Abstract
Purpose:
Using a mixed-methods formative evaluation, the purpose of this study was to provide a broad overview of the Alabama eHealth programme set-up and initial patient outcomes. The Alabama eHealth programme uses telemedicine to provide medical care to people living with HIV in rural Alabama. It was led by a community-based organisation, Medical Advocacy and Outreach (MAO), and supported by AIDS United and the Corporation for National Community Service’s Social Innovation Fund with matching support from non-federal donors.
Methods:
We conducted and transcribed in-depth interviews with Alabama eHealth staff and then performed directed content analysis. We also tracked patients’ (n=240) appointment attendance, CD4 counts, and viral loads.
Findings:
Staff described the steps taken to establish the programme, associated challenges (e.g., costly, inadequate broadband in rural areas), and technology enabling this programme (electronic medical records, telemedicine equipment). Of all enrolled patients, 76% were retained in care, 88% had antiretroviral therapy and 75% had a suppressed viral load. Among patients without missing data, 96% were retained in care, 97% used antiretroviral therapy and 93% had suppressed viral loads. There were no statistically significant demographic differences between those with and without missing data.
Conclusions:
Patients enrolled in a telemedicine programme evaluation successfully moved through the HIV continuum of care.
Keywords: eHealth, telecare, telehealth, telemedicine
Introduction
Southern US states have higher HIV incidence and lower survival rates than the USA overall.1 Alabama has steadily rising HIV prevalence and low care engagement: only 70% of Alabama’s estimated 13,710 people living with HIV (PLWH) were retained in care and 59% had suppressed viral loads (⩽200copies/ml).2 The highest incident HIV rates are in rural counties.3
Formidable barriers to care exist for rural PLWH: lack of medical providers trained in HIV; non-existent public transportation; long distances to providers’ offices; lack of confidentiality; poverty; and HIV-related stigma.4,5 Many PLWH travel to urban areas fearing limited confidentiality in the care from their rural physicians or that rural physicians are not well-equipped to manage HIV.6
Previous research on telemedicine in HIV care
One study directly compared telemedicine to in-person HIV care and found similar clinical and psychosocial outcomes.7 Two studies of Veteran’s Administration (VA) patients living in rural areas – one pre-post and one mixed-methods study – found reduced patient travel time, high acceptability, normal CD4 counts and improved appointment attendance.8,9 Telemedicine may have other advantages, such as reaching underserved populations and being cost effective.10–13
Outside of the VA or prison contexts, the literature on HIV care delivery in rural US areas through telemedicine remains nascent.8,9 There is an increasing HIV burden in the south-east, acute barriers to care in rural areas, and calls from a recent review for further study of the feasibility and efficacy of telemedicine programmes.14 In response, we conducted a mixed formative evaluation of a rural, southern telemedicine programme. Our research questions included: What were the steps to initiate a telemedicine programme? What were the initial HIV care continuum outcomes for its patients?
Methods
Intervention
Medical Advocacy and Outreach (MAO) began the Alabama eHealth programme in 2011. Patients seek care at a clinic near their residence and access a remotely located HIV specialist via telemedicine. This programme was supported by AIDS United and a grant from the Corporation for National and Community Service (CNCS)’s Social Innovation Fund with matching non-federal support.
In the Alabama eHealth programme, telemedicine-based medical appointments are facilitated by an on-site nurse. The telemedicine equipment transmits real-time, high-definition video for clear, virtual face-to-face communication. The provider is able to examine the patient using wireless blue-tooth peripheral stethoscopes (3M Littmann Electronic Stethoscope Model 3200, St Paul, Minnesota, USA), which uses 3M Telesteth Software (St Paul, Minnesota, USA). Other examination equipment includes an otoscope to examine patient’s ears, nose, and throat, and a dermascope for skin examination (Horus HD Digital Scope System-Series 1, JEDMED, St. Louis, Missouri, USA). Through the devices, real-time heart and lung sounds are transmitted to the provider. The telemedicine system is paired with a web-based electronic medical record system (EMR; SuccessEHS-Greenway Health, Carrollton, Georgia, USA), accessible from patient and provider locations. Prescriptions can also be completed electronically. All information is transmitted through a confidential, connection compliant with the Health Insurance Portability and Accountability Act (HIPAA).
Patients receiving services through telemedicine are new patients or existing patients switching to telemedicine. Whenever possible, all first appointments occur in-person. The provider travels to the patient (‘satellite’) site for the first in-person visit and future visits are typically done remotely through telemedicine. However, if patients prefer, they can continue seeing the provider in-person but most travel to a ‘satellite’ site (this provision was put in place to respect patients’ possible wishes for an in-person appointment). In practice, patients could have a combination of telemedicine and in-person visits, depending on their preferences. Wraparound services are also available to patients by telemedicine: social work case management, pharmacy adherence counselling, mental health counselling and translation services.
Partners
The Alabama eHealth programme initially had two main MAO locations and three satellite locations co-located with different partners (one rural Residency Program, two sites of one Federally Qualified Health Center (FQHC) organisation) (Table 1). Each location had telemedicine equipment. One partner, Thrive Alabama, had one rural ‘satellite’ site. Another partner, the Selma AIDS Information Resource (Selma AIR), identified and linked PLWH in one geographic area to care and social services. The Alabama Department of Public Health (ADPH) provided telemedicine equipment and Internet connections at all the county health department partner sites. At the time of this analysis, the Alabama eHealth programme had 12 sites (Table 1).
Table 1.
Organisations involved in Alabama eHealth.
| Organisation name | Location(s) | Date telemedicine started | Organisation type | Role in Alabama eHealth |
|---|---|---|---|---|
| Medical Advocacy and Outreach (MAO) | Montgomery | 2012 | Community-based organisation (CBO) | Lead organisation in Alabama eHealth. Main office location where HIV physician is located. Pharmacist, case management, Spanish translator, and food pantry are available here. |
| MAO | Dothan | 2012 | CBO | MAO satellite office; main mental health care provider location. Case management, transportation (van). |
| Thrive Alabama Thrive Alabama |
Huntsville Florence |
2012 2012 |
CBO CBO |
Main office location and main HIV physician location. Satellite clinic for in-person patients in Huntsville. Phlebotomy, on-site nurse, and periodic in-person physician services. |
| University of Alabama at Birmingham- Selma’s Family Medicine Residency Training Program | Selma | 2012 | Family Medicine Training Program | Satellite clinic; staffed by MAO nurse; MAO telemedicine equipment located here. Medical resident physicians learn about telemedicine and follow MAO patients if hospitalised. |
| Southeast Alabama Rural Health Associates (SARHA) | Troy | 2014 | FQHC | Satellite clinic. MAO staff (nursing, social work, and phlebotomy) travel here twice monthly. MAO also provides telemedicine equipment and Internet connection. |
| SARHA Health Services Incorporated (HSI) | Clayton Hayneville |
2014 2014 |
FQHC FQHC |
Satellite clinic. MAO staff (nursing, social work, and phlebotomy) travel here monthly. MAO also provides telemedicine equipment and Internet connection. Satellite clinic. MAO staff (nursing, social work, and phlebotomy) travel here monthly. MAO also provides telemedicine equipment and Internet connection. |
| County Health Department | Evergreen | 2015 | County Health Department | Satellite clinic. MAO staff (nursing, social work, and phlebotomy) travel here monthly. |
| Marion | 2015 | County Health Department | Satellite. MAO staff (nursing, social work, and phlebotomy) and travel here monthly. | |
| Linden | 2015 | County Health Department | Satellite clinic. MAO staff (nursing, social work, and phlebotomy) and travel here monthly. | |
| Andalusia | 2015 | County Health Department | Satellite clinic. MAO staff (nursing, social work, and phlebotomy) and travel here monthly. |
FQHC: Federally Qualified Health Center.
Study design
This formative evaluation mixes qualitative data from in-depth interviews (IDIs) and quantitative data from patient medical charts.15 The qualitative and quantitative strands were partially mixed and concurrently collected. The qualitative strand was given precedence over the quantitative making it a ‘partially mixed concurrent dominant status’ design.16
Qualitative data collection and analysis
One evaluator conducted seven semi-structured, in-depth phone interviews during October 2014 with programme staff. Each interview lasted 45–60min. These interviews were part of a national project evaluation described in detail elsewhere.17 At each organisation, the evaluator aimed to speak with an individual working in an administrative capacity, such as a programme manager, and another who provided services to PLWH. Examples of participants included professionals with training in mental health, substance use, medicine, policy and social work. Interviews focused on implementing the telemedicine programme, barriers to implementation and facilitating factors. The Institutional Review Board at the Johns Hopkins School of Public Health exempted this evaluation from review because it was considered non-human subjects’ research as interviewees were describing areas of professional expertise.
Interviews were digitally recorded (KMJ), professionally transcribed by a HIPAA-compliant group, Production Transcripts (Glendale, California, USA), and analysed in ATLAS.ti using directed content analysis.18 We (KMJ, CM) searched for common themes and disconfirming cases. Our initial coding schema was based on predefined research questions and existing literature. It was later refined based on emergent themes.
Quantitative data collection, analysis, and measures
Starting in October 2013, patients receiving HIV care from MAO were approached about this evaluation. If patients retrospectively consented to participation, their medical record and appointment data were included. A medical visit could be in-person or via telemedicine. Retention in care was defined as having two medical visits at least 60 days apart in the past year.19 Viral suppression was defined as having a viral load ⩽200 copies/ml.20 Viral load, antiretroviral therapy (ART) and retention in care data were abstracted from medical records. We (KMJ, TS) also analysed demographic data. To construct the HIV continuum of care, all participants with data at baseline, six or 12 months were included. All participants were accessing care and, therefore, considered linked to care. If participants were retained in care, on ART, or virally suppressed at six or 12 months, they were included in that category. Investigators working with quantitative data received institutional review board approval from the Western Institutional Review Board (#1141766).
Results
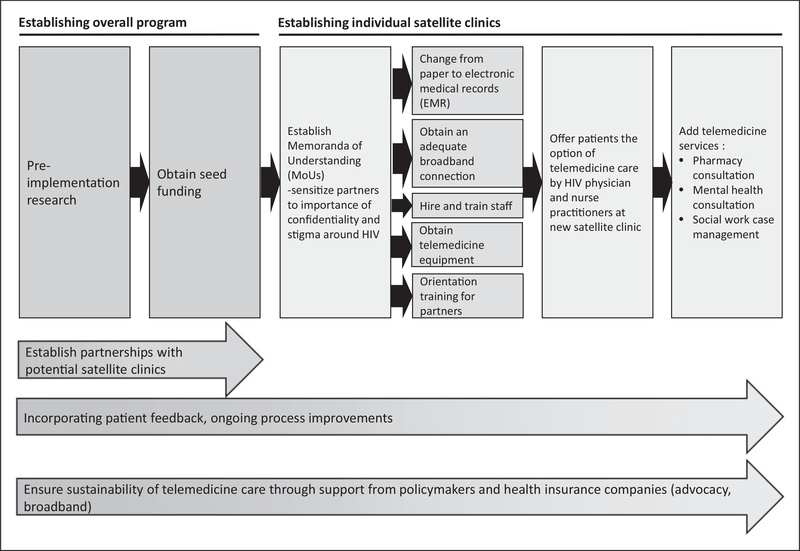
We analysed seven IDIs. Three interviewees were in administrative roles and four provided services to clients directly. We describe analysis results by theme below. Figure 1 illustrates steps to establish the programme starting with conducting pre-implementation research and obtaining seed funding. Programme leaders established partnerships with other programmes to set up satellite telemedicine clinics. This process is illustrated by an arrow below the rectangular boxes. Once complete, staff created memoranda of understanding (MoUs), and sensitised partners to confidentiality and stigma.
Figure 1.
Steps for establishing the telemedicine programme.
Next, staff switched from paper to Web-based electronic medical records; ensured an adequate broadband connection; hired and trained new staff; procured telemedicine equipment; and trained partners. After completion, satellite sites could offer care via telemedicine. Finally, additional services were offered via telemedicine. Throughout, MAO incorporated patient feedback, conducted ongoing process improvements and advocated for its support from policymakers and health insurance companies. These last two processes (two arrows at the bottom extending across the full width of the image) are represented by the long arrows at the bottom of the diagram (Figure 1). Examples of illustrative quotes are provided in Table 3.
Table 3.
Quotations describing steps to establish Alabama eHealth programme.
| Establishing overall programme | |
| Pre-implementation research | We look at minute basics, including what should be the background colour to what could be the instruments, what should be the voice and sound quality... We used the Emory University’s AIDSVu map to look at what areas in Alabama have the highest HIV burden and lack of resources. |
| Obtain seed funding |
It’s very hard for a nonprofit to get the upfront money to put in an EMR, but we did that as part of the [AIDS United-funded] telemed grant. We never had an in-house IT support before, and with the grant, we were able to hire an inhouse IT manager... we could not have afforded that on our own without the AIDS United SIF grant, and we could not have done the project without it. |
| Establishing individual telemedicine sites | |
| Establish MoUs | We already had very good working relationships with partners in our area. |
| Change to EMR, obtain an adequate broadband connection, hire and train | There are certain areas [with] a monopoly on the broadband services and it’s very, very hard to get the bandwidth that we need to run our telemedicine. |
| staff, obtain telemedicine equipment, | The [EMR] learning curve is horrific and time consuming and therefore costly. We’ve had it for |
| orientation training for providers | at least two years now. We are not as efficient now in terms of provider time and visits as we were on paper. |
| We may be able to go into three to six more health departments by the first of the year and the other major benefit to that is when they put in the telemedicine equipment with their broadband, they’re paying the broadband sustainability cost and we’re not. So it’s signifi- cantly easier for us to see relatively small numbers of people without it being a huge expense to us because we’re not paying for the broadband, we’re just sending the nurse. | |
| The resolution was not very good sometimes, and there was a delay. So, you would find sometimes that the patient and provider were speaking at the same time because of the delay... that was a little frustrating, but it really wasn’t the equipment itself. It had more to do with our Internet connection. | |
| I know that it’s [telemedicine] just another tool for us to be able to serve our rural population, but I’m just old school and they’re old school. We like to be able to touch our patient and be face-to-face and check out the body language and all that. But, we realise that this is where we’re going and I think we embrace it. | |
| Offer patients the option of telemedicine care by HIV physician and nurse practitioners at new satellite clinic | Those challenges were getting the staff to become accustomed to getting the patient in and getting them set up so that we don’t waste a lot of time... in the beginning... we would spend 10 or 15 minutes trying to get the patient into the telemedicine office, get the equipment operable. |
| Add telemedicine services: pharmacy consultation, mental health consult- ation, and social work case management | Our biggest challenge... has been the Internet. The week before last, the Internet was down so many times that the substance abuse and mental health programme couldn’t complete their support group because they were doing it over telemedicine, but the Internet was down. |
| When I have an actively suicidal patient, then I have to get assistance from the nursing staff... to assist me in maybe helping get a family member to come pick up this patient and transport them to the hospital... we have to work as a team so I have to be able to make contact with other staff members to assist me. |
EMR: electronic medical record; MoUs: memoranda of understanding.
Pre-implementation research
MAO staff examined existing telecare models starting in 2009, particularly telepsychiatry. Three staff described the process of reviewing HIV epidemiology in Alabama and available technology, such as telemedicine equipment and electronic medical records. The team ascertained levels of available bandwidth in Alabama for ensuring a confidential connection. Over time, the team defined detailed aspects of the programme set up.
Obtain seed funding
Seed funding was needed to support staff time, telemedicine equipment and a broadband connection. Four administrators and service providers emphasised that the Alabama eHealth programme would not have been possible without initial investments from AIDS United and the CNCS’s Social Innovation Fund. This grant enabled MAO to purchase telemedicine equipment and update recordkeeping systems from paper to web-based electronic medical records (EMRs).
These start-up funds supported a staff position devoted to providing information technology (IT) support, which was vital to the set up and ongoing support of the programme. Administrators described how this groundwork led to later funding from ADPH through the Centers for Disease Control and Prevention (CDC) for expansion.
Change from paper to EMRs
MAO’s multisite telemedicine programme was enabled by a web-based EMR described by four interviewees. The EMR allowed medical staff to access each patient’s information from multiple locations simultaneously. MAO nurses at satellite sites could access the online EMR by laptop. MAO had not had an EMR previously, and some staff felt that the EMR lowered efficiency because staff had to document patient-related information differently. There were also HIV performance tracking indicators added to the medical records. The EMR could be a challenging system to extract data from as the queries were complex to write; however, this challenge improved with support.
Forming partnerships: Establishing MoUs and sensitising partners
As Alabama eHealth connected with partners, they trained and reinforced these organisations on the need to ensure confidentiality and its importance given HIV stigma. Providers devised ways to reduce stigma, such as structuring clinics so that patients seeking HIV care would be indistinguishable from all clinic patients. Programme staff also ensured that staff at partner organisations understood clinical information about HIV to prevent inadvertently perpetuating stigma.
Staff leveraged existing connections and agreed that it would not have been possible to create the Alabama eHealth programme without strong partnerships. MAO placed telemedicine equipment at the initial partnership sites, and a nurse worked with the equipment, patient and remote provider at MAO to facilitate the appointment. Six administrators and providers described how partnerships with social services agencies aided the programme: Selma AIR scheduled appointments for patients, arranged transportation and addressed other structural barriers keeping patients from care in one section of MAO’s service area.
Obtain an adequate broadband connection
Six interviewees described how broadband infrastructure did not exist in all areas of rural Alabama counties or was prohibitively expensive in many areas. To support telemedicine, each location needed a sufficient number of patients, grant funding or cost-sharing with partner organisations. The Alabama eHealth programme partnered with the ADPH’s programme providing telemedicine and broadband equipment to county health department clinics, and the ADPH clinics provided the Internet connection. Administrators described how this innovative programme was modelled after the MAO Alabama eHealth programme and has helped expand telemedicine access. Programme staff successfully negotiated with Internet service providers to increase the amount of bandwidth.
Another challenge was sufficient bandwidth to sustain clear, stable connections as described by three interviewees. Care providers faced communication difficulties, such as time delays during appointments, which caused patients and providers to speak at the same time. In addition, there were times when the Internet was unavailable and telemedicine-based activities could not happen.
Hire and train staff
Providers learned to use the telemedicine equipment. Most were enthusiastic and adapted easily, but some found it challenging. One provider described how hiring individuals comfortable with the new technology proved challenging, and on occasion a staff member would separate from the project before fully learning the requisite skill set. Four staff described how physician champions and proved important for encouraging staff to become fluent in operating the telemedicine equipment.
Additional services delivered via telemedicine
All interviewees described how the MAO team also used telemedicine equipment for staff meetings across the Alabama eHealth programme’s multiple locations; for mental health care; social work/case management services; clinical pharmacy consultations; pre-exposure prophylaxis (PrEP); and hepatitis C care and treatment. Administrators and providers were enthusiastic about how these services could be seamlessly integrated into the existing telemedicine care infrastructure.
Ongoing course corrections
Some nurse facilitators found it difficult to administer care via telemedicine because of poor audio quality, and some providers remained uncomfortable with the technology. This lack of fluency with the equipment led to wasted patient and provider time initially, according to five interviewees. Programme staff increased their fluency with the equipment through practice and these initial barriers to efficiency were overcome.
Patients occasionally had difficulty understanding the provider through the telemedicine equipment and requested that staff improve the audio quality. Patients also requested a larger screen. Another course correction was whether the main site would call the satellite location where the patient was located, or vice versa. The team found that the satellite calling the main site worked best and made this standard procedure.
Ensuring sustainability of telemedicine care delivery
Many of Alabama eHealth’s patients did not have health insurance. As a result, the programme had to strategically keep the programme financially sustainable and, thus far, has expanded the programme through grants and partnerships. Administrators shared how telemedicine in Alabama is reimbursed by Medicare, Medicaid (without a facility fee) and, more recently, some insurance companies for services including HIV care. Ryan White reimbursement allows the provision of care for uninsured patients. Staff were optimistic and felt this was an innovative model that made them involved, more visible and relevant. Three administrators and providers recognised that grant funding to cover broadband was finite, time-limited and unsustainable. However, advocates, worked to improve reimbursement in Alabama.
Patient engagement in care
Of the 240 patients participating in the study, 75% were male, 65% were >40 years of age, and 68% were Black/African-American (Table 2). The average time from diagnosis to HIV care was 7.8 years (standard deviation (SD)=6.8 years).
Table 2.
Demographic characteristics and baseline health status of Alabama eHealth study participants.
| Age range, years | ||
| ≤19 | 1 | 0.4% |
| 20–24 | 10 | 4.2% |
| 25–29 | 25 | 10.4% |
| 30–39 | 48 | 20.0% |
| 40–49 | 69 | 28.8% |
| 50+ | 87 | 36.3% |
| Race and ethnieity | ||
| Black/African-American, non-Hispanic | 164 | 68.3% |
| White | 72 | 30.0% |
| Othera | 4 | 1.7% |
| Gender | ||
| Male | 181 | 75.4% |
| Female | 58 | 24.2% |
| Transgender M to F | 1 | 0.4% |
Other includes two White Hispanic participants; one Asian Non-Hispanic participant; and one of unspecified race, with Hispanic ethnicity.
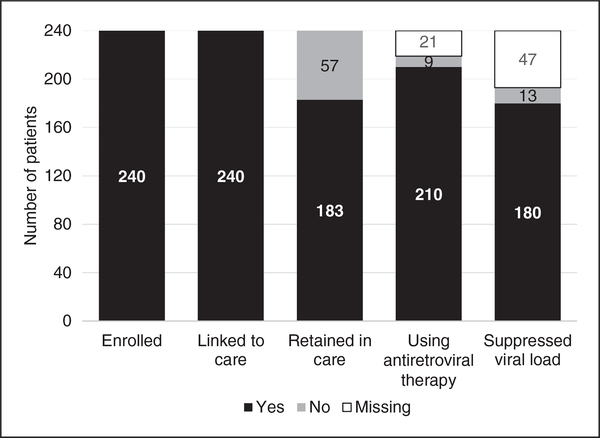
Of the 240 patients participating in the evaluation who had data at baseline, six or 12 months, the vast majority were retained in care (76.3%), using ART (87.5%), and had a suppressed viral load (75.0%). There were 3.8% of participants not using ART, and ART data were missing for the remaining 8.8%. Similarly, 5.4% of all patients did not have a suppressed viral load, and viral load data were missing for the remaining 19.6% (Figure 2). Of the 193 participants for whom clinical data for one year were available, 186 (96.4%) were retained in care, 187 (96.9%) were using ART and 180 (93.3%) had a suppressed viral load (not shown).
Figure 2.
HIV continuum of care for a subset of Alabama eHealth study participants.
There were no statistically significant race, age or gender differences between participants with (n=193) and without follow-up data (n=47) at 12 months (χ2=5.07 and p=0.08 for race; χ2=4.77 and p=0.09 for sex/gender; χ2=2.71 and p=0.75 for age group).
Discussion
Through IDIs, staff provided an overview of steps needed to establish the telemedicine programme, and challenges and solutions. Staff also described the benefits for patients beyond access to an HIV care specialist, such as providing access to other services needed by PLWH. Staff emphasised support enabling the programme: significant seed funding, access to technology, and support for using that technology. The quantitative results show that the majority of participants accessing care using this model had suppressed viral loads. Taken together, these results suggest that it may be worthwhile to expand and replicate this model to make care available to more PLWH living in rural areas.
This study adds to the telemedicine and HIV literature in several ways. A recent review of telemedicine in HIV points to the dearth of studies ‘exploring the human component’ of such programmes, which this study describes. This same review also pointed to a need for further exploration of some of the challenges described in this programme, which include addressing the lack of connectivity in rural areas and maintaining patient confidentiality.14 This programme successfully obtained needed connectivity through collaborations with the state department of public health and negotiating with Internet providers directly. Additionally, this study adds to a desired yet understudied area:1,2 HIV care delivered through telemedicine outside of prisons and the VA. It explores other gaps telemedicine literature described by recent reviews including solutions to lack of rural broadband connectivity and patient confidentiality concerns. It is also an early evaluation of feasibility.14,21 We join earlier studies in suggesting that telemedicine is a way to increase staff bandwidth and provide case management for patients.22
Strengths and limitations
There are several limitations of this study: patients enrolled into the Alabama eHealth programme were already seeking medical care at MAO or a partner, which may have made them more likely to be retained in care and trust the care providers at these organisations. Also, since nearly all of the patients at the ‘satellite’ sites opted to receive care via telemedicine, we could not compare outcomes between patients receiving care via telemedicine and those who opted not to do so. Since the programme was designed to allow patients to continue in-person if they preferred, patients could have a combination of telemedicine and in-person visits if they chose. Another challenge was missing data: while missing data is expected in studies where main outcomes include retention in the programme, its presence can cause difficulty in interpreting results. Here, it is not possible to discern whether patients for whom data are missing were actually receiving care in other locations, were not receiving care at all, or if data were not available for the specific time interval being measured. Patients were not asked about other sources of HIV medical care.
There are drawbacks with a formative evaluation design where it is possible to identify barriers but not explore programme design in-depth longitudinally (e.g. Did EMR implementation differ between sites? Were other uses of telemedicine tested? Did results vary by provider with differing patient loads?). Programme implementation is a dynamic process, but this study represents a single moment in time. Significant programme expansion has taken place since the time of data collection.
This mixed-methods formative evaluation describes a programme that is effective in delivering healthcare in rural areas and encompasses a variety of disease areas and services with a focus on those related to HIV. With appropriate partnerships, providing HIV care through telemedicine is feasible in this – and potentially other – geographies. Important future research directions include understanding how clinic systems can best support telemedicine through an in-depth examination of barriers identified in this study, as well as applications of similar models in other contexts (e.g. EMR implementation, training staff in telemedicine technology). Future research should apply rigorous study designs to compare HIV care delivered through telemedicine vs in-person approaches directly.14
Telemedicine might help achieve the health disparity reduction goals of the national HIV/AIDS strategy goals.23 However, despite strong patient outcomes and support by partners and funders, sustaining such programmes remains in question.11,12 Expanded funds are necessary for supporting broadband provision in rural areas, particularly in contexts where services provided through telemedicine are not fully reimbursable.24
Funding
The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This report is based upon the work of Alabama eHealth supported under Grant No. 10SIHDC001 and supported by the Social Innovation Fund (SIF), a programme of the CNCS. Opinions or points of view expressed in this document are those of the authors and do not necessarily reflect the official position of, or a position that is endorsed by, CNCS or the Social Innovation Fund programme. The Social Innovation Fund is a programme of the CNCS, a federal agency that engages millions of Americans in service through its AmeriCorps, Senior Corps, Social Innovation Fund, and Volunteer Generation Fund programmes, and leads the President’s national call to service initiative, United We Serve. For more information, visit NationalService.gov. This project was also supported by the generous contributions of 14 non-federal funders contributing to MAO (CNCS requires matching funding from non-federal sources).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article. Please note that all affiliations listed were applicable at the time of writing.
References
- 1.Reif S, Pence BW, Hall I, et al. HIV diagnoses, prevalence and outcomes in nine southern states. J Community Health 2014; 40: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alabama Department of Public Health. HIV treatment cascade by public health area. Montgomery, AL, 2014. [Google Scholar]
- 3.Reif S, Golin CE and Smith SR. Barriers to accessing HIV/AIDS care in North Carolina: Rural and urban differences. AIDS Care 2005; 17: 558–565. [DOI] [PubMed] [Google Scholar]
- 4.Whetten K and Reif S. Overview: HIV/AIDS in the deep south region of the United States. AIDS Care 2006; 18: S1–S5. [DOI] [PubMed] [Google Scholar]
- 5.Heckman TG, Somlai AM, Peters J, et al. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care 1998; 10: 365–375. [DOI] [PubMed] [Google Scholar]
- 6.McKinney MM. Variations in rural AIDS epidemiology and service delivery models in the United States. J Rural Heal 2002; 18: 455–466. [DOI] [PubMed] [Google Scholar]
- 7.León A, Cáceres C, Fernández E, et al. A new multidisciplinary home care telemedicine system to monitor stable chronic human immunodeficiency virus-infected patients: A randomized study. PLoS One 2011; 6: e14515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ohl M, Dillon D, Moeckli J, et al. Mixed-methods evaluation of a telehealth collaborative care program for persons with HIV infection in a rural setting. J Gen Intern Med 2013; 28: 1165–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saifu HN, Asch SM, Goetz MB, et al. Evaluation of human immunodeficiency virus and hepatitis C telemedicine clinics. Am J Manag Care 2012; 18: 207–212. [PubMed] [Google Scholar]
- 10.Saberi P, Yuan P, John M, et al. A pilot study to engage and counsel HIV-positive African American youth via telehealth technology. AIDS Patient Care STDS 2013; 27: 529–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCue MJ, Mazmanian PE, Hampton CL, et al. Cost-minimization analysis: A follow-up study of a telemedicine program. Telemed J 2009; 4: 323–327. [DOI] [PubMed] [Google Scholar]
- 12.Wong MT. HIV Care in correctional settings is cost-effective and improves medical outcomes. Infect Dis Clin Pract 2001; 10: S9–S15. [Google Scholar]
- 13.Young JD, Patel M, Badowski M, et al. Improved virologic suppression with HIV subspecialty care in a large prison system using telemedicine: An observational study with historical controls. Clin Infect Dis 2014; 59: 123–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Todd CS, Mills SJ and Innes AL. Electronic health, telemedicine, and new paradigms for training and care. Curr Opin HIV AIDS 2017; 12: 475–487. [DOI] [PubMed] [Google Scholar]
- 15.Creswell JW and Clark VLP. Designing and conducting mixed methods research, 2nd ed. Los Angeles: SAGE Publications, 2011. [Google Scholar]
- 16.Leech NL and Onwuegbuzie AJ. A typology of mixed methods research designs. Qual Quant 2009; 43: 265–275. [Google Scholar]
- 17.United AIDS. Access to care, http://www.aidsunited.org/Programs-0024-Grantmaking/Access-to-Care.aspx (2015, accessed 30 November 2015).
- 18.Hsieh H and Shannon S. Three approaches to qualitative content analysis. Qual Health Res 2005; 15: 1277–1288. [DOI] [PubMed] [Google Scholar]
- 19.Horberg M, Aberg J, Cheever LW, et al. Development of national and multiagency HIV care quality measures. Clin Infect Dis 2010; 51: 732–738. [DOI] [PubMed] [Google Scholar]
- 20.Bradley H, Hall HI, Wolitski RJ, et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV–United States, 2011. MMWR Morb Mortal Wkly Rep 2014; 63: 1113–1117. [PMC free article] [PubMed] [Google Scholar]
- 21.Nesbitt TS, Siddiqui J, Brunader RE, et al. Telemedicine for rural patients with HIV and AIDS: A national survey. In: The 131st Annual Meeting of the American Public Health Association Washington, DC, 2003, p. 69311. [Google Scholar]
- 22.Lillibridge J and Hanna B. Using telehealth to deliver nursing case management services to HIV/AIDS clients. Online J Issues Nurs 2009; 14: 9. [Google Scholar]
- 23.Office of National AIDS Policy. National HIV/AIDS strategy for the United States, https://www.hiv.gov/sites/default/files/nhas-2020-action-plan.pdf (2015, accessed 29 Jan 2018).
- 24.Parmar P, Mackie D, Varghese S, et al. Use of telemedicine technologies in the management of infectious diseases: A review. Clin Infect Dis 2015; 60: 1084–1094. [DOI] [PubMed] [Google Scholar]