Abstract
Objective
This project audited rate and extent of weight loss in a primary care/commercial weight management organisation partnership scheme.
Methods
34,271 patients were referred to Slimming World for 12 weekly sessions. Data were analysed using individual weekly weight records.
Results
Average (SD) BMI change was –1.5 kg/m2 (1.3), weight change –4.0 kg (3.7), percent weight change –4.0% (3.6), rate of weight change –0.3 kg/week, and number of sessions attended 8.9 (3.6) of 12. For patients attending at least 10 of 12 sessions (n = 19,907 or 58.1%), average (SD) BMI change was –2.0 kg/m2 (1.3), weight change –5.5 kg (3.8), percent weight change –5.5% (3.5), rate of weight change –0.4 kg/week, and average number of sessions attended was 11.5 (0.7) (p < 0.001, compared to all patients). Weight loss was greater in men (n = 3,651) than in women (n = 30,620) (p < 0.001). 35.8% of all patients enrolled and 54.7% in patients attending 10 or more sessions achieved at least 5% weight loss. Weight gain was prevented in 92.1% of all patients referred. Attendance explained 29.6% and percent weight lost in week 1 explained 18.4% of the variance in weight loss.
Conclusions
Referral to a commercial organisation is a practical option for National Health Service (NHS) weight management strategies, which achieves clinically safe and effective weight loss.
Keywords: Obesity, Treatment, Commercial slimming organisation, Effectiveness, Audit
Introduction
Despite a series of government reviews, documents, and action targets to halt the rising tide in obesity prevalence in the UK, the problem continues unabated. In England nearly a quarter of the men and women are now obese [1–3]. Projected trends for children paint an even more dismal picture [4]. Recent Foresight predictions suggest that if current trends continue, some 60% of the UK population will be obese by 2050 [1].
Obesity is now recognised as being at the forefront of current ‘lifestyle diseases’ creating a future of rising disease and chronic long-term ill health [1, 2, 4, 5]. Tackling the obesity epidemic will impact on other lifestyle diseases such as heart disease, stroke, cancer, and diabetes. This in turn will reduce the growing burden on health care resources that currently threatens the quality of care that national health care systems can provide [1, 6]. The Foresight projections estimate that the health burden of obesity will add an additional GBP 45.5 billion per year to UK national health care expenditure by 2050 [1, 6].
The UK Foresight Commission and other reports note that tackling obesity needs whole societal change with cross-government action and long-term commitment to make changes at all levels of society [1, 6]. The Foresight mapping exercise highlights the complexity of the obesity problem [1]. However, many therapists have emphasised that while much of the cause of obesity is due to a complex interplay between genetic susceptibility and environmental factors, its prevention and treatment need simple behavioural and lifestyle solutions that are accessible and accommodating to people living their normal lives in the community [5–12]. In this way people can realistically navigate towards a sustainable healthier body weight. With these considerations in mind it is pertinent to note that in their obesity guidance, the UK National Institute for Health and Clinical Excellence (NICE) recognises the importance of providing regular and ongoing support for behavioural change, to prevent weight gain, promote weight loss and its maintenance [4]. NICE recognises the role of commercial weight management organisations (CWMOs) which follow guidance criteria for best practice. Most recently the UK cross-departmental government report ‘Healthy Weight, Healthy Lives’ recognised the vital role played by the commercial sector and other providers in ensuring that more people can access effective services in order to increase cost-effective provision of health service capacity [13].
In 2006, the results of a feasibility study were published, examining the benefits of working in partnership with the UK National Health Service (NHS) by implementing a slimming on referral service in primary care, with Greater and Central Derby Primary Care Trusts. In that study, 91 out of 107 patients were offered free attendance at a CWMO for 12 sessions enrolled at a group, and 62 completed at least 10 out of the 12 weekly sessions, producing an average weight loss of 6.4% of baseline weight. 34 of those who completed 12 weeks went on to self-fund a further 12 weeks and achieved an average decrease in baseline weight of 11.3% [14].
Since the feasibility study, the referral scheme has been offered nationally to NHS Trusts and enables equal access to local group support for all adults seeking behaviour change solutions to their weight problems. The organisation has been working in partnership with Primary Care Trusts (PCTs) and NHS Trusts offering a subsidised scheme in order to provide free participation for 12 weeks to patients referred by their health professional. The purpose of this paper is to provide the largest audit of a UK slimming on referral service operated between the NHS and a commercial partner in terms of rate and extent of weight loss, attendance, comparison of the outcomes for men and women, and to briefly assess basic predictors of weight loss in this study population.
Methods
Referral Process
Patients were referred by a health care professional in primary or secondary care. Each participating PCT/NHS Trust set their own referral criteria, which varied between areas, depending on their local weight management care pathways. All areas incorporated in this analysis excluded patients under 16 years and pregnant women. At the point of referral, patients were issued a 12-week voucher pack to be completed in the space of 14 weeks (funded by the PCT/NHS Trust and subsidised by the CWMO). This voucher pack could be used by the patient to attend a local group of their choice, run by the CWMO, for 12 consecutive weeks. Extensions for up to 2 weeks were permitted for planned holidays or illness. The vouchers thus covered the patients’ membership and weekly fees for a 12–14 week period. On referral, participants were treated exactly as any other group member, receiving the usual programme and support provided by the CWMO. The CWMO, Slimming World, meets the NICE best practice criteria to help adults develop the lifestyle changes needed to reduce weight, prevent weight gain, and support long-term weight maintenance. The organisation has an extensive community-based infrastructure of around 6,700 support groups held each week across the UK. Groups are located in a variety of local venues at different times and days of the week, making the groups easily accessible for all members of the community.
Dataset
This report analyses data collected from participants in the slimming on referral scheme between May 2004 and November 2009, who had time to finish their full 12-week referral. This resulted in the inclusion of 38,614 patients who were referred from within 77 PCTs or NHS Trusts, for whom data on weight, height, age, and gender were collected. Among these were 2,625 cases where the data for one or more of the 12 referral vouchers issued per participant was unclear or could not be resolved (spoiled vouchers, illegible writing etc.) and 1,718 cases where the participant completed the scheme outside of the 14 (12 plus 2) week time window, due to circumstances such as bereavement or illness. This left 34,271 in the present audit. 80 participants were included in the database but there was no data for their date of birth. Age data are reported excluding these subjects. Some of the participants went on to self-fund further attendance following the initial 12-week referral and others were offered subsequent 12-week referral packages from their health care team (9,852 in total). The data in this analysis covers the initial 12-week sessions of the referral scheme.
Data Collection
Data for this audit was collected as part of routine data collection within the referral programme. At the point of referral the patients’ gender, date of birth, and height were recorded by the health professional. When the patient enrolled at the weight management group (week 1 of the referral), their start weight and date were recorded. Each week the patient returned to group their weekly weight change was recorded along with date of attendance. The same calibrated scales were used each week at a given group to record weight and weight change. The collected data were sent to the research team for input into the referral database.
This work is categorised as a service evaluation under the Ad Hoc Advisory Group on the Operation of NHS Research Ethics Committees guidelines (2006). Existing data were anonymised and analysed as an intervention in use only to ask the question ‘What standard does this service achieve?’.
Data Analysis
Data were extracted from the referral database and subjected to a number of parameter checks for outliers as well as anomalous data entry. Anomalies were checked against the raw source data to resolve any issues that arose. From the raw data collected, start BMI, end BMI, BMI change, weight change, and percent weight change were calculated. The end weight was calculated based on the members’ last attendance at group during the referral period using the Last Observation Carried Forward approach [15]. Patients were classified as ‘completers’ if they attended at least 10 out of the 12 sessions. Those who completed 9 or fewer sessions were defined as ‘non-completers’.
The effects of different factors on weight loss were assessed by fitting linear models and examining the significance of fitted terms in these models through regression and analysis of variance (ANOVA). Where binary outcomes (e.g. achieving 5% weight loss or not) are reported, the effects of factors were tested by Pearson’s Chi-square tests. Associations between weight losses in different weeks were examined by Pearson’s correlation coefficients. All analysis was performed using the GENSTAT 5 statistical programme (Genstat 5 Rothampstead Experimental Station, Harpenden, UK). Results are expressed as mean (SD) or percents with standard error (SE) where relevant. Where data are presented for men and women and completers and non-completers, the absolute means are given with statistics adjusted for potential confounding factors such as age and height in the regression analyses.
Results
Subjects
Characteristics of the 34,271 subjects (3,651 men; 30,620 women) were as follows: The mean (SD) age was 47.3 (14.4) years, height 1.65 (0.09) m, and weight was 99.4 (20.0) kg. Mean start BMI was 36.8 (6.5) kg/m2 and 25.4% of the referred population had a starting BMI in excess of 40 kg/m2.
Weight Change and Attendance
Mean (SD) weight change of all participants was –4.0 (3.7) kg, percent weight change was –4.0 (3.6), end BMI was 35.3 (6.4) kg/m2, and mean BMI change was –1.5 (1.3) kg/m2. Average (SD) attendance was 8.9 (3.6) sessions. 19,907 (58.1%) of the patients attended at least 10 of the 12 sessions (completers) and 14,364 (41.9%) were classed as non-completers (i.e. those who attended fewer than 10 of the 12 sessions). The characteristics and outcomes for completers and non-completers are given in table 1. Average (SD) attendance of completers was 11.5 (0.7) sessions and that of non-completers was 5.3 (2.6) sessions. 35.8% of the whole population and 54.7% of the completers lost at least 5% and 5.8% of the whole population lost equal to or more than 10% of their body weight over the 12 sessions. In the present audit, 92.1% of all participants lost weight or remained weight stable, using the assumption of the Last Observation Carried Forward Model [15].
Completers and Non-Completers
Table 1 shows that completers lost significantly more weight than non-completers (–5.5 vs. –1.8 kg, respectively; t = 95.09; p < 0.001) during the 12-session referral period. The same patterns were evident for percent weight loss (–5.5 vs. –1.8%, respectively; t = 99.94; p < 0.001). Thus, while completers and non-completers did not differ significantly in terms of initial height or much in weight or BMI, the completers lost a greater weight, percent weight, and had a greater change in BMI (table 1). Non-completers were on average 4.8 years younger than completers (t = –28.12; p < 0.001).
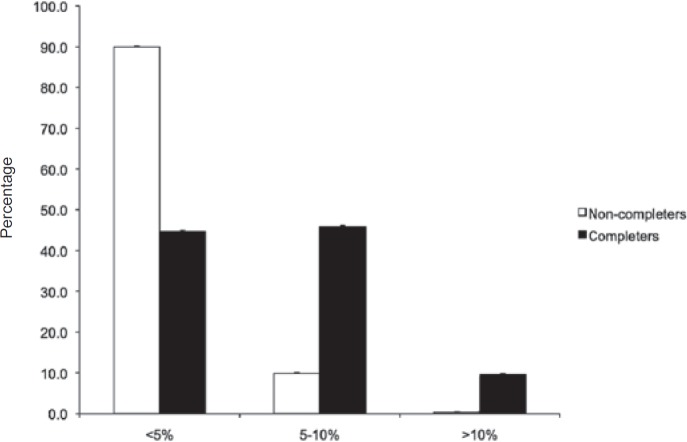
Figure 1 shows the percentage of completers and non-completers who achieved less than 5%, between 5–10%, and >10% weight loss by week 12. 54.7% of completers and 9.7% of non-completers achieved at least 5% weight loss (p < 0.001). 9.7% of completers and 0.3% of non-completers lost at least 10% of their initial body weight by the end of the referral period (p < 0.001).
Men and Women
Table 2 compares the characteristics and weight loss outcomes for men and women. Men were on average taller, older, heavier, and had a higher BMI on enrolment than women (all p < 0.001). Men tended to lose more weight than women both in absolute kg and as a percent of baseline body weight (both p < 0.001). Thus, while they did not, on average, attend to a greater degree than women, they had a greater BMI change than women for the 12 sessions of the referral scheme (p < 0.001). There was, however, a significant difference in the percentage of men and women classed as completers (men = 63.8%; women = 57.4%) (p < 0.001). Male completers and non-completers were significantly older than their female counterparts (p < 0.001). A significantly higher percentage of men than women lost 5% (46.3 vs. 34.6%) and 10% (10.6 vs. 5.2%, respectively) of their baseline weight by the 12th session (p < 0.001).
Rates of Weight Loss
The average rate of weight loss over the 12 sessions (when completed over the 14-week time window) for the total population was 0.3 kg/week. ANOVA showed that men lost weight at a significantly faster rate (0.4 vs. 0.3 kg/week) than women, both in absolute and percent terms (both p < 0.001). Completers lost weight at a significantly faster rate than did non-completers (0.4 vs. 0.1 kg/week). These patterns were also apparent for percent weight loss (both p < 0.001). Analysing only subjects who completed within a 12-week time window increased the slope for rate of weight loss by approximately 6–8%, depending on the group (men or women, completer or non-completer).
The rate of weight loss decreased as the process of weight reduction proceeded from the start to the end of the scheme. Thus the slope for the rate of weight loss was steeper during weeks 1–6 than weeks 7–12 for the whole population and for men compared to women. The rate of deceleration of weight loss was not significantly different between completers and non-completers.
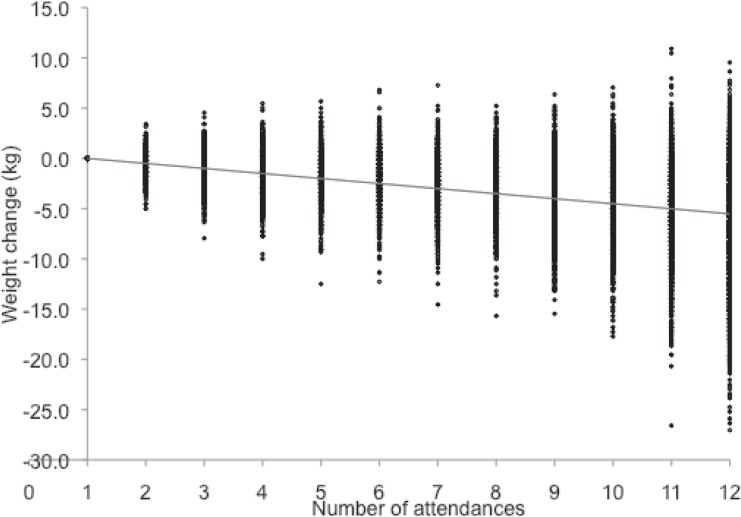
Prediction of Weight Loss
Table 3 gives the regression coefficients for percent weight loss at the end of the referral period for age, height, gender, starting BMI, attendances, and percent weight lost in the first week, together with t-statistics and probability values. It is clear that the greatest predictor of percent weight loss was the number of attendances (table 4). On average men lost more weight than women over the referral period (t = –11.61; p < 0.001). For every unit increase in start BMI subjects tended to lose an additional 0.01% weight by the end of the referral period (t = 3.92; p < 0.001). Age, but not height, significantly predicted percent weight lost by the end of the referral period; as with BMI the effect was small (t = –6.12; p < 0.001). Table 4 shows the accumulated ANOVA for the predictors of weight loss, giving the factors, percent of variance explained, F-ratios, and probability statistics for main effects. It is clear from table 4 that age, height, gender, and starting BMI all explained a very small amount of the variance in percent weight lost. Attendance accounted for 29.6% of the total variance in percent weight lost at the end of the referral period. Percent weight lost during the first week of referral was also an important predictor of total weight lost, accounting for 18.4% of the variance. 50.1% of the variance in weight lost was unaccounted for by this model.
Figure 2 shows the regression of attendance against weight loss over the 12 sessions of the scheme for the whole audit population. The model including attendance and percent weight lost during week 1 accounted for 49.9% of the variability in percent weight loss. As can be seen from table 4, the two key predictors of percent weight loss by the end of the referral period were percent weight lost in the first week and attendance throughout the 12 weekly sessions. However, week 1 weight loss was also related to attendance, since adding week 1 weight loss into the stepwise model first increased the percent variance explained by the first week’s weight loss to 31.3% and decreased the percent of the variance due to attendance to 17.3%. Those who lost more weight in week 1 tended to attend longer. Both cumulative stepwise regression models explained the similar total amounts of variance in percent weight lost.
Discussion
Weight management treatment in primary care is an important first stage of any stepped care model for weight control [4]. Reductions in at least 5% baseline weight can improve health outcomes as well as reduce the need for medication and use of health care resources [16–18]. Modest weight losses are an important component in prevention, since most Western adults appear to gain between 0.2–2.0 kg per annum [19, 20]. The most effective first line of prevention and treatment of obesity is dietary and lifestyle change [1, 8, 10, 12]. Partnership with CWMO has been recommended by various bodies as one means of expanding provision of obesity services in primary care [3, 4, 13]. Commercial organisations have the benefit of resource, infrastructure, and scale, which enables them to offer the regular support that is difficult to achieve within current NHS resources. However, there is a lack of consensus, due to a lack of evidence, as to how effective commercial partnerships are. A comprehensive review of major commercial weight loss programmes in the US noted that there needs to be more evidence to support the use of the major commercial and self-help programmes [21]. Since then evidence is emerging as to how effective commercial behaviour change programmes can be in helping people control their weight [14, 22–26]. The present dataset provides important components of the audit evidence base for the UK.
Rate and Extent of Weight Loss
The current audit is the largest examination of the impact of referral to commercial weight management support conducted in the UK to date. The results are similar to our initial feasibility trial of this scheme [14]. 58.1% of the audit population completed at least 10 of the 12 sessions of the programme, which is similar to previous work by ourselves [14] and others [25]. 35.8% of this whole population and 54.7% of the completers lost at least 5% of their body weight in about 3 months, which is the current recommended initial target weight loss (within 3–6 months), according to the NICE guidelines and the Department of Health [4, 13]. 92.1% of all participants lost weight or remained weight stable if we use the assumptions of the Last Observation Carried Forward Model [15]. It is possible that some of those who dropped out early gained more weight during the 12-session referral period. Nevertheless, these data are encouraging from a preventative perspective, since most adults tend to gain small amounts of weight over this time period [19, 20].
Average start BMI of the audit population was in the range that would be recommended for pharmacotherapy and many for surgery in the UK [4]. Start BMI averaged at 36.8 kg/m2 and 25.4% of this referral population had a BMI > 40 kg/m2. This suggests that lifestyle interventions can work in populations with BMIs that are normally recommended to receive secondary or tertiary care.
Length of Attendance
The data presented in this audit clearly emphasise how important it is for patients to attend or comply with their weight loss programme. In all outcomes, completers fared far better than non-completers. The trajectory of weight loss for the completer and non-completer groups is curvilinear, which is typical for obesity treatments in general [21, 27]. Weight loss begins rapidly and starts to slow as weight loss proceeds. It is clear from this report and a number of other studies in the literature [for review see 12] that attendance is a major correlate of weight lost. The exact mechanisms by which attendance translates into weight loss is not clear and may well differ for different people. For some the group support will be important while for others having their weight monitored by a third party will help with motivation [28]. Further studies are needed to assess which components of group support are important in different people and why some people drop out of the programme prematurely.
Men and Women
Weight losses (absolute and percent) appeared to be higher in men compared to women, although men did not attend a great deal more than did women. The percent of the audit population who were men was about two times greater than is seen among the general group membership (11 vs. about 6%). NHS referral may be an effective means of recruiting more men to attend weight management groups.
Comparison with Other Approaches to Weight Management
People treated with a comprehensive group behavioural approach lose approximately 9% of initial weight in 20–26 weeks of treatment [21]. Although the present dataset only gives a time window of approximately 3 months, results of previous work suggests that if patients continue to attend after the 12-session referral period these losses persist. When the period of audit is extended to 24 sessions, average weight losses of 11.3% have been seen for those still attending the group [14] and also 11.4% in 24 sessions (approximately 24 weeks) in self-referred male members of the CWMO [22]. We are currently developing further trials, with longer-term follow-up as an important adjunct to the present audit.
The present results show a mean weight loss of 4.0% (5.5% for completers) in 12 sessions. These data compare very favourably to pharmacological treatments for obesity [29–31]. Recent reviews and meta-analyses suggest that obesity drugs do not produce more than 5% weight loss on average in 12 months [29–31]. The average weekly net cost of referral to this organisation equates to GBP 3.95 per week, and average weekly weight loss was 0.3 kg. Taking into account the additional costs of health care staff and PCT resources [14], this is a very favourable cost compared to the equivalent prescription costs for obesity drugs, which cost approximately GBP 1.00 per day on a net basis according to the British National Formulary 2009 [32]. Even if we assume that both referral schemes and drugs produced the same weight loss in 3 months the referral scheme would cost GBP 47.39 for about 12 weeks compared to about GBP 84.00 for the net cost of obesity drugs. It can therefore be reasonably concluded that NHS referral schemes for weight loss are a cost-effective option.
Prediction of Weight Loss
The percent of weight lost was not strongly related to initial body weight and so those with more weight to lose did not achieve a greater percent weight loss. However, percent weight lost in the first week was almost as great a predictor of percent weight loss at the end of the referral period as was attendance throughout the referral period. This effect has been found in previous studies [12, 27]. Attendance is discussed above. The relationship between percent weight lost in the first week and end weight loss is less clear. It may be that those who lose a greater percent of baseline weight in the first week are more motivated (either before they attend or as a consequence of their experiences in the first week), so they may have familiarised themselves with the eating and activity programme to a greater extent and are simply on a consistent trajectory of greater weight loss or a combination of these variables. We have previously observed in our commercial weight management groups that those who lose most weight in the first week do go on to lose more weight [33]. Exactly how this relates to motivation and the prevention of lapses and relapses warrants further detailed investigation [7–9].
50.1% of the variance in weight loss was not explained by the simple predictive model, suggesting that much of the variability on weight loss is due to other psychological, behavioural, or even physiological traits of different individuals participating in the scheme. We are currently analysing studies collecting psychological and behavioural determinants of longer-term weight loss success.
Strengths and Limitations of the Study
As this was a service audit, limitations to this study include the absence of a control group and the fact that results were based upon those people who joined a group, rather than intention to treat. There were no comparable and consistent in-house options available in the NHS Trusts to provide a control group. However, the purpose of the study was not to compare the efficacy of this CWMO’s programme with other treatments. It was to audit the effectiveness of NHS referral to the programme in terms of rate and extent of weight loss and attrition rates. This study only observed weight changes over 12 weekly sessions and there was no longer-term follow-up after referral. Additional studies are examining longer-term weight trajectories over 1–2 years. Key strengths were that the referral programme audit assessed the effectiveness of the programme as it runs in real life, the large sample size, and the fact that the subjects were real consumers aiming to control their weight in their everyday lives.
Conclusion
In the present audit, 58.1% of enrolled participants completed at least 10 out of 12 sessions of the programme (completers). A total of 35.8% of all patients enrolled and 54.7% of completers lost at least 5% initial body weight. Weight gain was prevented in 92.1% of patients, using the assumptions of the Last Observation Carried Forward Model. This analysis has demonstrated that partnership working for weight management is effective, benefits patients, and (as previously reported [14]) can be less expensive than other in-house options and pharmacotherapy. It confirms that referral to commercial organisations can be a useful way of extending currently limited NHS resources to tackle the obesity epidemic. Although the initial referral period is limited to about 12 weeks, the partnership opens the door to long-term weight control through self-referral or continued NHS referral. Finally, these data have confirmed that there are two simple basic predictors (attendance and weight loss in the first week) of weight loss that together account for 48.0% of the variability in weight lost by the end of the referral period, which would be valuable indicators of the likelihood a person will lose approximately 5% of their initial body weight in about 12 weeks. In other words, regardless of age, gender, or starting weight, if a person is able to attend 10 or more of the 12 sessions and is supported and encouraged to achieve good weight losses in their first week, they are likely to be successful in beginning their weight loss journey.
Disclosure Statement
R.J. Stubbs, C. Pallister, A. Avery, and J. Lavin work for Slimming World. The analysis of the data was funded by Slimming World.
Fig. 1.
Percent of completers and non-completers achieving less than 5%, between 5–10%, and >10% weight loss by the end of the referral scheme (n = 34,271).
Fig. 2.
Regression of attendance against weight loss over the 12 sessions for the whole audit population (n = 34,271).
Table 1.
The characteristics and weight loss outcomes for completers and non-completers (completers are defined as those who attended for 10 or more of the 12 sessions of the referral period; non-completers are those who attended 9 or fewer sessions)
| Completers, n = 19,907 |
Non-completers, n = 14,364 |
t-value | p-value | |||
|---|---|---|---|---|---|---|
| average | SD | average | SD | |||
| Height, m | 1.65 | 0.09 | 1.65 | 0.09 | −1.46 | 0.144 |
| Weight, kg | 99.7 | 20.1 | 99.0 | 19.8 | −5.32 | <0.001 |
| Age, years | 49.3 | 14.4 | 44.5 | 14.1 | −28.12 | <0.001 |
| Weight change, kg | −5.5 | 3.8 | −1.8 | 2.3 | 95.09 | <0.001 |
| Percent weight change | −5.5 | 3.5 | −1.8 | 2.3 | 99.94 | <0.001 |
| Weeks attended | 11.5 | 0.7 | 5.3 | 2.6 | −292.13 | <0.001 |
| Start BMI, kg/m2 | 36.9 | 6.5 | 36.6 | 6.5 | −5.05 | <0.001 |
| End BMI, kg/m2 | 34.9 | 6.3 | 36.0 | 6.4 | 12.75 | <0.001 |
| BMI change, kg/m2 | −2.0 | 1.3 | −0.7 | 0.9 | 97.81 | <0.001 |
Table 2.
Characteristics and weight loss outcomes for men and women
| Men, n = 3,651 |
Women, n = 30,620 |
t-value | p-value | |||
|---|---|---|---|---|---|---|
| average | SD | average | SD | |||
| Height, m | 1.77 | 0.08 | 1.63 | 0.08 | 93.37 | <0.001 |
| Weight, kg | 117.9 | 22.4 | 97.2 | 18.5 | 52.27 | <0.001 |
| Age, years | 51.4 | 13.8 | 46.8 | 14.4 | 14.66 | <0.001 |
| Weight change, kg | −5.8 | 4.9 | −3.8 | 3.5 | −33.28 | <0.001 |
| Percent weight change | −4.9 | 4.0 | −3.9 | 3.5 | −14.65 | <0.001 |
| Weeks attended | 9.2 | 3.6 | 8.8 | 3.5 | 0.78 | 0.438 |
| Start BMI, kg/m2 | 37.8 | 6.6 | 36.7 | 6.5 | 8.88 | <0.001 |
| End BMI, kg/m2 | 36.0 | 6.5 | 35.3 | 6.4 | 5.85 | <0.001 |
| BMI change, kg/m2 | −1.8 | 1.6 | −1.4 | 1.3 | −17.48 | <0.001 |
Table 3.
Regression coefficients for percent weight loss at the end of the referral period for age, height, gender, starting BMI, attendances, and percent weight lost in the first week, together with t-statistics and probability values (n = 34,271)
| Estimate | Standard error | t (n = 34,184) | p-value | |
|---|---|---|---|---|
| Constant | 1.285 | 0.353 | 3.64 | <0.001 |
| Age, years | −0.006 | 0.001 | −6.12 | <0.001 |
| Height, m | 0.149 | 0.199 | 0.75 | 0.453 |
| Gender, male | −0.612 | 0.053 | −11.61 | <0.001 |
| Start BMI, kg/m2 | 0.008 | 0.002 | 3.92 | <0.001 |
| Attendances | −0.438 | 0.004 | −108.55 | <0.001 |
| % lost in week 1 | 1.429 | 0.013 | 112.02 | <0.001 |
Table 4.
Accumulated ANOVA for the predictors of weight loss, giving the factors, percent of variance explained, F-ratios, and probability statistics for main effects (n = 34,271)
| Change | Degrees of freedom | % variance | F-ratio | p-value |
|---|---|---|---|---|
| Age, years | 1 | 1.3 | 859.21 | <0.001 |
| Height, m | 1 | 0.3 | 167.07 | <0.001 |
| Gender | 1 | 0.3 | 233.55 | <0.001 |
| Start BMI, kg/m2 | 1 | 0.0 | 0.11 | 0.743 |
| Attendances, weeks | 1 | 29.6 | 20,202.28 | <0.001 |
| % weight lost in week 1 | 1 | 18.4 | 12,547.73 | <0.001 |
| Residual | 34,184 |
50.1 | ||
| Total | 34,190 |
Acknowledgement
We are grateful to GW Horgan of Biomathematics and Statistics Scotland, for conducting an independent statistical analysis of the data. We would like to thank the Slimming World on Referral team for entry of the raw data and their general support to all primary care/commercial partnerships.
References
- 1.Government Office for Science Tackling Obesities: Future Choices. London. 2007 [Google Scholar]
- 2.Department of Health/Joint Health Surveys Unit (on behalf of the Department of Health) Forecasting Obesity to 2010. London, The Stationary Office. 2006 [Google Scholar]
- 3.House of Commons Health Select Committee Obesity. London, The Stationary Office. 2004 [Google Scholar]
- 4.National Institute for Health and Clinical Excellence: Obesity: The Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children London, Department of Health. 2006 [PubMed] [Google Scholar]
- 5.World Health Organisation: Obesity: Preventing and Managing the Global Epidemic Geneva, World Health Organisation. 1998 [PubMed] [Google Scholar]
- 6.Swanton K, Frost M. Lightening the Load: Tackling Overweight and Obesity. London, National Heart Forum. 2007 [Google Scholar]
- 7.Brownell KD, Marlatt GA, Lichtenstein E, Wilson GT. Understanding and preventing relapse. Am Psychol. 1986;41:765–782. doi: 10.1037//0003-066x.41.7.765. [DOI] [PubMed] [Google Scholar]
- 8.Brownell KD, Rodin J. The dieting maelstrom. Is it possible and advisable to lose weight? Am Psychol. 1994;49:781–791. doi: 10.1037//0003-066x.49.9.781. [DOI] [PubMed] [Google Scholar]
- 9.Brownell KD, Wadden TA, The heterogeneity of obesity. fitting treatments to individuals. Behav Ther. 1991;22:153–177. doi: 10.1016/j.beth.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Friedman MA, Brownell KD, Psychological correlates of obesity. moving to the next research generation. Psychol Bull. 1995;117:3–20. doi: 10.1037/0033-2909.117.1.3. [DOI] [PubMed] [Google Scholar]
- 11.Foreyt JP, Goodrick GK, Prediction in weight management outcome: implications for practice . Obesity Treatment: Establishing Goals, Improving Outcomes, and Reviewing the Research Agenda. In: Allison DA, Pi-Sunyer FX, editors. New York: Plenum; 1995. pp. pp 199–208. [Google Scholar]
- 12.Institute of Medicine: Weighing the Options: Criteria for Evaluating Weight Management Programmes . Washington D.C.: National Academy Press; 1995. [Google Scholar]
- 13.Department of Health: Healthy Weight, Healthy Lives A Cross-Government Strategy for England. London. 2008 [Google Scholar]
- 14.Lavin JH, Avery A, Whitehead SM, Rees E, Parsons J, Bagnall T, Barth JH, Ruxton CHS. Feasibility and benefits of implementing a Slimming on Referral service in primary care using a commercial weight management partner. Public Health. 2006;120:872–881. doi: 10.1016/j.puhe.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Streiner DL. The case of the missing data: methods of dealing with dropouts and other research vagaries. Can J Psychol. 2002;47:68–75. [PubMed] [Google Scholar]
- 16.Foster GD, Reasonable weights: determinants, definitions and directions . Obesity Treatment Establishing Goals, Improving Outcomes, and Reviewing the Research Agenda. In: Allison DB, Pi-Sunyer FX, editors. New York: Plenum; 1995. pp. pp 35–44. [Google Scholar]
- 17.Heymsfield SB, What is the weight required for substantial health gains? Obesity Treatment Establishing Goals, Improving Outcomes, and Reviewing the Research Agenda. In: Allison DB, Pi-Sunyer FX, editors. New York: Plenum; 1995. pp. pp 21–27. [Google Scholar]
- 18.National Obesity Forum: Guidelines for Management of Adult Obesity and Overweight in Primary Care London, National Obesity Forum. 2004 [Google Scholar]
- 19.Lewis CE, Jacobs DR, McCreath H, Kiefe CI, Schreiner PJ, Smith DE, Williams OD. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Am J Epidemiol. 2000;151:1172–1181. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 20.Williamson DF, Kahn HS, Byers T. The 10-y incidence of obesity and major weight gain in black and white US women aged 30–55 y. Am J Clin Nutr. 1991;53:1515S–1518S. doi: 10.1093/ajcn/53.6.1515S. [DOI] [PubMed] [Google Scholar]
- 21.Wadden TA, Foster GD. Behavioral treatment of obesity. Med Clin North Am. 2000;84:441–461. doi: 10.1016/s0025-7125(05)70230-3. [DOI] [PubMed] [Google Scholar]
- 22.Bye C, Avery A, Lavin J. Tackling obesity in men - preliminary evaluation of men-only groups within a commercial slimming organization. J Hum Nutr Diet. 2005;18:391–394. doi: 10.1111/j.1365-277X.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 23.Heshka S, Anderson JW, Atkinson RL, Greenway FL, Hill JO, Phinney SD, Kolotkin RL, Miller-Kovach K, Pi-Sunyer FX, Weight loss with self-help compared with a structured commercial program. a randomized trial. JAMA. 2003;289:1792–1798. doi: 10.1001/jama.289.14.1792. [DOI] [PubMed] [Google Scholar]
- 24.Pallister C, Avery A, Stubbs J, Lavin J. Influence of Slimming World's lifestyle programme on diet, activity behaviour and health of participants and their families. J Hum Nutr Diet. 2009;22:351–358. doi: 10.1111/j.1365-277X.2009.00959.x. [DOI] [PubMed] [Google Scholar]
- 25.Poulter J, Hunt P. Weight change of participants in the Weight Watchers GP referral scheme. Int J Obes Relat Metab Disord. 2008;32:S233. [Google Scholar]
- 26.Truby H, Baic S, de Looy A, Fox KR, Livingstone MB, Logan CM, Macdonald IA, Morgan LM, Taylor MA, Millward DJ, Randomised controlled trial of four commercial weight loss programmes in the UK. initial findings from the BBC 'diet trials'. BMJ. 2006;332:1309–1314. doi: 10.1136/bmj.38833.411204.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glenny AM, O'Meara S, Melville A, Sheldon TA, Wilson C. The treatment and prevention of obesity: a systematic review of the literature. Int J Obes Relat Metab Disord. 1995;19:893–901. doi: 10.1038/sj.ijo.0800495. [DOI] [PubMed] [Google Scholar]
- 28.Ribisl KM, Humphreys K, Collaboration between professionals and mediating structures in the community: towards a third way in health promotion . The Handbook of Health Behavior Change. In: Shumaker SA, Ockene J, Schron E, McBee W, editors. New York: Springer; 1998. [Google Scholar]
- 29.Padwal R, Li SK, Lau DC, Long-term pharmacotherapy for overweight and obesity. a systematic review and meta-analysis of randomized controlled trials. Int J Obes Relat Metab Disord. 2003;27:1436–1446. doi: 10.1038/sj.ijo.0802475. [DOI] [PubMed] [Google Scholar]
- 30.Wirth A, Krause J. Long-term weight loss with sibutramine: a randomized controlled trial. JAMA. 2001;286:1331–1339. doi: 10.1001/jama.286.11.1331. [DOI] [PubMed] [Google Scholar]
- 31.Torgerson JS, Hauptman J, Boldrin MN, Sjostrom L. XENical in the prevention of Diabetes in Obese Subjects (XENDOS) Study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155–161. doi: 10.2337/diacare.27.1.155. [DOI] [PubMed] [Google Scholar]
- 32.BMJ Group and Royal Pharmaceutical Society of Great Britain Publishing: British National Formulary London. 2009 [Google Scholar]
- 33.Powell C, Lavin J, Russell J, Barker M. Factors associated with successful weight loss and attendance at commercial slimming group. Int J Obes Relat Metab Disord. 2004;28:S144. [Google Scholar]