Abstract
Patients suffering from borderline personality disorder (BPD) are at elevated risk for suicidal thoughts and behaviors (STBs), but this well-described and clinically important association is not well-understood. Prior research suggests that STBs often function as an attempt to escape aversive affect, and that people with BPD experience stronger emotion reactivity and greater discomfort with emotion than those without BPD. Here, we tested whether negative affective states are more likely to predict suicidal thoughts among those with BPD than those without this disorder. Data on affective states and suicidal thoughts were collected several times per day from 35 psychiatric inpatients using their smartphones to capture real-time associations between negative affect and suicidal thoughts. Results revealed that the association between negative affective states (e.g., abandonment, desperation, guilt, hopelessness, loneliness, rage, self-hatred, and upset), and severity of suicidal thinking was stronger among those with BPD than among those without BPD. This finding has implications for risk assessment and intervention in the clinical setting: for a given degree of reported negative affect, patients with BPD experience more suicidal ideation than those without. Further research needs to be done to elucidate the mechanism of this effect.
Keywords: Negative affect, BPD, Suicidal thinking
Borderline Personality Disorder (BPD) is a serious mental illness that is characterized by emotional instability and impulsiveness. Patients who suffer from BPD are more likely to engage in suicidal thoughts and behaviors (STBs). Indeed, 75% of patients with BPD will attempt suicide at least once, and 8–10% will die by suicide (Leichsenring et al., 2011; Oldham, 2006). However, it remains unclear what causes BPD to be so strongly associated with STBs. Prior research has suggested that people with STBs report higher emotion reactivity (i.e., intense aversive arousal in response to stressors) than those without STBs, and that the primary reason by suicide attempts for attempting to end their lives is to escape from such seemingly intolerable psychological states (Boergers et al., 1998; Nock et al., 2008; Woodberry et al., 2008). Another line of research has shown that people with symptoms of BPD report significant greater discomfort with the experience of emotion than do those without symptoms of BPD (Rasmussen et al., 2016). Taken together, it is possible that the experience of negative affective states might be more likely to lead to STBs among people diagnosed with BPD than among those without such a diagnosis. As an initial test of this hypothesis, here we tested whether negative affect is more strongly associated with suicidal thoughts among patients diagnosed with BPD than it is among those without BPD.
Prior research on affect and risk for suicidal ideation among individuals with BPD has largely relied on retrospective recall of emotion. Studies that depend on patients’ memory of their past emotions are highly susceptible to recall and recency biases. These concerns can be addressed with the use of ecological momentary assessment (EMA), a method that uses repeated samplings of data on affect and other states in real time in the natural environment, thereby limiting the effects of these biases (Kleiman and Nock, 2018; Shiffman et al., 2008). EMA can capture data at the resolution of hours, which provides more informative data about how quickly and often affect and suicidal ideation change. This is important because prior research has shown that suicidal thinking can vary dramatically over the course of only a few hours (Kleiman et al., 2017; Nock et al., 2009).
One prior study used EMA to show that reports of negative mood covary with suicidal behavior among those diagnosed with BPD (Links et al., 2007). Another study demonstrates an association between the degree of affective instability and suicidal behaviors in people with BPD (Yen et al., 2004). However, these studies only involved people diagnosed with BPD, so it remains unknown whether people with BPD experience more severe suicidal thinking in response to the same level of negative emotion as people without BPD. To address this question, we used EMA to test whether those diagnosed with BPD would experience a stronger relationship between negative affect and SI than those without such a diagnosis.
1. Method
1.1. Participants
Participants were 35 adult psychiatric inpatients who were hospitalized for a suicide attempt or severe suicidal thinking. The sample was 45.7% female with an average age of 44.3 years (SD = 13.27 years). 82.9% of the sample identified as being of European decent, 5.7% as Asian, 5.7% as Hispanic, 2.9% as African American, and 2.8% as another race/ethnicity. The most common Axis I diagnosis among subjects was Major Depressive Disorder (MDD), and the diagnoses for patients with and without BPD were not significantly different: χ2 (1, N = 35) = 0.17, p = .676. Similarly, there were no differences between other diagnoses between the two groups. Further details about recruitment could be found in Kleiman et al. (2018).
1.2. Procedures
Data on self-reported affective state and suicidal thinking were collected via brief surveys sent to participants four times per day randomly within pre-defined windows (i.e., to avoid interfering with sleep) using MovisensXS (http://xs.movisens.com), an EMA app for Android phones (Kleiman, 2017). If participants did not have an Android phone, we provided them with one for use in this study. Participants were monitored for the duration of their inpatient stay, which ranged from 2 to 46 days and averaged 8.8 days (Kleiman et al., 2018). Participants were given 4 prompts a day and the overall response rate was 57%.
1.3. Measures
1.3.1. Affect
At each survey, participants were asked to report on their current experience of each of 10 affect states (abandoned, anxious, desperate, guilty, hopeless, humiliated, lonely, rage, self-hatred, upset) on a 1 (low) to 10 (very high) scale.
1.3.2. Suicidal thinking
We created a composite suicidal ideation score using three composite items that assessed the (1) desire to die by suicide, (2) intent to die by suicide, and (3) ability to resist the urge to die by suicide (reverse coded) on a (0) none to (9) very much scale.
1.3.3. BPD
Presence of a BPD diagnosis was assessed via medical chart review. Eleven participants had a diagnosis of BPD and two participants had a diagnosis of an unspecified cluster B personality disorder. We made the decision a priori to include all of these participants in the BPD group because the cluster B diagnosis is used by some clinicians when they suspect that BPD is present but do not believe that one hospitalization is sufficient to diagnosis BPD, and in order to increase statistical power. Results are unchanged when these two participants are excluded.
1.4. Analytic strategy
To test our hypotheses, we estimated a series of multilevel models using the lme4 R package where we specified a cross-level interaction between affect state (e.g., abandoned, anxious) as a level-1 variable and BPD status as a level-2 variable. Suicidal ideation at level-1 was the outcome variable (Bates et al., 2015). We estimated a separate model for each affect state and participant-mean centered all predictor affect variables using the EMA tools R Package.10 We plotted all significant analyses using the sjPlot R package (Lüdecke, 2016) and probed them using the computational tools provided by Preacher, Curran, and Bauer (Preacher et al., 2006). To adjust for the number of analyses run, we applied a Bonferonni correction, which reduced the critical alpha to 0.005.
2. Results
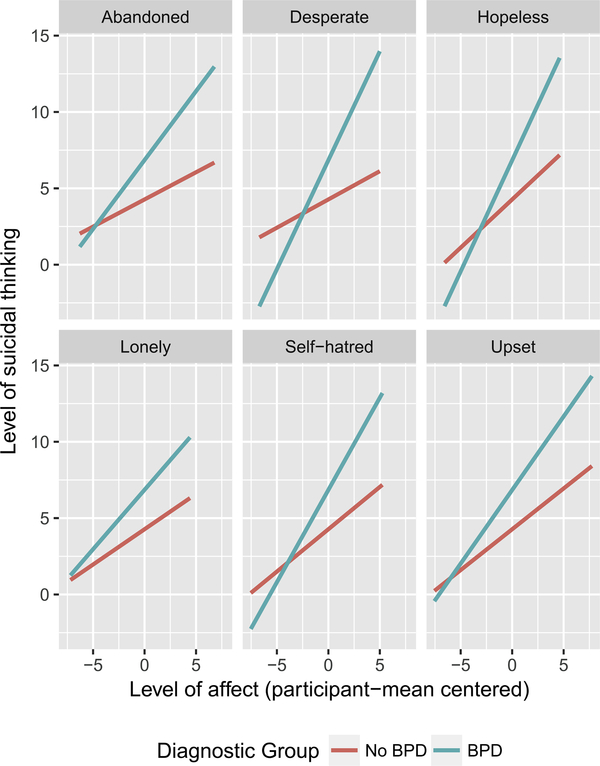
Results revealed that whereas the main effect of BPD was not significant in the prediction of suicidal ideation, a BPD diagnosis moderated the association between negative affect and suicidal thinking. More specifically, for eight out of the ten negative affective states examined, the interaction between BPD and intensity of affective state predicted severity of suicidal ideation – with six of ten remaining significant even after Bonferonni correction (Table 1). Across all of these interactions, the association between negative affect and suicidal thinking was consistently stronger for people with BPD compared to those without (Table 2; Fig. 1).
Table 1.
Multilevel models assessing the interaction between affect and BPD status predicting suicidal ideation.
| Model/variable | B | 95% CI | p | ICC | R2 |
|---|---|---|---|---|---|
| For all models | |||||
| Intercept | 4.27 | 2.55–5.99 | < .001 | ||
| Main effect of BPD (1 = BPD/0 = no BPD) | 2.58 | −0.27–5.48 | .076 | ||
| Abandoned | .649 | .73 | |||
| Main effect | 0.36 | 0.18–0.53 | < .001 | ||
| Abandoned*BPD status | 0.55 | 0.29–0.80 | < .001 | ||
| Anxious | .643 | .71 | |||
| Main effect | 0.55 | 0.36–0.75 | < .001 | ||
| Anxious*BPD status | 0.24 | −0.04–0.52 | .091 | ||
| Desperate | .682 | .76 | |||
| Main effect | 0.37 | 0.19–0.55 | < .001 | ||
| Desperate*BPD status | 1.06 | 0.79–1.32 | < .001 | ||
| Guilty | .642 | .72 | |||
| Main effect | 0.28 | 0.07–0.49 | .008 | ||
| Guilty*BPD status | 0.75 | 0.45–1.06 | < .001 | ||
| Hopeless | .695 | .78 | |||
| Main effect | 0.63 | 0.45–0.81 | < .001 | ||
| Hopeless*BPD status | 0.82 | 0.56–1.09 | < .001 | ||
| Humiliated | .629 | .70 | |||
| Main effect | 0.42 | 0.16–0.68 | .002 | ||
| Humiliated*BPD status | 0.33 | −0.02–0.67 | .062 | ||
| Lonely | .640 | .72 | |||
| Main effect | 0.46 | 0.28–0.65 | < .001 | ||
| Lonely*BPD status | 0.32 | 0.04–0.59 | .023 | ||
| Rage | .632 | .71 | |||
| Main effect | 0.36 | 0.12–0.60 | .003 | ||
| Rage*BPD status | 0.37 | 0.05–0.68 | .021 | ||
| Self-hatred | .663 | .74 | |||
| Main effect | 0.55 | 0.35–0.76 | < .001 | ||
| Self-hatred*BPD status | 0.65 | 0.36–0.95 | < .001 | ||
| Upset | 667 | 76 | |||
| Main effect | 0.53 | 0.38–0.69 | < .001 | ||
| Upset*BPD status | 0.43 | 0.21–0.64 | < .001 |
Table 2.
Slopes for significant interactions.
| B | SE | Z | p | |
|---|---|---|---|---|
| Abandoned | ||||
| No BPD | 0.36 | 0.09 | 4.86 | < .001 |
| BPD | 0.90 | 0.09 | 9.76 | < .001 |
| Desperate | ||||
| No BPD | 0.37 | 0.09 | 4.13 | < .001 |
| BPD | 1.43 | 0.10 | 14.26 | < .001 |
| Guilty | ||||
| No BPD | 0.28 | 0.11 | 2.64 | .008 |
| BPD | 1.04 | 0.11 | 9.07 | < .001 |
| Hopeless | ||||
| No BPD | 0.63 | 0.09 | 4.86 | < .001 |
| BPD | 1.46 | 0.10 | 14.94 | < .001 |
| Lonely | ||||
| No BPD | 0.46 | 0.10 | 4.86 | < .001 |
| BPD | 0.78 | 0.10 | 7.66 | < .001 |
| Rage | ||||
| No BPD | 0.36 | 0.12 | 2.94 | .003 |
| BPD | 0.72 | 0.10 | 7.11 | < .001 |
| Self-hatred | ||||
| No BPD | 0.55 | 0.11 | 5.22 | < .001 |
| BPD | 1.21 | 0.11 | 11.29 | < .001 |
| Upset | ||||
| No BPD | 0.53 | 0.08 | 6.90 | < .001 |
| BPD | 0.96 | 0.08 | 12.45 | < .001 |
Fig. 1.
Plots for significant interaction effects.
3. Discussion
We examined whether the association between negative affect and suicidal ideation is stronger among suicidal inpatients diagnosed with BPD compared to those without such a diagnosis. As hypothesized, we found that negative affective states are more strongly associated with suicidal ideation among those with BPD than among those at high clinical severity (i.e., suicidal inpatients) but without BPD. Importantly, these results also revealed that the main effect of BPD diagnosis was not significantly associated with severity of suicidal ideation in this high-risk clinical sample, suggesting that the presence of a BPD diagnosis by itself does not mean that suicidal thinking will always be more severe; only when patients are exposed to strong negative emotions are patients with BPD more likely to develop suicidal thoughts. This finding highlights the advantage of high-resolution methods like EMA. Had patients been surveyed over days or weeks rather than hours, these associations may not have been observed.
There are several important limitations of this study. First, BPD diagnoses were extracted from the clinical notes (i.e., discharge summaries) rather than gold-standard diagnostic interviews. Given that inpatient psychiatrists are often hesitant to diagnose inpatients with personality disorders, the frequency of BPD may be underestimated in this sample (Westen and Arkowitz-Westen, 1998). Second, all data relied on participant self-report, which is subject to social desirability and other potential biases. Third, the sample size was relatively small and we had limited power to detect small effects. On balance, the strengths of this study included high subject compliance with evaluations, the use of EMA to capture negative affect and degree of SI at the resolution of hours, a conservative use of the Bonferonni correction to adjust the threshold for statistical significance, and a rigorous and well-matched comparator group (high-risk inpatients hospitalized in the same psychiatric unit).
Overall, the main study findings have important implications for clinical practice: for the same degree of negative affect reported by psychiatric inpatients, those diagnosed with BPD are more likely to engage in suicidal ideation than equally high-risk patients without BPD.
Acknowledgements
The research was supported by the Chet and Will Griswold Suicide Prevention Fund (MKN) and the For the Love of Travis Foundation (MKN).
Footnotes
Conflicts of interest
David Mou receives consulting fees from Valera Health, a digital healthcare company.
Appendix A. Supplementary data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jpsychires.2018.08.006.
References
- Bates D, Mächler M, Bolker B, Walker S, 2015. Fitting linear mixed-effects models using lme4. J. Stat. Software 67, 1–48. 10.18637/jss.v067.i01. [DOI] [Google Scholar]
- Boergers J, Spirito A, Donaldson D, 1998. Reasons for adolescent suicide attempts: associations with psychological functioning. J. Am. Acad. Child Adolesc. Psychiatr 37, 1287–1293. 10.1097/00004583-199812000-00012. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, 2017. EMAtools: Data Management Tools for Real-time Monitoring/ecological Momentary Assessment Data.
- Kleiman EM, Nock MK, 2018. Real-time assessment of suicidal thoughts and behaviors. Curr. Opin. Psychol., Suicide 22, 33–37. 10.1016/j.copsyc.2017.07.026. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, Nock MK, 2017. Examination of real-time fluctuations in suicidal ideation and its risk factors: results from two ecological momentary assessment studies. J. Abnorm. Psychol 126, 726–738. 10.1037/abn0000273. [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Picard RW, Huffman JC, Nock MK, 2018. Digital phenotyping of suicidal thoughts. Depress. Anxiety 35, 601–608. 10.1002/da.22730. [DOI] [PubMed] [Google Scholar]
- Leichsenring F, Leibing E, Kruse J, New AS, Leweke F, 2011. Borderline personality disorder. Lancet 377, 74–84. 10.1016/S0140-6736(10)61422-5. [DOI] [PubMed] [Google Scholar]
- Links PS, Eynan R, Heisel MJ, Barr A, Korzekwa M, McMain S, Ball JS, 2007. Affective instability and suicidal ideation and behavior in patients with borderline personality disorder. J. Pers. Disord 21, 72–86. 10.1521/pedi.2007.21.1.72. [DOI] [PubMed] [Google Scholar]
- Lüdecke D, 2016. SjPlot: Data Visualization for Statistics in Social Science.
- Nock MK, Prinstein MJ, Sterba SK, 2009. Revealing the form and function of self-injurious thoughts and behaviors: a real-time ecological assessment study among adolescents and young adults. J. Abnorm. Psychol 118, 816–827. 10.1037/a0016948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Wedig MM, Holmberg EB, Hooley JM, 2008. The emotion reactivity scale: development, evaluation, and relation to self-injurious thoughts and behaviors. Behav. Ther 39, 107–116. 10.1016/j.beth.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Oldham JM, 2006. Borderline personality disorder and suicidality. Am. J. Psychiatr 163, 20–26. 10.1176/appi.ajp.163.1.20. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ, 2006. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. J. Educ. Behav. Stat 31, 437–448. 10.3102/10769986031004437. [DOI] [Google Scholar]
- Rasmussen S, Hawton K, Philpott-Morgan S, O’Connor RC, 2016. Why do adolescents self-harm? Crisis 37, 176–183. 10.1027/0227-5910/a000369. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR, 2008. Ecological momentary assessment. Annu. Rev. Clin. Psychol 4, 1–32. [DOI] [PubMed] [Google Scholar]
- Westen D, Arkowitz-Westen L, 1998. Limitations of Axis II in diagnosing personality pathology in clinical practice. Am. J. Psychiatr 155, 1767–1771. 10.1176/ajp.155.12.1767. [DOI] [PubMed] [Google Scholar]
- Woodberry KA, Gallo KP, Nock MK, 2008. An experimental pilot study of response to invalidation in young women with features of borderline personality disorder. Psychiatr. Res 157, 169–180. 10.1016/j.psychres.2007.06.007. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, McGlashan TH, Zanarini MC, Morey LC, 2004. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. Am. J. Psychiatr 161, 1296–1298. 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]