Abstract
Objectives:
Suicide in older adults is a major public health issue. Past research across the US adult population has linked prescription medication misuse with suicidal ideation. No work has evaluated associations between prescription opioid or benzodiazepine misuse and suicidal ideation in older adults, and this work aimed to address that gap.
Methods/Design:
Data were from adults 50 years and older participating in the 2015-16 National Survey on Drug Use and Health (n = 17,608). Design-based logistic regression evaluated links between any past-year prescription opioid or benzodiazepine use without misuse or prescription misuse and past-year suicidal ideation, after controlling for sociodemographic, physical health, mental health and substance use correlates associated with suicidal ideation.
Results:
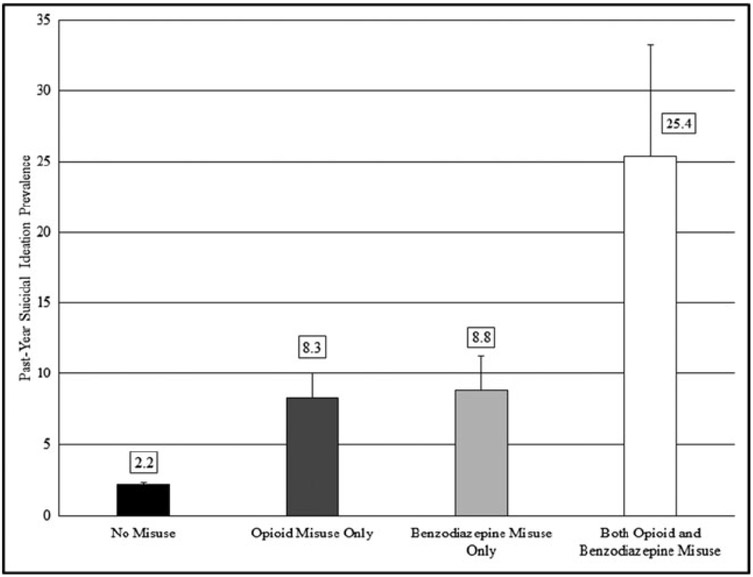
After controlling for all correlates, past-year use without misuse of prescription opioids or benzodiazepines were not associated with past-year suicidal ideation in older adults. In contrast, past-year opioid misuse (AOR = 1.84, 95% CI = 1.07-3.19) and benzodiazepine misuse (AOR = 2.00, 95% CI = 1.01-3.94) were significantly associated with past-year suicidal ideation, even after controlling for all covariates. While 2.2% of US older adults not engaged in either opioid or benzodiazepine misuse reported past-year suicidal ideation, 25.4% of those who misused both medication classes endorsed such suicidality (AOR = 4.73, 95% CI = 2.07-10.79).
Conclusions:
Both past-year prescription opioid and benzodiazepine misuse are associated with past-year suicidal ideation in US older adults. Clinicians encountering older adult patients at-risk for or engaged in prescription medication misuse also should screen for suicidality.
Keywords: Older adult, opioid, benzodiazepine, prescription misuse, suicidality
INTRODUCTION
In 2015, over 44,000 US residents completed suicide, making it the tenth leading cause of death.1 This followed increases in US age-adjusted suicide rates between 1999 and 2014 from 10.5 to 13.0 per 100,000.2 In particular, older adult suicide is a public health problem in the US specifically and worldwide;3-5 while only 8.2% of the worldwide population is 65 years and older, they accounted for roughly 17% of completed suicides.3 While suicide rates are highest in women aged 45 to 64 years,2 older males evidence the greatest risk of suicide across the US population, with four of the five highest suicide rates in males 55 and older.1
Research has identified many factors associated with older adult suicidal ideation and behavior. One of the most salient is psychopathology,6 particularly major depression.3,7-9 Research in US,3 South Korean,8,9 Brazilian7 and Australian10 older adults suggests that psychological distress generally and major depression specifically account for the most variance in models examining suicidal ideation. Other risk factors for suicidal ideation and behavior include male sex11 (also noted above), being divorced or widowed3 or otherwise unmarried,11 lower household income,12 and lower educational attainment.11,13,14 Sexual minority (i.e., LGB) status is a robust correlate of suicide across ages, though it appears unexamined in older adults specifically.15 Finally, a substance use disorder (SUD) diagnosis,4,9,11,16 poorer physical health,3 and frequent visits to the emergency department (ED)11 appear to be strong correlates of suicidal ideation and behavior in older adults.
One unexamined potential correlate of older adult suicidal ideation is prescription drug misuse (PDM), which describes use of another person’s medication or use of one’s own medication in ways not intended by the prescribing clinician. In adolescents, both cross-sectional17,18 and longitudinal evidence19 link opioid and benzodiazepine PDM with suicidal ideation. Work across the US adult population also supports a link between opioid PDM and suicidal ideation.20-22 While opioid-related mortality rates rose among US older adults from 2006 to 2013,23 it is not clear that these increased rates were from intentional misuse. In all, no research could be found on the relationship of PDM and suicidal ideation in older adults.
Two factors suggest the importance of studying potential links between suicidal ideation and PDM in older adults. First, US adults aged 55 and older are prescribed benzodiazepine medication at higher rates than other age groups,24,25 with opioid prescription rates that are in the top two among age cohorts.24 This is despite clinical recommendations against most benzodiazepine use in older adults26 and that opioid use should be cautiously initiated, especially in older adults with cognitive deficits.27 Second, benzodiazepine and opioid medication are commonly used in intentional overdose. Older adults have a heightened potential for accidental overdose28 and appear to have more lethal suicide attempts than those of younger individuals.29,30 Thus, the evidence suggests that research is needed evaluating potential links between opioid and benzodiazepine PDM in older adults and suicidal ideation; work also is needed that evaluates potential links between use (without misuse) of these medications and suicidal ideation. This study is intended to address those gaps in the literature through analyses of the 2015 and 2016 National Survey on Drug Use and Health (NSDUH) public use files.
Aims and Hypotheses
The primary aims of this work were to evaluate whether past-year prescription opioid and benzodiazepine use without misuse or misuse were associated with past-year suicidal ideation in US older adults (aged 50 and older). We hypothesized that, after controlling for sociodemographic, physical health, mental health and substance use of past-year suicidal ideation, past-year use without misuse of either opioids or benzodiazepines would not be associated with suicidal ideation but that misuse of either opioids or benzodiazepines would be associated with suicidal ideation, given past work across the population.20
MATERIALS AND METHODS
The NSDUH is an annual US survey of substance use, SUD, mental health, and other associated behaviors. It uses an independent, multistage probability sample, with population-based weighting for nationally-representative and unbiased estimates. The NSUDH assesses all sensitive questions (e.g., on PDM) via audio computer-assisted self-interviewing (ACASI) to maximize honest reporting. The 2015-16 versions included skip-outs and consistency checks to promote full responding and data consistency. Beginning in 2015, the NSDUH’s PDM assessment was redesigned to assess any medication use and a greater variety of PDM variables. More information on the NSDUH, including on psychometrics and the 2015 redesign, is available elsewhere.31-34
Participants
Participants were adults 50 years and older (n = 17,608, 40.9% of the weighted sample) in the 2015-16 NSDUH public use files. Within the weighted older adult sample, 53.2% was female and 43.2% was 65 years and older. The most common racial/ethnic groups were white/Caucasian (73.2%), African-American (10.3%), and Hispanic/Latino (10.2%); no other racial/ethnic group was above 4%. Also, 2.4% identified as gay, lesbian, or bisexual. In terms of educational attainment, 14.6% did not complete high school and 31.1% were college/university graduates. Finally, 16.2% had household incomes below $20,000 (USD), while 36.5% had household incomes of $75,000 (USD) or greater.
Measures
Primary Outcome
The primary outcome of interest was past-year suicidal ideation. All participants were asked (bolding from the NSDUH): “The next few questions are about thoughts of suicide. At any time in the past 12 months, that is from [date 12 months ago inserted] up to and including today, did you seriously think about trying to kill yourself?” Participants answering “yes” had past-year suicidal ideation. Of the 17,608 older adults, 96 (0.55%) refused to answer or provided bad data on this question. A further 398 (2.2% of the older adult sample) were missing data on various correlates (below), leaving a total of 17,114 older adults for our analytic sample.
Correlates
Correlate selection drew mainly from past work on older adult suicidality,3,4,35,36 with additional attention to research that examined suicidal ideation and PDM.17,19,20,22 Correlates were grouped into sociodemographic, physical health, mental health, substance use and prescription use/misuse variables.
Sociodemographic variables were: age group (restricted by the public use file to 50-64 years or 65 and older), sex, race/ethnicity, sexual orientation (heterosexual, gay male, lesbian, bisexual), population density, household income, marital status, educational attainment and employment status.
Physical Health Correlates were: self-reported health (excellent, very good, good, fair/poor), past-year cancer, past-year heart condition, number of past-year emergency department (ED) visits and any past-year inpatient hospitalization.
Mental Health Correlates were: past-year major depressive episode (MDE), past-year serious psychological distress (SPD) and past-year level of impairment from mental health symptoms. Past-year MDE was assessed based on the DSM-IV,37 with good psychometrics.38 The SPD assessment comes from the K6 assessment of nonspecific psychological distress39 for the worst month in the past year; scores of 12 or greater (out of 24) signify past-year SPD.31,40 Past-year mental health-related impairment comes from the World Health Organization’s Disability Assessment Scale (WHODAS), a 13-item assessment in the NSUDH.31,41
Substance Use Correlates were a series of three-level variables patterned as no past-year use, past-year use without a use disorder, and past-year use disorder. These variables captured past-year tobacco (non-use/use without dependence/dependence) and alcohol or marijuana (non-use/use without disorder/abuse or dependence) use. Past-year alcohol or marijuana abuse or dependence are assessed using DSM-IV criteria,37 with strong psychometrics.33 For nicotine dependence, either a score of 2.75 or greater on the Nicotine Dependence Syndrome Scale42 or needing to smoke a cigarette within 30 minutes of waking up, as assessed by the Fagerstrom Test of Nicotine Dependence43 qualified as dependence (among those who smoked in the past month).31
Prescription Opioid and Benzodiazepine Use/Misuse: Assessment of opioid and benzodiazepine use or misuse occur separately in the NSDUH, with the opioid assessment in one module (i.e., pain relievers, such as OxyContin®, Vicodin® and hydrocodone) and the benzodiazepine assessment in two modules (i.e., tranquilizers and sedatives, such as Xanax®, Valium® or alprazolam). To aid recall, the NSDUH used trade and generic drug names and medication pictures.
Initially, past-year opioid and benzodiazepine exposure (i.e., any medical use or misuse) were assessed separately by asking about any use of a large number of generic and trade named medications in these classes. In those with past-year exposure, past-year opioid misuse and/or past-year benzodiazepine misuse were assessed. To introduce the assessment of misuse, the following instruction is given: “The next question asks about using [medication class] in any way a doctor did not direct you to use them. [P]lease think only about your use of the drug in any way a doctor did not direct you to use it, including: Using it without a prescription of your own; Using it in greater amounts, more often, or longer than you were told to take it; Using it in any other way a doctor did not direct you to use it.”
For these analyses, two three-level variables were created: past-year benzodiazepine use/misuse status and past-year opioid use/misuse status. These captured, separately for benzodiazepines and opioids, no past-year use, use without misuse (i.e., those with exposure who denied misuse) and misuse.
Data Analyses
Data were clustered on primary sampling units and stratified appropriately. An adjusted person-level weight (weight/2) was used to produce unbiased estimates, given use of two years of aggregated data. The Taylor series linearization with adjusted degrees of freedom44,45 was used for the complex survey data, creating robust variance estimates. Analyses were performed in Stata 15.1.
Initial analyses employed design-based univariable regressions to test the relationship between past-year suicidal ideation in older adults (primary outcome) and each correlate, including the opioid and benzodiazepine use/misuse variables. Correlates with a p-value of 0.25 or lower were retained in the multivariable models that followed.46 A more stringent p-value for retention (e.g., 0.05) was not chosen, as it can exclude variables that account for theoretically important variance in multivariable models.47,48
Multivariable models proceeded as follows: an initial block was entered containing sociodemographic correlates and both of the prescription opioid or benzodiazepine use/misuse variables. If a significant association between either of the opioid or benzodiazepine use/misuse variables and suicidal ideation remained, a further block of correlates was added in this order: physical health, mental health and substance use. For the substance use variables (including benzodiazepine and opioid use/misuse), non-use was set as the reference.
RESULTS
Univariable Associations between Past-Year Suicidal Ideation and Correlates
All univariable regression results are captured in Table 1. For sociodemographics, neither sex nor population density were retained in multivariable models (ps > 0.25), but race/ethnicity, marital status, educational attainment and employment status were retained (ps ≤ 0.25). Finally, lower household income, membership in the 50 to 64 age group and gay male or bisexual sexual orientation were significantly associated with past-year suicidal ideation (both ps < 0.001).
Table 1:
Univariable Relationships between Correlates/Outcomes and Suicidal Ideation
| t | SE | p-value | OR | 95% CI | |
|---|---|---|---|---|---|
| Sociodemographics | |||||
| Age Group | −4.43 | 0.07 | < 0.001 | 0.57 | 0.44-0.74 |
| Race/Ethnicity | −1.60 | 0.03 | 0.12 | 0.94 | 0.88-1.02 |
| Sex | −0.84 | 0.10 | 0.41 | 0.91 | 0.73-1.14 |
| Population Density | 0.86 | 0.10 | 0.39 | 1.08 | 0.90-1.30 |
| Income | −6.45 | 0.02 | < 0.001 | 0.83 | 0.78-0.88 |
| Marital Status | 3.80 | 0.05 | < 0.001 | 1.19 | 1.08-1.30 |
| Education | −1.95 | 0.05 | 0.06 | 0.90 | 0.80-1.00 |
| Employment Status | 1.85 | 0.05 | 0.07 | 1.09 | 0.99-1.19 |
| Sexual Orientation | 3.37 | 0.15 | 0.001 | 1.41 | 1.15-1.74 |
| Physical Health | |||||
| Past-Year Hospitalization | 6.36 | 0.30 | < 0.001 | 2.31 | 1.77-3.00 |
| Self-Reported Health | 7.23 | 0.13 | < 0.001 | 1.74 | 1.49-2.03 |
| Past-Year Cancer | 1.91 | 0.54 | 0.06 | 1.79 | 0.97-3.30 |
| Past-Year Heart Condition | 0.94 | 0.20 | 0.35 | 1.17 | 0.83-1.66 |
| Past-Year Number of ED Visits | 0.31 | 0.004 | 0.76 | 1.00 | 1.00-1.00 |
| Mental Health | |||||
| Past-Year SPD | 22.71 | 2.67 | < 0.001 | 20.16 | 15.45-26.29 |
| Past-Year MDE | 22.92 | 0.01 | < 0.001 | 11.09 | 8.98-13.69 |
| Mental Health Impairment | 26.20 | 0.03 | < 0.001 | 1.57 | 1.52-1.63 |
| Alcohol Use | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Use Disorder | −1.19 | 0.12 | 0.24 | 0.84 | 0.64-1.12 |
| Past-Year Alcohol Use Disorder | 6.08 | 0.81 | <0.001 | 3.74 | 2.42-5.79 |
| Tobacco Use | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Dependence | 0.34 | 0.18 | 0.74 | 1.06 | 0.76-1.48 |
| Past-Year Nicotine Dependence | 5.52 | 0.46 | <0.001 | 2.63 | 1.85-3.75 |
| Marijuana Use | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Use Disorder | 6.58 | 0.33 | <0.001 | 2.43 | 1.85-3.19 |
| Past-Year Cannabis Use Disorder | 6.39 | 4.14 | <0.001 | 11.03 | 5.19-23.47 |
| Benzodiazepine Use and Misuse | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Misuse | 8.27 | 0.41 | <0.001 | 3.03 | 2.31-3.96 |
| Past-Year Misuse | 7.66 | 2.53 | <0.001 | 8.87 | 5.01-15.73 |
| Opioid Use and Misuse | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Misuse | 5.37 | 0.25 | <0.001 | 1.97 | 1.53-2.53 |
| Past-Year Misuse | 8.51 | 1.64 | <0.001 | 7.10 | 4.47-11.28 |
Source: NSDUH, 2015-2016 cohorts.
Abbreviations: SE = Standard Error, OR = Odds Ratio, SUD = Substance Use Disorder, SPD = Serious Psychological Distress, MDE = Major Depressive Episode
For physical health, both self-reported health and past-year inpatient hospitalization were significantly associated with suicidal ideation (p < 0.001). Past-year cancer was retained (ps < 0.25), while past-year heart condition (p = 0.35) and number of past-year ED visits (p = 0.76) were not retained. Also, all examined mental health variables (i.e., past-year MDE, SPD and mental health-related impairment) were significantly and positively associated with past-year suicidal ideation in older adults (ps < 0.001). For other substance use, past-year alcohol use disorder, nicotine dependence, marijuana use without use disorder, and marijuana use disorder were significantly associated with increased odds of past-year suicidal ideation (ps < 0.001). Past-year alcohol use without use disorder was retained for multivariable models (p = 0.24), but past-year tobacco use without nicotine dependence was not (p = 0.74).
Finally, all four past-year benzodiazepine and opioid use/misuse variables (i.e., benzodiazepine use without misuse, benzodiazepine misuse, opioid use without misuse and opioid misuse) were significantly associated with past-year suicidal ideation in US adults aged 50 and older (ps < 0.001).
Multivariable Associations between Past-Year Suicidal Ideation and Benzodiazepine or Opioid Use/Misuse
As noted in the Methods section, initial analysis examined the association of the benzodiazepine and opioid use/misuse variables in a single model, controlling for sociodemographics. In these models, all benzodiazepine and opioid outcomes remained associated with a greater likelihood of suicidal ideation in older adults. Specifically, past-year benzodiazepine use without misuse (adjusted odds ratio [AOR] = 2.37, 95% confidence interval [CI] = 1.80-3.11, p < 0.001), benzodiazepine misuse (AOR = 4.57, 95% CI = 2.62-7.98, p < 0.001), opioid use without misuse (AOR = 1.53, 95% CI = 1.17-1.99, p = 0.002) and opioid misuse (AOR = 3.91, 95% CI = 2.43-6.29, p < 0.001) were significant correlates of past-year suicidal ideation after controlling for sociodemographics.
The second model included both sociodemographic and physical health controls in models. All benzodiazepine outcomes and opioid misuse remained significant correlates: benzodiazepine use without misuse (AOR = 2.14, 95% CI = 1.62-2.82, p < 0.001), benzodiazepine misuse (AOR = 4.37, 95% CI = 2.59-7.36, p < 0.001) and opioid misuse (AOR = 3.29, 95% CI = 2.00-5.40, p < 0.001). Opioid use without misuse (AOR = 1.26, 95% CI = 0.94-1.67, p = 0.12) ceased to be significant, however.
The third model added mental health variables, and, in these models, past-year benzodiazepine use without misuse ceased to be significant (AOR = 1.05, 95% CI = 0.74-1.47, p = 0.79) and opioid use without misuse remained non-significant (AOR = 1.01, 95% CI = 0.73-1.40, p = 0.95). In contrast, both past-year benzodiazepine misuse (AOR = 2.18, 95% CI = 1.13-4.20, p = 0.022) and opioid misuse (AOR = 2.23, 95% CI = 1.31-3.80, p = 0.004) remained significant correlates of past-year suicidal ideation in older adults.
A final set of models included all control variables: sociodemographics, physical health, mental health and substance use; this final model is captured in Table 2. As in the third model, neither past-year benzodiazepine use without misuse (AOR = 1.06, 95% CI = 0.75-1.49, p = 0.74) nor past-year opioid use without misuse (AOR = 1.00, 95% CI = 0.73-1.37, p = 0.99) were associated with past-year suicidal ideation. Even after controlling for all sociodemographic, physical and mental health and substance use covariates, both benzodiazepine misuse (AOR = 2.00, 95% CI = 1.01-3.94, p = 0.046) and opioid misuse (AOR = 1.84, 95% CI = 1.07-3.19, p = 0.03) remained significantly associated with past-year suicidal ideation in older adults.
Table 2:
Multivariable Relationships between Correlates/Outcomes and Suicidal Ideation
| t | SE | p-value | AOR | 95% CI | |
|---|---|---|---|---|---|
| Sociodemographics | |||||
| Age Group | 0.13 | 0.13 | 0.90 | 1.02 | 0.79-1.31 |
| Race/Ethnicity | −2.14 | 0.04 | 0.038 | 0.92 | 0.85-0.99 |
| Income | −3.06 | 0.03 | 0.004 | 0.89 | 0.82-0.96 |
| Marital Status | −2.51 | 0.05 | 0.015 | 0.86 | 0.76-0.97 |
| Education | −0.05 | 0.07 | 0.98 | 1.00 | 0.88-1.14 |
| Employment Status | −2.09 | 0.06 | 0.042 | 0.88 | 0.77-0.99 |
| Sexual Orientation | 0.93 | 0.15 | 0.36 | 1.13 | 0.86-1.49 |
| Physical Health | |||||
| Past-Year Hospitalization | 1.79 | 0.24 | 0.08 | 1.37 | 0.96-1.96 |
| Self-Reported Health | 1.34 | 0.09 | 0.19 | 1.12 | 0.95-1.32 |
| Past-Year Cancer | 0.72 | 0.54 | 0.48 | 1.34 | 0.59-3.02 |
| Mental Health | |||||
| Past-Year SPD | 8.23 | 0.80 | < 0.001 | 4.42 | 3.08-6.35 |
| Past-Year MDE | 6.00 | 0.06 | < 0.001 | 2.53 | 1.86-3.46 |
| Mental Health Impairment | 7.21 | 0.03 | < 0.001 | 1.23 | 1.16-1.30 |
| Alcohol Use | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Use Disorder | −0.24 | 0.15 | 0.81 | 0.96 | 0.70-1.32 |
| Past-Year Alcohol Use Disorder | 2.85 | 0.48 | 0.006 | 1.99 | 1.23-3.23 |
| Nicotine Use | |||||
| Nicotine Dependence | 0.38 | 0.21 | 0.71 | 1.08 | 0.73-1.59 |
| Marijuana Use | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Use Disorder | 0.79 | 0.21 | 0.44 | 1.15 | 0.80-1.65 |
| Past-Year Cannabis Use Disorder | 2.67 | 1.72 | 0.01 | 3.59 | 1.37-9.39 |
| Benzodiazepine Use and Misuse | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Misuse | 0.33 | 0.18 | 0.74 | 1.06 | 0.75-1.49 |
| Past-Year Misuse | 2.05 | 0.68 | 0.046 | 2.00 | 1.01-3.94 |
| Opioid Use and Misuse | |||||
| No Past-Year Use | ----------------Reference Group--------------- | ||||
| Past-Year Use, without Misuse | 0.02 | 0.16 | 0.99 | 1.00 | 0.73-1.37 |
| Past-Year Misuse | 2.24 | 0.50 | 0.03 | 1.84 | 1.07-3.19 |
Source: NSDUH, 2015-2016 cohorts.
Abbreviations: SE = Standard Error, OR = Odds Ratio, SUD = Substance Use Disorder, SPD = Serious Psychological Distress, MDE = Major Depressive Episode
Past-Year Suicidal Ideation Prevalence in Older Adults as a Function of PDM
Per Figure 1, in older adults with neither opioid nor benzodiazepine misuse, 2.2% endorsed past-year suicidal ideation. Past-year misuse of only one medication class (i.e., opioids or benzodiazepines) was associated with roughly a 6% increase in suicidal ideation prevalence: 8.3% and 8.8% for opioids and benzodiazepines, respectively. In contrast, 25.4% of older adults with past-year misuse of both opioids and benzodiazepines reported past-year suicidal ideation. Multivariable logistic regression, controlling for all correlates (including use without misuse of opioid or benzodiazepine medication), indicated that those with past-year opioid misuse only (AOR = 1.68, 95% CI = 0.96-2.93, p = 0.068) or benzodiazepine misuse only (AOR = 1.44, 95% CI = 0.57-3.67, p = 0.44) did not differ from those without past-year misuse in past-year suicidal ideation odds. In contrast, those with past-year misuse of both opioids and benzodiazepines had significantly elevated odds of suicidal ideation over those with no misuse (AOR = 4.53, 95% CI = 1.82-11.28, p = 0.002).
Figure 1:
Prevalence of Past-Year Suicidal Ideation by Past-Year Prescription Drug Misuse Status
Notes: Error bars represent standard errors
DISCUSSION
Past-year prescription opioid misuse and past-year prescription benzodiazepine misuse were each associated with elevated odds of past-year suicidal ideation in adults 50 years and older, with an 84% increase in odds with opioid misuse and a 100% increase in odds with benzodiazepine misuse. The significant relationships between past-year opioid or benzodiazepine misuse and past-year suicidal ideation remained after controlling past-year use without misuse from each medication class and misuse of the other medication class (i.e., opioid misuse was significantly associated with suicidal ideation after accounting for benzodiazepine misuse). Furthermore, these models controlled for a variety of sociodemographic, substance use, physical health and mental health correlates of suicidal ideation, suggesting that the link between suicidal ideation and benzodiazepine and/or opioid misuse is robust. These findings are also consistent with past work on opioid misuse in adolescents17-19 and adults20-22 and add to the literature by both highlighting benzodiazepine misuse and establishing these relationships in older adults.
In contrast, links between past-year suicidal ideation and past-year use without misuse of either opioids or benzodiazepines were not significant when known correlates of suicidality were included in models. Thus, while use without misuse does not mark suicidal ideation, opioid and/or benzodiazepine misuse indicate the need for screening and potentially intervention to prevent suicide in older adults. The SOAPP is a validated screening measure for opioid misuse risk49 that can aid clinician decision-making, though no such instruments exist for benzodiazepine misuse.
Most notably, over one-quarter (25.4%) of those with both past-year opioid and benzodiazepine misuse endorsed past-year suicidal ideation, roughly triple the prevalence of suicidal ideation in those with only opioid misuse (8.3%) or only benzodiazepine misuse (8.8%). Older adults with both opioid and benzodiazepine misuse have 353% greater odds of past-year suicidal ideation than those without misuse, and those with co-misuse are particularly at-risk and likely need both significant substance use and psychiatric interventions.
In addition, the analyses support screening for suicidal ideation in those with past-year MDE, SPD, or mental health-related impairment; as mental health is a well-established suicidality correlate,3,6 this result was expected. Past-year alcohol or cannabis use disorders also were significant and robust correlates of past-year suicidality. These factors – past-year MDE, SPD, mental health-related impairment, past-year alcohol use disorder, past-year cannabis use disorder and past-year prescription opioid and/or benzodiazepine misuse – appear particularly crucial to assess in older adults, as they are both intervention targets in their own right and signal potential suicidal ideation. Opioid and benzodiazepine medication each are associated with unintentional and intentional overdose (i.e., suicide), making assessment of their misuse especially important.
Notably, only self-reported health was significantly associated with past-year suicidal ideation in the final models, with increasingly poor health associated with increased suicidal ideation. In part, the relative lack of significant health variables may reflect the limited variable choices available in the NSDUH. Age, income, marital status, and sexual orientation were each associated with suicidal ideation in univariable models, with only income and marital status remaining significant in the final models. Younger age group (50-64), lower household income, divorced, or gay or bisexual male status were associated with increased odds of suicidal ideation. Both lower household income and divorced status are established correlates of suicidality in older adults,3,12 while sexual orientation needs further study in older adults specifically.
Clinically, these results further reinforce that benzodiazepine use in older adults should be generally avoided,26 though recent work found that roughly 22% of US older adults had used a benzodiazepine in the past year.25 Greater use of non-pharmacological therapies for anxiety or insomnia, like cognitive-behavioral therapy,45 may be warranted. For opioid medication, more time-limited prescribing at lower dose (consistent with recent guidelines)27 may be the best course, given the risks for gastrointestinal bleeding associated with older adult non-steroidal anti-inflammatory drug (NSAID) use.26
Limitations
The NSDUH data are cross-sectional, preventing causal inference about the relationship between suicidal ideation and PDM in older adults. While one variable may have influenced the other, both could have been related through a third factor (e.g., internalizing psychopathology). A second limitation was the limited availability of variables, especially those pertaining to pain and physical health, and these limited unassessed measures may have influenced the patterns of relationships with suicidal ideation. Third, self-report bias was possible, though research indicates that self-report substance use data are reliable and valid;50,51 in addition, use of medication pictures, numerous trade and generic medication names and ACASI self-interview methods should reduce self-report bias.52,53 Finally, older adults in non-household settings were likely under-sampled, despite the efforts of the NSDUH to sample older adults in controlled access dwellings (e.g., assisted living).54 Rates of psychopathology, including depression,55 are higher in older adults in long-term care than in community-dwelling older adults, and suicidal ideation56 appears somewhat common in older adults in long-term care settings. Conversely, medication access is restricted in these settings, potentially limiting PDM. Given that many older adults reside in controlled access settings, more research is needed on PDM and suicidal ideation in these older adults.
Conclusions
Past-year misuse of opioid or benzodiazepine medication was associated with increased odds of past-year suicidal ideation in adults 50 years and older, though use without misuse of either medication was not. Strikingly, 25.4% of older adults with both past-year opioid and benzodiazepine misuse endorsed past-year suicidal ideation. Together, these results suggest that older adults need to be screened for prescription opioid and/or benzodiazepine misuse and that those endorsing misuse or with signs of misuse (e.g., early refill requests, inconsistent pill counts) also need to be screened for suicidal ideation. Use of prescription drug monitoring program (PDMP) databases is also encouraged to identify potential co-use of opioid and benzodiazepine medication in older adults. In addition to limiting the potential harms in older adults of prescription misuse, such screening could identify those at-risk for more frank suicidal behavior, limiting the consequences of PDM and suicidality in older adults.
KEY POINTS:
Use without misuse of either prescription benzodiazepine or opioid medication in the past year was not associated with past-year suicidal ideation in adults 50 years and older, after controlling for correlates of suicide in this age group.
In contrast, past-year misuse of either prescription benzodiazepine or opioid medication was associated with suicidal ideation in older adults, even after controlling for the correlates of suicide.
Of those with no past-year misuse from either medication class, 2.2% reported past-year suicidal ideation, while 25.4% of those who misused both classes reported such ideation.
These results highlight the importance of screening for opioid and benzodiazepine misuse in older adults, with screening for suicidality warranted in those with signs of misuse, such as early refill requests.
ACKNOWLEDGEMENTS
The NSDUH is funded by the Substance Abuse and Mental Health Services Administration; this work was supported by the National Institutes of Health [R01AA025684, R01CA212517, R01DA036541, R01DA042146, and R01DA043696]. Neither NIH nor SAMHSA had any further role in study design, the collection, analysis or interpretation of data, the writing of the report, or the decision to submit the paper for publication. The authors noted no conflicts of interest.
REFERENCES
- 1.National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-term Trends in Health. In. Hyattsville, MD: Author; 2017. [PubMed] [Google Scholar]
- 2.Curtin SC, Warner M, Hedegaard H. Increase in Suicide in the United States, 1999-2014. NCHS data brief. 2016(241):1–8. [PubMed] [Google Scholar]
- 3.Draper BM. Suicidal behaviour and suicide prevention in later life. Maturitas. 2014;79(2):179–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raue PJ, Ghesquiere AR, Bruce ML. Suicide risk in primary care: identification and management in older adults. Curr Psychiatry Rep. 2014;16(9):466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiosses DN, Szanto K, Alexopoulos GS. Suicide in older adults: the role of emotions and cognition. Curr Psychiatry Rep. 2014;16(11):495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramirez J Suicide: Across the Life Span. Nurs Clin North Am. 2016;51(2):275–286. [DOI] [PubMed] [Google Scholar]
- 7.Ponte C, Almeida V, Fernandes L. Suicidal ideation, depression and quality of life in the elderly: study in a gerontopsychiatric consultation. The Spanish journal of psychology. 2014;17:E14. [DOI] [PubMed] [Google Scholar]
- 8.Park JI, Han MI, Kim MS, et al. Predictors of suicidal ideation in older individuals receiving home-care services. Int J Geriatr Psychiatry. 2014;29(4):367–376. [DOI] [PubMed] [Google Scholar]
- 9.Kang HJ, Stewart R, Jeong BO, et al. Suicidal ideation in elderly Korean population: a two-year longitudinal study. Int Psychogeriatr. 2014;26(1):59–67. [DOI] [PubMed] [Google Scholar]
- 10.Handley TE, Hiles SA, Inder KJ, et al. Predictors of suicidal ideation in older people: a decision tree analysis. Am J Geriatr Psychiatry. 2014;22(11):1325–1335. [DOI] [PubMed] [Google Scholar]
- 11.Han B, McKeon R, Gfroerer J. Suicidal ideation among community-dwelling adults in the United States. Am J Public Health. 2014;104(3):488–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SU, Oh IH, Jeon HJ, Roh S. Suicide rates across income levels: Retrospective cohort data on 1 million participants collected between 2003 and 2013 in South Korea. Journal of epidemiology / Japan Epidemiological Association. 2017;27(6):258–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pompili M, Vichi M, Qin P, Innamorati M, De Leo D, Girardi P. Does the level of education influence completed suicide? A nationwide register study. J Affect Disord. 2013;147(1-3):437–440. [DOI] [PubMed] [Google Scholar]
- 14.Terranova C, Cardin F, Bruttocao A, Militello C. Analysis of suicide in the elderly in Italy. Risk factors and prevention of suicidal behavior. Aging clinical and experimental research. 2012;24(3 Suppl):20–23. [PubMed] [Google Scholar]
- 15.Hottes TS, Bogaert L, Rhodes AE, Brennan DJ, Gesink D. Lifetime Prevalence of Suicide Attempts Among Sexual Minority Adults by Study Sampling Strategies: A Systematic Review and Meta-Analysis. Am J Public Health. 2016;106(5):e1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wiktorsson S, Rydberg Sterner T, Mellqvist Fassberg M, et al. Few Sex Differences in Hospitalized Suicide Attempters Aged 70 and Above. International journal of environmental research and public health. 2018;15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zullig KJ, Divin AL, Weiler RM, Haddox JD, Pealer LN. Adolescent Nonmedical Use of Prescription Pain Relievers, Stimulants, and Depressants, and Suicide Risk. Subst Use Misuse. 2015;50(13):1678–1689. [DOI] [PubMed] [Google Scholar]
- 18.Juan W, Jian-Xiong D, Lan G, et al. Non-medical use of psychoactive drugs in relation to suicide tendencies among Chinese adolescents. Addict Behav. 2015;51:31–37. [DOI] [PubMed] [Google Scholar]
- 19.Guo L, Xu Y, Deng J, et al. Association Between Nonmedical Use of Prescription Drugs and Suicidal Behavior Among Adolescents. JAMA pediatrics. 2016;170(10):971–978. [DOI] [PubMed] [Google Scholar]
- 20.Ford JA, Perna D. Prescription drug misuse and suicidal ideation: Findings from the National Survey on Drug Use and Health. Drug Alcohol Depend. 2015;157:192–196. [DOI] [PubMed] [Google Scholar]
- 21.Kuramoto SJ, Chilcoat HD, Ko J, Martins SS. Suicidal ideation and suicide attempt across stages of nonmedical prescription opioid use and presence of prescription opioid disorders among U.S. adults. J Stud Alcohol Drugs. 2012;73(2):178–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ashrafioun L, Bishop TM, Conner KR, Pigeon WR. Frequency of prescription opioid misuse and suicidal ideation, planning, and attempts. J Psychiatr Res. 2017;92:1–7. [DOI] [PubMed] [Google Scholar]
- 23.West NA, Severtson SG, Green JL, Dart RC. Trends in abuse and misuse of prescription opioids among older adults. Drug and Alcohol Dependence. 2015;149:117–121. [DOI] [PubMed] [Google Scholar]
- 24.Paulozzi LJ, Strickler GK, Kreiner PW, Koris CM. Controlled Substance Prescribing Patterns--Prescription Behavior Surveillance System, Eight States, 2013. Morbidity and mortality weekly report Surveillance summaries (Washington, DC : 2002). 2015;64(9):1–14. [DOI] [PubMed] [Google Scholar]
- 25.Schepis TS, Teter CJ, Simoni-Wastila L, McCabe SE. Prescription tranquilizer/sedative misuse prevalence and correlates across age cohorts in the US. Addict Behav. 2018;87:24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Journal of the American Geriatrics Society. 2015;63(11):2227–2246. [DOI] [PubMed] [Google Scholar]
- 27.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maree RD, Marcum ZA, Saghafi E, Weiner DK, Karp JF. A Systematic Review of Opioid and Benzodiazepine Misuse in Older Adults. Am J Geriatr Psychiatry. 2016;24(11):949–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shearer SL, Peters CP, Quaytman MS, Wadman BE. Intent and lethality of suicide attempts among female borderline inpatients. Am J Psychiatry. 1988;145(11):1424–1427. [DOI] [PubMed] [Google Scholar]
- 30.Oquendo MA, Placidi GP, Malone KM, et al. Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Arch Gen Psychiatry. 2003;60(1):14–22. [DOI] [PubMed] [Google Scholar]
- 31.Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health public use file codebook. In. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 32.Center for Behavioral Health Statistics and Quality. 2016 National Survey on Drug Use and Health: Methodological summary and definitions. In. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017. [Google Scholar]
- 33.Substance Abuse and Mental Health Services Administration. Reliability of Key Measures in the National Survey on Drug Use and Health (Office of Applied Studies, Methodology Series M-8, HHS Publication No. SMA 09-4425). In. Rockville, MD: 2010. [PubMed] [Google Scholar]
- 34.Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health: 2014 and 2015 Redesign Changes. In. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [PubMed] [Google Scholar]
- 35.Conwell Y Suicide later in life: challenges and priorities for prevention. Am J Prev Med. 2014;47(3 Suppl 2):S244–250. [DOI] [PubMed] [Google Scholar]
- 36.Van Orden KA, Wiktorsson S, Duberstein P, Berg AI, Fassberg MM, Waern M. Reasons for attempted suicide in later life. Am J Geriatr Psychiatry. 2015;23(5):536–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 38.Zanarini MC, Frankenburg FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Compr Psychiatry. 2001;42(5):369–374. [DOI] [PubMed] [Google Scholar]
- 39.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. [DOI] [PubMed] [Google Scholar]
- 40.Colpe LJ, Epstein JF, Barker PR, Gfroerer JC. Screening for serious mental illness in the National Survey on Drug Use and Health (NSDUH). Ann Epidemiol. 2009;19(3):210–211. [DOI] [PubMed] [Google Scholar]
- 41.Novak SP, Colpe LJ, Barker PR, Gfroerer JC. Development of a brief mental health impairment scale using a nationally representative sample in the USA. Int J Methods Psychiatr Res. 2010;19 Suppl 1:49–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6(2):327–348. [DOI] [PubMed] [Google Scholar]
- 43.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. British journal of addiction. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 44.Rust K Variance estimation for complex estimators in sample surveys. Journal of Official Statistics. 1985;1(4):381. [Google Scholar]
- 45.Yansaneh IS. Estimation of sampling errors for complex survey data. In. New York, NY: United Nations Secretariat, Statistics Division; 2003. [Google Scholar]
- 46.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York: Wiley; 2000. [Google Scholar]
- 47.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. American journal of epidemiology. 1989;129(1):125–137. [DOI] [PubMed] [Google Scholar]
- 48.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code for Biology and Medicine. 2008;3:17–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Varney SM, Perez CA, Arana AA, et al. Detecting aberrant opioid behavior in the emergency department: a prospective study using the screener and Opioid Assessment for Patients with Pain-Revised (SOAPP((R))-R), Current Opioid Misuse Measure (COMM), and provider gestalt. Internal and emergency medicine. 2018. [DOI] [PubMed] [Google Scholar]
- 50.O’Malley PM, Bachman JG, Johnston LD. Reliability and consistency in self-reports of drug use. International Journal of Addiction. 1983;18:805–824. [DOI] [PubMed] [Google Scholar]
- 51.Johnston LD, O’Malley PM. Issues of validity and population coverage in student surveys of drug use. NIDA Research Monograph. 1985;57:31–54. [PubMed] [Google Scholar]
- 52.Center for Behavioral Health Statistics and Quality. National Survey on Drug Use and Health (NSDUH): Summary of Methodological Studies, 1971-2014. In. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [PubMed] [Google Scholar]
- 53.Center for Behavioral Health Statistics and Quality. 2014 National Survey on Drug Use and Health: Methodological summary and definitions. In. Rockville, MD:: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- 54.Cunningham D, Flicker L, Murphy J, Aldworth J, Myers S, Kennet J. Incidence and Impact of Controlled Access Situations on Nonresponse. American Association for Public Opinion Research 60th Annual Conference; 2015; Miami Beach, FL. [Google Scholar]
- 55.Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. International Psychogeriatrics. 2010;22(7):1025–1039. [DOI] [PubMed] [Google Scholar]
- 56.Mezuk B, Rock A, Lohman MC, Choi M. Suicide risk in long-term care facilities: A systematic review. International journal of geriatric psychiatry. 2014;29(12):1198–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]