Abstract
The management of paraesophageal hernia (PEH) can be challenging due to the lack of consensus regarding indications and principles of operative treatment. In addition, data about the pathophysiology of the hernias are scant. Therefore, the goal of this review is to shed light and describe the classification, pathophysiology, clinical presentation, and indications for treatment of PEHs, and provide an overview of the surgical management and a description of the technical principles of the repair.
Keywords: : paraesophageal hernias, laparoscopic approach, esophageal function testing
Introduction
A paraesophageal hernia (PEH) occurs when part of the gastric fundus herniates through the esophageal hiatus of the diaphragm and lies alongside the esophagus. PEHs represent less than 10% of all hiatal hernias and are more common in the elderly.1,2 Today, there are still some controversies about the indication for surgery and principles of operative treatment. In addition, data about the pathophysiology of the hernias are scant. Therefore, the goal of this review is to shed light and describe the classification, pathophysiology, clinical presentation, and indications for treatment of PEHs, and provide an overview of the surgical management and a description of the technical principles of the repair. This review is qualitative and selective in the studies included.3
Materials and Methods
A literature search was performed on Medline and PubMed databases for articles published between 1996 and 2016 using the following keywords: hiatal hernia, paraesophageal hernia, gastroesophageal reflux disease, GERD, heartburn, regurgitation, dysphagia, manometry, pH monitoring, fundoplication, sac excision, and mesh. The searches were restricted to English language articles. A manual cross-reference search of the bibliographies of included articles was carried out to identify additional relevant studies. Case reports, editorials, and pediatric studies were excluded. We finally selected 85 significant articles.
Current Classification
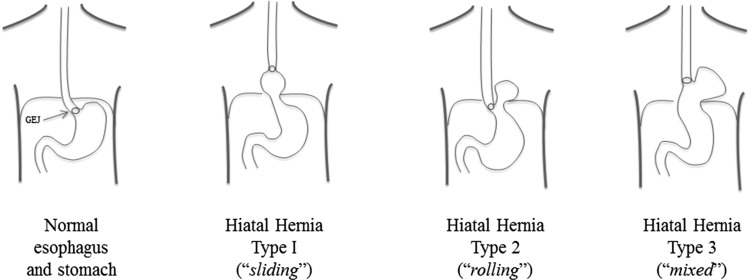
PEH is a subclass of hiatal hernia (type II and III), usually defined as a herniation of organ into the chest through the esophageal diaphragmatic hiatus. It always contains part of the stomach and rarely other abdominal viscera. Hiatal hernias can be classified in four types (Fig. 1) by the position of the gastroesophageal junction relative to the diaphragm: type I, commonly known as a sliding hiatal hernia, is the most common (95%) and occurs when the gastroesophageal junction is displaced superiorly into the thoracic cavity; type II, also called “rolling” PEH, occurs when the stomach migrates into the chest and “rolls” over the esophagus with the gastroesophageal junction still laying down into the abdomen; type III occurs when the stomach migrates into the chest and “rolls” over the esophagus with a concomitant migration of the gastroesophageal junction into the chest (this type of hernia or “mixed,” or “true paraesophageal” is a combination of the “sliding” and “rolling” types); type IV occurs when, together with the stomach, there is herniation of other intra-abdominal contents through the hiatus (e.g., small bowel, colon, duodenum, or pancreas).4–10
FIG. 1.
Classification of hiatal hernias is shown. “True” paraesophageal hernias are of type III. Note the location of the GEJ in the different types of hernias. GEJ, gastroesophageal junction.
This classification helps to understand the symptoms experienced by patients. Usually a type I hiatal hernia presents typical symptoms of gastroesophageal reflux disease (GERD), such as heartburn and regurgitation.11 As the gastroesophageal junction is displaced into the chest, the lower esophageal sphincter (LES) is subjected to the negative pressure of the thoracic cavity and becomes incompetent; at the same time, the pinchcock action of the “external sphincter” of the diaphragm is lost. The role of the angle of His is also missing as the hernia becomes compartmentalized in the chest. Rather than typical symptoms of GERD, patients with a type II hernia can experience dysphagia due to external compression of the PEH. Patients with type III and IV hernias, in general, complain of a combination of symptoms of GERD and dysphagia.12,13
Pathophysiology of Hiatal Hernias
As the pathogenesis of hiatal hernia is not completely understood, many theories are still widely debated. As described by Weber et al., there appear to be three dominant beliefs underlying the pathogenesis of hiatal hernias: (1) increased intra-abdominal pressure that displaces the gastroesophageal junction upward into the thorax; (2) esophageal shortening from congenital causes or acquired secondary to fibrosis; and (3) widening of the hiatus from congenital or acquired molecular and cellular changes in the crural muscles or in the connective tissue of the diaphragm.14 Some authors also suggest a possible role of defective collagen formation, as an increased incidence of other abdominal hernias was found in patients with type II hiatal hernia.15–18 Furthermore, obesity is also a risk factor for recurrence after surgical repair.19–22
Clinical Presentation
PEH in many patients can be asymptomatic but, when symptoms are present, its presentation differs from type I hiatal hernias. While sliding hiatal hernias are associated with an incompetent LES leading to worsening gastroesophageal reflux,23 PEHs traditionally do not affect the competency of the LES. In contrast, PEHs involve an anteriorly herniated fundus, predisposing it to twist on itself. Thus, symptoms due to PEHs are predominantly mechanical, including gastric obstruction, strangulation, incarceration, and ulceration.8,24,25 Pulmonary symptoms either from chronic aspiration due to gastric obstruction or from the thoracic displacement secondary to the herniation can also be observed.26 Chronic venous congestion of the herniated gastric mucosa along with ulceration (Cameron's ulcers) can also result in occult bleeding leading to iron deficiency anemia.13,27,28,82 Typically this anemia resolves in more than 90% of patients following the hernia repair.29,30 Type III PEHs are essentially a combination of types I and II, and their symptomology is a combination of reflux and mechanical symptoms. Type IV PEHs present similar to other hiatal hernias, although their symptomology will also depend on the abdominal contents herniated through the hiatus.12,13
Diagnostic Testing
Although most patients with PEHs are symptomatic, there is still a significant group of patients who are diagnosed incidentally, during tests performed for other conditions.
The evaluation of these patients usually includes a complete history and physical examination. Standard workup typically begins with a barium swallow, followed by upper endoscopy and esophageal manometry.31
Barium swallow is probably the best diagnostic study, giving information about the size of the stomach herniated and the location of the gastroesophageal junction.32,33 Some authors prefer a computed tomography scan of the chest and the abdomen because it may provide additional information on the type and location of the hernia.13
Upper endoscopy is useful for visualization of the esophageal and gastric mucosa, as it can detect the presence of Barrett's esophagus, erosive esophagitis, and Cameron's ulcers. Furthermore, it can also determine if there are any lesions suspicious for malignancy, which needs to be documented before surgical management.
Since all patients require a fundoplication in addition to a hernia repair, an esophageal manometry should be included in diagnostic approach for surgical planning to exclude achalasia or other esophageal motility disorders, which would contraindicate a total fundoplication.34–38 In cases when the patient cannot tolerate the manometry catheter, or if they present emergently, the surgical repair should not be postponed and a partial fundoplication is preferred to avoid postoperative dysphagia.39
Even if ambulatory 24-hour pH monitoring may provide a quantitative analysis of reflux episodes, correlating them with patient's symptoms, it is not usually required in patients with PEHs. Although many patients may have GERD, pH testing would not alter the planned operation.40,41
Indications for Surgery
The indications for surgical treatment are still debated.31 Gastric volvulus is an absolute indication for emergent surgical intervention and is classically described by the Borchardt triad, which includes the inability to pass a nasogastric tube, retching without actual food regurgitation, and chest or epigastric pain.52,53 Due to the risks of complications and the perioperative mortality of emergent surgeries, traditionally most surgeons opted to repair PEHs regardless of whether the patient was symptomatic or not.42 Afterward, the strategies moved away from this attitude to a more conservative one because some studies showed that elective and emergent hernia repairs were equally effective.2,43–45 Furthermore, there has been a growing appreciation that repair of large type III hernias could be a difficult operation, associated with high rate of recurrence and complications, particularly in patients with a short esophagus, where its extensive mobilization can lead to an iatrogenic vagotomy.54,55 Hence, for elderly patients who were minimally symptomatic and in whom the hernia was discovered incidentally, a “watchful waiting” strategy could be a reasonable alternative.2,44,45 The only symptoms considered for elective repair would include severe regurgitation, aspiration, cough, anemia, or dysphagia. However, recent literature suggests that symptoms associated with PEH are much broader and subtly been present for longer than previously thought and truly asymptomatic patients are rare. Carrott et al. found that symptoms are wide ranging and patients with PEHs are often labeled as asymptomatic or minimally symptomatic because the hernia has been present for years in an older patient, and the gradual alterations in eating and postprandial symptoms had been attributed to aging. In addition, symptoms such as dysphagia, early satiety, and postprandial dyspnea are often insidious and increase over the course of years.80 While gastrointestinal symptoms of PEH are the main focus of the indications for repair, pulmonary symptoms still remain underappreciated. In fact, many PEH repair series in the literature do not assess patients for dyspnea, likely because in elderly population dyspnea is often assumed to arise from other comorbidities.81 On the other hand, patients who are younger (<50 years old) and healthier may be more likely to encounter complications from their hernia given their life expectancy. Considering that the capability to perform the operation laparoscopically has provided further impetus to surgeons favoring the surgical approach,37,46–51 for all these patients, elective repair may be a more appropriate solution, provided that a comprehensive review of the risks, benefits, and alternatives available is thoroughly discussed with the patients as well as incidence of recurrence, complications, and expected quality of life.56
Overview of Surgical Management
PEH repair generally includes four steps: hernia sac dissection and resection, esophageal mobilization, crural repair, and fundoplication.57–59 Traditionally, these steps have been accomplished using an open transthoracic approach, which included a left thoracotomy, direct visualization of the hernia, mobilization of the esophagus to the aortic arch, and dissection and resection of the hernia sac. The main advantage of the transthoracic approach is the direct visualization and accessibility of the esophagus, which is essential in this procedure. Proper mobilization of the esophagus is highly correlated to the success rate of the procedure (recurrence rates are low after open repairs), as it ensures a tension-free repair.48,49
The advent of laparoscopy has introduced an alternative to open procedures, provided that the essential steps of the procedure can be adequately accomplished. As described by many authors, the recurrence rate with laparoscopic approach is somewhat higher, but the repair can be equally effective with significant reduction in morbidity and mortality in experienced hands.60–62 Recurrences, in fact, are usually small and asymptomatic and are mostly linked to the presence of short esophagus and tension at the diaphragmatic crura during their closure.63
Techniques to overcome the presence of axial tension due to the presence of short esophagus include aggressively mobilizing the esophagus and an extensive dissection of the hernia sac in the posterior mediastinum.55 An esophageal lengthening procedure, such as a Collis gastroplasty, can be used to further reduce this tension and decrease the risk of recurrence.63 This procedure consists in stapling vertically and laterally alongside the esophagus onto the angle of His, thus effectively creating a “neoesophagus.” This procedure lengthens the esophagus inferior to the diaphragm and allows for a more successful fundoplication without tension.
Techniques to avoid tension due to a large hiatus include relaxation of the diaphragmatic crura, along with the use of mesh. The goal of mesh repair is to oppose the radial tension by strengthening the hiatal orifice. While many surgeons use mesh, this issue continues to be debated, as many have shown that if improperly positioned, the mesh can cause severe complications, such as erosions requiring gastric resection. As of today, there is no clear accepted use of mesh and, when preferred, absorbable mesh is the most commonly adopted.64–67 As described by Huddy et al. in a meta-analysis and European survey, both biological and synthetic mesh reduce the rate of recurrence, but there is still no evidence regarding the optimum technique if risks and benefits are considered.68 Another review from Tam et al. shows no evidence supporting the use of mesh.69 Finally, a randomized controlled trial from Watson et al. demonstrated similar outcomes between suture and mesh repair.70 In general, mesh is placed to buttress the hiatus after closure in those patients with thin crura, unable to withstand the tension of the primary closure.
The need for antireflux surgery in addition to PEH repair has also been debated. However, most surgeons prefer to perform a total fundoplication as this corrects gastroesophageal reflux if present preoperatively. It also prevents the development of reflux due to the extensive dissection and destruction of some of the continence mechanisms of the gastroesophageal junction; and it is a very good form of gastropexy, anchoring the stomach below the diaphragm, thereby reducing recurrences.71 A fundoplication reduces the need for a tube gastrostomy, which is seldom performed in the modern era. Accordingly, a randomized controlled pilot study from Muller-Stich et al. confirmed that a laparoscopic repair of PEHs should be combined with a fundoplication to avoid postoperative reflux.72
Although a Nissen fundoplication is the procedure of choice, a partial posterior (Toupet) or anterior (Dor) fundoplication may be considered when a patient presents with signs and symptoms of incarceration or strangulation and when an underlying esophageal motility disorder is present, which would reduce the risk of postoperative dysphagia.73,74
The connection between obesity, hiatal hernia, and GERD is well established. In 1999, Wilson et al. found that individuals with a body mass index (BMI) exceeding 30 kg/m2 were 4.2 times more likely to have hiatal hernia than those with a BMI lower than 25 kg/m2.83 Hiatal hernia also has been found in up to 40% of patients who underwent preoperative esophago-gastro-duodenoscopy for bariatric surgery.84 As described above, several studies have shown that laparoscopic PEH repair is safe and feasible and provides short and long-term resolution of symptoms.79 However, a recent 10-year retrospective review of laparoscopic hiatal hernia repair in giant PEH identified obesity as a risk factor for long-term adverse outcomes.78 In the nonobese population, therefore, surgical options are readily considered for definitive treatment of PEH. However, concomitant obesity complicates this decision, as obesity has also been shown to increase the failure rate of antireflux surgery.85 Because of the increased risk of surgical failure in this challenging population, a sleeve gastrectomy or gastric bypass should be considered along with PEH repair.75–77 During the last few years, there has been an increased acceptance of bariatric surgery, however, there are still several obstacles, such as patient preference and lack of insurance coverage. Many patients with severe reflux or hiatal hernia do not meet Medicare requirements for bariatric surgery (BMI >40 kg/m2, alone, or 35–40 kg/m2, with significant comorbidities). Other patients may meet these requirements, but may prefer not to undergo gastric bypass or are unable to comply with postoperative lifestyle modifications.
Conclusions
Based on the studies we reviewed, we conclude that (1) patients younger than 50, even if asymptomatic, and older patients with symptoms such as regurgitation, aspiration, cough, anemia, or dysphagia should be considered for surgery; (2) the gold standard of repair in most cases remains laparoscopic surgery, which has been demonstrated to provide excellent patient satisfaction, symptom improvement, and a recurrence rate comparable to open surgery; (3) the use of mesh must be selectively reserved to patients in which the crura is unable to tolerate the tension of a primary closure; and (4) in patients with a BMI greater than 35 kg/m2, bariatric surgery should be considered.
Acknowledgment
No funding was obtained for this work.
Disclosure Statement
No competing financial interests exist.
References
- 1.Poncet G, Robert M, Roman S, et al. Laparoscopic repair of large hiatal hernia without prosthetic reinforcement: Late results and relevance of anterior gastropexy. J Gastrointest Surg 2010;14:1910–1916 [DOI] [PubMed] [Google Scholar]
- 2.Dahlberg PS, Deschamps C, Miller DC, et al. Laparoscopic repair of large paraesophageal hernia. Ann Thorac Surg 2001;72:1125–1129 [DOI] [PubMed] [Google Scholar]
- 3.Eva KW. On the limits of systematicity. Med Educ 2008;42:852–853 [DOI] [PubMed] [Google Scholar]
- 4.Hashemi M, Peters JH, DeMeester TR, et al. Laparoscopic repair of large type III hiatal hernia: Objective followup reveals high recurrence rate. J Am Coll Surg 2000;190:553–560; discussion 560–561. [DOI] [PubMed] [Google Scholar]
- 5.Lal D. Laparoscopic repair of paraoesophageal hernia. Surg Clin North Am 2005;85:105–118 [DOI] [PubMed] [Google Scholar]
- 6.Landrenau RJ, Del Pino M, Santos R. Management of paraesophageal hernias. Surg Clin North Am 2005;85:411–432 [DOI] [PubMed] [Google Scholar]
- 7.Scheidler MG, Keenan RJ, Maley RH, Wiechmann RJ, Fowler D, Landrenau RJ. “True” parahiatal hernia: A rare entity radiologic presentation and clinical management. Ann Thorac Surg 2002;73:416–419 [DOI] [PubMed] [Google Scholar]
- 8.Maziak DE, Todd TR, Pearson FG. Massive hiatus hernia: Evaluation and surgical management. J Thorac Cardiovasc Surg 1998;115:53–60; discussion 1–2. [DOI] [PubMed] [Google Scholar]
- 9.Altorki NK, Yankelevitz D, Skinner DB. Massive hiatal hernias: The anatomical basis of repair. J Thorac Cardiovasc Surg 1998;115:828–835 [DOI] [PubMed] [Google Scholar]
- 10.Luketich JD, Raja S, Fernando HC, et al. Laparoscopic repair of giant paraesophageal hernia: 100 consecutive cases. Ann Surg 2000;232:608–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kahrilas PJ. The role of hiatus hernia in GERD. Yale J Biol Med 1999;72:101–111 [PMC free article] [PubMed] [Google Scholar]
- 12.Mattioli S, D'Ovidio F, Di Simone MP, et al. Clinical and surgical relevance of the progressive phases of intrathoracic migration of the gastroesophageal reflux disease. J Thorac Cardiovasc Surg 1998;116:267–275 [DOI] [PubMed] [Google Scholar]
- 13.Schieman C, Grondin SC. Paraesophageal hernia: Clinical presentation, evaluation, and management controversies. Thorac Surg Clin 2009;19:473–484 [DOI] [PubMed] [Google Scholar]
- 14.Weber C, Davis CS, Shankaran V, Fisichella PM. Hiatal hernias: A review of the pathophysiologic theories and implication for research. Surg Endosc 2011;25:3149–3153 [DOI] [PubMed] [Google Scholar]
- 15.Rosch R, Klinge U, Si Z, Junge K, Klosterhalfen B, Schumpelick V. A role for collagen I/III and MMP-1/13 genes in primary inguinal hernia? BMC Med Genet 2002;3:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Si Z, Bhardwaj R, Rosch R, Mertens PR, Klosterhalfen B, Klinge U. Impaired balance of type I and type III procollagen mRNA in cultured fibroblasts of patients with incisional hernia. Surgery 2002;131:324–331 [DOI] [PubMed] [Google Scholar]
- 17.Klinge U, Si ZY, Zheng H, Schumpelick V, Bhardwaj RS, Klosterhalfen B. Collagen I/III and matrix metalloproteinases (MMP) 1 and 13 in the fascia of patients with incisional hernias. J Invest Surg 2001;13:47–54 [DOI] [PubMed] [Google Scholar]
- 18.Zheng H, Si Z, Kasperk R, et al. Recurrent inguinal hernia: Disease of collagen matrix? World J Surg 2002;26:401–408 [DOI] [PubMed] [Google Scholar]
- 19.Herbella FA, Sweet MP, Tedesco P, Nipomnick I, Patti MG. Gastroesophageal reflux disease and obesity. Pathophysiology and implications for treatment. J Gastrointest Surg 2007;11:286–290 [DOI] [PubMed] [Google Scholar]
- 20.Nadaleto BF, Herbella FA, Patti MG. Gastroesophageal reflux disease in the obese: Pathophysiology and treatment. Surgery 2016;159:475–486 [DOI] [PubMed] [Google Scholar]
- 21.Perez AR, Moncure AC, Rattner DW. Obesity adversely affects the outcome of antireflux operations. Surg Endosc 2001;15:986–989 [DOI] [PubMed] [Google Scholar]
- 22.Akimoto S, Nandipati KC, Kapoor H, Yamamoto SR, Pallati PK, Mittal SK. Association of body mass index (BMI) with patterns of fundoplication failure: Insights gained. J Gastrointest Surg 2015;19:1943–1948 [DOI] [PubMed] [Google Scholar]
- 23.Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW. Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury. Am J Surg 1996;171:182–186 [DOI] [PubMed] [Google Scholar]
- 24.Wo JM, Branum GD, Hunter JG, et al. Clinical features of type III (mixed) paraesophageal hernia. Am J Gastroenterol 1996;91:914–916 [PubMed] [Google Scholar]
- 25.Velanovich V, Karmy-Jones R. Surgical management of paraesophageal hernia: Outcome and quality of life analysis. Dig Surg 2001;18:432–437 [DOI] [PubMed] [Google Scholar]
- 26.Low DE, Simchuck EJ. Effect of paraesophageal hernia repair on pulmonary function. Ann Thorac Surg 2002;74:333–337; discussion 7. [DOI] [PubMed] [Google Scholar]
- 27.Weston AP. Hiatal hernia with Cameron ulcers and erosions. Gastrointest Endosc Clin N Am 1996;6:671–679 [PubMed] [Google Scholar]
- 28.Maganty K, Smith RL. Cameron lesions: Unusual cause of gastrointestinal bleeding and anemia. Digestion 2008;77:214–217 [DOI] [PubMed] [Google Scholar]
- 29.Pauwelyn KA, Verhamme M. Large hiatal hernia and iron deficiency anaemia: Clinico-endoscopical findings. Acta Clin Belg 2005;60:166–172 [DOI] [PubMed] [Google Scholar]
- 30.Hayden JD, Jamieson GG. Effect on iron deficiency anemia of laparoscopic repair of large paraesophageal hernias. Dis Esophagus 2005;18:329–331 [DOI] [PubMed] [Google Scholar]
- 31.Bonrath EM, Grantcharov TP. Contemporary management of paraesophaegeal hernias: Establishing a European expert consensus. Surg Endosc 2015;29:2180–2195 [DOI] [PubMed] [Google Scholar]
- 32.Linke GR, Borovicka J, Schneider P, et al. Is a barium swallow complementary to endoscopy essential in the preoperative assessment of laparoscopic antireflux and hiatal hernia surgery? Surg Endosc 2008;22:96–100 [DOI] [PubMed] [Google Scholar]
- 33.Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol 2008;22:601–616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bello B, Zoccali M, Gullo R, et al. Gastroesophageal reflux disease and antireflux surgery—what is the proper preoperative work-up? J Gastrointest Surg 2013;17:14–20 [DOI] [PubMed] [Google Scholar]
- 35.Fisichella PM, Patti MG. GERD procedures: When and what? J Gastrointest Surg 2014;18:2047–2053 [DOI] [PubMed] [Google Scholar]
- 36.Patti MG, Gasper WJ, Fisichella PM, Nipomnick I, Palazzo F. Gastroesophageal reflux disease and connective tissue disorders: Pathophysiology and implications for treatment. J Gastrointest Surg 2008;12:1900–1906 [DOI] [PubMed] [Google Scholar]
- 37.Gantert WA, Patti MG, Arcerito M, et al. Laparoscopic repair of paraesophageal hiatal hernias. J Am Coll Surg 1998;186:428–432; discussion 432–433. [DOI] [PubMed] [Google Scholar]
- 38.Swanstrom LL, Jobe BA, Kinzie LR, et al. Esophageal motility and outcomes following laparoscopic paraesophageal hernia repair and fundoplication. Am J Surg 1999;177:359–363 [DOI] [PubMed] [Google Scholar]
- 39.Bawahab M, Mitchell P, Church N, et al. Management of acute paraesophageal hernia. Surg Endosc 2009;23:255–259 [DOI] [PubMed] [Google Scholar]
- 40.Wolf PS, Oelschlager BK. Laparoscopic paraesophageal hernia repair. Adv Surg 2007;41:199–210 [DOI] [PubMed] [Google Scholar]
- 41.Fuller CB, Hagen JA, DeMeester TR, Peters JH, Ritter M, Bremmer CG. The role of fundoplication in the treatment of type II paraesophageal hernia. J Thorac Cardiovasc Surg 1996;111:655–661 [DOI] [PubMed] [Google Scholar]
- 42.Lebenthal A, Waterford SD, Fisichella PM. Treatment and controversies in paraesophageal hernia repair. Front Surg 2015;2:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal hernias: Operation or observation? Ann Surg 2002;236:492–500; discussion 500–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Horgan S, Eubanks TR, Jacobsen G, et al. Repair of paraesophageal hernias. Am J Surg 1999;177:354–358 [DOI] [PubMed] [Google Scholar]
- 45.Floch NR. Paraesophageal hernias: Current concepts. J Clin Gastroenterol 1999;29:6–7 [DOI] [PubMed] [Google Scholar]
- 46.Wiechmanm RJ, Ferguson MK, Naunheim KS, et al. Laparoscopic management of giant paraesophageal herniation. Ann Thorac Surg 2001;71:1080–1087 [DOI] [PubMed] [Google Scholar]
- 47.Hawasli A, Zonca S. Laparoscopic repair of paraesophageal hiatal hernia. Am Surg 1998;64:703–710 [PubMed] [Google Scholar]
- 48.Fullum TM, Oyetunji TA, Ortega G, et al. Open versus laparoscopic hiatal hernia repair. JSLS 2013;17:23–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zehetner J, Demeester SR, Ayazi S, et al. Laparoscopic versus open repair of paraesophageal hernia: The second decade. J Am Coll Surg 2011;212:813–820 [DOI] [PubMed] [Google Scholar]
- 50.Hashemi M, Sillin LF, Peters JH. Current concepts in the management of paraesophageal hiatal hernia. J Clin Gasroenterol 1999;187:227–230 [DOI] [PubMed] [Google Scholar]
- 51.Oddsdottir M. Paraesophageal hernia. Surg Clin North Am 2000;80:1243–1252 [DOI] [PubMed] [Google Scholar]
- 52.Perdikis G, Hinder RA, Filipi CJ, et al. Laparoscopic paraesophageal hernia repair. Arch Surg 1997;132:586–589; discussion 590–591. [DOI] [PubMed] [Google Scholar]
- 53.El Khoury R, Ramirez M, Hungness ES, et al. Symptom relief after laparoscopic paraesophageal hernia repair without mesh. J Gastrointest Surg 2015;19:1938–1942 [DOI] [PubMed] [Google Scholar]
- 54.Oelschlager BK, Yamamoto K, Woltman T, et al. Vagotomy during hiatal hernia repair: A benign esophageal lengthening procedure. J Gastrointest Surg 2008;12:1155–1162 [DOI] [PubMed] [Google Scholar]
- 55.Horvath KD, Swanstrom LL, Jobe BA. The short esophagus: Pathophysiology, incidence, presentation, and treatment in the era of laparoscopic antireflux surgery. Ann Surg 2000;232:630–640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Duranceau A. Massive hiatal hernia: A review. Dis Esophagus 2015. [Epub ahead of print]; DOI: 10.111/dote.12328 [DOI] [PubMed]
- 57.Fisichella PM. A synopsis of techniques for paraesophageal hernia repair: Different approaches to current controversies. Surg Laparosc Endosc Percutan Tech 2013;23:423–424 [DOI] [PubMed] [Google Scholar]
- 58.Fisichella PM, Patti MG. Laparoscopic repair of paraesophageal hiatal hernias. J Laparoendosc Adv Surg Tech A 2008;18:629–632 [DOI] [PubMed] [Google Scholar]
- 59.Patti MG, Fisichella PM. Laparoscopic paraesophageal hernia repair. How I do it. J Gastrointest Surg 2009;13:1728–1732 [DOI] [PubMed] [Google Scholar]
- 60.Dallemagne B, Kohnen L, Perretta S, et al. Laparoscopic repair of paraesophageal hernia. Long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann Surg 2011;253:291–296 [DOI] [PubMed] [Google Scholar]
- 61.Willekes CL, Edoga JK, Frezza EE. Laparoscopic repair of paraesophageal hernia. Ann Surg 1997;225:31–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Latzko M, Borao F, Squillaro A, et al. Laparoscopic repair of paraesophageal hernias. JSLS 2014;18:e2014.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Swanstrom LL, Marcus DR, Galloway GQ. Laparoscopic Collis gastroplasty is the treatment of choice for the shortened esophagus. Am J Surg 1996;171:477–481 [DOI] [PubMed] [Google Scholar]
- 64.Pfluke JM, Parker M, Bowers SP, et al. Use of mesh for hiatal hernia repair: A survey of SAGES members. Surg Endosc 2012;26:1843–1848 [DOI] [PubMed] [Google Scholar]
- 65.Priego P, Perez de Oteyza J, Galindo J, et al. Long-term results and complications related to Crurasoft mesh repair for paraesophageal hiatal hernias. Hernia 2016. [Epub ahead of print]. DOI: 10.1007/s10029-016-1486-6 [DOI] [PubMed]
- 66.Oelschlager BK, Pellegrini CA, Hunter JG, et al. Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: Long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 2011;213:461–468 [DOI] [PubMed] [Google Scholar]
- 67.Jones R, Simorov A, Lomelin D, et al. Long-term outcomes of radiologic recurrence after paraesophageal hernia repair with mesh. Surg Endosc 2015;29:425–430 [DOI] [PubMed] [Google Scholar]
- 68.Huddy JR, Markar SR, Ni MZ, et al. Laparoscopic repair of hiatus hernia: Does mesh type influence outcome? A meta-analysis and European survey study. Surg Endosc 2016. [Epub ahead of print]. DOI: 10.1007/s00464-016-4900-3 [DOI] [PubMed]
- 69.Tam V, Winger DG, Nason KS. A systematic review and meta-analysis of mesh vs suture cruroplasty in laparoscopic large hiatal hernia repair. Am J Surg 2016;211:226–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Watson DI, Thompson SK, Devitt PG, et al. Laparoscopic repair of very large hiatus hernia with sutures versus absorbable mesh versus nonabsorbable mesh: A randomized controlled trial. Ann Surg 2015;261:282–289 [DOI] [PubMed] [Google Scholar]
- 71.Casabella F, Sinanan M, Horgan S, et al. Systematic use of gastric fundoplication in laparoscopic repair of paraesophageal hernias. Am J Surg 1996;171:485–489 [DOI] [PubMed] [Google Scholar]
- 72.Muller-Stich BP, Achtstatter V, Diener MK, et al. Repair of paraesophageal hiatal hernias-is a fundoplication needed? A randomized controlled pilot trial. J Am Coll Surg 2015;221:602–610 [DOI] [PubMed] [Google Scholar]
- 73.Fisichella PM, Patti MG. GERD procedures: When and what? J Gastrointest Surg 2014;18:2047–2053 [DOI] [PubMed] [Google Scholar]
- 74.Patti MG, Gasper WJ, Fisichella PM, Nipomnick I, Palazzo F. Gastroesophageal reflux disease and connective tissue disorders: Pathophysiology and implications for treatment. J Gastrointest Surg 2008;12:1900–1906 [DOI] [PubMed] [Google Scholar]
- 75.Merchant AM, Cook MW, Srinivasan J, et al. Comparison between laparoscopic paraesophageal hernia repair with sleeve gastrectomy and paraesophageal hernia repair alone in morbidly obese patients. Am Surg 2009;75:620–625 [PubMed] [Google Scholar]
- 76.Davis M, Rodriguez J, El-Hayek K, et al. Paraesophageal hernia repair with partial longitudinal gastrectomy in obese patients. JSLS 2015;19:e2015.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Patel AD, Lin E, Lytle NW, et al. Combining laparoscopic giant paraesophageal hernia repair with sleeve gastrectomy in obese patients. Surg Endosc 2015;29:1115–1122 [DOI] [PubMed] [Google Scholar]
- 78.Luketich JD, Nason KS, Christie NA, et al. Outcomes after a decade of laparoscopic giant paraesophageal hernia repair. J Thorac Cardiovasc Surg 2010;139:395–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Le Page PA, Furtado R, Hayward M, et al. Durability of giant hiatus hernia repair in 455 patients over 20 years. Ann R Coll Surg Engl 2015;97:188–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Carrott PW, Hong J, Kuppusamy M, Koehler RP, Low DE. Clinical ramifications of giant paraesophageal hernias are underappreciated making the case for routine surgical repair. Ann Thorac Surg 2012;94:421–426 [DOI] [PubMed] [Google Scholar]
- 81.Carrott PW, Hong J, Kuppusamy M, Kirtland S, Koehler RP, Low DE. Repair of giant paraesophageal hernias routinely produces improvement in respiratory function. J Thorac Cardiovasc Surg 2012;143:398–404 [DOI] [PubMed] [Google Scholar]
- 82.Haurani C, Carlin AM, Hammoud ZT, Velanovich V. Prevalence and resolution of anemia with paraesophageal hernia repair. J Gastrointest Surg 2012;16:1817–1820 [DOI] [PubMed] [Google Scholar]
- 83.Wilson LJ, Ma W, Hirschowitz BI. Association of obesity with hiatal hernia and esophagitis. Am J Gastroenterol 1999;94:2840–2844 [DOI] [PubMed] [Google Scholar]
- 84.Sharaf RN, Weinshel EH, Bini EJ, Rosenberg J, Sherman A, Ren CJ. Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg 2004;14:1367–1372 [DOI] [PubMed] [Google Scholar]
- 85.Anvari M, Allen C, Marshall J, et al. Randomized controlled trial of laparoscopic Nissen fundoplication versus proton pump inhibitors for treatment of patients with chronic gastroesophageal reflux disease: One-year follow-up. Surg Innov 2006;13:238–249 [DOI] [PubMed] [Google Scholar]