European countries: The Vaccine Safety, Attitudes, Training and Communication Project (VACSATC). Vaccine 2010;28:5731-7. [DOI] [PubMed] [Google Scholar]
- 32.Tickner S, Leman PJ, Woodcock A. Factors underlying suboptimal childhood immunisation. Vaccine 2006;24:7030-6. [DOI] [PubMed] [Google Scholar]
- 33.Leask J, Quinn HE, Macartney K, et al. Immunisation attitudes, knowledge and practices of health professionals in regional NSW. Aust N Z J Public Health 2008;32:224-9. [DOI] [PubMed] [Google Scholar]
- 34.Squeri R, Genovese C, Trimarchi G, et al. An evaluation of attitude toward vaccines among healthcare workers of a University Hospital in Southern Italy. Ann Ig 2017;29:595-606. [DOI] [PubMed] [Google Scholar]
- 35.Squeri R, Riso R, Facciolà A, et al. Management of two influenza vaccination campaign in health care workers of a university hospital in the south Italy. Ann Ig 2017;29:223-31. [DOI] [PubMed] [Google Scholar]
- 36.Tolunay O, Celik U, Karaman SS, et al. Awareness and attitude relating to the human papilloma virus and its vaccines among pediatrics, obstetrics and gynecology specialists in Turkey. Asian Pac J Cancer Prev 2014;15:10723-8. [DOI] [PubMed] [Google Scholar]
- 37.Visalli G, Picerno I, Vita G, et al. Knowledge of sexually transmitted infections among younger subjects of the city of Messina (Sicily). J Prev Med Hyg 2014;55:17-22. [PMC free article] [PubMed] [Google Scholar]
- 38.Kreimer AR, Bhatia RK, Messeguer AL, et al. Oral human papillomavirus in healthy individuals: a systematic review of the literature. Sex Transm Dis 2010;37:386-91. [DOI] [PubMed] [Google Scholar]
- 39.Visalli G, Currò M, Facciolà A, et al. Prevalence of human papillomavirus in saliva of women with HPV genital lesions. Infect Agent Cancer 2016;26;11:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Klug SJ, Hukelmann M, Blettner M. Knowledge about infection with human papillomavirus: a systematic review. Prev Med 2008;46:87-98. [DOI] [PubMed] [Google Scholar]
- 41.La Fauci V, Riso R, Facciolà A, et al. Response to anti-HBV vaccine and 10-year follow-up of antibody levels in healthcare workers. Public Health 2016;139:198-202. [DOI] [PubMed] [Google Scholar]
- 42.Signorelli C, Guerra R, Siliquini R, Ricciardi W. Italy's response to vaccine hesitancy: an innovative and cost effective National Immunization Plan based on scientific evidence. Vaccine 2017;35:4057-9. [DOI] [PubMed] [Google Scholar]
- 43.Ricciardi W, Boccia S, Siliquini R. Moving towards compulsory vaccination: the Italian experience. Eur J Public Health 2018;28:2-3. [DOI] [PubMed] [Google Scholar]
- 44.Lo Giudice D, Cannavò G, Capua A, et al. Eliminating congenital rubella: a seroepidemiological study on women of child-bearing age and MMR vaccine coverage in newborns. J Prev Med Hyg 2009;50:236-40. [PubMed] [Google Scholar]


