Abstract
Background:
Intraperitoneal local anesthetic is an effective analgesic approach following laparoscopic cholecystectomy.
Aims:
The aim of the present study was to compare the antinociceptive effects of intraperitoneal ropivacaine plus fentanyl with ropivacaine plus dexmedetomidine in patients undergoing laparoscopic cholecystectomy.
Settings and Designs:
This was randomized, prospective, double-blinded, observational clinical study.
Methods:
A total of 80 patients, undergoing elective laparoscopic cholecystectomy under general anesthesia were randomly assigned to one of the two equal groups to receive either of the following: Group RF (n = 40) were given 30 mL of 0.2% ropivacaine combined with 1 μg/kg fentanyl (diluted in 2 mL normal saline) and Group RD (n = 40) were given 30 mL of 0.2% ropivacaine combined with 1 μg/kg dexmedetomidine (diluted in 2 mL normal saline) through trocars. The quality of analgesia was assessed using visual analog scale score (VAS). Time to the first request of analgesia, the total dose of analgesic in the first 24 h and adverse effects were noted.
Statistical Analysis:
The data were analyzed with the Students’ t-test and Chi-square test.
Results:
VAS score at different time intervals, overall VAS in 24 h was significantly lower (1.68 ± 0.46 vs. 4.47 ± 0.94), time to first request of analgesia (min) was longest (122.7 ± 24.5 vs. 89.3 ± 13.2) and total analgesic consumption (mg) was lowest (95.3 ± 15.6 vs. 135.7 ± 75.1) in RD group than in RF group.
Conclusion:
The antinociceptive effect of the intraperitoneal instillation of ropivacaine in combination with dexmedetomidine is superior to ropivacaine combined with fentanyl.
Keywords: Dexmedetomidine, fentanyl, intraperitoneal instillation, postoperative pain, ropivacaine
INTRODUCTION
Postoperative pain management after laparoscopic surgeries remains a major challenge. Although minimally invasive, many of the patients experience moderate-to-severe pain in the early postoperative period.[1] Postoperative pain is a major obstacle for early postoperative ambulation. It increases the risk of venous thromboembolism and respiratory complications and prolongs hospital stay.[2] Inadequately treated postoperative pain may lead to chronic regional pain syndromes.[3]
Multimodal analgesia regimens such as parenteral opioids, nonsteroidal anti-inflammatory drugs or local wound infiltration with local anesthetics, have been tried to reduce overall pain and postoperative complications of patients undergoing laparoscopic surgeries.[4] Despite their efficacy, with all parenteral medications, there are associated adverse effects. In this modern era of surgery, intraperitoneal instillation of local anesthetic agents has become an important method to control postoperative pain, nausea, vomiting, and reduced hospital stay.[5,6]
Because of gas insufflation and raised intraperitoneal pressure during laparoscopic surgeries, there is peritoneal inflammation and neuronal rupture with a linear relationship between abdominal compliance and resultant severity of postoperative pain.[7] Hence, we chose the intraperitoneal route because it blocks the visceral afferent signals and modifies visceral nociception.
The local anesthetic agents provide antinociception by affecting nerve membrane-associated proteins and by inhibiting the release and action of prostaglandins which stimulates the nociceptors and cause inflammation.[8] Intraperitoneal instillation of 0.2% ropivacaine provide effective analgesia, in addition to this, we added either dexmedetomidine or fentanyl to compare the antinociceptive efficacy if mixed with ropivacaine. The antinociceptive effects of dexmedetomidine occur at dorsal root neuron level, where it blocks the release of substance P in the nociceptive pathway and through action on inhibitory G protein, which increases the conductance through potassium channels.[9]
This prospective study was conducted to evaluate the analgesic efficacy of intraperitoneal ropivacaine with fentanyl and ropivacaine with dexmedetomidine following laparoscopic cholecystectomy. The primary outcome variable was to compare pain (visual analog scale [VAS]) score. The secondary outcome included time to the first request of analgesia in the postoperative period, the total dose of analgesic used in 24 h period (postoperative) and any adverse effects.
METHODS
After the Institutional Ethics Committee approval, written informed consent was obtained from all patients, who were included in the study. Totally 80 patients, with the American Society of Anesthesiologists (ASA) physical status I and II, of both sexes, aged between 30 and 60 years, undergoing elective laparoscopic cholecystectomies under general anesthesia were randomized into two groups [Figure 1].
Figure 1.
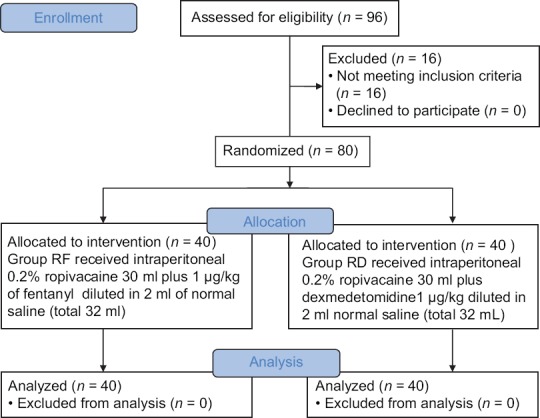
Consort diagram showing the number of patients included and analyzed
Patients with known sensitivity to local anesthetics, allergy to the study drugs, 2nd or 3rd degree heart block, renal and hepatic insufficiency, uncontrolled diabetes and hypertension, obesity (body mass index > 30/kg/m), pregnant and lactating females were excluded from the study. All patients were examined preoperatively, and all routine investigations were done. Patients were explained about the concerned technique and were instructed to keep fasting for 6 h. 10 cm visual analog scale (VAS) (0, no pain and 10, worst pain imaginable) was also explained during the preoperative visit. All patients received clonazepam tablet (0.5 mg) orally on the night before the surgery.
Eighty patients were randomly allocated to one of the two equal groups using computer-generated table of randomization. Group RF (n = 40) received intraperitoneal 0.2% ropivacaine 30 ml plus 1 μg/kg of fentanyl diluted in 2 ml of normal saline (total 32 ml), and Group RD (n = 40) received intraperitoneal 0.2% ropivacaine 30 ml plus dexmedetomidine 1 μg/kg diluted in 2 ml normal saline (total 32 ml).
On arrival to the operating room, an 18G intravenous (i. v.) catheter was inserted and 6 mL/kg/h crystalloid was infused. Noninvasive monitors, such as electrocardiography, noninvasive blood pressure, oxygen saturation (SpO2), were attached and baseline parameters such as heart rate, systemic arterial pressure, and peripheral SpO2 and level of sedation were noted down.
A conventional balanced general anesthesia was administered to all patients. Pre-oxygenation with 100% oxygen (O2) was done for 3 min. General anesthesia was induced with IV fentanyl 2 μg/kg, propofol 2 mg/kg followed by succinylcholine 2 mg/kg to facilitate orotracheal intubation. The trachea was intubated with a cuffed endotracheal tube of appropriate size. Anesthesia was maintained with O2-N2O (33%–66%), sevoflurane 0.8% MAC, and vecuronium bromide 0.1 mg/kg bolus followed by 1 mg intermittently for neuromuscular blockade. Minute ventilation was adjusted to maintain normocapnia (end-tidal carbon dioxide [EtCO2] between 34 and 38 mm Hg) and EtCO2 was monitored. Nasogastric tube of appropriate size was inserted. Patients were placed in 15°–20° reverse Trendelenberg's position with the left side tilt position. During laparoscopy, intra-abdominal pressure was maintained 12–14 mm Hg.
Study drugs were prepared by an anesthesiologist not involved in the study. Anesthesiologist who observed the patient and surgeon were unaware of the study group until the end of the study. At the end of the surgery, the study solution was given intraperitoneally before removal of the trocar in Trendelenberg's position, into the hepato-diaphragmatic space, on gall bladder bed and near and above hepatoduodenal ligament. The neuro-muscular blockade was antagonized with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg and trachea was extubated. The nasogastric tube was removed, and the patient was shifted to the postanesthesia care unit.
The degree of postoperative pain was assessed using the VAS at 30 min, 1 h, 4 h, 8 h, 12 h, 16 h, and 24 h postoperatively. Those patients who had VAS >4, were administered a bolus of diclofenac aqueous (75 mg) as rescue analgesia. Ondansetron (4 mg i. v.) was administered on the complaint of nausea and vomiting. Time to first analgesic requirement after completion of surgery, the total analgesic requirement in the first 24 h postoperatively for each patient and occurrence of adverse events in the postoperative period, was also recorded.
A total sample size of 80 patients (n = 40 each for two groups) was calculated using Power and Sample size calculator (PS version 3.0.0.34), assuming 30% improvement in pain scores with ∝ error of 0.05 and power of 80%. To obtain 80 study sample size, a total of 96 patients were included; but 16 patients were excluded on the basis of exclusion criteria. Data were checked, entered and analyzed using SPSS version 19 for Windows (IBM Corp., Armonk, NY, USA). Quantitative data were represented as mean ± standard deviation, and for qualitative data, number, and percentages were used. Students’ t-test was used as test of significance to find an association for quantitative data. Chi-square test was used as test of significance to find the association for qualitative data. P < 0.05 was considered statistically significant.
RESULTS
There was no statistically significant difference with respect to age, sex, weight, BMI, ASA physical status of the patients and the duration of surgery [Table 1]. VAS at different time intervals were statistically significantly lower at all times in RD group compared to RF group [Table 2].
Table 1.
Demographic data
| Parameter | Group RF (n=40) | Group RD (n=40) | P |
|---|---|---|---|
| Age (years) | 37.3±9.2 | 36.1±9.4 | 0.88 |
| Sex (female/male) | 12/28 | 11/29 | 0.69 |
| Weight (kg) | 61.6±6.8 | 59.8±7.1 | 0.81 |
| BMI (kg/m2) | 21.2±1.4 | 20.3±1.7 | 0.62 |
| ASA grade (I/II) | 30/10 | 28/12 | 0.74 |
| Duration of surgery (min) | 64.7±9.2 | 67.3±12.5 | 0.55 |
Data are represented as mean±SD. ASA=American Society of Anesthesiologists, BMI=Body mass index, SD=Standard deviation
Table 2.
Visual analog scale pain score
| Time (h) | Group RF (n=40) | Group RD (n=40) | P |
|---|---|---|---|
| At 0.5 | 3.27±1.40 | 2.08±0.72 | 0.001 |
| At 1 | 4.81±0.10 | 2.24±0.36 | 0.001 |
| At 4 | 4.28±1.02 | 2.03±0.70 | 0.001 |
| At 8 | 3.64±1.40 | 1.64±0.42 | 0.001 |
| At 12 | 3.22±0.80 | 2.07±0.25 | 0.001 |
| At 16 | 4.10±0.90 | 1.71±0.70 | 0.001 |
| At 24 h | 2.04±0.82 | 1.02±0.61 | 0.001 |
Data are represented as mean±SD. P<0.05 was considered statistically significant. SD=Standard deviation
Regarding the pattern of pain, it was predominantly of the generalized abdominal type of pain occurring patients from both the groups [Table 3], followed by incisional pain. One patient from RF group and one from RD group complained of perineal pain. None of the patients from both groups complained of shoulder pain.
Table 3.
Pattern of pain
| Types of pain | Group RF (n=40), n (%) | Group RD (n=40), n (%) | P |
|---|---|---|---|
| Incisional | 10 (25) | 6 (15) | 0.007 |
| Generalized abdominal | 13 (32.5) | 8 (20) | 0.001 |
| Perineal | 1 (2.5) | 1 (2.5) | 1 |
| Shoulder | 0 | 0 | 1 |
| Total | 24 (60) | 15 (37.5) | 0.002 |
Values are expressed as number of patients
Furthermore, overall VAS in 24 h was also significantly lower in the RD group (1.68 ± 0.46) compared to RF group (4.47 ± 0.94) [Table 4]. The time required for the first dose of rescue analgesia was longer in the RD group (122.7 ± 24.5 min) than in RF group (89.3 ± 13.2 min), indicating better and longer pain relief in the RD group compared to that of RF group. The difference was also statistically significant among the two groups [Table 4]. Total analgesic consumption was high in RF group than in the RD group [Table 4]. Total diclofenac consumption was also low in RD group (95.3 ± 15.6 mg) than in R group (135.7 ± 75.1 mg) [Table 4]. Incidence of nausea and vomiting was significantly lower in RD group than in RF group. There was no significant difference between both groups regarding other adverse effects [Table 5].
Table 4.
Postoperative overall vas score and analgesic requirements
| Variable | Group RF (n=40) | Group RD (n=40) | P |
|---|---|---|---|
| Over all VAS over 24 h postoperatively | 4.47±0.94 | 1.68±0.46 | 0.01 |
| Time to first request of analgesia in postoperative period (min) | 89.3±13.2 | 122.7±24.5 | 0.01 |
| Total dose of diclofenac (mg) in 24 h | 135.7±75.1 | 95.3±15.6 | 0.01 |
VAS=Visual analog scale
Table 5.
Postoperative adverse/side effects (%)
| Adverse effect | Group RF (n=40), n (%) | Group RD (n=40), n (%) | P |
|---|---|---|---|
| Nausea | 8 (20) | 3 (7.5) | 0.03 |
| Vomiting | 5 (12.5) | 1 (2.5) | 0.02 |
| Pruritus | 1 (2.5) | 0 | 0.29 |
| Sedation | 2 (5) | 0 | 0.47 |
Values are expressed as number of patients
DISCUSSION
In the present study, we noted that intraperitoneal administration of dexmedetomidine (1 μg/kg) in combination with ropivacaine 0.2%, as compared to ropivacaine 0.2% combined with fentanyl (1 μg/kg), in adult patients undergoing elective laparoscopic cholecystectomies under general anesthesia, was associated with reduced postoperative pain, increased time to first rescue analgesia, and reduced requirements for rescue diclofenac postoperatively. Dexmedetomidine offered also a shorter postoperative length of hospital stay with no significant side effects.
Joris et al., in their study observed that postoperative pain from laparoscopic cholecystectomy consists of 3 components, visceral, parietal, and referred shoulder pain. These three types of pains are distinguishing from each other in the intensity, latency, and duration.[10] Bisgaard et al., and Ure et al., suggested that parietal pain is the predominant cause of pain.[11,12] In contrast, emphasis on the visceral pain occupying greater portion of pain from laparoscopic cholecystectomy in the early convalescent period because the surgical manipulation and tissue destruction is the most in the visceral organ itself compared to the small incisions and limited trauma of the abdominal wall.
Numbers of studies have been performed on the effects of intraperitoneal instillation local anesthetics on postoperative analgesia following laparoscopic surgeries. In these studies, different local anesthetics in different volumes and concentrations have been used. Goldstein et al. reported that the IP instillation of 20 mL of either 0.5% bupivacaine or 0.75% ropivacaine reduced postoperative pain and decreased the need for postoperative analgesia, when compared with placebo in patients undergoing laparoscopic gynecologic surgery.[13] Another trail by Callesen et al. combined port site and mesosalpinx infiltration and peritoneal instillation by using 285 mg of ropivacaine (50 mL) in a double-blind, randomized, placebo-controlled study on 80 patients undergoing laparoscopic tubal sterilization.[14]
Many studies have reported dexmedetomidine and fentanyl as an adjuvant to intraperitoneal local anesthetic in laparoscopic surgeries to reduce postoperative pain, prolong the time to the first request of analgesia, and decrease the postoperative analgesic consumption. Our results are very similar to the previous studies by Rahimzadeh et al. and Kiran et al.
Saadalla and Khalifa compared dexmedetomidine and fentanyl added to intrathecal bupivacaine in orthopedic procedures in lower limbs.[15] In this study, patients received 2.5 ml hyperbaric bupivacaine 0.5% plus 5 μg dexmedetomidine (BD group), 25 μg fentanyl (BF group) or 0.5 ml normal saline (BN group), respectively. They concluded that using dexmedetomidine as an adjuvant to bupivacaine for intrathecal analgesia in lower limb surgeries has longer duration of sensory and motor block, longer postoperative analgesia with low side effects.
Kiran et al. evaluate the clinical efficacy of dexmedetomidine versus fentanyl as an additive to ropivacaine for epidural anesthesia.[16] Patients undergoing infraumbilical surgeries were divided randomly into three groups - Group R (n = 25): Received 18 ml of 0.5% ropivacaine for epidural anesthesia and 10 ml of 0.1% ropivacaine boluses for postoperative analgesia; Group RF (n = 25): Received 18 ml of 0.5% ropivacaine with 20 μg fentanyl for epidural anesthesia and 10 ml of 0.1% ropivacaine with 10 μg fentanyl boluses for postoperative analgesia; and Group RD (n = 25): Received 18 ml of 0.5% ropivacaine with 10 μg dexmedetomidine for epidural anesthesia and 10 ml of 0.1% ropivacaine with 5 μg dexmedetomidine boluses for postoperative analgesia. The investigator observed that epidural anesthesia achieved with 10 μg dexmedetomidine as an additive to 0.5% ropivacaine is more effective with respect to duration and intensity of analgesia when compared to 0.5% ropivacaine alone or addition of 20 μg fentanyl to 0.5% ropivacaine.
Our results correlate with study done by Ahmed et al. which has shown that intraperitoneal instillation of meperidine or dexmedetomidine in combination with bupivacaine 0.25% significantly decreases the postoperative analgesic requirements and decreased incidence of shoulder pain in patients undergoing laparoscopic gynecological surgeries.[17]
Limitation of the present study is the post-operative pain, which is a subjective experience and can be difficult to quantify objectively and compare when comparing various treatment options. As there are very few studies in the past on addition of dexmedetomidine and fentanyl to intraperitoneal ropivacaine, further studies with different doses of dexmedetomidine and fentanyl, timing, concentrations of local anesthetics and routes of administration are needed to provide maximal benefit in terms of post-operative pain relief with minimal adverse effects after laparoscopic surgeries.
CONCLUSION
We conclude that intraperitoneal instillation of dexmedetomidine 1 μg/kg in combination with ropivacaine 0.2% in elective laparoscopic cholecystectomy significantly reduces the post-operative pain and significantly reduces the analgesic requirement in postoperative period as compared to fentanyl 1 μg/kg in combination with ropivacaine.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bisgaard T, Kehlet H, Rosenberg J. Pain and convalescence after laparoscopic cholecystectomy. Eur J Surg. 2001;167:84–96. doi: 10.1080/110241501750070510. [DOI] [PubMed] [Google Scholar]
- 2.Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg. 2000;87:273–84. doi: 10.1046/j.1365-2168.2000.01374.x. [DOI] [PubMed] [Google Scholar]
- 3.Kehlet H. Acute pain control and accelerated postoperative surgical recovery. Surg Clin North Am. 1999;79:431–43. doi: 10.1016/s0039-6109(05)70390-x. [DOI] [PubMed] [Google Scholar]
- 4.Abdulla S, Eckhardt R, Netter U, Abdulla W. A randomized, double-blind, controlled trial on non-opioid analgesics and opioid consumption for postoperative pain relief after laparoscopic cholecystectomy. Acta Anaesthesiol Belg. 2012;63:43–50. [PubMed] [Google Scholar]
- 5.Kim TH, Kang HK, Park JS, Chang IT, Park SG. Intraperitoneal ropivacaine instillation for postoperative pain relief after laparoscopic cholecystectomy. J Korean Surg Soc. 2010;79:130–6. [Google Scholar]
- 6.Shukla U, Prabhakar T, Malhotra K, Srivastava D, Malhotra K. Intraperitoneal bupivacaine alone or with dexmedetomidine or tramadol for post-operative analgesia following laparoscopic cholecystectomy: A comparative evaluation. Indian J Anaesth. 2015;59:234–9. doi: 10.4103/0019-5049.155001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Albanese AM, Albanese EF, Miño JH, Gómez E, Gómez M, Zandomeni M, et al. Peritoneal surface area: Measurements of 40 structures covered by peritoneum: Correlation between total peritoneal surface area and the surface calculated by formulas. Surg Radiol Anat. 2009;31:369–77. doi: 10.1007/s00276-008-0456-9. [DOI] [PubMed] [Google Scholar]
- 8.Esmat ME, Elsebae MM, Nasr MM, Elsebaie SB. Combined low pressure pneumoperitoneum and intraperitoneal infusion of normal saline for reducing shoulder tip pain following laparoscopic cholecystectomy. World J Surg. 2006;30:1969–73. doi: 10.1007/s00268-005-0752-z. [DOI] [PubMed] [Google Scholar]
- 9.El-Labban GM, Hokkam EN, El-Labban MA, Morsy K, Saadl S, Heissam KS, et al. Intraincisional vs. intraperitoneal infiltration of local anaesthetic for controlling early post-laparoscopic cholecystectomy pain. J Minim Access Surg. 2011;7:173–7. doi: 10.4103/0972-9941.83508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joris J, Thiry E, Paris P, Weerts J, Lamy M. Pain after laparoscopic cholecystectomy: Characteristics and effect of intraperitoneal bupivacaine. Anesth Analg. 1995;81:379–84. doi: 10.1097/00000539-199508000-00029. [DOI] [PubMed] [Google Scholar]
- 11.Bisgaard T, Klarskov B, Kristiansen VB, Callesen T, Schulze S, Kehlet H, et al. Multi-regional local anesthetic infiltration during laparoscopic cholecystectomy in patients receiving prophylactic multi-modal analgesia: A randomized, double-blinded, placebo-controlled study. Anesth Analg. 1999;89:1017–24. doi: 10.1097/00000539-199910000-00036. [DOI] [PubMed] [Google Scholar]
- 12.Ure BM, Troidl H, Spangenberger W, Dietrich A, Lefering R, Neugebauer E, et al. Pain after laparoscopic cholecystectomy. Intensity and localization of pain and analysis of predictors in preoperative symptoms and intraoperative events. Surg Endosc. 1994;8:90–6. doi: 10.1007/BF00316616. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein A, Grimault P, Henique A, Keller M, Fortin A, Darai E, et al. Preventing postoperative pain by local anesthetic instillation after laparoscopic gynecologic surgery: A placebo-controlled comparison of bupivacaine and ropivacaine. Anesth Analg. 2000;91:403–7. doi: 10.1097/00000539-200008000-00032. [DOI] [PubMed] [Google Scholar]
- 14.Callesen T, Hjort D, Mogensen T, Schouenborg L, Nielsen D, Reventlid H, et al. Combined field block and i.p. Instillation of ropivacaine for pain management after laparoscopic sterilization. Br J Anaesth. 1999;82:586–90. doi: 10.1093/bja/82.4.586. [DOI] [PubMed] [Google Scholar]
- 15.Saadalla AE, Khalifa OY. Influence of addition of dexmedetomidine or fentanyl to bupivacaine lumber spinal subarachnoid anesthesia for inguinal hernioplasty. Anesth Essays Res. 2017;11:554–7. doi: 10.4103/aer.AER_210_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kiran S, Jinjil K, Tandon U, Kar S. Evaluation of dexmedetomidine and fentanyl as additives to ropivacaine for epidural anesthesia and postoperative analgesia. J Anaesthesiol Clin Pharmacol. 2018;34:41–5. doi: 10.4103/joacp.JOACP_205_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmed B, Elmawgoud AA, Dosa R. Antinociceptive effect of (ἀ2 adrenoceptor agonist) dexmedetomidine versus meperidine, topically, after laproscopic gynecologic surgery. J Med Sci. 2008;8:400–4. [Google Scholar]


