Highlights
-
•
Brain metastasis from gastric adenocarcinoma is rare and the prognosis is poor.
-
•
Brain MRI remains the key examination in the preoperative diagnosis of metastatic lesions.
-
•
Combination of SR (surgical resection) and WBRT (whole brain radiation therapy) seems to increase survival.
-
•
Clarification of physiopathologic mechanisms of metastases and new target treatments remain a challenge.
Abbreviations: WBRT, whole brain radiation therapy; SR, surgical resection; KPS, Karnofsky performance status
Keywords: Gastric cancer, Adenocarcinoma, Brain metastasis, Isolated
Abstract
Introduction
The present study reports a case of signet-ring gastric adenocarcinoma with isolated cerebellum metastasis 2 years after gastrectomy.
Presentation of a case
Brain metastases originating from gastric cancer are rare accounting for 2.1–3.3% of all brain tumors registered in Japan. There are no established therapeutic strategies for brain metastases, which accordingly have a poor prognosis. We present here a 69 year old female patient who was diagnosed with solitary cerebellum metastasis 2 years after treatment for gastric adenocarcinoma. The primary gastric cancer was treated by laparotomy with distal gastrectomy and D2 lymphadenectomy. It was diagnosed as a signet ring gastric adenocarcinoma on histopathological examination of the surgical specimen. Two years postoperatively the patient reported back to our clinic complaining of vomiting, persistent headache and instability. MRI of the head showed an enhanced tumor in the left hemisphere of cerebellum and surrounding edematous changes on T1-enhanced imaging. Given the medical history brain metastasis was the first thought in differential diagnosis. Surgical resection was chosen as treatment.
Discussion
Until recently there are only two large studies that refer to metastatic brain tumors from primary gastric cancer. Besides that, official treatment guidelines for these cases do not exist. Treatment options include surgical resection (SR), whole brain radiotherapy (WBRT), steroids, chemotherapy or a combination.
Conclusion
A solitary cerebellum metastasis from primary gastric adenocarcinoma is a very rare presentation. Early detection of metastatic lesion and successful treatment is challenging.
1. Introduction
Each year approximately 990,000 people are diagnosed with GC worldwide, of whom about 738,000 die from this disease [18], making GC the 4th most common incident cancer and the 2nd most common cause of cancer death [19]. GC also causes one of the highest cancer burdens, as measured by disability-adjusted life years lost. Adenocarcinoma constitutes the 95% of all types of gastric cancer. There are, however, other types of cancer arising from the stomach, including mucosa-associated lymphoid tissue (MALT) lymphomas, which originate from the lymphoid tissue of the stomach, and leiomyosarcomas, which arise from the muscles surrounding the mucosa. Metastases deriving from the GI tract usually concern topical or distant lymph nodes, liver, lungs and bones. Isolated brain metastasis from gastric cancer is extremely rare (<1%) and prognosis is poor. Only two large retrospective studies have been conducted until recently. The most important single institution retrospective study was conducted at M.D Anderson Cancer Center (Houston,TX,USA) between 1957 and 1997. A total of 3320 patients were diagnosed with gastric cancer and only 24 of these patients (0,7%) were observed to have brain metastases following imaging studies or autopsy. The median survival time was ˜9 weeks, and in certain patients surgical resection followed by whole-brain radiation therapy (WBRT) was associated with relatively long survival times of 54 weeks. [4] Another study conducted in Japan identified brain metastasis in only 11 out of 2322 patients (0.47%) treated for gastric cancer between 1980 and 1998. York et al. noted neurological improvement in only 4 out of 24 patients (16.7%) treated with either surgical resection with whole brain radiation therapy (WBRT) (n = 3) or WBRT alone (n = 1). Kaskura et al. reported a median survival time of 24.0 weeks in patients that had undergone surgery or surgery with WBRT compared with 10.8 weeks in patients that received WBRT alone [5]. The current study presents a rare case of gastric adenocarcinoma with cerebellum metastasis 2 years after resection for the primary lesion.
2. Case report
A 69 year old female patient, G2P2 with a clear medical history presented to our department suffering from epigastric pain, burning after food intake, nausea, vomiting and weight loss during the last two months. Patient’s diet was balanced and she had no previous history of peptic ulcer or other gastrointestinal disorders and no family history of gastric cancer. Physical examination was normal. Laboratory examinations identified anemia (Ht: 321%) and positive carcinoembryonic antigen (CEA) at 566 ng/ml (normal range, <0.5 ng/ml); all other laboratory examinations were negative. Gastric endoscopy revealed a protruding mass on the antrum of the stomach and biopsy was taken from the lesion. A computed tomography scan confirmed a gastric antrum tumor. The patient underwent distal gastrectomy with D2 lymphadenectomy, and Roux en Y gastrointestinal tract reconstruction. The histopathological examination revealed a signet-ring gastric adenocarcinoma. Post-operative course was uneventful and patient was discharged ten days later. After surgery she was subject to adjuvant chemotherapy. Annual follow-up with blood test and CT scan was suggested.
Two years later the patient reported back complaining of vomiting, persistent headache and weakness of walking. A neurological exam demonstrated instability. Magnetic resonance imaging of the head showed an enhanced tumor in the left hemisphere of cerebellum and surrounding edematous changes on T1-enhanced imaging (Fig. 1). Given the medical history the patient was diagnosed with brain metastasis of gastric cancer. Scans for other sites of metastatic disease were negative. The patient underwent stereotactic left posterior-occipital craniotomy with resection of the lesion. Pathology revealed a poorly differentiated adenocarcinoma similar with her previous gastric cancer. More specific, infiltration of cerebellum parenchyma from signet-ring cells was proven (Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6). Postoperatively the patient was able to move both arms and legs but suffered from diplopia in left eye movements. She was discharged in good general condition a few days later and a new MRI of the head was suggested in 3 months. The new MRI revealed another metastatic lesion. The physical condition and the quality of life of the patient progressively worsened and she finally died 4 months later.
Fig. 1.

MRI T1 post contrast image (gadolinium). Coronal view: 4,1 × 3,5 cm well circumscribed heterogeneously enhancing soft tissue mass in the paramedian aspect of the left cerebellum hemisphere with mild surrounding vasogenic edema.
Fig. 2.

Axial view of post contrast (gadolinium) MRI showing well circumscribed heterogeneously enhancing soft tissue mass in the left cerebellum hemisphere with mild surrounding vasogenic edema.
Fig. 3.

PDX-1 nuclear expression by neoplastic cells.
Fig. 4.

CDX-2 expression by neoplastic cells.
Fig. 5.
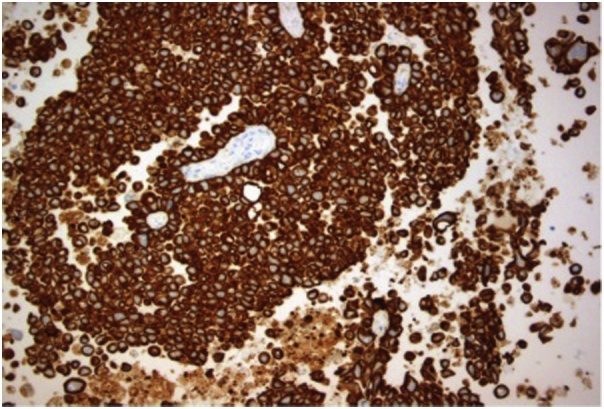
CK8.18 cytoplasmic cytokeratin expression.
Fig. 6.

Brain infiltration by metastatic gastric carcinoma composed by cell with signet ring morphology or solid neoplastic areas.
3. Discussion
Although gastric cancer incidence and mortality have dramatically fallen during the last 70 years, gastric cancer still remains the fourth most common cancer and the second leading cause of cancer-related death worldwide. According to the American Cancer Society there are 28.000 estimated new cases in 2017 and 10.960 estimated deaths. [1,2] Metastases typically occur intra- abdominaly to lymph nodes and liver or extra- abdominaly to lungs and bones. Brain metastasis from gastric cancer is quite rare especially isolated. Until today there are two large studies realized in USA and Japan respectively that refer to metastatic brain tumors from primary gastric cancer. The first one was conducted in M.D. Anderson Cancer center and included over 3000 gastric cancer cases over a 40-year period. Brain metastases were reported in only 0.7% of patients. The second included 2322 patients diagnosed with gastric cancer from 1980 to 1998 and only 11 of them (0.47%) had metastatic brain lesions [4,5]. Besides these two large series the international literature consists basically of case reports.
For the moment there are no official guidelines for the treatment of patients suffering from gastric cancer with brain metastasis. Treatment options include surgical resection (SR), brain radiotherapy, steroids, chemotherapy or a combination. [7,8,12]. Bartlelt et al. realized a retrospective study in nine hundred and sixteen patients with brain metastases from the GI tract, treated with WBRT between 1985 and 2000.
According to this study the independent factors correlated with a better prognosis were a KPS > 70 and the presence of a solitary brain metastasis. [8].So the selection of treatment modality depends on these factors. In the M.D Anderson Cancer Center York et al. reported a median survival of 54 weeks (range, 22–83 weeks) in patients with gastric cancer with brain metastases who underwent surgical resection, whole brain radiotherapy (WBRT) and steroid therapy. In retrospective analyses WBRT or Steroid therapy as monotherapies seem to have similar results.
4. Conclusions
Prognosis of gastric cancer patients who present with brain metastasis is poor and treatment is palliative [3,6,11]. Treatment options include SR, WBRT, steroids, chemotherapy or a combination. Combination of surgical resection and WBRT seems to increase survival. We treated our patient only with SR as unfortunately her general condition quickly deteriorated. Clarification of physiopathologic mechanisms of metastases and new target treatments remain a challenge.
Conflict of interests
The authors have no conflicts of interest to disclose.
Funding
There is no funding source.
Ethical approval
Case reports do not require Ethical approval from the Ethical Committee in our Hospital.
Consent
Informed consent for the publication of this work has been taken by the patient.
Author contribution
KA: Treated the patient, collected the data, wrote and revised the paper
TN: Treated the patient, read and approved the paper.
EI: Interpretated the data.
VK: Read and approved the paper.
SP: Designed the study, read and approved the paper.
FD: Concept of the study,and revised the paper.
Research studies
The present work is a case report and does not need Registration.
Guarantor
Kostoglpu Aikaterini is the Guarantor.
Provenance and peer review
Not commissioned, externally peer reviewed.
References
- 1.Siegel Rebecca L., Miller Kimberly D., Jemal Ahmedin. Cancer statistics, 2017. CA Cancer J. Clin. 2017;(67):7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2.WHO . Globocan; 2012. Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012.http://globocan.iarc.fr/Default.aspx Available online: [Google Scholar]
- 3.Philip A.Z., Namakydoust A., Varilla V.M., Macatangay C., Dowsett R., Tannenbaum S.H. Late recurrence of gastric cancer with isolated brain metastasis. Transl. Gastroenterol. Hepatol. 2016;1(61) doi: 10.21037/tgh.2016.07.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.York J.E., Stringer J., Ajani J.A. Gastric cancer and metastasis to the brain. Ann. Surg. Oncol. 1999;6:771–776. doi: 10.1007/s10434-999-0771-3. [DOI] [PubMed] [Google Scholar]
- 5.Hashimoto K., Narita Y., Miyakita Y. Comparison of clinical outcomes of surgery followed by local brain radiotherapy and surgery followed by whole brain radiotherapy in patients with single brain metastasis: single-center retrospective analysis. Int. J. Radiat. Oncol. Biol. Phys. 2011;81:e475–80. doi: 10.1016/j.ijrobp.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Tamura S., Takeno A., Miki H. Clinical outcomes in patients with brain metastasis from gastric cancer. Gan To Kagaku Ryoho. 2011;38:2093–2096. [PubMed] [Google Scholar]
- 7.Zhang S., Wang M., Xue Y.H., Chen Y.P. Cerebral metastasis from hepatoid adenocarcinoma of the stomach. World J. Gastroenterol. 2007;13:5787–5793. doi: 10.3748/wjg.v13.i43.5787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartelt Susanne, Momm Felix. Christian Weissenberger, and Johannes Lutterbach Patients with brain metastases from gastrointestinal tract cancer treated with whole brain radiation therapy: prognostic factors and survival. World J. Gastroenterol. 2004;10(November (22)):3345–3348. doi: 10.3748/wjg.v10.i22.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nomura T., Yoshikawa T., Kato H. Early gastric cancer manifested as brain metastasis: report of a case. Surg. Today. 1997;27:334–336. doi: 10.1007/BF00941808. [DOI] [PubMed] [Google Scholar]
- 12.Katsunobu S., Kazuya M., Akihiro M., Takahiro T. Early gastric cancer with suspected brain metastasis arising eight years after curative resection: a case report. BMC Res. Notes. 2014;7(818) doi: 10.1186/1756-0500-7-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jemal A., Center M.M., DeSantis C., Ward E.M. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol. Biomark. Prev. 2010;19:1893–1907. doi: 10.1158/1055-9965.EPI-10-0437. [DOI] [PubMed] [Google Scholar]
- 19.Soerjomataram I., Lortet-Tieulent J., Parkin D.M., Ferlay J., Mathers C., Forman D. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012;380:1840–1850. doi: 10.1016/S0140-6736(12)60919-2. [DOI] [PubMed] [Google Scholar]


