Abstract
Background/purpose
Tranexamic acid (TA) is one of the commonly used local hemostatic agents for dental procedures and a previous study has demonstrated a significantly lower incidence of post-procedural bleeding (PPB) in patients taking warfarin and received local TA treatment after the dental procedures than those who took warfarin and did not receive local TA treatment. However, it is still unknown whether post-procedural local TA treatment can lower the bleeding risk to the same level as individuals who do not take oral anticoagulant (OAC). The current study aimed to compare the PPB risk in patients who took OAC and received local TA treatment after the dental procedures and individuals who did not take OAC and underwent similar dental procedures.
Materials and methods
We systematically searched primary researches from two databases and four eligible cohort studies were identified. The bleeding incidence was collected from each study and the pooled odds ratio (OR) and 95% confidence interval (CI) of PPB were calculated using Mantel-Haenzel method.
Results
The analysis revealed a higher risk of PPB in patients who took OAC and received local TA treatment after the dental procedures than individuals who did not take OAC and underwent similar dental procedures with the pooled OR of 2.4, although the pooled effect estimate had a relatively wide 95% CI with non-statistically difference (0.69–8.12).
Conclusion
This study results serve as a reminder to dentists that the increased risk of PPB in those who took OAC is not entirely resolved by the local TA treatment.
Keywords: Anticoagulants, Bleeding, Dental procedure, Tranexamic acid, Warfarin
Introduction
Warfarin, a widely-used conventional oral anticoagulants (OAC), is an antagonist to vitamin K that decreases the synthesis of vitamin K-dependent clotting factors.1 The half-life of warfarin is quite long (about 40 h), and a close monitoring is required to ensure that the International Normalized Ratio (INR) is achieved in the therapeutic range.2 More recently, direct oral anticoagulants (DOACs) have been used alternatively to warfarin that does not require frequent laboratory testing. These medications work by directly inhibiting specific coagulation factors.3 For instance, factor II (thrombin) is inhibited by dabigatran, while factor Xa is inhibited by rivaroxaban, apixaban, and edoxaban.3 The main indications for warfarin and DOACs are for the stroke prevention in atrial fibrillation patients, treatment of venous thromboembolism (VTE), and VTE prophylaxis in orthopedic surgery.4 The downside of the use of OAC is the bleeding risk, especially in patients who undergo invasive procedures. In such situation, the risk of bleeding from OAC needs to be balanced with the risk of thromboembolic events from withholding the medications.
Similar to other invasive procedures, the use of OAC in patients undergoing dental procedures presents a special challenge to dentists. Tranexamic acid (TA), an antiplasmin agent that helps promoting hemostasis by preventing the proteolytic degradation of fibrin, is one of most commonly used local hemostatic agents for dental procedures.5 The efficacy of local TA treatment is well-established as a study has demonstrated that the incidence of post-procedural bleeding (PPB) was significantly lower among patients who took warfarin and received 4.8% TA mouthwash after dental procedures versus those who took warfarin and did not receive TA mouthwash after dental procedures.6 However, it is still unknown whether the administration of post-procedural local TA treatment can lower the risk of bleeding to the same level as individuals who do not take OAC which would have a significant clinical implication on how these patients should be managed after dental procedures. The present systematic review and meta-analysis was performed to compare the risk of PPB between patients who took OACs and received local TA treatment after the dental procedures and individuals who did not take OACs and underwent similar dental procedures.
Materials and methods
Data sources and searches
Two authors (DO and WO) independently searched for published articles indexed in the MEDLINE and EMBASE databases before June 2018, using search terms that consisted of anticoagulant, tranexamic acid, and dental procedures. The search terms are provided in supplementary data 1. References of the included studies were also manually reviewed to identify additional eligible studies. This study was conducted corresponding to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (supplementary data 2).7
Selection criteria and data extraction
Included studies of this meta-analysis had to be cohort studies (either prospective or retrospective) that compared the rate of post-procedural bleeding between patients who took OAC and received local TA treatment after the dental procedures and individuals who did not take OAC and underwent similar dental procedures (i.e., eligible studies must consist of two cohorts, cohort of patients who took OAC and received local TA treatment after the dental procedures and cohort of individuals who did not take OAC and underwent similar dental procedures, and must report the rate of post-procedural bleeding in both cohorts). The eligible studies were evaluated independently by the two authors. If the decisions by the authors were different, the studies in question were jointly reassessed and the final decisions were determined by consensus.
Quality assessment
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of nonrandomized studies. It is a 3-item scoring system consisted of the selection of the participants, the comparability between the groups and the ascertainment of exposure for case–control study and the outcome of interest for cohort study.8 Although a higher NOS score indicates a higher quality, it was not used as inclusion criteria for this meta-analysis.
Statistical analysis
Review Manager Software, version 5.3, from the Cochrane Collaboration (London, UK) was applied for all statistical analyses. Two authors (DO and WO) collected and tabulated all data from each study by using a standardized data collecting form. The pooled odds ratio (OR) and 95% confidence interval (CI) of PPB were calculated using Mantel-Haenzel method.9 Due to the high possibility of heterogeneity among included studies, random-effect model was preferable to fixed-effect model. Heterogeneity between the included studies were tested by using Cochran's Q test and the I2 statistic. I2-values were classified, as follows: 0%–25% demonstrated insignificant heterogeneity; 26%–50% demonstrated low heterogeneity; >50% to ≤75% demonstrated moderate heterogeneity; and, >75% demonstrated high heterogeneity.10 Publication bias was arranged to be evaluate by using funnel plot.
Results
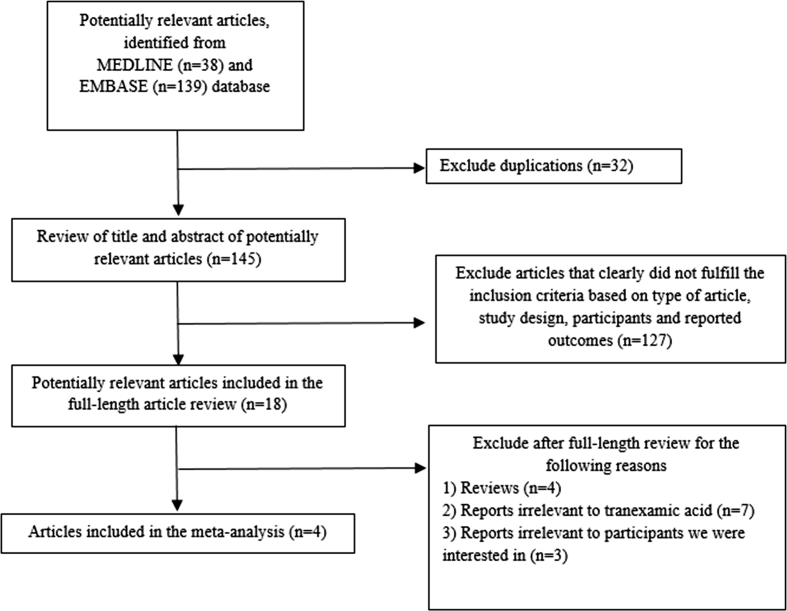
There were a total of 177 potentially relevant articles (38 articles from MEDLINE, and 139 articles from EMBASE). Thirty-two duplicated articles were excluded, and the remaining 145 articles underwent titles and abstracts review. Of those, 127 articles were excluded at this stage as they did not apparently meet the inclusion criteria's requirements. The remaining 18 articles were thoroughly reviewed and 14 articles were excluded after the full-length article review for the following reason; 4 articles were review articles, 7 articles did not use local TA treatment, and 3 articles did not recruit the participants that we were interested in, leaving four studies to be included in the meta-analysis.11, 12, 13, 14 Fig. 1 summarizes the literature review process. Clinical features and laboratory findings of the included studies and their participants as well as NOS scores are described in Table 1.
Figure 1.
The literature review process.
Table 1.
Characteristics of the included studies and their participants.
| Bacci et al.11 |
Bacci et al.12 |
Febbo et al.13 |
Gómez-Moreno et al.14 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Case (n = 451) | Comparator (n = 449) | Case (n = 50) | Comparator (n = 109) | Case (n = 261) | Comparator (n = 439) | Case (n = 18) | Comparator (n = 39) | ||
| Mean age in years (range) | 63.5 (38–89) | 66.4 (35–92) | 56.2 (41–77) | NR | 70.2 | 65.2 | 64.4 (46–73) | NR | |
| Gender | Male | 246 | 202 | NR | NR | 170 | 234 | 12 | NR |
| Female | 205 | 247 | NR | NR | 91 | 205 | 6 | NR | |
| Procedure | Dental extractions | Dental implants | Dental extractions | Dental implants | |||||
| Total number of extractions | 926 | 894 | – | – | 629 | 1049 | – | – | |
| Single extraction | 477 | 452 | – | – | 146 | 281 | – | – | |
| Multiple extractions | 449 | 442 | – | – | 115 | 158 | – | – | |
| Type of oral anticoagulant | Warfarin | – | Warfarin | – | Warfarin | – | Rivaroxaban | – | |
| INR range | 1.8–4.0 | Normal INR | 1.80–2.98 | 0.98–1.21 | Mean INR: 2.68 | – | – | Normal PT value | |
| Local hemostatic strategy | - Oxidized cellulose - Absorbable sutures - Gauzes saturated with TA for 30–40 min - Ice pack on the cheek |
- Silk sutures - Compressive gauze soaked with TA for 30–60 min - Ice pack for 6–8 h post-operatively |
(only in case group) - Irrigation socket with a 4.8% solution of TA - Oxidized cellulose - Sutures - Bite gauze-soaked TA for 30 min - Administration of 4.8% of TA mouthwash 4 times per day for 2 days |
- Non-absorbable sutures - Compression with gauzes soaked in 5% TA for 30–60 min - Ice pack for 6–8 h post-operatively |
|||||
| Number of participants with post-procedural bleeding | 7 | 4 | 2 | 3 | 9 | 0 | 1 | 2 | |
| Days after surgery that post-procedural bleeding occurred | 2–6 | 2 | 2 | 2 | 0–10 | 0 | 1 | 1 | |
| Country | Italy | Italy | Australia | Spain | |||||
| Study period | January 2006–December 2008 | NR | June 2010– June 2014 |
NR | |||||
| Study design | Prospective cohort study | Prospective cohort study | Retrospective cohort study | Prospective cohort study | |||||
| Newcastle–Ottawa scale scores | Selection: 3 Comparability: 2 Outcome: 3 |
Selection: 3 Comparability: 2 Outcome: 2 |
Selection: 2 Comparability: 2 Outcome: 1 |
Selection: 3 Comparability: 2 Outcome: 2 |
|||||
Abbreviation NR, not reported; TA, Tranexamic acid, INR, international normalized ratio.
Clinical features and laboratory findings of participants
The meta-analysis included a total of 1816 participants (780 in the OAC group, and 1036 in the no OAC group). The mean age of participants in the OAC group ranged between 56.2 and 70.6 years across the included studies.11, 12, 13, 14 More than half of the patients in the OAC group were male (58.6%)11,13,14 but male accounted for only 49.1% of participants in the no OAC group.11,13 The dental procedures in the included studies were dental extraction,11,13 and dental implants.12,14 The OAC used in three studies was warfarin11, 12, 13 while rivaroxaban was used in one study.14
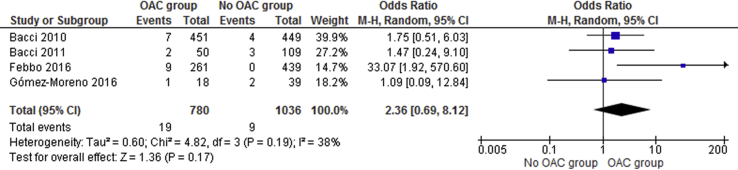
Risk of post-procedural bleeding
The pooled analysis displayed a higher risk of PPB in patients who took OAC and received local TA treatment after the dental procedures than individuals who did not take OAC and underwent similar dental procedures with the pooled OR of 2.4, although the pooled effect estimate had a relatively wide 95% CI and was not statistically significant (95% CI, 0.69–8.12). The heterogeneity of the meta-analysis was low with I2-value of 38% (Fig. 2).
Figure 2.
Forest plots comparing the odds of post-procedural bleeding among patients who took anticoagulant and received local tranexamic acid after the dental procedures versus individuals who did not take anticoagulant.
PPB in the OAC group could occur as late as 10 days after the dental procedure, whereas all PPB in the no OAC group occurred within the first two days. PPB of all participants in both groups could be controlled by re-suturing, placing oxidized cellulose over the bleeding area, or pressing compressive gauze soaked with TA on the surgical wound for an hour three times a day for 2–4 days. There was one patient in the OAC group who was hospitalized because of the bleeding and received red blood cell transfusion during the hospitalization.13
Evaluation of publication bias
Evaluation of publication bias using funnel plot was not evaluated because of only four included studies into this meta-analysis.
Discussion
A previous study has demonstrated that the use of local TA treatment after dental procedures can significantly reduce the risk of PPB in patients taking OAC. However, it is still unknown if the risk is reduced to the same level as individuals who did not take OAC. The present systematic review and meta-analysis was conducted to answer this question and found that the odds of developing PPB in patients who took OAC and received local TA treatment after the procedure was approximately 2.4 times higher than individuals who did not take OAC. Nonetheless, it should be noted that the pooled effect estimate of this meta-analysis did not reach statistical significance which was probably due to the relatively small number of primary studies included in this study.
The results of this study may serve as a reminder to dentists that the increased risk of PPB in those who took OAC is not entirely resolved by the administration of local TA treatment. Patients who take OAC and receive local TA treatment may have a lower incidence of PPB than those who take OAC and do not receive local TA treatment but the risk remains higher than individuals who do not need OAC. Therefore, special caution for PPB must still be exercised for these patients, despite the administration of local TA treatment. There are several ways to manage PPB, including re-suturing and local TA, which could be either TA mouthwash or pressing compressive gauze soaked with 4.8% or 5% TA on the surgical wound for an hour three times a day for 2–4 days. However, these methods are less convenient and patient's compliance is generally poor. A more convenient alternative is to use compressive dry gauze on sockets packed with Gelfoam impregnated with TA powder which is safe, simple and less bothersome than administration of TA mouthwash for several days.15 The major limitation lies within the relatively limited number of studies included into the meta-analysis. Even though a relatively big pooled effect estimate was observed, the result still did not reach a statistical significance. In addition, an evaluation for publication bias could not be performed and, therefore, publication bias in favor of positive studies may have been present which may have skewed the pooled effect estimate. Therefore, even the current systematic review and meta-analysis found that the odds of developing post-procedural bleeding among patients who took OAC and received local TA after the dental procedures was approximately 2.4 times higher than individuals who did not take OAC and underwent similar dental procedures, a definite conclusion still cannot be made and further studies are still needed.
Conflicts of interest
All authors declare that there are no personal or professional conflicts of interest.
Acknowledgments
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jds.2018.10.001.
Contributor Information
Duangrat Owattanapanich, Email: duangrat_tal@yahoo.com.
Patompong Ungprasert, Email: p.ungprasert@gmail.com.
Weerapat Owattanapanich, Email: weerapato36733@gmail.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.McDonald M.G., Rieder M.J., Nakano M., Hsia C.K., Rettie A.E. CYP4F2 is a vitamin K1 oxidase: an explanation for altered warfarin dose in carriers of the V433M variant. Mol Pharmacol. 2009;75:1337–1346. doi: 10.1124/mol.109.054833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuruvilla M., Gurk-Turner C. A review of warfarin dosing and monitoring. Proc (Bayl Univ Med Cent) 2001;14:305–306. doi: 10.1080/08998280.2001.11927781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rose D.K., Bar B. Direct oral anticoagulant agents: pharmacologic profile, indications, coagulation monitoring, and reversal agents. J Stroke Cerebrovasc Dis. 2018 doi: 10.1016/j.jstrokecerebrovasdis.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Gomez-Outes A., Suarez-Gea M.L., Calvo-Rojas G. Discovery of anticoagulant drugs: a historical perspective. Curr Drug Discov Technol. 2012;9:83–104. doi: 10.2174/1570163811209020083. [DOI] [PubMed] [Google Scholar]
- 5.Costa F.W., Rodrigues R.R., Sousa L.H. Local hemostatic measures in anticoagulated patients undergoing oral surgery: a systematized literature review. Acta Cir Bras. 2013;28:78–83. doi: 10.1590/s0102-86502013000100013. [DOI] [PubMed] [Google Scholar]
- 6.Ramstrom G., Sindet-Pedersen S., Hall G., Blomback M., Alander U. Prevention of postsurgical bleeding in oral surgery using tranexamic acid without dose modification of oral anticoagulants. J Oral Maxillofac Surg. 1993;51:1211–1216. doi: 10.1016/s0278-2391(10)80291-5. [DOI] [PubMed] [Google Scholar]
- 7.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 9.Borenstein M., Hedges L.V., Higgins J.P.T., Rothstein H.R. John Wiley & Sons; West Sussex: 2009. Introduction to meta-analysis. [Google Scholar]
- 10.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bacci C., Maglione M., Favero L. Management of dental extraction in patients undergoing anticoagulant treatment. Results from a large, multicentre, prospective, case-control study. Thromb Haemostasis. 2010;104:972–975. doi: 10.1160/TH10-02-0139. [DOI] [PubMed] [Google Scholar]
- 12.Bacci C., Berengo M., Favero L., Zanon E. Safety of dental implant surgery in patients undergoing anticoagulation therapy: a prospective case-control study. Clin Oral Implants Res. 2011;22:151–156. doi: 10.1111/j.1600-0501.2010.01963.x. [DOI] [PubMed] [Google Scholar]
- 13.Febbo A., Cheng A., Stein B., Goss A., Sambrook P. Postoperative bleeding following dental extractions in patients anticoagulated with warfarin. J Oral Maxillofac Surg. 2016;74:1518–1523. doi: 10.1016/j.joms.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Gómez-Moreno G., Aguilar-Salvatierra A., Fernández-Cejas E., Delgado-Ruiz R.A., Markovic A., Calvo-Guirado J.L. Dental implant surgery in patients in treatment with the anticoagulant oral rivaroxaban. Clin Oral Implants Res. 2016;27:730–733. doi: 10.1111/clr.12653. [DOI] [PubMed] [Google Scholar]
- 15.Lu S.Y., Lin L.H., Hsue S.S. Management of dental extractions in patients on warfarin and antiplatelet therapy. J Formos Med Assoc. 2018 doi: 10.1016/j.jfma.2018.08.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.