Abstract
Background
Understanding the socioeconomic impact of chronic GVHD on affected patients is essential to help improve their overall well-being. Using data from the chronic GVHD Consortium, we describe the insurance, employment and financial challenges for these patients and factors associated with being able to work/ go to school and financial burden.
Methods
A 15-item cross-sectional questionnaire designed to measure financial concerns, income, employment and insurance was completed by 190 patients (response rate=68%, 10 centers) enrolled on a multi-center chronic GVHD Consortium Response Measures Validation study. Multivariable logistic regression models examined the factors associated with financial burden and ability to work/ go to school.
Results
Median age of respondents was 56 years and 87% of the patients were White. A higher proportion of non-respondents had lower income before HCT and less than a college degree. All except one patient had insurance. 34% had faced delayed/denied insurance coverage for chronic GVHD treatments. 66% reported financial burden. Patients with financial burden had higher depression/ anxiety and difficulty sleeping. Non-white race, lower mental functioning and lower activity score were associated with a higher likelihood of financial burden. Younger age, early risk disease and higher mental functioning were associated with higher likelihood of being able to work/ go to school.
Conclusions
Significant negative effects on finances were observed in this multi-center cohort of chronic GVHD patients despite health insurance coverage. Future research should investigate potential interventions to provide optimal and affordable care to at-risk patients and prevent long-term adverse financial outcomes in this vulnerable group.
Introduction
Financial hardship as a result of cancer diagnosis and treatment is a well-recognized challenge for patients and healthcare providers and has been shown to be associated with increased distress and poor quality of life.1–4 Several studies have explored financial burden as reflected by decreased income, high out of pocket costs/ medical bills and adverse impact on lifestyle/ treatment due to cost burden of patients who have undergone hematopoietic cell transplantation (HCT), despite a majority of them having insurance coverage.5–8
Chronic graft vs. host disease (GVHD) is an important complication after allogeneic HCT that contributes to the long-term morbidity and mortality from the procedure.9–12 There is a growing concern about the long-term social and financial implications of chronic GVHD because of the need for intense, prolonged medical follow-up/ treatments and impaired functional status preventing return to work.
The multi-institutional cohort of chronic GVHD patients assembled by the North American Chronic GVHD Consortium for the validation of response measures (n=383) provides a valuable and unique opportunity to study these aspects of psychosocial outcomes of chronic GVHD. Understanding the impact of financial burden on people with chronic GVHD can help identify at risk patients, mitigate the distress associated with it, and improve the overall well-being of these patients. The extensive clinical, sociodemographic and patient-reported outcome information collected through the parent study provides a rich context for understanding the financial burden and related issues such as insurance and employment for these patients. We supplemented the data already collected as part of the parent study with a cross-sectional questionnaire to obtain and report information about financial concerns, income, employment and insurance for these patients.
Patients and Methods
Patients:
The Chronic GVHD Consortium Response Measures Validation study is a prospective, multicenter observational study that collects data on a cohort of HCT recipients with chronic GVHD.13 Patients enrolled in the cohort are allogeneic HCT recipients with a diagnosis of chronic GVHD who initiated a new systemic treatment for chronic GVHD within four weeks prior to or after enrollment. Primary disease relapse, or inability to comply with study procedures are exclusion criteria. The protocol was approved by the Institutional Review Board at each site (Fred Hutchinson Cancer Research Center, University of Minnesota, Dana-Farber Cancer Institute, Vanderbilt University, H. Lee Moffitt Cancer Center, Roswell Park Cancer Institute, Cleveland Clinic Foundation, University of British Columbia, M.D. Anderson Cancer Center and Duke University) and all patients on the study provided informed consent in accordance with the Declaration of Helsinki. This analysis includes data from 190 patients who completed cross-sectional survey collecting information regarding financial concerns, household income, employment status, insurance and out-of-pocket expenses. The survey was completed between June 2016 and July 2017 by the enrolled participants at the time of their standard clinic assessment and by some patients as a mailed-in survey since they had already completed their study-related visits on the parent study.
Financial Burden survey
Multiple instruments have been developed to measure financial burden, however, none of them has been validated in the HCT population yet.14–16 For this reason, we developed a 15-item survey (available in appendix) to collect information regarding financial concerns, household income, employment status, insurance and out-of-pocket expenses based on literature review and discussion with investigators on this study. Feedback regarding content and face validity of the survey, ability of the respondent to interpret essential information as well as the time required to read, comprehend, and complete it was collected from a small group of transplant physicians and by piloting it with 3 chronic GVHD patients at Mayo Clinic Arizona.
Study Variables
At enrollment, 3 months, 6 months and 18 months, physicians and patients report standardized information on chronic GVHD organ involvement and symptoms. Chronic GVHD severity according to the NIH Chronic GVHD Consensus was scored using objective criteria for each organ, and summarized to give an overall score of mild, moderate or severe. Standardized questions were given to patients to assess sociodemographic information at the time of study enrollment. Patients recorded their approximate annual family income in the year before the transplant as <$15,000, $15,000-$24,999, $25,000-$49,999, $50,000-$74,999, $75,000$99,999, or ≥$100,000. These were categorized into three groups for analysis: <$25,000 (low), $25,000-$74,999 (medium), or ≥$75,000 (high). Highest grade of education was analyzed as high school or less (grade school, some high school, or high school graduate), some college, college graduate, or post graduate degree. Current work status was analyzed as ability to work or go to school (in school full-time, in school part-time, working full-time, working part-time, unemployed/ looking for work); at home (homemaker, retired) or inability to work or go to school (on medical leave from work, disabled/ unable to work, unemployed). Some variables such as income and work status were reported both at the time of enrollment and at the time of the financial survey.
Patient reported outcomes
Physical and mental functioning
The Short Form Health Survey (SF-36), is a validated 36-item self-report questionnaire, that measures patient-reported health and functioning. The physical component score (PCS) and the mental component score (MCS) are two summary scales.17 The scoring on this survey is norm-based with a general population mean score of 50 and a standard deviation of 10. Higher scores indicate better functional status. The Human Activity Profile (HAP) consists of 94 questions for measuring activity level. Three scores can be obtained from HAP: maximum activity score, adjusted activity score, and modified adjusted activity score (mAAS). Only mAAS was included in our analysis because it excludes activities that are restricted after HCT. Higher scores represent greater physical activity.
Depression/ Anxiety/ Difficulty sleeping
Three validated items from the Lee chronic GVHD Symptom Scale were used to assess self-reported psychological symptoms.18 Specifically, patients reported how much they have been bothered by 1) depression and 2) anxiety and 3) difficulty sleeping in the past month using a 5point scale (ranging from “not at all” to “extremely”). Summary scores were then calculated with a range of 0 to 100; higher scores indicating greater bother.
Financial Burden
Respondents were asked to report out-of-pocket medical (prescriptions, co-payments and deductibles) and non-medical (transportation to the clinic (gas, parking), child-care etc.) expenses over the last 3 months. Financial burden was defined as the following: difficulty paying medical bills, not having enough money at the end of the month, reducing spending on home/ leisure activities, needing assistance for gas, electric bills etc. from utility companies, using retirement savings, borrowing money or selling assets (e.g. house/ car), or declaring bankruptcy. This was a dichotomous outcome and was operationally defined by the patient reporting at least 1 of the above since being diagnosed with chronic GVHD. Perceived reasons for financial challenges were offered for endorsement: losing/ changing insurance, inability of self/ caregiver to return to work/ having to return to a job with lower salary, frequent physician visits and need for multiple medications/ treatment requirements. Resources used to help with financial difficulties were also assessed such as assistance from family/ friends/ fundraisers, help from charitable or non-profit organizations and resources suggested by social workers at transplant centers.
Ability to work/ go to school
Patients were considered as able to go back to work/ school if they reported to being in school or at work part-time or full-time at the time of survey irrespective of what the work status was at the time of enrollment.
Statistical Analysis
Differences between respondents and non-respondents and between those who completed the survey in clinic versus by mail were determined using chi-square tests, Fisher’s exact test, t-tests and the Wilcoxon rank-sum test. Chi-squared tests and t-tests were used to compare the sociodemographic and clinical characteristics between respondents who endorsed financial burden vs. those who did not. A stepwise regression analysis was used to select significant variables to build multivariate models for financial burden, using a p-value threshold < 0.1. The first model only considered baseline factors: age as a continuous variable/ sex/ race/ education level/ disease risk/ graft source and conditioning intensity. A second enhanced model examined chronic GVHD severity at baseline, HCT-comorbidity index, physical and mental functioning (measured by SF-36) and activity level (measured by modified adjusted activity score) closest to survey completion and time from transplant added to the baseline model for their association to financial burden. Because of the collinearity between income and employment with financial burden, we did not include these two variables in the multivariate model but only reported their correlation with it. Assessment of factors associated with being able to return to work/ school was similarly analyzed.
Results
Baseline Characteristics
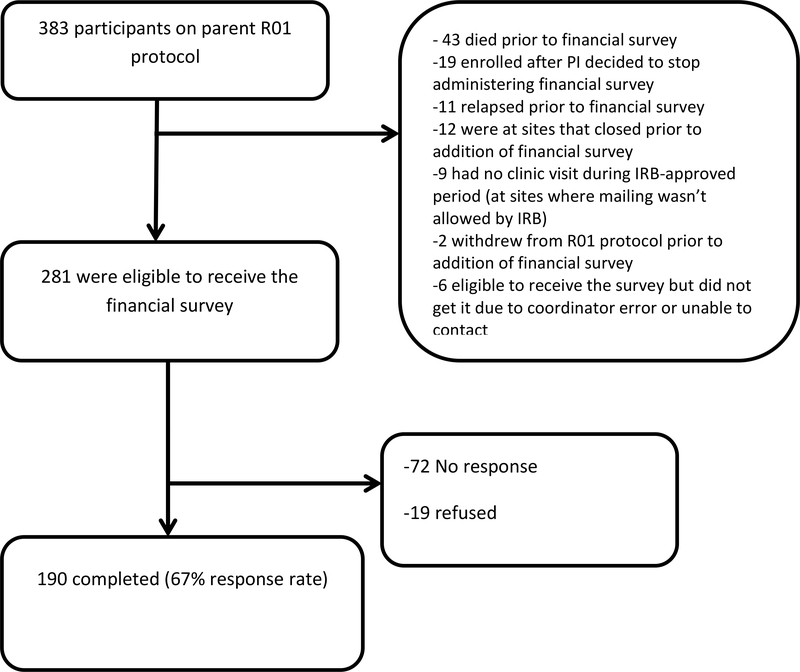
A total of 383 patients were enrolled on the original chronic GVHD consortium protocol out of which 281 were eligible to be surveyed and 190 responded for a response rate of 68%. (Figure 1) Demographic and disease-related characteristics of the respondents (in clinic vs. by mail survey) vs. non-respondents are shown in Table 1. There were no significant differences between non-respondents and respondents except that a higher proportion of non-respondents had lower income before HCT and less than a college degree. Disease distribution and conditioning intensity were different between the respondents who completed the survey in clinic vs. those who completed it by mail. Also, the respondents who completed it by mail were further out from HCT as compared to those completing it in clinic, as expected since mail was used for patients who had completed their study visits. Median age was 56 years (range 12–79) and 87% of the patients were White. Median time from HCT to chronic GVHD onset was 7.5 months and median time from HCT to completion of the financial survey was 2.3 years. Physician reported chronic GVHD severity was mild in 22%, moderate in 53% and severe in 22% respondents. Median physical and mental component scores closest to survey completion (median time 21 days between the survey and SF-36) were 40.3 (range 9–58) and 50.7 (range 9–70), respectively.
Figure 1:
Response flowchart
Table 1:
Baseline Characteristics by Financial Survey response
| Respondents (n=190) | Non-respondents (n=91) | p-value1 | |||
|---|---|---|---|---|---|
| In-Clinic (n=110) n (%) | Mailed (n=80) n (%) | n (%) | Respondents vs. non-respondents | In-Clinic vs. Mailed | |
| Age at enrollment | |||||
| Median (IQR) | 55 (39–63) | 59 (46–65) | 53 (38–62) | 0.13 | 0.06 |
| Patient gender | |||||
| Male | 72 (66) | 52 (65) | 62 (68) | 0.63 | 0.95 |
| Race | 0.18 | 0.17 | |||
| White | 93 (85) | 73 (91) | 74 (81) | ||
| Other | 17 (15) | 7 (9) | 17 (19) | ||
| Disease diagnosis | 0.08 | 0.02 | |||
| Acute Leukemia | 49 (45) | 43 (54) | 36 (40) | ||
| CML/MDS/MPD | 37 (34) | 12 (15) | 18 (20) | ||
| Lymphoma including CLL | 19 (17) | 17 (21) | 25 (28) | ||
| AA/Other | 5 (4) | 8 (11) | 12 (13) | ||
| Disease status | 0.56 | 0.61 | |||
| Early | 50 (45) | 40 (50) | 41 (45) | ||
| Intermediate | 39 (36) | 29 (36) | 38 (42) | ||
| Advanced | 21 (19) | 11 (14) | 12 (13) | ||
| Stem cell source | 0.06 | 0.16 | |||
| Bone marrow | 11 (10) | 3 (4) | 2 (2) | ||
| Cord | 4 (4) | 1 (1) | 0 | ||
| Peripheral Blood | 94 (85) | 76 (95) | 89 (99) | ||
| Missing | 1 (1) | 0 | 0 | ||
| Conditioning | 0.70 | 0.01 | |||
| Myeloablative | 64 (58) | 30 (38) | 47 (51) | ||
| Reduced intensity | 22 (20) | 28 (35) | 26 (29) | ||
| Non-myeloablative | 24 (22) | 22 (28) | 18 (20) | ||
| Chronic GVHD severity | 0.07 | 0.45 | |||
| None | 0 | 0 | 1 (1) | ||
| Mild | 24(23) | 20 (26) | 13 (14) | ||
| Moderate | 62 (58) | 38 (49) | 50 (55) | ||
| Severe | 20 (19) | 19 (25) | 27 (30) | ||
| Income before transplant | 0.03 | 0.44 | |||
| <$25,000 | 12 (13) | 6 (9) | 6 (12) | ||
| $25,000–74,999 | 31 (33) | 18 (27) | 26 (50) | ||
| ≥$75,000 | 51 (54) | 43 (64) | 20 (38) | ||
| Baseline employment status | 0.19 | 0.59 | |||
| Disabled/Unemployed | 44 (44) | 27 (36) | 32 (53) | ||
| Full/part time | 31 (31) | 25 (34) | 13 (22) | ||
| Homemaker/retired | 25 (25) | 22 (30) | 15 (25) | ||
| Education | 0.03 | 0.72 | |||
| Any college or higher | 80 (82) | 58 (79) | 41 (67) | ||
| No college | 18 (18) | 15 (21) | 20 (33) | ||
|
HCT to enrollment
(years) |
|||||
| Median (IQR) | 1.5 (0.7–2.8) | 1.7 (08.8–3.8) | 2.1 (1–3.3) | 0.08 | 0.49 |
| HCT to survey completion (years) | |||||
| Median (IQR) | 2.3 (1.3–3.8) | 3.9 (2.6–5.3) | <0.0001 | ||
| SF36 PCS at baseline2 | |||||
| Mean (SD) | 40.0 (8.8) | 39.3 (10.1) | 37.1 (11.6) | 0.08 | 0.63 |
| SF36 MCS at baseline2 | |||||
| Mean (SD) | 47.8 (12.2) | 48.7 (10.7) | 46.7 (12.4) | 0.39 | 0.63 |
| Modified adjusted activity score | |||||
| Mean (SD) | 72.7 (11.5) | 71.6 (9.9) | 71.3 (11.8) | 0.55 | 0.50 |
Chi-square test or Fisher‟s Exact Test for categorical outcomes, t-test or Wilcoxon rank-sum test for continuous variables
n=99 of 110 In-clinic, n=74 of 80 Mailed, n=60 of 91 non-responders
Abbreviations: IQR, Interquartile range; CML, chronic myelogenous leukemia; MDS, Myelodysplastic syndrome; MPD, Myeloproliferative disease; CLL, chronic lymphocytic leukemia; AA, Aplastic anemia; HCT, Hematopoietic cell transplantation; SF-36 PCS, short form-36 physical component scale; SF-36 MCS, short form-36 mental component scale
Income/ education and work status
Seventy three percent of patients had a graduate or higher degree. The proportion of patients reporting annual household income <$25,000 increased from 10% at enrollment to 20% at the time of survey completion. There was no significant change in proportion of patients at work/ school from enrollment to the time of survey (33% vs. 38%; p=0.36). Working or being in school at the time of enrollment was associated with working/being in school at the time of survey (88% of those working at enrollment were currently working or in school vs. 12% of those working at enrollment currently not working or in school; p<0.001). Twenty seven percent of respondents reported being „disabled/ unable to work‟ at the time of the survey. Table 2 highlights some comments of respondents in response to the question “Did your work status change since transplant?” Not surprisingly, working or being in school part-time/ full-time at the time of the survey was associated with a higher income category (81% of those working/ in school vs. 47% of those not working/ in school had an annual income ≥$50,000). Respondents who were working or in school also had higher physical and mental functioning as well as activity levels as compared to those who were not working or in school (p=0.002).
Table 2:
Narrative comments from patients about financial and employment issues
| Change in work status |
|
Yes, unable to work due to neuropathy, fatigue, multiple doctor visits, treatment every day.
Chronic GVHD restricted movement |
| I went from full-time to retired on disability once cancer treatment started. Now post-transplant almost 5 years I am unable to work full-time due to fatigue and immune suppression |
| Became disabled-- too much missed work due to doctor appointments every 2 weeks and if I had a fever, being in the hospital for 6 days at a time |
| Unable to work-- too many negative side effects from medications and hospitalizations and appointments, Unpredictable complications keep arising |
| I now work part-time, maybe 30 hours a week vs 50 hours/week pre-transplant. Reduction due to less physical energy and less mental agility |
| I was terminated from my position of president/CEO, now working part time for the same company in a lower capacity at 1/4 the pay |
| Being a health care professional not able to work due to immunosuppression/steroid use and chronic GVHD |
| I intended to return to the kind of work I’ve done before but can’t because of gvhd related eye problems |
| Causes and assistance for financial burden |
| Reduction in pay due to having to move to a part-time status |
| Divorce and loss of stable housing, rent is a huge challenge |
| Short sale of house; liquidating assets including retirement; living off disability |
| Selling everything that I owned that had any value, cashed out IRA |
| Savings are diminished drastically but I managed |
| Retirement savings, sold automobile |
| Get food from food banks |
Out-of-pocket costs and Insurance issues
Twenty three percent and 39% of patients reported spending >$500 in the last 3 months on healthcare-related non-medical (transportation to the clinic (gas, parking), child-care etc.) and medical (prescriptions, co-payments and deductibles etc.) out-of-pocket costs, respectively. All except one patient had health insurance at the time of the survey (51% private and 36% Medicaid/ Medicare and 13% other). 34% had faced insurance difficulties such as delayed/denied coverage for specific treatments for chronic GVHD (65% for medications and 38% for labs/ procedures, such as extra-corporeal photopheresis), and this experience was correlated with reporting financial burden (p=0.05).
Financial Burden, reported causes and sources for assistance
Sixty six percent of the respondents reported financial burden: 24% had difficulty paying medical bills, 28% reported not having enough money at the end of the month, 49% reduced spending on utilities and other expenses, 31% used retirement savings and 16% borrowed money or sold assets. Bankruptcy rate was <1%. The determinants for financial burden included need for multiple medications/ treatments (41%), inability to return to work (40%), frequent physician visits (32%) and losing/ changing insurance (8%). Approximately half of the patients >1 year out from HCT had made ≥4 visits to their transplant center clinic (46%) or their hematologist (51%) in the last 6 months, respectively. Assistance from family/ friends/ conducting fund-raisers was a source for help with finances for 32% of respondents, while resources suggested by transplant social workers/ charitable organizations were used by 10% of respondents. Table 2 shows some of the selective narrative comments from respondents for causes of and assistance with financial concerns.
Factors associated with financial burden and return to work/ school
Table 3 describes the differences in sociodemographic and clinical characteristics between the respondents who experienced financial burden vs. those who did not. In this univariate analysis, younger age, lower income, being disabled/ unemployed, those with lower physical and mental functioning and activity level as well as Medicare and Medicaid beneficiaries were more likely to be financially burdened. Additionally, psychological burden such as depression/ anxiety and difficulty sleeping were higher in those that endorsed financial burden as compared to those who didn’t (mean score 26 vs. 16; p=0.004 in those with and without financial burden).
Table 3:
Differences in clinical and sociodemographic characteristics between respondents without and with financial burden (FB)
| No FB (n=64) | FB present (n=126) | p value | |
|---|---|---|---|
| Age at enrollment | 0.010 | ||
| Mean (SD) | 56 (14.2) | 51 (14) | |
| Race | 0.03 | ||
| White | 61 (95%) | 105 (83%) | |
| Others | 3 (5%) | 5 (17%) | |
| Gender | 1.000 | ||
| Male | 42 (66%) | 82 (65%) | |
| Income before transplant | 0.07 | ||
| <25,000 (low) | 2 (4%) | 16 (15%) | |
| $25,000–74,999 (medium) | 18 (32%) | 31 (30%) | |
| ≥75,000 (high) | 36 (64%) | 58 (55%) | |
| Income at survey | < 0.001 | ||
| <25,000 (low) | 3 (5%) | 34 (29%) | |
| $25,000–74,999 (medium) | 20 (35%) | 51 (43%) | |
| ≥75,000 (high) | 35(60%) | 34(29%) | |
| Education | 0.900 | ||
| Any college or higher | 46 (79%) | 92 (81%) | |
| No college | 12 (21%) | 21 (19%) | |
| Baseline employment status | 0.001 | ||
| Disabled/Unemployed | 13 (22%) | 58 (50%) | |
| Full/part-time | 25 (42%) | 31 (27%) | |
| Homemaker/retired | 21 (36%) | 26 (23%) | |
| Employment status at survey | < 0.001 | ||
| Disabled/Unemployed | 11 (17%) | 56 (44%) | |
| Full/part-time | 31 (48%) | 39 (31%) | |
| Homemaker/retired | 22 (34%) | 31 (25%) | |
| Insurance type | 0.061 | ||
| Medicare/ Medicaid | 17 (27%) | 50 (40%) | |
| Private | 40 (63%) | 55 (44%) | |
| Other | 7 (11%) | 19 (15%) | |
| Transplant source | 0.236 | ||
| Bone marrow | 4 (6%) | 10 (8%) | |
| Cord blood | 0 (0.0%) | 5 (4%) | |
| Peripheral blood | 60 (94%) | 110 (88%) | |
| Disease Diagnosis | 0.73 | ||
| Acute Leukemia | 29 (45%) | 63 (50%) | |
| CML/MDS/MPD | 16 (25%) | 33 (26%) | |
| Lymphoma including CLL | 15 (23%) | 21 (17%) | |
| AA/Other | 4 (6%) | 9 (7%) | |
| Disease status | 0.263 | ||
| Advanced | 7 (11%) | 25 (20%) | |
| Early | 34 (53%) | 56 (44%) | |
| Intermediate | 23 (36%) | 45 (36%) | |
| Conditioning | 0.262 | ||
| Myeloablative | 28 (44%) | 66 (52%) | |
| Reduced intensity | 16 (25%) | 34 (27%) | |
| Non-myeloablative | 20 (31%) | 26 (21%) | |
| SF-36 physical component score closest to survey completion | 0.004 | ||
| Mean (SD) | 42.5(9.6) | 38.2 (8.9) | |
| SF-36 mental component score closest to survey completion | 0.006 | ||
| Mean (SD) | 51.5 (9) | 46.4 (12.3) | |
| Modified adjusted activity score, closest to survey completion | 0.007 | ||
| Mean (SD) | 69.5 (13.3) | 63.5 (13.9) | |
| Comorbidity index, baseline | 0.848 | ||
| Median (Range) | 2 (0 – 7) | 2 (0–9) | |
| Chronic GVHD severity | 0.431 | ||
| Mild | 17 (27%) | 27 (22%) | |
| Moderate | 35 (57%) | 65 (54%) | |
| Severe | 10 (16%) | 29 (24%) | |
| Visit type | 0.157 | ||
| Clinic | 32 (50%) | 78 (62%) | |
| Mailed in | 32 (50%) | 48 (38%) | |
| Institution location | 0.779 | ||
| Canada | 6 (9%) | 15 (12%) | |
| United States | 58 (91%) | 111 (88%) | |
| Years from transplant to survey | 0.610 | ||
| Mean (SD) | 3.6 (2.2) | 3.5(2.6) | |
| Depression/anxiety/difficulty sleeping score | 0.004 | ||
| Mean (SD) | 15.7 (14.3) | 25.6 (23.9) |
Abbreviations: CML, chronic myelogenous leukemia; MDS, Myelodysplastic syndrome; MPD, Myeloproliferative disease; CLL, chronic lymphocytic leukemia; AA, Aplastic anemia; SD, standard deviation
Race (white vs. others: OR 0.30, 95% CI 0.07–0.92, p=0.06) and age at enrollment (OR 0.97, 95% CI 0.95–0.99, p=0.03) emerged as significant predictors of financial burden in the baseline multivariate model. In the enhanced model for financial burden, race (OR 0.25, 95% CI 0.060.78; p=0.03), SF36-MCS (OR 0.97, 95% CI 0.93–1.0; p=0.03), and mAAS (OR 0.97, 95% CI 0.95–1.0, p=0.05) were significant. Age lost its significance in the enhanced model.
In the stepwise regression analysis of ability to return to work/ school at the time of survey, age again emerged as a significant predictor in the baseline model (OR 0.97, 95% CI 0.95–0.99; p=0.009) and remained significant in the enhanced model (OR 0.97, 95% CI 0.94–0.99; p=0.005). Early risk disease was associated with a higher likelihood of returning to work/ school in the baseline model (OR 2.73, 95% CI 1.1–7.3; p=0.03) but lost its significance in the enhanced model where mental functioning (SF36-MCS) (OR 1.06, 95% CI 1.03–1.10; p< 0.001) and time from transplant to survey (OR 0.82, 95% CI 0.69–0.94; p=0.01) emerged as significant.
Discussion
Financial, insurance and employment implications of allogeneic HCT have been reported.5–8, 19 In this multi-center cohort of patients who all had chronic GVHD, financial burden was reported by two-thirds of the respondents despite being insured. Need for multiple medications/ ongoing treatment and inability to go back to work were the major reasons for financial burden, consistent with ongoing treatment for chronic GVHD. One third reported health insurance difficulties with delays or denials of coverage, which is not surprising due to scarcity of FDA approved treatments and no clearly defined pathways for treatment, but concerning since patients with chronic GVHD have ongoing active medical issues. One fourth of respondents were unable to go back to work due to being disabled. Income decline was reported even from the time of enrollment to the current time. The interplay of socioeconomic factors leading to financial hardships as has been reported in cancer survivors were also seen in our study.20, 21 Younger age was associated with a higher likelihood of financial burden in our baseline model (though not in the enhanced model), as it has been reported in other studies in the area likely due to financial responsibilities of a younger household, inadequate time to build on savings and lack of universal coverage such as with Medicare,22, 23 Non-White race, lower SF36-MCS and worse functional status have also been reported to be significantly associated with higher financial burden.22, 24, 25 Out-of-pocket expenditures, in part from prescription copayments, known to be an important source of financial burden, remained high for this population even a long time after HCT.26, 27 Finally, we observed an increased occurrence of depression and anxiety in those with financial burden as has been described previously.8, 24
Our study clearly indicates that the prevention and amelioration of socioeconomic problems should be an adjunct to the care of patients with chronic GVHD, since improving the overall well-being of the patient is a vital tenet of patient-centered care. It is important for chronic GVHD providers to be able to recognize which patients and caregivers are at risk for adverse effects from financial burden in order to offer them timely assistance and support. A point to be noted is that this is a large cohort of chronic GVHD patients across different transplant centers in United States and Canada who have a steady health insurance, are getting ongoing, optimal post-HCT medical care and have a reasonable functional status despite which they report substantial socioeconomic impact from their disease. The situation is likely to be worse for patients who are extremely disabled, or lose their insurance, or are forced to switch to plans with high deductibles causing them to forego optimal care or being seen at transplant centers. Unfortunately, it may not always be possible to capture this population because of fragmented post-HCT care and lack of adequate longitudinal follow-up at most centers. While the transplant centers have a reasonably strong infrastructure that helps assess benefits and provide support to get the patients through transplant, it is not quite as robust for the post-HCT care.
Deleterious effects of financial burden, specifically high out-of-pocket costs worsening adherence to treatment and clinical outcomes have been reported by other investigators.28–31 Patients with chronic GVHD are a medically vulnerable population and the potential of noncompliance with care due to financial hardship may lead to worse biomedical outcomes. Future research should investigate use of tailored resources such as structured rehabilitation programs, vocational assistance, interventions to increase employment rights awareness, financial planning and assistance programs to ameliorate adverse financial and work-related implications for these patients. While some of these strategies could be implemented by a multidisciplinary team at the transplant center, others may require active engagement of referring/ treating physicians, employers, payers and non-profit health care organizations/ societies. Also, the need for additional policy changes at the level of various stakeholders such as the transplant center, payers and federal government to ensure provision of adequate and affordable post-HCT care cannot be emphasized enough. 28–31
A cross-sectional design, low representation of minority population, a heavily insured population subset and a high proportion of respondents with a higher educational status are some of the limitations of our study. Lack of matched chronic GVHD free controls makes it difficult to tease out the specific impact of this complication from the overall financial burden occurring as a result of HCT itself. It is possible that those who did not respond or declined to participate were sicker and had more significant financial burden which is suggested by the lower income and lower education levels of non-respondents at the time they enrolled into the parent study. We also did not ask specifically about the details of denial/ delay in coverage or about the details of insurance coverage that would have impacted financial burden such as deductibles, coverage gaps, lifetime caps and out-of-network costs. Patients from Canada were included in the study even though they have a different health care insurance system because some of the other factors for financial burden such as inability to go to work and need for multiple visits to the health care provider may still be prevalent in this subset. No differences were observed in the results when Canadian patients were removed from the dataset (data not shown). Finally, even though we had a good response rate and reasonable sample size, it may have still been too small to detect significant associations in the multivariate analysis. Other studies have reported age, race, income level, gender, primary language, and work status as significant predictors of financial burden in other cancer populations.
Notwithstanding the limitations, this study, to our knowledge, is one of the first comprehensive reports on the socio-medical profile of patients with chronic GVHD. The adverse socioeconomic and psychosocial consequences of this devastating iatrogenic complication of HCT add on to the burden caused by medical complications associated with it. Efforts to decrease the incidence of chronic GVHD and to help those suffering from chronic GVHD to preserve their assets and minimize financial burden may significantly improve quality of life after HCT.
Supplementary Material
Highlight.
A significant proportion of allogeneic hematopoietic cell transplantation patients with chronic GVHD experience financial burden despite being insured. Non-white race, lower mental functioning and lower activity score are associated with a higher likelihood of financial burden.
Patients with financial burden had poor psychosocial outcomes such as higher depression/ anxiety and difficulty sleeping.
Acknowledgements
This study was funded by National Cancer Institute (CA118953).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nekhlyudov L, Walker R, Ziebell R, Rabin B, Nutt S, Chubak J. Cancer survivors’ experiences with insurance, finances, and employment: results from a multisite study. Journal of cancer survivorship : research and practice. 2016. [DOI] [PubMed] [Google Scholar]
- 2.Zafar SY, Peppercorn JM, Schrag D, et al. The Financial Toxicity of Cancer Treatment: A Pilot Study Assessing Out-of-Pocket Expenses and the Insured Cancer Patient’s Experience. Oncologist. 2013;18:381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meeker CR, Geynisman DM, Egleston BL, et al. Relationships Among Financial Distress, Emotional Distress, and Overall Distress in Insured Patients With Cancer. Journal of Oncology Practice. 2016;12:e755–e764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meneses K, Azuero A, Hassey L, McNees P, Pisu M. Does economic burden influence quality of life in breast cancer survivors? Gynecologic Oncology. 2012;124:437–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khera N, Chang YH, Hashmi S, et al. Financial burden in recipients of allogeneic hematopoietic cell transplantation. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2014;20:1375–1381. [DOI] [PubMed] [Google Scholar]
- 6.Majhail NS, Rizzo JD, Hahn T, et al. Pilot study of patient and caregiver out-of-pocket costs of allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2013;48:865871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abel GA, Albelda R, Khera N, et al. Financial Hardship and Patient-Reported Outcomes after Hematopoietic Cell Transplantation. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2016;22:1504–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamilton JG, Wu LM, Austin JE, et al. Economic survivorship stress is associated with poor health-related quality of life among distressed survivors of hematopoietic stem cell transplantation. Psycho-Oncology. 2013;22:911–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Syrjala KL, Martin PJ, Lee SJ. Delivering care to long-term adult survivors of hematopoietic cell transplantation. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012;30:3746–3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhatia S, Francisco L, Carter A, et al. Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood. 2007;110:3784–3792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pidala J, Kurland B, Chai X, et al. Patient-reported quality of life is associated with severity of chronic graft-versus-host disease as measured by NIH criteria: report on baseline data from the Chronic GVHD Consortium. Blood. 2011;117:4651–4657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SJ, Onstad L, Chow EJ, et al. Patient-reported outcomes and health status associated with chronic graft-versus-host disease. Haematologica. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee SJ, Hamilton BK, Pidala J, et al. Design and Patient Characteristics of the Chronic Graft-versus-Host Disease Response Measures Validation Study. Biology of Blood and Marrow Transplantation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: The validation of the COmprehensive Score for financial Toxicity. Cancer. 2016:n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prawitz A D GET, Sorhaindo B, O’Neill B, Kim J, and, P D. InCharge Financial Distress/Financial Well-Being Scale: Development, Administration, and Score Interpretation. Financial Counseling and Planning 2006;17:34–49. [Google Scholar]
- 16.Head BA, Faul AC. Development and validation of a scale to measure socioeconomic well-being in persons with cancer. J Support Oncol. 2008;6:183–192. [PubMed] [Google Scholar]
- 17.McHorney CA, Ware JE, Jr., Raczek AE The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. [DOI] [PubMed] [Google Scholar]
- 18.Lee SJ, Cook EF, Soiffer R, Antin JH. Development and validation of a scale to measure symptoms of chronic graft-versus-host disease. Biology of Blood and Marrow Transplantation. 2002;8:444–452. [DOI] [PubMed] [Google Scholar]
- 19.PreusslerJ DE, Majhail NS. Costs and Cost-Effectiveness of Hematopoietic Cell Transplantation. Biology of Blood and Marrow Transplantation.In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jagsi R, Pottow JAE, Griffith KA, et al. Long-Term Financial Burden of Breast Cancer: Experiences of a Diverse Cohort of Survivors Identified Through Population-Based Registries. Journal of Clinical Oncology. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Warner EL, Kirchhoff AC, Nam GE, Fluchel M. Financial Burden of Pediatric Cancer for Patients and Their Families. Journal of Oncology Practice. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shankaran V, Jolly S, Blough D, Ramsey SD. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: a population-based exploratory analysis. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2012;30:1608–1614. [DOI] [PubMed] [Google Scholar]
- 23.Weaver KE, Rowland JH, Bellizzi KM, Aziz NM. Forgoing medical care because of cost: assessing disparities in healthcare access among cancer survivors living in the United States. Cancer.116:3493–3504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharp L, Carsin A-E, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psycho-Oncology. 2013;22:745–755. [DOI] [PubMed] [Google Scholar]
- 25.Fenn KM, Evans SB, McCorkle R, et al. Impact of Financial Burden of Cancer on Survivors’ Quality of Life? Journal of Oncology Practice. 2014. [DOI] [PubMed] [Google Scholar]
- 26.Narang AK, Nicholas L. Out-of-pocket spending and financial burden among medicare beneficiaries with cancer. JAMA Oncology. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farnia S, Ganetsky A, Silver A, et al. Challenges around Access to and Cost of Life-Saving Medications after Allogeneic Hematopoietic Cell Transplantation for Medicare Patients. Biology of Blood and Marrow Transplantation. 2017;23:1387–1392. [DOI] [PubMed] [Google Scholar]
- 28.Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32:306311. [DOI] [PubMed] [Google Scholar]
- 29.Khera N, Chow EJ, Leisenring WM, et al. Factors associated with adherence to preventive care practices among hematopoietic cell transplantation survivors. Biology of blood and marrow transplantation : journal of the American Society for Blood and Marrow Transplantation. 2011;17:995–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kent EE, Forsythe LP, Yabroff KR, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer. 2013;119:3710–3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Doshi JA, Li P, Huo H, Pettit AR, Armstrong KA. Association of Patient Out-of-Pocket Costs With Prescription Abandonment and Delay in Fills of Novel Oral Anticancer Agents. Journal of Clinical Oncology. 2018;36:476–482. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.