Abstract
Background
Both group and individual modes of delivery are employed for obesity treatments. Commercial weight loss groups commonly employ group-based delivery, while many clinical based settings employ one-to-one delivery. We systematically reviewed randomised controlled trials of treatments for adult obesity to compare the effectiveness of group-based to individual-based modes of treatment delivery.
Methods
We searched 7 electronic databases and 2 journals and reviewed secondary references, based on a priori criteria to systematically review: randomised controlled trials of obesity treatments, participants with BMI ≥28 kg/m2, age ≥18 years, comparison groups including at least 1 group-based and 1 individual-based treatment group, and follow-up ≥1 year. We extracted data and conducted meta-analysis of weight change.
Results
Eleven comparison groups from 5 qualifying trials were obtained, representing a total participant pool of 336. Significantly greater (p = 0.03) weight change at 12 months was found in group-based over individualbased treatment, and sub-analyses showed that increased effectiveness was associated with the use of financial reward and psychologist-led interventions.
Conclusion
Group-based interventions were more effective than individual-based interventions among a predominantly female participant pool receiving psychologist-led interventions. Future studies to explore differences by professional group and interventions among men, which are accompanied by economic evaluation, are recommended.
Key Words: Obesity, Group versus individual, Randomised controlled trials
Introduction
There is a need for effective and cost-effective approaches to obesity management that are well-tailored to the individual's needs. Exploring the effects of different modes and settings of delivery in treatments for obesity, such as the role of group-based or individual-based treatments, is needed for evidence-based practice in the management of adult obesity, and to plan the design and evaluation of future interventions [1]. Group-based interventions in obesity treatment offer the promise of being more resource-effective and the opportunity for enhanced social support, but are only rarely used in clinical settings, e.g. the UK National Health Service. They may, however, require more space for delivery and special skills in group leaders. In groups there may be more limited opportunities for attending to more specific individual needs, and all participants need to agree to set meeting times and location [2,3].
A previous analysis of group versus individually delivered obesity interventions conducted as part of a broader systematic review of randomised controlled trials (RCTs) [4] reported no significant differences in weight change at 12 months and 18 months but significant effects in favour of individual treatment at the 24-month follow-up. However, these analyses were conducted with few studies, and included some groups that differed in some aspects of treatments received (e.g. intensity, length or type of therapy) that could have influenced the results of comparisons. A second systematic review of group-based training for self-management strategies in people with type 2 diabetes reported clinically and statistically significant benefits (weight change was not among the main outcomes) for group-based patient-centred educational programmes [5], but also included some studies in which treatments received were not comparable across study arms and other studies that did not have any individual-based comparison treatment groups. Another review of group treatments for obese participants [6] also did not compare group to individual setting of delivery.
This systematic review was therefore conducted to address the need for a focused systematic review of RCTs comparing group-based versus individual-based setting for delivery of treatments for adult obesity to determine the long-term effectiveness (and cost-effectiveness if available) of each of these settings in treatments for adult obesity.
Material and Methods
This review was conducted following a pre-specified protocol and reported in keeping with the QUOROM statement [7].
Search Strategy
We searched through our existing database of RCTs and reviews of obesity treatments, made up of screened searches conducted in Medline, Embase, Cinahl, Psychinfo [4] and two update searches with citation alerts to July 2008 [8] for trials involving comparisons of group versus individual mode of delivery of treatments. We complemented this with hand searching for references in two obesity journals (Obesity Research (now Obesity) and the International Journal of Obesity) and cited in identified relevant articles.
Study Selection
Studies were retrieved independently by both reviewers and subjected to selection according to agreed a priori criteria as summarised in table 1.
Quality Assessment
Quality assessment was carried out by the first author on all retrieved relevant studies using the form originally designed in an earlier systematic review [4], and checked by the second author.
Data Abstraction
Using the same form from Avenell [4], data were abstracted by the first author and double-checked by the second author. Graphical data images were scanned onto a computer and analysed. Missing standard deviations (SD) were computed using the linear regression plot of the SD of the mean change in weight on the absolute mean change for weight derived in Avenell et al. [4].
Data Analysis
Meta-analysis, using Review Manager software RevMan version 4.2.10 (The Cochrane Collaboration, Oxford, UK), involving all possible comparison groups from our included studies, was first conducted, followed by pre-specified sub-analyses on whether or not rewards were used as part of treatment and to compare interventions based on the health professional delivering the intervention.
Three planned sub-analyses (duration of intervention above and below the median time period, provision or non-provision of training in group therapy for providers of the intervention, and comparing multi-component to single component interventions) could not be conducted due to insufficient data. Heterogeneity across studies was explored and a fixed effects approach employed where I2 was <50% but a random effects approach employed where I2 was >50% [9].
Results
Results of Search Strategy
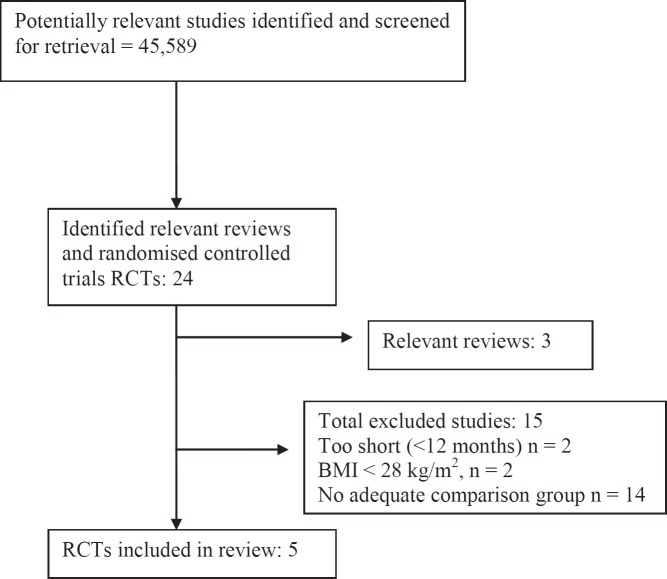
Details of the results of our search strategy are shown in figure 1.
Quality of Included Studies
No study gave details indicating concealment of random allocation. Blinding of participants was not mentioned in any included study, while outcome assessors’ blinding was mentioned only in the most recent study by Waleekhachonloet [10]. Numbers of withdrawals were stated in all included studies and reasons for withdrawals given in two studies [11,12]. Only one study [10] was analysed on an intention-to-treat basis.
Description of Included Studies and Participants
Details of the 5 included studies (1 in the UK, 3 in the USA, and 1 in Thailand) meeting the criteria for inclusion in this systematic review are shown in table 2.
One study included only men [12,13] while in all other studies participants were women. Participants’ ages ranged from 20 to 76 years, and BMI from 30 to 49 kg/m2. Jeffery et al. [12,13] gave details of the socioeconomic group with the mean social class being class III on a 5-point scale, and Waleekhachonloet et al. [10] gave the percentage of participants earning lower and higher than a monthly income of 5,000 Baht (USD 149.30). Ethnicity was not described in any of our included studies. Chronicity of obesity among participants was reported in two studies – in Kingsley and Wilson [14] the mean number of years with obesity was 15.9 and the percentage of participants with obesity since childhood or adolescence 82%, and (our computed) difference between the reported mean age of participants and reported mean age of onset of obesity in Jeffery et al. [12,13] was 26 years. Average number of previous formal weight loss attempts by participants was 1.7 in Kingsley and Wilson [14] while 27% of all participants reported previous formal attempts at weight loss in Jeffery et al. [12,13] which was a study undertaken in men only. No trial reported a pre-treatment programme prior to randomisation. Where mentioned, participants were excluded from the trial if they took medication known to affect weight [10,14].
Description of Interventions
As shown in table 3, all groups used in meta-analyses received general lifestyle and nutrition advice. Stated numbers employed in the group-based treatment groups were between 5 and 7 in Jones et al. [15], 8 and 10 in Straw and Terre [11], and 3 and 12 in Waleekhachonloet et al. [10]. Provision of some training in the delivery of group-based interventions was only implied in two studies, namely Kingsley and Wilson [14] which stated a ‘provision of a therapist orientation manual for all treatment conditions’, and Waleekhachonloet et al. [10] which stated more generally that ‘program providers were trained in nutrition, education and behavioural interventions’. No included studies were explicit about the provision of training in the delivery of group-based treatments.
Two studies employing the use of monetary reward. In the study of Jeffery et al. [12,13], assignment to intervention groups was on the basis of varying the amount of monetary reward and the mode of delivery of this reward (reward for group performance or reward for individual performance); in the study of Kingsley and Wilson [14], all participants were required to make monetary deposits (refundable for attendance at treatment sessions).
Results of Outcomes
Attrition rates ranged from 3.4% in Jeffery et al. [12,13], a study among respondents to an advertisement conducted by psychologists, with treatment involving the use of financial reward, to 64% in Jones et al. [15], a study conducted among referrals from health professionals by dieticians.
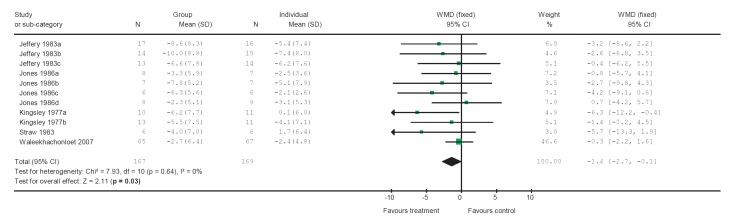
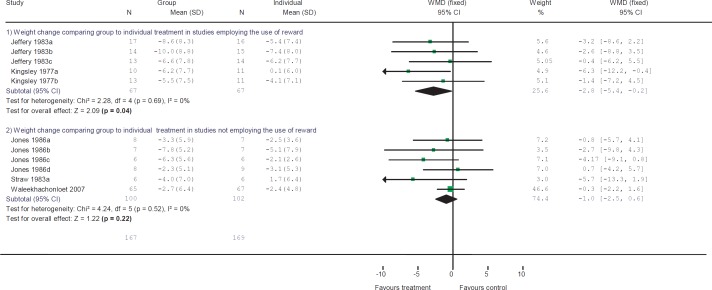
From the 11 comparable groups with group or individual treatment obtained from all five studies, we performed meta-analysis and sub-analyses on weight change at 1 year (fig. 2) and found a statistically significant weight change in group-based over individual treatment with a weighted mean difference (WMD) of −1.4 kg (95% confidence interval (95% CI) −2.7 to −0.1 kg). Sub-analysis comparing group to individual treatment in trials employing the use of financial reward (fig. 3) gave a statistically significant effect in favour of group-based intervention with WMD for weight change at 1 year of −2.8 kg (95% CI −5.4 to −0.2 kg), while comparing group to individual treatment in trials not involving the use of financial rewards showed no significant difference with a WMD for weight change at 1 year of −1.0 kg (95% CI −2.5 to 0.6 kg).
Comparing group to individual treatment in the dietician-led comparison groups gave a non-significant difference with WMD for weight change at 1 year of −1.6 kg (95% CI −4.2 to 1.1 kg), while comparing group to individual treatment in psychologist-led comparison groups gave a statistically significant difference with a WMD for weight change at 1 year of −3.1 kg (95% CI −5.5 to −0.6 kg).
Discussion
In general, the studies did not report some important aspects of RCTs [16], such as the concealment of random allocation, blinding and intention-to-treat analysis. Numbers of dropouts were stated in all studies, and reasons were given in two studies [11,12]. The greatest attrition rates were recorded in dietician-led groups (64%), compared to the rates recorded in the psychologist-led groups (range 3.4–18%). Whether this difference is due to different kinds of individuals represented in the different study groups (the dietician-led groups were referred by health professionals while the psychologist-led groups were self-referred in response to adverts) or to differences in training and/or expertise between the dieticians and the psychologists remains to be explored.
Obesity prevalence is greatest in lower socio-economic groups, but only two studies described participants’ socio-economic status [10,12]. Reporting of socio-economic status of participants would better inform the generalisability of findings. Details of the chronicity of obesity in participants and of previous weight loss attempts as given in two studies [12,14] are also very useful in assessing the generalisability of findings.
Jones et al. [15] reported among inclusion criteria that participants were judged suitable for dietary treatment by the responsible dietician but gave no reference to any tools or guidelines used to ensure uniformity in judgement made by the dieticians. For reasons of external validity and generalisability, we suggest that future studies are more explicit about inclusion and exclusion criteria, protocols, guidelines or other validated tools employed. As noted earlier, we were only able to assume that some training in the delivery of group-based interventions was given to treatment providers in two trials [10,14] and suggest that future studies or evaluated programmes are more explicit in reporting training in group therapy, and incorporate training and monitoring of the delivery of group-based interventions to treatment providers.
In evaluating the effectiveness of group-based interventions, it would be useful to have treatments that are validated and largely comparable across both group and individual comparison groups, and studies should include cost comparisons as was reported in Katz et al. [17].
Some excluded studies did not have comparable lifestyle interventions, intensity of intervention or ease of access to interventions. Such instances include Katz et al. [17] and Yeh et al. [18] who compared a novel group-based ‘skill-building’ intervention to an individual-based ‘counselling’ intervention; Ash et al. [19] who compared a group-based ‘cognitive behaviour therapy’ to individualised ‘dietetic treatment’; Hakala [20] who compared a group counselling intervention (involving a 2-week in-patient period, up to 40 group sessions, a multidisciplinary team, and individual physician appointments) to an individual counselling group (receiving no in-patient treatment phase, and attending 15 maximum possible physician visits); Long et al. [21] who compared individual treatment groups attending ‘weekly weigh-ins with opportunity for feedback’ to a group treatment with participants attending ‘4 brief weigh-ins’ only; and Perri et al. [22] who compared individual treatment participants required to perform home-based exercise to group-based treatment participants who had to access the exercise facility away from home.
Meta-analysis of our included studies showed that group-based interventions are significantly more effective than individual-based interventions. One study excluded for lasting only 6 months [3], in which participants’ preferences were assessed before randomisation to individual- or group-based treatment, also reported group-based treatments to be significantly more effective than individual-based treatments even among participants with expressed preference for the individual setting.
We conclude that group-based interventions are more effective than individual-based interventions in the population represented by the participants in our included studies. Group-based interventions are also potentially more resource-saving in terms of total health professional hours involved per participant. Future cost-effectiveness modelling or economic evaluation studies that incorporate other resources such as the costs for space or for social contacts (e.g. phone call reminders among ‘group-based’ participants) and other perspectives (e.g. societal) could help in informing the development of evidence-based guidelines. We therefore recommend that any future trials or evaluation of group and individual treatments for obesity are accompanied by an economic evaluation. Sensitivity analyses incorporating the costs and effects due to co-morbidities attributable to obesity could further inform the evidence base for decision-makers to provide infrastructure in favour of group-based rather than individual-based services for obesity management. We also found that incorporating financial rewards in treatment is associated with greater effectiveness of obesity treatments. Only one trial [12,13] was conducted in men, so more work is needed to examine the use of group-based approaches in men. Findings from the sub-analyses of groups represented in this systematic review may suggest that psychologists are more effective at group therapy than dieticians (although only one trial had dietician-led groups and recruitment of participants differed). We therefore recommend studies to explore reasons for observed differences in outcome between dieticians and psychologists which might inform training needs.
One of our excluded studies (recruited as groups or as individuals, but did not compare group to individual treatment) [23] has been cited in support of greater success being reported in interventions providing peer support than in interventions without peer support [24]. Although our systematic review was not aimed at comparing the provision of structural support (and there was no report in any of our included studies that the groups in the group-based treatment groups were formed from available significant others) or the provision of functional support (subjective measure of perception of support by the recipient of the intervention), it is assumed that participants in the group-based treatment groups could have developed peer relationships leading to the modification of the social network of participants. Findings in this review are thus in principle in keeping with the statement by Christakis and Fowler [24] that weight loss interventions that provide peer support (thus modifying the social network) are more successful than those that do not.
Disclosure
The authors declared no conflict of interest.
Fig. 1.
Flow chart for selection of studies.
Fig. 2.
Weight change (kg) in group versus individual treatment at 12 months.
Fig. 3.
Sub-analysis of comparison of group to individual treatment by use of financial reward.
Table 1.
Study selection criteria
| Study design | RCTs |
|---|---|
| Participants | Adults, aged ≥18 years Mean BMI ≥ 28 kg/m2 (except among ethnic groups with obvious justification to allow for a lower cut-off BMI) No groups with obesity-associated eating disorders, e.g. binge eating disorder |
| Intervention | Any weight loss trial with at least one comparable group-based intervention to individual-based intervention Follow-up for at least 1 year |
| Principal outcome | Change in weight or BMI |
Table 2.
Details of included studies
| Reference | Participants | Interventions | Outcomes | Other observations |
|---|---|---|---|---|
| Jeffery et al., 1983 [12]; Jeffery et al., 1984 [13] |
Country: USA Source of recruitment: ineligibles from an existing trial pool Mean age (range): 52.8 (35–57) years Sex: 100% male Mean weight: 100.2 kg Mean BMI: 31.8 kg/m2 SES: 33.1 Mean age of onset: 26.7 years % with prior weight program experience: 27 |
All: Educational programme on behaviour, diet and exercise; weekly group meetings; calorie and exercise records. Groups: Assigned by amount of initial deposit and means of refund:
|
Randomisation to follow-up assessment: 67 weeks and 119 weeks Overall attrition rates: 3.4% at 67 weeks and 1.1% at 119 weeks Outcomes:
|
Possible failure of randomisation as heavier individuals happened to be in groups assigned to larger monetary deposits. Only aspect of treatment differing in setting (comparing group vs. individual) is the means of refund. |
| Jones et al., 1986 [15] |
Country: UK Source of recruitment: referrals to dietetic service from medical practitioners Mean age: 50.3 years Sex: 100% female Weight: not given Mean BMI: 35.1 kg/m2 SES: not indicated Other: mean % overweight (SD): 52 (11.2) |
All (n = 160): Individualised dietary advice of 1,000 kcal/day or 1,000 kcal/day below energy requirements at first session and offered four additional (or more ‘if warranted’) additional sessions = ‘A’ Groups:
|
Randomisation to follow-up assessment: 69 weeks Overall attrition rate: 64% Outcomes:
|
Authors’ statement that ‘participants should have been judged suitable for dietary treatment by the responsible dietician’ makes the objectivity in making such judgement unclear |
| Kingsley and Wilson, 1977 [14] |
Country: USA Source of recruitment: newspaper advertisement Age (range): 20–60 years Sex: 100% female Weight: not given BMI: not given SES: not indicated % with obesity from childhood/adolescence: 87.2 Average years with obesity: 15.9 Participants’ average number of prior weight programs: 1.7 |
All (n = 78): USD 55.– contracts of which USD 25.– refundable for attendance during treatment and USD 25.– refundable for attendance during maintenance, and dietary advice to limit to 1,200 kcal/day with or without exercise. Groups:
|
Randomisation to follow-up assessment: 60 weeks Overall attrition rate: 16.7% Outcome: i) Weight | ‘Social pressure’ intervention groups (‘v’ and ‘vi’) not used in meta-analysis for lack of comparable individual treatment groups. Individual weight loss was reported even in the group-based treatment groups (i, ii, v, and vi). Paired comparison (post hoc) of therapist competency ratings significantly higher in individual than group conditions. No significant difference in participants’ rating of program usefulness for effecting weight loss. Participants’ rating of programme usefulness for effecting behaviour change in favour of groups ‘i’ to ‘iv’ but not ‘v’ and ‘vi’. Booster conditions significantly better at 3 and 6 months, but not at 9 months and 12 months follow-up |
| Straw and Terre, 1983 [11] |
Country: USA Source of recruitment: newspaper advertisement Mean age (range): 39.3 (23–76) years Sex: 100% female Mean weight (range): 85.8 (60.6–135.6) kg BMI: not stated SES : not indicated |
All (n = 49): Active intervention phase made of ten 1-hour weekly meetings. Optional participation in maintenance phase. Possible maintenance conditions are ‘a’ or ‘b’ below. ‘a’ = weigh in only maintenance made of monthly weight checks ‘b’ = individual problem solving condition made of twice monthly (about 30-min) sessions for 3 months and then monthly until the 12-month follow-up. Subjects not wishing to participate in maintenance assigned to type ‘a’ maintenance condition. Groups:
|
Randomisation to follow-up assessment: 52 weeks Overall attrition rate: 18% Outcome:
|
Baseline data reported for completers only (n = 42) For groups ‘v’ and ‘vi’, authors state that ‘some clinical judgement was exercised in choosing the target problems’ and the client was asked to rank order her problems where consensus could not be reached by author and therapist. Groups ‘v’ and ‘vi’ not used in meta-analysis because there was no comparable group-based intervention group. Group ‘ii’ in reality experienced both a group-based treatment (first 10 weeks) and an individual treatment (during type ‘b’ maintenance). |
| Waleekhachonloet et al., 2007 [10] |
Country: Thailand Source of recruitment: unspecified Age (mean / by group: 38.6 years/individual / 38.3 years/group Sex: 100% female Weight (mean / by group): 70.1 kg/individual / 69.7 kg/group BMI (mean / by group): 28.9 kg/m2/individual / 28.8 kg/m2/group SES (% earning less than 5,000 Baht) (mean / by group): 94.6%/individual; 95.3%/group |
All: Goal of 1% weight loss per month; 4 behaviour therapy sessions using constructs of theory of planned behaviour including intention, perceived behavioural control, attitude and subjective norm; instructions given to maintain a physically active lifestyle and a low calorie diet of approximately 1,200–1,500 kcal/day; Weight control handbook for self-study provided. Groups: i) Meetings lasting 60 min per session with programme provider in groups with a 1:5 provider to participant ratio. ii) Meetings lasting 30 min each with programme provider. |
Randomisation to follow-up assessment: 52 weeks Overall attrition rate: 9% Outcome:
|
Behaviour change measurements employed – intention, attitude toward behaviour change, subjective norm and perceived behavioural control were not significantly different between groups at 1 year. |
HR = Heart rate; SES = socio-economic status (Hollingshead two factor index of social position).
% value computed from numbers or fractions provided.
Table 3.
Description of study groups used in meta-analyses
| Study and year (group vs. individual comparison groups) | Health professional | Active intervention/randomisation to follow-up, weeks | Group therapy training provided | Number assigned to ‘group’ setting | Monetary reward employed | Multi-component (details) |
|---|---|---|---|---|---|---|
| Jeffery et al., 1983 [12] (iv vs. i) | psychologist | 16/67 | U | U | Y (monetary USD 30.– for weight) | Y (B and L) |
| Jeffery et al., 1983 [12] (v vs. ii) | psychologist | 16/67 | U | U | Y (monetary USD 150.– for weight) | Y (B and L) |
| Jeffery et al. 1983 [12] (vi vs. iii) | psychologist | 16/67 | U | U | Y (monetary USD 300.– for weight) | Y (B and L) |
| Jones et al., 1986 [15] (i vs. ii) | dietician | 17/69 | N | 5–7 | N | Y (B and L with monitoring diary) |
| Jones et al., 1986 [15] (iii vs. iv) | dietician | 17/69 | N | 5–7 | N | Y (B and L) |
| Jones et al., 1986 [15] (v vs. vi) | dietician | 17/69 | N | 5–7 | N | N (L with monitoring diary) |
| Jones et al., 1986 [15] (vii vs. viii) | dietician | 17/69 | N | 5–7 | N | N (L only) |
| Kingsley and Wilson, 1977 [14] (i vs. iii) | psychologist | 8/60 | A | U | Y (monetary USD 50.– for attendance) | Y (B and L) |
| Kingsley and Wilson, 1977 [14] (ii vs. iv) | psychologist | 26/60 | A | U | Y (monetary USD 50.– for attendance) | Y (B and L) |
| Straw and Terre, 1983 [11] (i vs. iii) | psychologist | 10/52 | N | 8–10 | N | Y (B and L) |
| Waleekhachonloet et al., 2007 [10] (i vs. ii) | unspecified | 10/52 | A | 3–12 | N | Y (B and L) |
Y = Yes; N= no; U = unclear or not stated; A = can be assumed or implied; B = behavioural programme; L = lifestyle (including diet and exercise) advice; E = supervised/prescribed exercise.
Acknowledgments
The Health Services Research Unit is funded by the Chief Scientist Office of the Scottish Government Health Directorates. Alison Avenell is funded by a Career Scientist Award from the Chief Scientist Office of the Scottish Government Health Directorates.
References
- 1.Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, Tyrer P. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ayala GX. An experimental evaluation of a group-versus computer-based intervention to improve food portion size estimation skills. Health Educ Res. 2006;21:133–145. doi: 10.1093/her/cyh049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Renjilian DA, Perri MG, Nezu AM, McKelvey WF, Shermer RL, Anton SD. Individual versus group therapy for obesity: effects of matching participants to their treatment preferences. J Consult Clin Psychol. 2001;69:717–721. [PubMed] [Google Scholar]
- 4.Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, Smith WC, Jung RT, Campbell MK, Grant AM. Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement. Health Technol Assess. 2004;8:21. doi: 10.3310/hta8210. [DOI] [PubMed] [Google Scholar]
- 5.Deakin T, McShane CE, Cade JE, Williams RDRR. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;2:CD003417. doi: 10.1002/14651858.CD003417.pub2. www.cochrane.org/reviews/en/ab003417.html. [DOI] [PubMed] [Google Scholar]
- 6.Melcarne R, Cognolato S, Santonastaso P. Group therapy programmes for obese patients. Minerva Gastroenterol Dietol. 1996;42:27–38. [PubMed] [Google Scholar]
- 7.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Lancet. 1999;354:1896–1900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 8.Paul-Ebhohimhen V, Avenell A. Long-term effects of financial incentives on treatments for obesity: a systematic review of randomised controlled trials. Obes Rev. 2007;9:355–367. doi: 10.1111/j.1467-789X.2007.00409.x. [DOI] [PubMed] [Google Scholar]
- 9.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waleekhachonloet O, Limwattananon C, Limwattananon S, Gross CR. Group behavior therapy versus individual behavior therapy for healthy dieting and weight control management in overweight and obese women living in rural community. Obes Res Clin Pract. 2007;12:223–232. doi: 10.1016/j.orcp.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Straw MK, Terre L. An evaluation of individualized behavioral obesity treatment and maintenance strategies. Behav Ther. 1983;14:255–266. [Google Scholar]
- 12.Jeffery RW, Gerber WM, Rosenthal BS, Lindquist RA. Monetary contracts in weight control: effectiveness of group and individual contracts of varying size. J Consult Clin Psychol. 1983;51:242–248. doi: 10.1037//0022-006x.51.2.242. [DOI] [PubMed] [Google Scholar]
- 13.Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist RA, Johnson SL. Behavioral treatment of obesity with monetary contracting: two-year follow-up. Addict Behav. 1984;9:311–313. doi: 10.1016/0306-4603(84)90027-3. [DOI] [PubMed] [Google Scholar]
- 14.Kingsley RG, Wilson GT. Behavior therapy for obesity: a comparative investigation of long-term efficacy. J Consult Clin Psychol. 1977;45:288–298. doi: 10.1037//0022-006x.45.2.288. [DOI] [PubMed] [Google Scholar]
- 15.Jones SE, Owens HM, Bennett GA. Does behaviour therapy work for dietitians? An experimental evaluation of the effects of three procedures in a weight reduction clinic. Hum Nutr Appl Nutr. 1986;40:272–281. [PubMed] [Google Scholar]
- 16.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. Lancet. 2001;357:1191–1194. [PubMed] [Google Scholar]
- 17.Katz DL, Chan W, Gonzalez M, Larson D, Nawaz H, Abdulrahman M, Yeh MC. Technical skills for weight loss: preliminary data from a randomized trial. Prev Med. 2002;34:608–615. doi: 10.1006/pmed.2002.1025. [DOI] [PubMed] [Google Scholar]
- 18.Yeh MC, Rodriguez E, Nawaz H, Gonzalez M, Nakamoto D, Katz DL. Technical skills for weight loss: 2-y follow-up results of a randomized trial. Int J Obes Relat Metab Disord. 2003;27:1500–1506. doi: 10.1038/sj.ijo.0802430. [DOI] [PubMed] [Google Scholar]
- 19.Ash S, Reeves M, Bauer J, Dover T, Vivanti A, Leong C, Sullivan TO, Capra S. A randomised control trial comparing lifestyle groups, individual counselling and written information in the management of weight and health outcomes over 12 months. Int J Obes. 2006;30:1557–1564. doi: 10.1038/sj.ijo.0803263. [DOI] [PubMed] [Google Scholar]
- 20.Hakala P, Karvetti RL, Ronnemaa T. Group vs. individual weight reduction programmes in the treatment of severe obesity - a five year follow-up study. Int J Obes Relat Metab Disord. 1993;17:97–102. [PubMed] [Google Scholar]
- 21.Long CG, Simpson CM, Allott EA. Psychological and dietetic counselling combined in the treatment of obesity: a comparative study in a hospital outpatient clinic. Hum Nutr Appl Nutr. 1983;37:94–102. [PubMed] [Google Scholar]
- 22.Perri MG, Martin AD, Leermakers EA, Sears SF, Notelovitz M. Effects of group- versus home-based exercise in the treatment of obesity. J Consult Clin Psychol. 1997;65:278–285. doi: 10.1037//0022-006x.65.2.278. [DOI] [PubMed] [Google Scholar]
- 23.Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol. 1999;67:132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- 24.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]