The erbium-doped:yttrium, aluminum, and garnet (Er:YAG) as a solid-state laser that produces a pulsed beam with a wavelength of 2940 nm.1 Because of its thermomechanical ablation mechanism and the high absorption of its high absorbability in both water and hydroxyapatite, Er:YAG laser is indicated not only for the management of soft tissues but also for the ablation of hard tissues.2 Er:YAG laser has been reported for periodontal therapy,3 intraoral soft tissue excisional biopsy,4 and dentin desensitization.5 This case report aimed to demonstrate a perspective and simplified option for periodontal regeneration by using Er:YAG laser-assisted nonsurgical treatment.
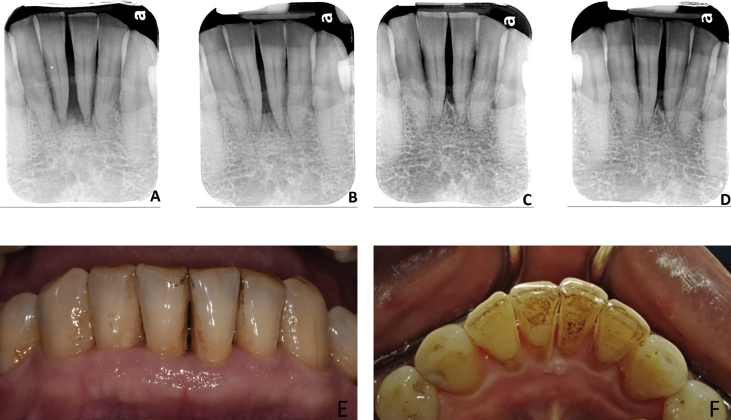
This 67-year-old man came to the Department of Periodontics, Chung Shan Medical University Hospital, Taichung, Taiwan, with the chief complaint of gum disease, especially in the anterior mandibular region. Accumulation of heavy plaque and calculus was noted, and persistent pus discharge was found from the gingival sulci of teeth 31 and 41. After periodontal examination and radiographic evaluation, attachment loss, infrabony defects, and trauma from occlusion were noted on teeth 31 and 41 (Fig. 1A). Initial therapy consisted of oral hygiene instructions, scaling, root planning, and occlusal reduction were performed on teeth 31 and 41. After phase I therapy, the results of reevaluation showed overall pocket depth reduction and less bleeding upon probing. However, pus discharged from the lingual aspects of teeth 31 and 41 off and on. Because this patient worked overseas without willingness to receive periodontal surgery. The non-surgical procedure with Er:YAG laser and possible alternatives were discussed with the patient and informed consent was obtained from the patient. According to the manufacture's guideline, the clinical application of an Er:YAG laser (KEY Laser 3, KaVo, Biberach, Germany) was used to debride root surface. In addition, contact irradiation on the inner surface of the gingival wall under water spray was performed to remove inflammatory tissues such as the pocket epithelia and granulation tissues. The wound healing progressed uneventfully without any clinical complications. Supportive therapy was initiated and the patient was followed up regularly. The original periapical radiographs showed severe bone resorption and infrabony defect at teeth 31 and 41 (Fig. 1A). After 5.5-year follow-up, bone-like dense tissue was found and the bone defect was successfully repaired (Fig. 1B, C, and D). In addition, no adverse side effects were observed. The intraoral pictures revealed the healthy gingival architecture over teeth 31 and 41 after 5.6-year follow-up (Fig. 1E and F).
Figure 1.
(A) Periapical radiography revealed severe infrabony defects and trauma from occlusion on teeth 31 and 41. (B) Periapical radiography revealed dense bone-like tissues on teeth 31 and 41 after one-year follow-up. After 4.3-year (C) and 5.6-year (D) follow-up, no further alveolar bone loss was observed. Clinical photograph after 5.6-year follow-up revealed clinical health gingival architectures: (E) buccal view (F) lingual view.
Er:YAG laser has been reported to ablate subgingival calculus without significant thermal damage on the root surface.1 The KEY Laser 3® with an automatic calculus-detecting system provides a safer and more effective non-surgical periodontal therapy. Er:YAG Laser treatment inside the periodontal pocket can decontaminate, debride, and remove inflammatory tissues to prevent downgrowth of pocket epithelium. In addition, increased bleeding from the debrided inner gingival wall is advantageous for tissue regeneration resulting in bone-like dense tissue repair in this case. Moreover, the simultaneously exerted low-level laser effect may modulate periodontally related cell proliferation and differentiation, leading to an enhanced wound healing and even regeneration.2 Taken together, Er:YAG laser-assisted non-surgical treatment for periodontal therapy with regular recall can effectively improve and maintain the periodontal health.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
References
- 1.Aoki A., Sasaki K.M., Watanabe H., Ishikawa I. Lasers in nonsurgical periodontal therapy. Periodontol 2000. 2004;36:59–97. doi: 10.1111/j.1600-0757.2004.03679.x. [DOI] [PubMed] [Google Scholar]
- 2.Aoki A., Mizutani K., Schwarz F. Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000. 2015;68:217–269. doi: 10.1111/prd.12080. [DOI] [PubMed] [Google Scholar]
- 3.Ishikawa I., Aoki A., Takasaki A.A. Clinical application of erbium:YAG laser in periodontology. J Int Acad Periodontol. 2008;10:22–30. [PubMed] [Google Scholar]
- 4.Chen C.K., Chang N.J., Ke J.H., Fu E., Lan W.H. Er:YAG laser application for removal of keratosis using topical anesthesia. J Dent Sci. 2013;8:196–199. [Google Scholar]
- 5.Yu C.H., Chang Y.C. Clinical efficacy of the Er:YAG laser treatment on hypersensitive dentin. J Formos Med Assoc. 2014;113:388–391. doi: 10.1016/j.jfma.2013.02.013. [DOI] [PubMed] [Google Scholar]