Abstract
Objective
This study aimed to evaluate the effect of non-surgical periodontal therapy on the fibrinogen levels in chronic periodontitis patients when compared to the levels seen in healthy subjects.
Materials and methods
A total of 30 subjects, with an average age of 38 ± 25 years, were enrolled in the present study. They were divided into two groups, namely Group 1 (15 periodontally healthy subjects) and Group 2 (15 moderate to severe chronic periodontitis patients). The periodontal condition of each periodontitis patient was assessed by recording the probing pocket depth (PD), clinical attachment level (CAL), plaque index (PI), and bleeding index (BI) both before and after periodontal therapy had been administered for one month. Additionally, blood samples were collected from the healthy subjects and the periodontitis patients before and after the periodontal treatment in order to assay the plasma fibrinogen levels.
Results
The clinical parameters were found to be improved after one month of periodontal therapy, with the statistical difference in the mean values of the BI and PD being highly significant (P < 0.01), while the statistical differences concerning the PI and CAL were significant (P < 0.05). The fibrinogen levels (mg/dL) for the periodontitis patients before and after treatment were 342.26 ± 69.00 and 352.93 ± 64.3 mg/dL, respectively. The level was 269.85 ± 43.68 mg/dL for the healthy subjects. In terms of the between-group comparison, the fibrinogen levels of the healthy subjects were observed to be highly significantly lower than the levels of the periodontitis patients before and after the treatment (P < 0.01), in contrast the statistical analysis showed a non-significant difference in the fibrinogen levels (P > 0.05) before and after the periodontal treatment. In addition, the statistical analysis revealed non-significant correlation between the fibrinogen levels and all the periodontal parameters (P > 0.05).
Conclusion
The non-surgical periodontal therapy proved to be effective in improving the clinical periodontal condition of the periodontitis patients, while the plasma fibrinogen levels were not found to be influenced by the periodontal therapy. Further studies are needed to evaluate the fibrinogen levels over a longer duration after periodontal treatment in patients following a periodontal maintenance program.
Keywords: Fibrinogen, Chronic periodontitis, Periodontal therapy
1. Introduction
Chronic periodontitis is an inflammatory disease that occurs due to an imbalance between the host’s immune defense and specific periodontal pathogens. The disease is characterized by inflammation and the long-term destruction of the periodontal supporting tissue (Kornman and Kenneth, 2008). If the inflammation is left untreated, bacterial infiltration will increase and the resultant destruction of both the supporting tissue and the alveolar bone will likely lead to a deep periodontal pocket, which is associated with an increase in tooth loss (Hernandez et al., 2011, Matuliene et al., 2008). There are many species of bacteria associated with chronic periodontitis, for example, Treponema denticola, Porphyromonas gingivalis and Prevotella intermedia (Loesche et al., 2001).
The level of chronic periodontitis can be classified as either mild, moderate, or severe. Mild periodontitis involves only slight bone loss and a 1–2 mm clinical attachment loss (CAL), while moderate periodontitis involves a greater degree of bone loss and a 3–4 mm CAL. In the case of severe periodontitis, the progression of the disease results in the severe destruction of the tooth-supporting structures and a ≥ 5 mm CAL (Armitage, 1999).
Fibrinogen is synthesized in the liver (Marucco et al., 2013), and its typical concentration in the blood plasma is approximately 2.5 g/l (Erickson, 2009). Fibrinogen plays an essential role within the body, since it is part of the acute-phase protein that becomes elevated following tissue inflammation or tissue destruction, and it also serves to increase the production of cytokines. Further, it is involved in the standard pathway of the coagulation process (Kamath and Lip, 2003, Pagana, 1998). More specifically, fibrinogen converts blood clots into fibrin by means of the thrombin enzyme, which is triggered by both tissue injury and platelet activation. Fibrin molecules can clump together in order to form a solid clot, which suggests that an increase in the level of fibrinogen may pose a risk in cases of cardiovascular disease (Kweider et al., 1993, Pagana, 1998, Van der Bom et al., 1997).
When a bacterial invasion of the periodontal pocket occurs, the epithelial lining of the pocket experiences inflammation. As a result, the immune response initiates the production of inflammatory cytokines, which in turn prompts the liver to produce acute-phase proteins, including fibrinogen and C-reactive protein (Radafshar et al., 2010).
Several studies have confirmed the relationship between periodontal disease and an increased level of fibrinogen in chronic periodontitis patients when compared to healthy subjects (Ana et al., 2013, Brown et al., 1990, Chandy et al., 2017, Tripathi, 2014, Wu et al., 2000). Moreover, Humphrey et al. (2009) reported the association between a patient’s periodontal health status and certain cardiovascular risk factors, namely C-reactive protein and plasma fibrinogen. They concluded that a significant relationship exists between the indicators of poor periodontal health and increased levels of both C-reactive protein and fibrinogen. Additionally, patients with periodontal disease have been found to exhibit increased fibrinogen and white blood cell levels (Christan et al., 2002, Kweider et al., 1993).
Previous studies have shown the effectiveness of non-surgical periodontal therapy in terms of decreasing the fibrinogen levels after treatment when compared to the baseline levels (Bresolin et al., 2014, Ertugrul et al., 2017, Itam and Jyoti, 2013, Rai et al., 2009, Vidal et al., 2009). However, some researchers have reported that the fibrinogen levels are not decreased after periodontal therapy (Ide et al., 2003, Ellis et al., 2007, Mattila et al., 2002, Montebugnoli et al., 2005, Radafshar et al., 2010).
Due to these inconsistent findings, the present study aimed to assess the levels of fibrinogen in patients with chronic periodontitis when compared to the levels seen in healthy subjects, as well as to evaluate the effect of periodontal therapy on the fibrinogen levels in chronic periodontitis patients before and after treatment. Moreover, the study aimed to correlate the fibrinogen level with various clinical parameters in systemically healthy chronic periodontitis patients.
2. Materials and methods
2.1. Study design
The present study was an interventional controlled clinical trial in which the subjects were examined in the Department of Periodontology of the Teaching Hospital of the Dental College at Umm Alqura University. In terms of the inclusion criteria, the subjects were required to be systemically healthy according to the Cornell Medical Index (Brodman et al., 1951), non-smokers, and non-pregnant women. All the periodontitis patients involved in the study had moderate to severe chronic periodontitis (CAL ≥ 3–5 mm). A total of 30 individuals (mean age of 38 ± 25 years) were enrolled in the study. They were divided into two groups. Group 1 was the healthy control group, and it comprised 15 subjects aged between 20 and 40 years old. Group 2 was the chronic periodontitis group, and it comprised 15 patients aged between 25 and 50 years old.
2.2. Periodontal examination
The periodontal condition of each patient was ascertained using a number of clinical parameters, namely the probing pocket depth (PD), clinical attachment level (CAL) (Ramfjord et al., 1968), plaque index (PI) (O’Leary et al., 1972), and bleeding index (BI) (Carter et al., 1974). All the parameters were measured both before and after the periodontal treatment.
2.3. Periodontal therapy
The non-surgical periodontal therapy was performed for each patient after their clinical parameters had been measured. The therapy process included the removal of the supragingival and subgingival calculus using an ultrasonic device and Gracey curettes over the course of two visits to the dental hospital. Additionally, the patients were motivated and advised regarding suitable oral hygiene techniques, such as using a toothbrush three times per day and other cleaning measures.
2.4. Blood samples
Five milliliters (ml) of peripheral blood were collected from both the healthy subjects and the chronic periodontitis patients before and after the treatment. The blood samples were transferred into tubes containing an anticoagulant (sodium citrate). To achieve the separation of the plasma sample, the tubes were centrifuged at 3000 rpm for 12 min. Half an hour after the collection, the plasma samples were separated in Eppendorf tubes and then stored at −80 °C until they were analyzed.
2.5. Assaying the fibrinogen levels
The Clauss fibrinogen assay was performed according to the standard operating procedures (Clauss, 1957). A clotting reaction was initiated by means of the addition of a thrombin reagent, and the time required for clot formation was measured. The coagulation signal was detected using a photo-optical method. The time required for clot formation (in seconds) was converted into the fibrinogen concentration (mg/dL) according to a local standard calibration curve prepared by testing the calibrators of each Clauss assay according to the manufacturer’s instructions.
2.6. Follow up
The patients came after four weeks for follow up of periodontal therapy, the previous steps were performed to them again.
2.7. Statistical analysis
All the collected data were analyzed using the SPSS version 21 software program. The descriptive analysis included the minimum, maximum, mean, range, and standard deviation of the data. Student’s t-test was used to compare between the groups, as was Spearmen's correlation test. The data were tabulated and graphed using Microsoft’s program.
3. Results
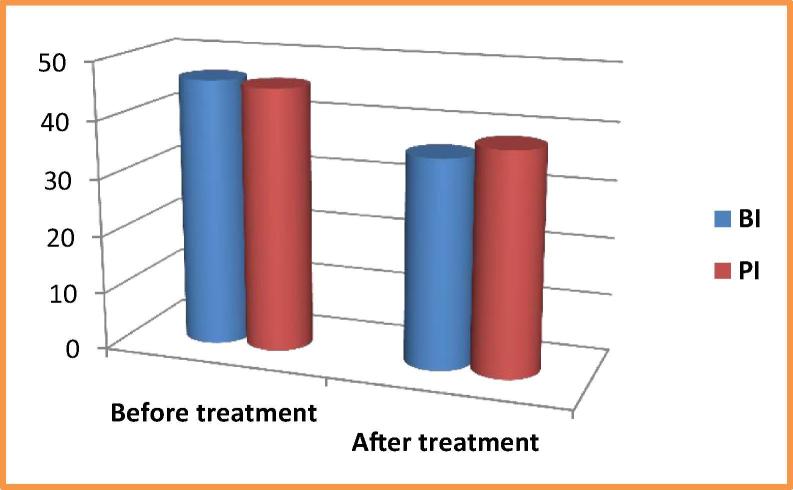
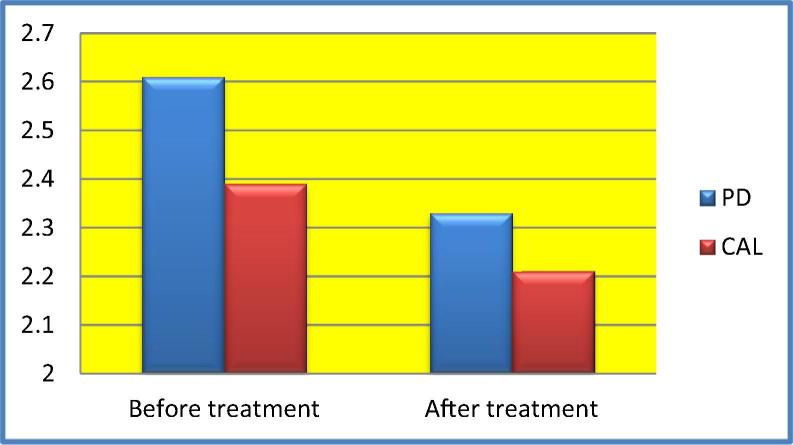
With regard to the periodontitis patients, the clinical parameters were improved after one month of periodontal therapy. The statistical differences for the mean BI and PD values were highly significant (P < 0.01), while the statistical differences for the mean PI and CAL values were significant (P < 0.05). The results are illustrated in Table 1, as well as in Fig. 1, Fig. 2.
Table 1.
Comparison of the clinical parameters (bleeding index [BI], plaque index [PI], pocket depth [PD], and clinical attachment level [CAL]) in the periodontitis group.
| Mean | SD | T-test | P value | ||
|---|---|---|---|---|---|
| BI | Before | 46.34 | 14.20 | 3.570 | 0.003** |
| After | 36.04 | 15.22 | |||
| PI | Before | 45.64 | 16.20 | 2.484 | 0.026* |
| After | 38.27 | 13.18 | |||
| PD | Before | 2.61 | 0.621 | 3.205 | 0.006** |
| After | 2.33 | 0.480 | |||
| CAL | Before | 2.39 | 0.517 | 2.703 | 0.017* |
| After | 2.21 | 0.530 | |||
Significant (P < 0.05).
Highly significant (P ≤ 0.01).
Fig. 1.
Demonstration of the mean plaque and bleeding index values among the chronic periodontitis patients.
Fig. 2.
Demonstration of the mean pocket depth and clinical attachment level values among the chronic periodontitis patients.
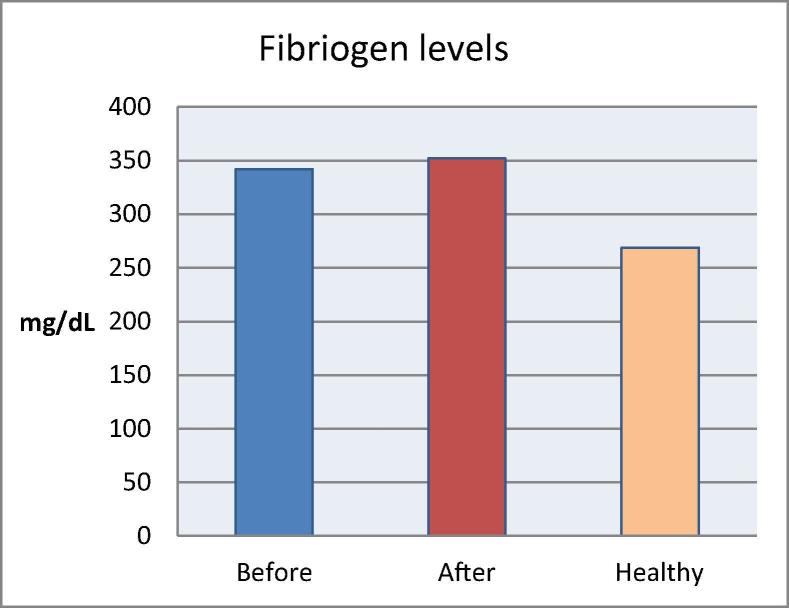
The mean fibrinogen levels were found to be 342.26 ± 69.00 mg/dL and 352.93 ± 64.30 mg/dL for the periodontitis patient’s before and after treatment, respectively. The mean level was found to be 269.85 ± 43.68 mg/dL for the healthy subjects. The statistical analysis showed a non-significant difference between the before and after fibrinogen levels of the patient group (P > 0.05), as well as highly significant differences in the fibrinogen levels when comparing the healthy subjects and the periodontitis patients before and after treatment (P < 0.01). The results can be seen in Table 2, Table 3, as well as in Fig. 3.
Table 2.
Plasma levels of the fibrinogen baseline, follow-up, and control group.
| Patient | Fibrinogen (mg/dL) |
||
|---|---|---|---|
| Pre intervention | Post intervention | Healthy group | |
| 1 | 326.00 | 224.00 | 323.80 |
| 2 | 408.00 | 392.00 | 330.00 |
| 3 | 224.00 | 344.00 | 240.00 |
| 4 | 304.00 | 236.00 | 270.00 |
| 5 | 366.00 | 388.00 | 266.40 |
| 6 | 408.00 | 424.00 | 311.00 |
| 7 | 394.00 | 370.00 | 247.00 |
| 8 | 368.00 | 332.00 | 259.10 |
| 9 | 214.00 | 418.00 | 283.00 |
| 10 | 306.00 | 434.00 | 175.20 |
| 11 | 340.00 | 298.00 | 294.00 |
| 12 | 396.00 | 364.00 | 319.00 |
| 13 | 460.00 | 385.00 | 281.70 |
| 14 | 340.00 | 386.00 | 209.00 |
| 15 | 280.00 | 299.00 | 238.60 |
Table 3.
Statistical analysis of the fibrinogen levels (mg/dL) in the different examined groups.
| Fibrinogen levels | Mean ± SD | T-test | P value |
|---|---|---|---|
| Before treatment | 342.26 ± 69.00 | 0.490 | 0.632 |
| After treatment | 352.93 ± 64.30 | ||
| Before treatment | 342.26 ± 69.00 | 4.207 | 0.001** |
| Healthy | 269.85 ± 43.68 | ||
| After treatment | 352.93 ± 64.30 | 3.749 | 0.002** |
| Healthy | 269.85 ± 43.68 |
Highly significant (P < 0.01).
Fig. 3.
The mean fibrinogen values in the healthy and periodontitis groups.
The statistical analysis of the Pearson’s correlation between the fibrinogen levels and the various clinical periodontal parameters before and after treatment indicated non-significant correlation (P > 0.05), as can be seen in Table 4.
Table 4.
Correlation between the fibrinogen levels and the periodontal parameters.
| Fibrinogen level | BI | PI | PD | CAL | |
|---|---|---|---|---|---|
| Before treatment | Pearson′s correlation sig. (two-tailed) | 0.029 | 0.006 | 0.285 | 0.453 |
| 0.920 | 0.983 | 0.303 | 0.090 | ||
| After treatment | Pearson′s correlation sig. (two-tailed) | 0.163 | 0.259 | 0.285 | 0.324 |
| 0.563 | 0.352 | 0.302 | 0.239 |
4. Discussion
Periodontal disease is associated with a moderate systemic inflammatory response, while increased levels of fibrinogen are considered to indicate a high risk of cardiovascular disease (Loos et al., 2000). The present study hence aimed to evaluate the fibrinogen levels in moderate to severe chronic periodontitis patients both before and after periodontal therapy, as well as to compare the levels with those of periodontally healthy subjects.
The assessed clinical parameters (PI, PD, CAL, and BI) were found to be improved after the non-surgical periodontal therapy. These findings were in agreement with those of previous studies (Bresolin et al., 2014, Radafshar et al., 2010). For instance, a prospective interventional trial conducted among 35 systemically healthy subjects indicated an improvement in the assessed periodontal parameters after four months of follow-up. This finding was similar to the finding of Taylor et al. (2010), who also showed an improvement in the clinical parameters after three months of follow-up, which was again similar to previously reported findings (Ritam and Jyoti, 2013, Tripathi, 2014, Vidal et al., 2009).
This study aimed to clarify the potential effect of periodontal treatment in terms of modulating the fibrinogen levels in periodontitis patients, as well as to interpret the impact of periodontitis on patients’ systemic inflammatory status. Some prior studies have investigated the efficacy of periodontal therapy in relation to fibrinogen as a systemic inflammatory marker (Bresolin et al., 2014, Ritam and Jyoti, 2013, Tripathi, 2014, Vidal et al., 2009).
The findings of this study indicated that the chronic periodontitis group exhibited a higher mean fibrinogen level (342.26 ± 69.00 mg/dL) than the healthy group (269.85 ± 43.68 mg/dL). The observed difference was found to be statistically significant (P ≤ 0.01), in addition to being in agreement with certain prior studies that reported an association between the fibrinogen level and the severity of the periodontitis disease. For instance, Ana et al. (2013) reported that an increased level of the inflammatory marker correlated with the severity of the periodontitis, while Sahingur et al. (2003) found that the H1H2 and H2H2 genotypes played a role in the increased level of fibrinogen seen in chronic periodontitis patients (Brown et al., 1990, Chandy et al., 2017, Tripathi, 2014, Wu et al., 2000). The above-mentioned results and the supporting literature thus indicate that periodontitis may play a role in increasing the fibrinogen levels of patients.
The statistical analysis of the difference in the fibrinogen levels before treatment (342.26 ± 69.00 mg/dL) and after treatment (352.93 ± 64.30 mg/dL) indicated that the difference was non-significant, which was similar to the finding of a previously reported study (Montebugnoli et al., 2005). That study involved 18 patients with chronic periodontitis, and the authors reported that the mean fibrinogen level did not decrease after four months of non-surgical periodontal therapy (Montebugnoli et al., 2005). This was again similar to the finding of Ide et al. (2003), who studied the effect of periodontal therapy on the inflammatory marker. They found a non-significant decrease in the fibrinogen level as measured after six weeks of periodontal therapy. This finding is also consistent with the results of other reported studies (Ellis et al., 2007, Mattila et al., 2002, Radafshar et al., 2010).
However, the fibrinogen levels after the periodontal therapy in this study were found to be significantly decreased when compared to the pre-treatment levels. Ritam et al. (2013) performed a study on 40 healthy adult patients who had chronic periodontitis, and they showed a decrease in the improvement in the fibrinogen level after four months of periodontal treatment, which was similar to the findings of a number of other reports (Bresolin et al., 2014, Ertugrul et al., 2017, Itam and Jyoti, 2013, Rai et al., 2009, Taylor et al., 2010, Vidal et al., 2009). Ritam et al. (2013) commented that the periodontal therapy could play a role in decreasing systemic inflammatory markers, such as fibrinogen, and improving the patient’s systemic health condition. Their conclusions differ from our findings, which could be due to the short evaluation time after treatment or the low sample size in the present study.
The statistical analysis conducted in the present study revealed non-significant correlation between the fibrinogen level and the assessed clinical periodontal parameters, although this observation contrasts with the results obtained by Chandy et al. (2017). Their results indicated a weak relationship between the fibrinogen level and the indices of periodontitis.
5. Conclusion
This study showed that both the oral health condition and periodontal therapy are essential to patients’ systemic health. Further, both factors decrease the potential impact of oral microorganisms, which can be a risk factor for the progression of certain systemic disorders. With regard to fibrinogen, further studies involving larger population samples are needed to evaluate the efficacy of periodontal treatment in terms of decreasing fibrinogen levels over an extended period.
Conflict of interest
There is no conflict with others research workers.
Ethical approval
The article ethical approved from IRB Committee of Collage Dentistry Umm AlQura University under number (70-17) at 8th January 2018.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgement
The author highly appreciate the valuable input from Dr. Hussain Alessa and Dr. Abdulrahman Yousef during the experimental work and within the preparation of this manuscript.
Footnotes
Peer review under responsibility of King Saud University.
References
- Ana P., Dimitrije M., Draginja K., Ivan M., Mariola S. The markers of systemic inflammation in patients with chronic periodontitis: Leukocytes, C-reactive protein, and fibrinogen. J. Prevent. Med. 2013;1(3):43–49. [Google Scholar]
- Armitage G.C. Development of a classification system for periodontal diseases and conditions. Ann. Periodontol. 1999;4(1):1–6. doi: 10.1902/annals.1999.4.1.1. [DOI] [PubMed] [Google Scholar]
- Bresolin A.C., Pasqualotto L.N., Pronsatti M.M., Nassar P.O., Jorge A.S., da Silva E.A.A., Nassar C.A. The effectiveness of periodontal treatment on the improvement of inflammatory markers in children. Arch. Oral Biol. 2014;59(6):639–644. doi: 10.1016/j.archoralbio.2014.03.010. [DOI] [PubMed] [Google Scholar]
- Brodman K., Lorge I., Erdmann A.J., Wolff H.G., Broadbent T.H. The Cornell medical index-health questionnaire: II. As a diagnostic instrument. J. Am. Med. Assoc. 1951;145(3):152–157. doi: 10.1001/jama.1951.02920210024006. [DOI] [PubMed] [Google Scholar]
- Brown R.C.O., Jackson L., Loe H. Evaluating periodontal status of US employed adults. J. Am. Dent. Assoc. 1990;121(2):226–232. doi: 10.14219/jada.archive.1990.0252. [DOI] [PubMed] [Google Scholar]
- Carter H.G., Barnes G.P. The gingival bleeding index. J. Periodontol. 1974;45(11):801–805. doi: 10.1902/jop.1974.45.11.801. [DOI] [PubMed] [Google Scholar]
- Chandy S., Joseph K., Sankaranarayanan A., Issac A., Babu G., Wilson B., Joseph J. Evaluation of C-reactive protein and fibrinogen in patients with chronic and aggressive periodontitis: a clinico-biochemical study. J. Clin. Diagnostic Res. 2017;11(3):41–45. doi: 10.7860/JCDR/2017/23100.9552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christan C., Hägewald S., Kage A., Dietrich T., Bernimoulin J.P. White blood cell count in generalized aggressive periodontitis after non-surgical therapy. J. Clin. Periodontol. 2002;29(3):201–206. doi: 10.1034/j.1600-051x.2002.290303.x. [DOI] [PubMed] [Google Scholar]
- Clauss A. Rapid physiological coagulation method in determination of fibrinogen. Acta Haematologica. 1957;17(4):237–246. doi: 10.1159/000205234. [DOI] [PubMed] [Google Scholar]
- Ellis J.S., Averley P.A., Preshaw P.M., Steele J.G., Seymour R.A., Thomason J.M. Change in cardiovascular risk status after dental clearance. Br. Dent. J. 2007;202(9):543–544. doi: 10.1038/bdj.2007.373. [DOI] [PubMed] [Google Scholar]
- Erickson H.P. Size and shape of protein molecules at the nanometer level determined by sedimentation, gel filtration, and electron microscopy. Biol. Proc. Online. 2009;11(1):32–51. doi: 10.1007/s12575-009-9008-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertugrul A.S., Taspınar M., Bozoglan A. The effect of non-surgical periodontal treatment on serum and gingival crevicular fluid markers in patients with atherosclerosis. Nigerian J. Clin. Pract. 2017;20(3):361–368. doi: 10.4103/1119-3077.181369. [DOI] [PubMed] [Google Scholar]
- Humphrey L.L., Freeman M., Fu R., Buckley D.I., Helfand M. Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J. Gen. Intern. Med. 2008;23(12):2079–2086. doi: 10.1007/s11606-008-0787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez M., Abusleme L., García-Sesnich J., Dutzan N., Dezerega A., Silva N., Gamonal J. Host-pathogen interactions in progressive chronic periodontitis. J. Dent. Res. 2011;90(10):1164–1170. doi: 10.1177/0022034511401405. [DOI] [PubMed] [Google Scholar]
- Itam S.N., Jyoti R.R. Effect of periodontal treatment on plasma fibrinogen, serum C-reactive protein and total white blood cell count in periodontitis patients: A prospective interventional trial. Rom. J. Intern. Med. 2013;51(1):45–51. [Google Scholar]
- Kamath S., Lip G.Y.H. Fibrinogen: Biochemistry, epidemiology, and determinants. QJM. 2003;96(10):711–729. doi: 10.1093/qjmed/hcg129. [DOI] [PubMed] [Google Scholar]
- Kornman K.S. Mapping the pathogenesis of periodontitis: a new look. J. Periodontol. 2008;79(8S):1560–1568. doi: 10.1902/jop.2008.080213. [DOI] [PubMed] [Google Scholar]
- Kweider M., Kinane D.F., Lowe G.D.O., Murray G.D., McGowan D.A. Dental disease, fibrinogen and white cell count: Links with myocardial infarction? Scott. Med. J. 1993;38(3):73–74. doi: 10.1177/003693309303800304. [DOI] [PubMed] [Google Scholar]
- Ide M., McPartlin D., Coward P.Y., Crook M., Lumb P., Wilson R.F. Effect of treatment of chronic periodontitis on levels of serum markers of acute-phase inflammatory and vascular responses. J. Clin. Periodontol. 2003;30(4):334–340. doi: 10.1034/j.1600-051x.2003.00282.x. [DOI] [PubMed] [Google Scholar]
- Loesche W.J., Grossman N.S. Periodontal disease as a specific, albeit chronic, infection: Diagnosis and treatment. Clin. Microbiol. Rev. 2001;14(4):727–752. doi: 10.1128/CMR.14.4.727-752.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loos B.G., Craandijk J., Dillen P.M.W.V., Hoek F.J., Velden U.V.D. Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. J. Periodontol. 2000;71(10):1528–1534. doi: 10.1902/jop.2000.71.10.1528. [DOI] [PubMed] [Google Scholar]
- Marucco A., Turci F., Fenoglio I., Fubini B. Interaction of fibrinogen and albumin with titanium dioxide nanoparticles of different crystalline phases. J. Phys. 2013;429(1):1–10. [Google Scholar]
- Mattila K., Valtonen V., Vesanen M., Nieminen M., Palosuo T., Rasi V., Asikainen S. Effect of treating periodontitis on C-reactive protein levels: a pilot study. BMC Infect. Dis. 2002;2(1):30–32. doi: 10.1186/1471-2334-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matuliene G., Brägger U., Pjetursson B.E., Salvi G.E., Schmidlin K., Zwahlen M., Lang N.P. Influence of residual pockets on progression of periodontitis and tooth loss: Results after 11 years of maintenance. J. Clin. Periodontol. 2008;35(8):685–695. doi: 10.1111/j.1600-051X.2008.01245.x. [DOI] [PubMed] [Google Scholar]
- Montebugnoli L., Servidio D., Miaton R.A., Prati C., Tricoci P., Melloni C., Melandri G. Periodontal health improves systemic inflammatory and haemostatic status in subjects with coronary heart disease. J. Clin. Periodontol. 2005;32(2):188–192. doi: 10.1111/j.1600-051X.2005.00641.x. [DOI] [PubMed] [Google Scholar]
- O’Leary T.J., Drake R.B., Naylor J.E. The plaque control record. J. Periodontol. 1972;43(1):38. doi: 10.1902/jop.1972.43.1.38. [DOI] [PubMed] [Google Scholar]
- Pagana K.D. Manual of diagnostic and laboratory tests. St. Louis; Mosby, Inc. Proc. Soc. Exp. Biol. Med. 1998;90:210–213. [Google Scholar]
- Radafshar G., Ariamajd E., Shad B., Geranmayeh S. Effect of intensive non-surgical treatment on the level of serum inflammatory markers in advanced periodontitis. J. Dentistry (Tehran, Iran) 2010;7(1):24–30. [PMC free article] [PubMed] [Google Scholar]
- Rai B., Kharb S., Jain R., Anand S.C. Periodontitis, C-reactive protein, and peripheral blood: links with cardiovascular disease. Adv. Med. Dent. Sci. 2009:76–80. [Google Scholar]
- Ramfjord S.P., Greene J.C., Emslie R.D., Held A.J., Waerhaug J. Epidemiological studies of periodontal diseases. Am. J. Public Health Nation’s Health. 1968;58(9):1713–1722. doi: 10.2105/ajph.58.9.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritam S.N.T., Jyoti R.R. Effect of periodontal treatment on plasma fibrinogen, serum C-reactive protein and total white blood cell count in periodontitis patients: a prospective interventional trial. Rom. J. Intern. Med. 2013;51(1):45–51. [Google Scholar]
- Sahingur S.E., Genco R.J., Sharma A., De Nardin E. Association of increased levels of fibrinogen and the -455G/A fibrinogen gene polymorphism with chronic periodontitis. J. Periodontol. 2003;74(3):329–337. doi: 10.1902/jop.2003.74.3.329. [DOI] [PubMed] [Google Scholar]
- Tripathi V.D. Estimation of fibrinogen and ESR - hemostatic markers in patients with mild, moderate and severe periodontitis. Indian J. Dental Sci. 2014;6(1):32–36. [Google Scholar]
- Taylor B., Morel-Kopp M.C., Tofler G., Carey H., Carter T., Elliott M., Schenck K. The effect of initial treatment of periodontitis on systemic markers of inflammation and cardiovascular risk: a randomized controlled trial. Eur. J. Oral Sci. 2010;118(4):350–356. doi: 10.1111/j.1600-0722.2010.00748.x. [DOI] [PubMed] [Google Scholar]
- Vidal F., Cordovil I., Figueredo C.M.S., Fischer R.G. Periodontal therapy reduces plasma levels of interleukin-6, C-reactive protein, and fibrinogen in patients with severe periodontitis and refractory arterial hypertension. J. Periodontol. 2009;80(5):786–791. doi: 10.1902/jop.2009.080471. [DOI] [PubMed] [Google Scholar]
- Van der Bom J.G., De Maat M.P.M., Bots M.L., Hofman A., Kluft C., Grobbee D.E. Seasonal variation in fibrinogen in the Rotterdam Study. Thromb. Haemost. 1997;78(01):1059–1062. [PubMed] [Google Scholar]
- Wu T., Falkner K.L., Trevisan M., Dorn J.P., Genco R.J., Sempos C.T. Examination of the relation between periodontal health status and cardiovascular risk factors: Serum total and high-density lipoprotein cholesterol, C-reactive protein, and plasma fibrinogen. Am. J. Epidemiol. 2000;151(3):273–282. doi: 10.1093/oxfordjournals.aje.a010203. [DOI] [PubMed] [Google Scholar]