Abstract
Objective
This study aims to estimate the up-to-date prevalence of overweight/obesity in the suburban area of Beijing, China, and its associations with hypertension, diabetes, dyslipidemia, and metabolic syndrome (MetS).
Methods
A cross-sectional survey in 19,003 suburban adults was carried out in Beijing, 2007. Overweight and obesity class 1, 2, and 3 were defined as a body mass index (BMI) of 25.0–29.9, 30.0–34.9, 35.0–39.9, and = 40 kg/m2, respectively.
Results
The age-standardized prevalence of overweight/obesity was 31.9% in the study. With increasing BMI, the prevalence of hypertension, diabetes, dyslipidemia, and MetS also increased. With normal body weight as reference, the adjusted odds ratio (95% confidence interval) of hypertension for overweight and obesity class 1–3 was 2.5 (2.2–2.7), 3.1 (2.8–3.4), 3.6 (3.1–4.3), and 4.5 (4.0–5.2), respectively. The same trend was observed for diabetes and MetS. For dyslipidemia, however, participants with obesity class 2 had the highest odds ratio.
Conclusion
The prevalence of hypertension, diabetes, dyslipidemia, and MetS increases with increasing BMI. Overweight/obesity is an important risk factor for these diseases. To reduce the social burden of these obesity-related diseases, effective strategies for the prevention of overweight/obesity should be implemented.
Key Words: Overweight, Obesity, Diabetes, Hypertension, Dyslipidemia, Metabolic syndrome
Introduction
With the rapid industrialization and urbanization in recent decades, the prevalence of overweight and obesity has increased significantly in China. Data from the China National Nutrition and Health Survey (CNNS) in 2002 indicates that the prevalence of overweight and obesity is 18.9 and 2.9%, respectively, among adults aged 18 years and over, with overweight defined as a body weight index (BMI) of 25.0–29.9 kg/m2 and obesity as a BMI of 30.0 kg/m2 or greater [1]. Between 1992 and 2002, the prevalence of overweight and obesity increased by about 38.6 and 80.6%, respectively, among Chinese residents, with a 40.7% increase in overweight detection rate and 97.2% increase in obesity prevalence among adults [1].
Overweight/obesity is an important modifiable risk factor for cardiovascular disease (CVD) and other chronic diseases [2–5]. Excess weight has been shown to be associated with increased prevalence of type 2 diabetes, hypertension, dyslipidemia, metabolic syndrome (MetS) and certain cancers; while weight loss dramatically reduces these obesity-related diseases [6, 7]. These diseases have become the main cause of death worldwide [8]. In China, chronic diseases, most of which relate to overweight/obesity, account for 85% of all deaths in urban and 84% of deaths in rural areas [9]. An improved understanding of the associations between obesity and obesity-related diseases may increase public awareness of the benefits of maintaining a healthy weight, which is of special importance for obesity prevention and treatment in areas where industrialization and urbanization are taking place. The aims of the present study were to i) provide the up-to-date prevalence estimates of overweight/obesity in individuals aged 18 years and over; ii) investigate the associations between overweight/obesity and the above obesity-related diseases in the suburban area of Beijing, China.
Participants and Methods
Study Population
A cross-sectional population-based survey by stratified multi-stage cluster sampling was conducted in the Haidian district suburban area of Beijing, 2007. In brief, a random 3-stage stratified sampling method was used to select a representative sample of the general population. In stage 1, 5 towns were randomly selected. In the second stage of sampling, 30 villages/street districts were randomly selected from a total of 76 villages/street districts. In the final stage, a total of 20,655 people aged 18 years and over were randomly chosen from these districts and invited to participate, whose age and sex distribution was similar to that of the total population. Finally, 19,003 people completed the anthropometric survey and laboratory examination and were included in the present study. The overall response rate was 92.0% (men 89.7%, women 92.9%).
Data Collection
Data collection was performed in local health centers or in community clinics in the participant’s residential area. During the study visit, trained research staff members administered a standardized questionnaire to obtain the subject’s information of age, sex, education, family history, physical activity, alcohol use, dietary habits, cigarette smoking, and the previous diagnosis and treatment of certain diseases including hypertension, high cholesterol, and diabetes. Body weight and height were measured twice during the interview. Weight was measured in light indoor clothing without shoes on electronic scales placed on a firm level surface to the nearest 0.1 kg. Height was measured without shoes with a wall-mounted stadiometer to the nearest 0.1 cm. Blood pressure was measured 3 times for participants in the seated position after at least 5 min of rest using a calibrated mercury sphygmomanometer. Participants were advised to avoid cigarette smoking, alcohol, caffeinated beverages, and exercise for at least 30 min before measurement.
Laboratory Measurements
Overnight fasting blood specimens were obtained by venipuncture for measurement of serum lipids and plasma glucose. Participants who did not meet overnight fasting were asked to visit centers later when their fasting time was more than 10 h. Blood specimens were centrifuged and plasma was stored at –80 °C until the laboratory assay. Plasma glucose was measured using a modified hexokinase enzymatic method (Hitachi Automatic Clinical Analyser, Model 7060, Tokyo, Japan). Concentrations of total cholesterol (TC), high density lipoprotein (HDL) cholesterol, and triglycerides (TG) were assessed enzymatically with commercially available reagents [10]. Lipid measurements were standardized according to the criteria of the Centers for Disease Control and Prevention – National Heart, Lung, and Blood Institute Lipid Standardization Program [11]. For participants with a TG level < 4.5 mmol/l, low density lipoprotein (LDL) cholesterol levels were calculated from the Friedewald equation (LDL cholesterol = TC – HDL cholesterol – TG/5) [12]. All subjects had complete laboratory results.
Criteria for Data Interpretation
BMI was calculated as body weight in kilograms per square meters of height. Overweight and obesity class 1, 2, and 3 were defined as a BMI of 25.0–29.9, 30.0–34.9, 35.0–39.9, and ≥ 40 kg/m2, respectively [13]. In this study, we did not differentiate between normal weight and underweight class.
Hypertension was defined as an average (calculated from 3 measurements) systolic blood pressure (SBP) ≥ 140 mm Hg and/or an average diastolic blood pressure (DBP) ≥ 90 mm Hg. Participants on self-reported regular antihypertensive treatment were considered to have hypertension [14].
Diabetes was diagnosed as having a fasting plasma glucose (FPG) level ≥ 7.0 mmol/l or the self-reported the previous diagnosis of diabetes, or current use of anti-diabetes medication [15].
Dyslipidemia included any one of the following: TC ≥ 5.2 mmol/l, TG ≥ 1.7 mmol/l, HDL cholesterol < 1.0 mmol/l, LDL cholesterol ≥ 3.4 mmol/l. Dyslipidemia also included participants who reported treatment with cholesterol-lowering medication [11].
According to the criteria from the China Diabetes Society (CDS), MetS was defined as the presence of 3 or more of the following risk factors: BMI ≥ 25 kg/m2; serum TG ≥ 1.7 mmol/l and/or HDL cholesterol < 0.9 mmol/l in men or < 1.0 mmol/l in women; blood pressure ≥ 140/90 mm Hg or patients with hypertension; or serum glucose concentration ≥ 6.1 mmol/l or patients with diabetes [16].
Statistical Analysis
Data were analyzed using SAS (version 9.1, 2005, SAS Institute Inc, Cary, NC). Descriptive statistics, such as means for continuous variables and their 95% confidence interval (CI), frequencies for categorical variables were computed. Differences in continuous variables were tested using t tests for independent samples. Prevalence of overweight/obesity by sex was compared using χ2 test, and prevalence trends across age group were analyzed using trend χ2 test. PROC SURVEYFREQ was used to obtain the prevalence of hypertension, diabetes, dyslipidemia, and MetS by different BMI, age and sex standardization was performed with the China 2000 Census population as the standard population. Odds ratio (OR) with 95% CI adjusted for age, sex, smoking, drinking, and other potential confounders was calculated by multivariate logistic regression to estimate the associations of hypertension, diabetes, dyslipidemia and MetS with overweight/obesity. Statistical significance was established at p < 0.05.
Results
General characteristics of the study participants are shown in table 1. A total of 19,003 people (7,148 men and 11,855 women) aged 18 years and over were included in this study. The average age of all participants was 48.0 (95% CI 46.5–49.6) years old. The average BMI was 23.7 (95% CI 23.2–24.3) kg/m2. The average age and BMI between men and women had no statistically significant difference (p > 0.05). Men had higher body weight, SBP, DBP, and TG (all p < 0.05). Conversely, women had higher FPG, TC, LDL cholesterol, and HDL cholesterol (all p < 0.05).
As shown in table 2, the age-standardized prevalence of overweight/obesity was 31.9% (24.2% for overweight and 7.7% for obesity). Although there was no significance in the overall prevalence of overweight/obesity between different genders (32.4% in men and 31.6% in women), the prevalence of overweight was significantly higher and the prevalence of obesity class 2 and 3 was significantly lower in men than in women (all p < 0.05). Prevalence of overweight and obesity class 1–3 increased in groups age < 50 years old, and decreased in groups age ≥ 40 years old among men and women (all p <0.05).
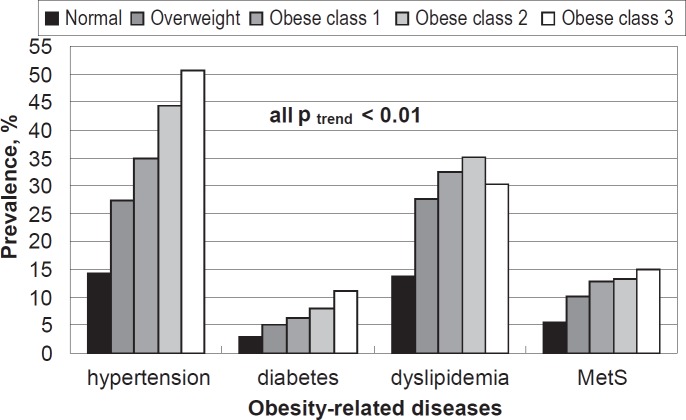
In general, the prevalence of hypertension, diabetes, dyslipidemia, and MetS was 33.6, 6.1, 30.3, and 11.6%, respectively. The prevalence of these conditions by BMI is shown in figure 1. The test for trend showed a significant increase of prevalence with increasing BMI classification of these obesity-related diseases. The most common obesity-related disease was hypertension, followed by dyslipidemia, MetS, and diabetes. For hypertension, the prevalence was 27.5, 34.8, 44.3, and 50.7% in the participants with overweight and obesity class 1–3, respectively. The same trend was observed for diabetes and MetS. It is notable that the highest prevalence of dyslipidemia was in the participants with obesity class 2 (35.1%), instead of obesity class 3 (30.4%).
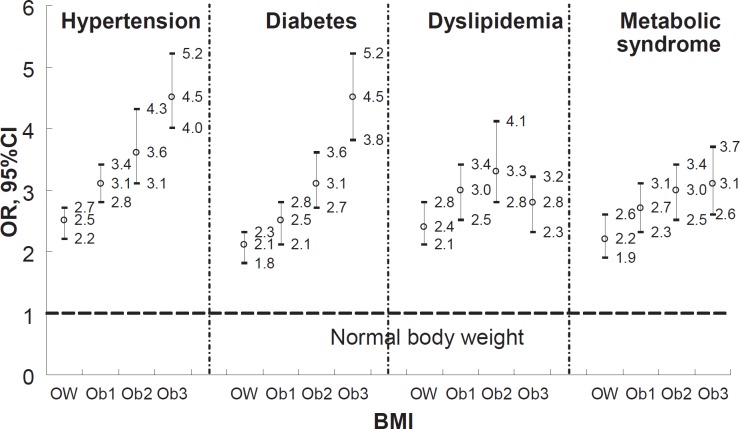
The adjusted OR (95% CI) was calculated by multivariate logistic regression to estimate the associations between obesity-related diseases and BMI (fig. 2). For hypertension, the participants with overweight and obesity class 1–3 had an adjusted OR of 2.5 (2.2–2.7), 3.1 (2.8–3.4), 3.6 (3.1–4.3), and 4.5 (4.0–5.2), respectively, with normal body weight as reference. The same trend was observed for diabetes and MetS, where the participants with obesity class 3 had the highest OR of 4.5, (3.8–5.2) and 3.1 (2.6–3.7), respectively. For dyslipidemia, however, the participants with obesity class 2 had the highest odds ratio of 3.3 (2.8–4.1).
Discussion
In this population-based cross-sectional study, the age-standardized prevalence of overweight/obesity was 31.9% in the suburban areas of Beijing. The prevalence in our study was notably high compared with that from CNNS data under the same criteria [1]. A possible explanation is the different area from which participants were recruited. Beijing as the capital is one of the biggest metropolises in China, and the suburban area of Beijing is experiencing rapid industrialization and urbanization which has dramatically changed the individual lifestyle. The previous CNNS study also demonstrated the high prevalence of overweight/obesity in Northern China including Beijing [17, 18]. Thus, the relatively high prevalence in our study is not surprising. On the other hand, our study was conducted in 2007. The high prevalence reflects, at least in part, the real increase in prevalence from 2002 when the CNNS study was conducted to 2007 when our study was conducted. Hence, a population-based nationwide survey for obesity should be carried out to update this data.
Several surveys with a relatively small sample size have been conducted in China. For example, one study from the metropolis of Shanghai found that the prevalence of overweight/obesity (BMI ≥ 25 kg/m2) was 44.6% among adults aged 40 years and over [5]. Another study from Beijing and Shanghai provided a prevalence as high as 53.4% in adults aged 50–70 years when overweight/obesity was classified as BMI ≥ 24 kg/m2 [18]. The high prevalence in both studies was due to the higher age and/or lower criteria for overweight/obesity. Some studies suggested that a BMI cut-off of 24 kg/m2 might be appropriate for the criteria of overweight in China [3, 18]. In our study, the cut-off of 25 kg/m2 was used because the WHO Expert Consultation [19] agreed that this cut-off point should be maintained for international comparison. Data also show the prevalence of overweight/obesity in US adults aged 18 years and over to be 66.3% [20]. In comparison, the prevalence observed in China was notably low. However, this is not a reason to ignore this issue because prevalence in China is increasing and has an impact on many chronic diseases. Overweight and obesity have been consistently associated with the risk of CVD as well as other chronic conditions such as hypertension, diabetes, dyslipidemia, and MetS [2–7]. The health consequences of overweight and obesity have become the main problem of public health worldwide.
In the present study, the participants showed the highest prevalence of hypertension among the observed obesity-related diseases. Its prevalence increased with increasing BMI and the prevalence was 4.7-fold higher in the participants with obesity class 3 (BMI ≥ 40 kg/m2) than in the participants with non-overweight/obesity. Our study was consistent with previous studies from China and other countries [4, 5, 21, 22]. For example, participants with obesity (BMI ≥ 25 kg/m2) had an adjusted OR of 2.5 (1.9–3.1) with normal body weight as reference in a study with adults aged 40 years and over in Shanghai, China [5]. A US study collected data from participants aged 18 years and over and used the same criteria for overweight/obesity as our study [4]. Interestingly, the participants with overweight and obesity class 1 had a higher OR in our study than in the US study (2.5 vs. 1.7 for overweight; 3.1 vs. 2.6 for obesity class 1), suggesting that the impact of BMI on hypertension may be greater in the Chinese population. Since hypertension is an important risk factor for CVD and diabetes [23, 24], lower BMI cut-off might be appropriate to use as a threshold for public health action in the Chinese population.
The prevalence of diabetes was 6.1% in our study, which is the same as shown in participants aged 20–74 years from Qingdao City, China [25]. The prevalence increased with increasing BMI, which was consistent with previous studies [4, 5, 22]. In other words, obesity is a risk factor for diabetes, and this risk factor becomes stronger for extreme obesity. Similar to hypertension, participants with overweight and obesity class 1 in our study had a higher OR for diabetes than observed in the US study (2.1 vs. 1.2 for overweight; 2.5 vs. 1.6 for obesity class 1) [4]. It has been reported that there is a high prevalence of diabetic patients who remain undiagnosed in Mainland China [26], and obese participants are no more likely to have their diabetes diagnosed than normal-weight participants [27]. Thus, the diagnosis and treatment of diabetic patients from obese populations is urgently needed to decrease the social burden of this obesity-related disease.
In the present study, the highest prevalence of dyslipidemia was found in participants with obesity class 2, instead of obesity class 3. Other studies also showed that the increase in the prevalence of dyslipidemia peaked for individuals with obesity class 2 and hit a plateau for obesity class 3 individuals; they found that the prevalence of dyslipidemia increases until BMI surpasses 30 kg/m2 and decreases with BMI > 40 kg/m2 [4, 22]. This was considered to be linked to the conservative definition of dyslipidemia including the following criteria: TC ≥ 6.22 mmol/l, TG ≥ 2.26 mmol/l, HDL cholesterol < 1.04 mmol/l, LDL cholesterol ≥ 4.14 mmol/l [21]. However, the definition in our study (TC ≥ 5.2 mmol/l, TG ≥ 1.7 mmol/l, HDL cholesterol < 1.0 mmol/l, LDL cholesterol ≥ 3.4 mmol/l) was less conservative. Thus, a further study should be carried to explore this unanticipated phenomenon.
MetS has become a major public health issue worldwide. The prevalence of MetS in a cross-sectional survey of 15,540 Chinese adults aged 35–74 years was 9.8% in men and 17.8% in women [16]. In another study conducted in China with 10,326 participants aged 50–85 years, the prevalence was 15.6% [28]. Caution should be used in direct comparisons because those 2 studies selected older participants and used the definition of the US National Cholesterol Education Program (NCEP) instead of CDS. Similar to hypertension and diabetes, an increasing overweight and obesity class was associated with increased prevalence of MetS in our study and the study from the USA [4].
A limitation of our study is its reliance on estimates derived from a cross-sectional study. Cross-sectional study design does not allow for quantification of the importance of overweight/obesity in the incidence of these obesity-related conditions, which limits our ability to comment on causal relationships between overweight/obesity and the incidence of these conditions. However, previous studies have demonstrated the importance of overweight/obesity for the development of obesity-related conditions. Nevertheless, a further prospective study can be considered among the population in the future. A second limitation is that the applicability of diagnostic thresholds for overweight/obesity may be questioned. Despite some previous reports that BMI ≥ 24 kg/m2 may best define overweight/obesity among Chinese adults, we chose BMI ≥ 25 kg/m2 to defined overweight/obesity for the current analysis to provide a prevalence of overweigh/obesity that is comparable to other studies and populations (such as Europeans, Japanese, and Americans).
Conclusion
In summary, findings from the present study showed an association between increasing BMI and an increase in the prevalence of hypertension, diabetes, dyslipidemia, and MetS. Overweight/obesity is an important risk factor for these obesity-related diseases. Some programs for body weight control should be initiated to combat these obesity-related conditions and reduce the overwhelming burden on the Chinese health care system.
Disclosure Statement
The authors declare no conflict of interests.
Fig. 1.
The age and sex standardized prevalence of obesity-related diseases by BMI classification.
Fig. 2.
Multivariate logistic regression adjusted odds ratio (adjusted for age, sex, drinking, smoking, physical activity) of obesity-related diseases by BMI (OW = overweight, Ob = obesity class).
Table 1.
General characteristics of the study participantsa
| Characteristics | Total | Men | Women | p valueb |
|---|---|---|---|---|
| Age, years | 48.0 ± 6.9 | 47.7 ± 7.1 | 48.2 ± 6.9 | > 0.05 |
| Weight, kg | 68.0 ± 11.2 | 74.1 ± 11.5 | 64.5 ± 11.4 | < 0.01 |
| BMI, kg/m2 | 23.7 ± 3.3 | 23.8 ± 3.1 | 23.6 ± 3.0 | > 0.05 |
| SBP, mm Hg | 127.9 ± 16.2 | 129.5 ± 15.9 | 127.0 ± 16.4 | < 0.01 |
| DBP, mm Hg | 83.7 ± 11.9 | 84.5 ± 12.2 | 80.5 ± 11.5 | < 0.01 |
| FPG, mmol/l | 5.60 ± 1.06 | 5.56 ± 1.05 | 5.66 ± 1.09 | < 0.01 |
| TC, mmol/l | 4.76 ± 1.11 | 4.74 ± 1.14 | 4.78 ± 1.12 | 0.02 |
| TG, mmol/l | 1.61 ± 0.55 | 1.67 ± 0.59 | 1.58 ± 0.54 | < 0.01 |
| HDL-C, mmol/l | 1.37 ± 0.38 | 1.34 ± 0.37 | 1.39 ± 0.35 | < 0.01 |
| LDL-C, mmol/l | 2.79 ± 0.81 | 2.76 ± 0.77 | 2.81 ± 0.85 | < 0.01 |
Values are expressed as mean ± SD.
p values are from t test.
DBP = Diastolic blood pressure; FPG = fasting plasma glucose; HDL-C = high density lipoprotein cholesterol; LDL-C = low density lipoprotein cholesterol; SBP = systolic blood pressure;
TC = total cholesterol; TG = triglycerides.
Table 2.
BMI distribution of the study participants by sex and agea
| Sex | BMI, kg/m2 |
||||
|---|---|---|---|---|---|
| Normal (18.5–24.9) | Overweight (25.0–29.9) | obesity class 1 (30.0–34.9) | obesity class 2 (35.0–39.9) | obesity class 3 (≥ 40.0) | |
| Totalb | 62.7 (11,915) | 24.2 (4,597) | 4.6 (872) | 2.1 (407) | 1.0 (190) |
| Men overallb | 63.2 (4,518) | 25.5 (1,823) | 4.4 (315) | 1.7 (122) | 0.8 (60) |
| 18–29 years | 66.0 (388) | 21.5 (127) | 3.9 (20) | 1.4 (7) | 0.5 (2) |
| 30–39 years | 65.3 (750) | 24.0 (289) | 4.2 (44) | 1.6 (17) | 0.8 (8) |
| 40–49 years | 61.9 (1,560) | 25.9 (667) | 5.0 (121) | 2.0 (49) | 1.2 (27) |
| 50–59 years | 61.9 (1,112) | 26.0 (483) | 4.9 (84) | 1.9 (33) | 1.0 (16) |
| 60–69 years | 65.1 (466) | 22.3 (176) | 4.7 (32) | 1.7 (11) | 0.7 (5) |
| ≥ 70 years | 64.2 (242) | 20.1 (81) | 4.1 (14) | 1.6 (5) | 0.7 (2) |
| Women overallb | 62.4 (7,397) | 23.4 (2,774)c | 4.7 (557)c | 2.4 (285)c | 1.1 (130) |
| 18–29 years | 66.9 (472) | 18.8 (133) | 4.1 (27) | 1.9 (13) | 0.6 (4) |
| 30–39 years | 63.8 (1,397) | 21.5 (471) | 4.7 (97) | 2.3 (50) | 1.0 (21) |
| 40–49 years | 60.1 (2,351) | 25.3 (991) | 5.3 (199) | 2.7 (105) | 1.3 (51) |
| 50–59 years | 61.5 (1,956) | 24.2 (770) | 5.1 (155) | 2.6 (83) | 1.2 (38) |
| 60–69 years | 65.3 (871) | 22.3 (298) | 4.6 (58) | 1.9 (25) | 0.9 (12) |
| ≥ 70 years | 65.6 (350) | 20.7 (111) | 4.2 (21) | 1.6 (9) | 0.7 (4) |
Values are expressed as percentages (n).
Age-standardized prevalence rate.
p < 0.05.
References
- 1.National Center for Cardiovascular Diseases, China: Report on Cardiovascular Diseases in China . 1st ed. Beijing: Encyclopedia of China Publication; 2008. [Google Scholar]
- 2.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss an update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 3.Li R, Lu W, Jia J, Zhang S Shi L, Li Y, et al. Relationships between indices of obesity and its cardiovascular comorbidities in a Chinese population. Circ J. 2008;72:973–978. doi: 10.1253/circj.72.973. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS, Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity. findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207:928–934. doi: 10.1016/j.jamcollsurg.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 5.Hu D, Xie J, Fu P, Zhou J, Yu D, Whelton PK, et al. Central rather than overall obesity is related to diabetes in the Chinese population The InterASIA Study. Obesity. 2007;15:2809–2816. doi: 10.1038/oby.2007.333. [DOI] [PubMed] [Google Scholar]
- 6.Hill AM, Kris-Etherton PM. Contemporary strategies for weight loss and cardiovascular disease risk factor modification. Curr Atheroscler Rep. 2008;10:486–496. doi: 10.1007/s11883-008-0076-1. [DOI] [PubMed] [Google Scholar]
- 7.Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 8.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gasroenterology. 2007;132:2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 9.Center for Statistics and Information, MOH: The Report of National Health Service Survey . 1st ed. Beijing: Publishing Company of Xiehe Medical University; 2004. [Google Scholar]
- 10.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–475. [PubMed] [Google Scholar]
- 11.Myers GL, Cooper GR, Winn CL, et al. The Centers for Disease Control – National Heart, Lung and Blood Institute Lipid Standardization Program. An approach to accurate and precise lipid measurements. Clin Lab Med. 1989;9:105–135. [PubMed] [Google Scholar]
- 12.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 13.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension. 2003;41:1178–1179. doi: 10.1161/01.HYP.0000075790.33892.AE. [DOI] [PubMed] [Google Scholar]
- 14.The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26:S5–S20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 15.Myers GL, Cooper GR, Winn CL, Smith SJ. The Centers for Disease Control – National Heart, Lung and Blood Institute Lipid Standardization Program. An approach to accurate and precise lipid measurements. Clin Lab Med. 1989;9:105–135. [PubMed] [Google Scholar]
- 16.The Cooperation Group of the Chinese Medical Association Diabetes Branch Studying on the Metabolic Syndrome Suggestion for the metabolic syndrome by the Chinese Medical Association Diabetes Branch. Chin J Diabetes. 2004;12:156–161. [Google Scholar]
- 17.Gu D, Reynolds K, Wu X, Chen J, Duan X, Reynolds RF, et al. Prevalence of the metabolic syndrome and overweight among adult in China. Lancet. 2005;365:1398–1405. doi: 10.1016/S0140-6736(05)66375-1. [DOI] [PubMed] [Google Scholar]
- 18.Yu Z, Lin X, Haas JD, Franco OH, Rennie KL, Li H, et al. Obesity related metabolic abnormalities distribution and geographic differences among middle-aged and older Chinese populations. Prev Med. 2009;48:272–278. doi: 10.1016/j.ypmed.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 19.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 20.Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS, Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity. findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207:928–934. doi: 10.1016/j.jamcollsurg.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 21.Sun Z, Zheng L, Xu C, Li J, Zhang X, Liu S, et al. Prevalence of pre-hypertension, hypertension and associated risk factors in Mongolian and Han Chinese populations in Northeast China. Int J Cardiol. 2008;128:250–254. doi: 10.1016/j.ijcard.2007.08.127. [DOI] [PubMed] [Google Scholar]
- 22.Bays HE, Chapman RH, Grandy S. The relationship of body mass index to diabetes mellitus, hypertension, and dyslipidemia: comparison of data from two national surveys. Int J Clin Pract. 2007;61:737–747. doi: 10.1111/j.1742-1241.2007.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glasser SP. Hypertension syndrome and cardiovascular events. High blood pressure is only one risk factor. Postgrad Med. 2001;110:29–36. doi: 10.1080/00325481.2001.11445493. [DOI] [PubMed] [Google Scholar]
- 24.Sun Z, Zheng L, Xu C, Zhang X, Li J, Liu S, et al. Prevalence of diabetes and impaired fasting glucose in hypertensive adults in rural China. Acta Cardiol. 2009;64:351–356. doi: 10.2143/AC.64.3.2038021. [DOI] [PubMed] [Google Scholar]
- 25.Dong Y, Gao W, Nan H, Yu H, Li F, Duan W, et al. Prevalence of type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabet Med. 2005;22:1427–1433. doi: 10.1111/j.1464-5491.2005.01658.x. [DOI] [PubMed] [Google Scholar]
- 26.Wong KC, Wang Z. Prevalence of type 2 diabetes mellitus of Chinese populations in Mainland China, Hong Kong, and Taiwan. Diabetes Res Clin Pract. 2006;73:126–134. doi: 10.1016/j.diabres.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 27.Wee CC, Hamel MB, Huang A, Davis RB, Mittleman MA, McCarthy EP. Obesity and undiagnosed diabetes in the U.S. Diabetes Care. 2008;31:1813–1815. doi: 10.2337/dc07-1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lao XQ, Thomas GN, Jiang CQ, Zhang WS, Yin P, Adab P, et al. Association of the metabolic syndrome with vascular disease in an older Chinese population Guangzhou Biobank Cohort Study. J Endocrinol Invest. 2006;29:989–996. doi: 10.1007/BF03349212. [DOI] [PubMed] [Google Scholar]