Abstract
Background
Previous studies have demonstrated that acupuncture was an effective alternative for treating major depressive disorders. However, the use of acupuncture for the treatment of postpartum depression remains controversial. This review summarizes the most significant studies in the area of acupuncture treatment for postpartum depression and provides a detailed overview of the efficacy of acupuncture for the treatment of postpartum depression.
Methods
We undertook a systematic review of publicly available electronic databases to identify studies that evaluated acupuncture for the treatment of postpartum depression. Our meta-analysis selected randomized controlled trials (RCTs) and quasi-RCTs that reported on the treatment effect of acupuncture on postpartum depression.
Results
Eight prospective trials reporting data on postpartum depression were included in our meta-analysis. The results demonstrated that acupuncture treatment could significantly reduce HAMD scores (SMD: -1.08; 95%CI: -2.11 to -0.05; P=0.040). However, with regard to EPDS, clinical response, and serum estradiol levels, pooled analysis suggested no beneficial effects of acupuncture for postpartum women in EPDS (RR: 1.23; 95%CI: 0.90 to 1.67; P=0.195); clinical response (RR: 1.00; 95%CI: 0.89 to 1.12; P=0.969); and the levels of serum estradiol (SMD: 1.96; 95%CI: -0.01 to 3.93; P=0.051).
Limitations
First, there was relatively high heterogeneity among the studies, except for clinical response. In order to identify the sources of heterogeneity, we divided the studies into subgroups by way of controls. However, heterogeneity still existed, which suggested that it arose from participants rather than controls. Second, the sample size of the studies was small, causing the power of summary results to be low. This may result in over- or underestimating the interpretation of the results. Third, our analysis used pooled data, which restricted us from performing a more detailed analysis.
Conclusions
Our meta-analysis suggested that acupuncture treatment may reduce HAMD scores, while no significant effects on EPDS, clinical response, and serum estradiol levels were observed.
1. Introduction
Postpartum depression is a type of mood disorder associated with childbirth, and onset usually begins between day one and four months after delivery [1]. The clinical manifestations of postpartum depression include low energy, extreme sadness, irritability, and suicidal tendencies. Postpartum depression can also lead to subtle negative effects on the newborn child, which may result in a higher incidence of violence during adolescence or adulthood [2].
Given the high prevalence and potentially negative consequences of postpartum depression, it is critical to develop effective treatment strategies for patients with postpartum depression. Currently, the standard therapeutic method for depression is pharmacotherapy. However, most postpartum women are reluctant to take antidepressants due to their potential side effects [3]. Additionally, women with postpartum depression are reluctant to receive psychological and behavioral therapies [4]. Alternative treatment strategies for postpartum depression are gaining prominence, especially acupuncture, and has gained acceptance due to its efficacy and safety.
Previous meta-analysis has demonstrated that acupuncture is a safe and effective treatment for depressive disorders [5, 6]. Furthermore, it is well tolerated and has demonstrated potential anti-depression efficacy in pregnant women [7]. Though several studies have investigated the efficacy of acupuncture on postpartum depression, several of these studies showed inconsistencies in their efficacy. There is a need to determine the efficacy of acupuncture particularly in women with postpartum depression. In this context, we conducted a systematic review and meta-analysis on published studies to evaluate the efficacy of acupuncture treatment for postpartum depression.
2. Materials and Methods
2.1. Sources
This review and meta-analysis was conducted according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Statement (Checklist S1) [8]. We searched PubMed, EmBase, Cochrane Library, ClinicalTrials.gov, China National Knowledge Infrastructure, and Wanfang electronic databases for articles published through September 1st, 2018.
2.2. Study Selection
Randomized controlled trials (RCTs) or quasi-RCTs that investigated the effect of acupuncture on postpartum depression women were selected for this study. No limitations were placed on language or publication status (published, in press, or in progress). Keywords and phrases used for queries included “puerperal depression”, “postnatal depression”, “postpartum depression”, “puerperium depression”, “acupuncture”, and “electroacupuncture”. Additionally, we conducted manual searches of the reference lists from all relevant original and review articles to identify additional qualified studies. The study topic, study design, participant's status, intervention, controls, and outcome variables of these studies were used to identify potentially relevant studies.
The literature search was independently handled by two of the authors using the standardized approach. Any inconsistencies during the literature search were scrutinized against the following inclusion criteria: (1) randomized control or quasi-randomized control design was essential; (2) all women were diagnosed with postpartum depression; (3) patients received either acupuncture or traditional therapies; (4) available data concerns the effective rate of acupuncture treatment for extraction; (5) the diagnosis criteria of postpartum depression were based on the International Classification of Diseases (ICD), Chinese Classification of Mental Disorders (CCMD), or the Diagnostic and Statistical Manual of Mental Disorders (DSM). Additionally, the major exclusion criteria were as follows: (1) no available data regarding HAMD scores, EPDS, clinical response, and the levels of serum estradiol; (2) non-case-control studies, case reports, letters, reviewed editorial articles; (3) duplicated publications with previous studies.
2.3. Data Collection and Quality Assessment
The collected data comprised the methods and outcome results, the diagnostic instruments and efficacy assessments, treatment regime (monotherapy or additional therapy), controlled conditions (antidepressants and sham acupuncture), and treatment duration. Treatment outcomes were categorized as dichotomous or continuous data. Any adverse effects were noted if they were reported during the meta-analysis. Dichotomous data were mainly response rates, which were generally defined as an improvement in scores on depressive scales or clinical symptoms from baseline to endpoint for acupuncture and controlled groups. Continuous data were baseline-to-endpoint changes in scores on depressive scales that were derived from the Hamilton Rating Scale for Depression (HAMD), Edinburgh Postnatal Depression Scale (EPDS), and serum estradiol levels. Judgments on the methodological qualities of included trials using the Cochrane criteria guidelines [9] were based on the following subscales: concealment of randomization, patients blinding, healthcare providers blinded, data collectors blinded, outcome assessors blinded, and the use of intention-to-treat analysis (Table 2). The data extraction and quality assessments were conducted independently by two of the authors. Any disagreements in assessing the studies were further scrutinized using the above criteria until a consensus was reached.
Table 2.
Assessment for risk of bias in the randomized clinical trials.
| Study | Concealment of Randomization | Patients Blind | Healthcare Providers Blinded | Data Collectors Blinded | Outcome Assessors Blinded | Intention-to-treat analysis |
|---|---|---|---|---|---|---|
| Chen 2010 [21] | Yes | No | No | No | No | Yes |
| Xi 2015 [22] | Yes | No | No | No | No | Yes |
| Ai 2013 [23] | Yes | No | No | No | No | Yes |
| Yu 2015 [24] | Yes | No | No | No | No | Yes |
| Dou 2016 [25] | NA | No | No | No | No | Yes |
| Chen 2007 [26] | NA | No | No | No | No | No |
| Chung 2012 [27] | Yes | Yes | No | NA | NA | Yes |
| Xu 2013 [28] | Yes | No | No | No | No | NA |
2.4. Statistical Analysis
Dichotomous and continuous data were analysed with risk ratio (RR) and standard mean difference (SMD) with 95% confidence intervals (95% CIs) using the random-effects model. The assumptions made were that the true underlying effect varied among the included trials [10, 11]. Heterogeneity between the studies was investigated using Q statistic, and P values < 0.10 were considered as indicative of significant heterogeneity [12, 13]. Sensitivity analysis was conducted by removing each trial from the overall analysis [14], and subgroup analysis was conducted based on the controls. Visual inspections of funnel plots were performed, and the Egger [15] and Begg [16] tests were used for quantitative evaluate publication bias. All reported P values were 2-sided, and P values < 0.05 were considered statistically significant for all included studies. Statistical analyses were performed using STATA software (version 10.0; Stata Corporation, College Station, TX, USA).
3. Results
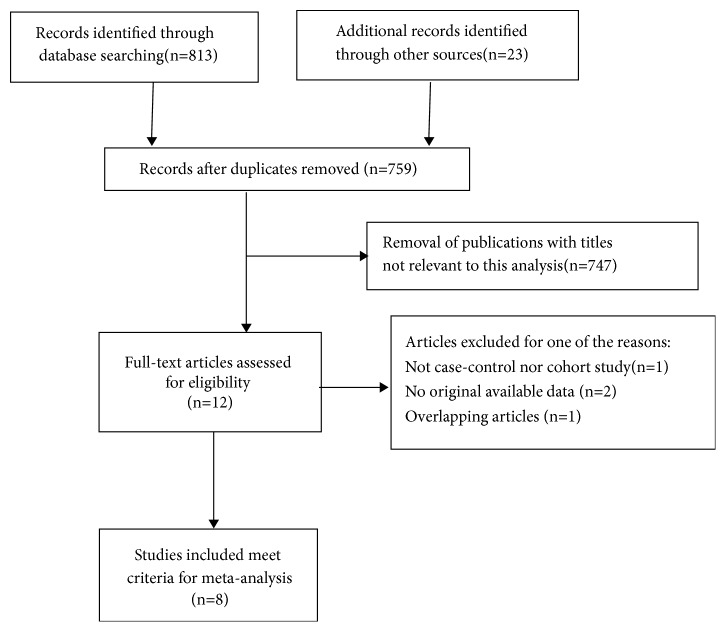
As shown in Figure 1, a total of 759 potentially useful relevant studies regarding the effect of acupuncture treatment for postpartum depression were initially identified. After screening titles and abstracts of the relevant articles, 747 articles were excluded because they did not meet the inclusion criteria. Afterwards, twelve potentially eligible studies were selected. Upon detailed evaluation, two studies had additional therapeutic benefits for acupuncture on postpartum women [17, 18]. Participants on one of the studies comprised pregnant women and one study did not report primary outcomes [19, 20]. After selection, eight prospective trials were selected for the final meta-analysis [21–28]. A manual search of the reference lists of these studies did not yield any new eligible studies.
Figure 1.
Flow schematic depicting the procedure for retrieving literature and selection of studies.
In this meta-analysis, a total of 517 participants were selected. All of the patients were diagnosed with postpartum depression according to CCMD-III, HAMD, or DSM-IV criteria, except for two where clinical symptoms were used as the diagnostic criteria [24]. Dou et al. failed to report their diagnosis criteria in their studies [25]. Three of these studies compared acupuncture monotherapy to antidepressants [21, 24, 26], while there were two cohorts that compared acupuncture along with psychological therapy versus antidepressants [23, 25]. There was another study that set electroacupuncture as the intervention with sham acupuncture as the control [27]. Five of these eight selected studies reported clinical response as the outcome [25]. In addition, five studies reported HAMD as the primary parameter used to determine acupuncture treatment efficacy [21–24, 26] (Table 1). The results of the bias within the selected trials are listed in Table 2.
Table 1.
Characteristics of the selected studies used in the meta-analysis.
| Authors | Sample size | Diagnostic Criteria | Intervention | Controls | Outcomes |
|---|---|---|---|---|---|
| Chen 2010 [21] | 52 | CCMD-III, HAMD | Acupuncture | Antidepressant (Fluoxetine) | Clinical Response, HAMD, Estradiol |
| Xi 2015 [22] | 104 | CCMD-III, HAMD | Acupuncture | Psychological therapy | HAMD, Estradiol |
| Ai 2013 [23] | 70 | CCMD-III | Acupuncture and psychological therapy | Antidepressant (Citalopram) | Clinical Response, HAMD, EPDS |
| Yu 2015 [24] | 60 | Clinical Symptoms | Acupuncture | Antidepressant (Fluoxetine) | HAMD |
| Dou 2016 [25] | 80 | Unknown | Acupuncture and psychological therapy | Antidepressant (Fluoxetine) | Clinical Response, EPDS |
| Chen 2007 [26] | 41 | DSM-IV | Acupuncture | Antidepressant (Probucil) | Clinical Response, HAMD |
| Chung 2012 [27] | 20 | DSM-IV, HDRS17 | Electroacupuncture | Sham acupuncture | Clinical Response, EPDS, |
| Xu 2013 [28] | 90 | DSM-IV | Acupuncture | Placebo | EPDS, Estradiol |
HAMD: Hamilton Rating Scale for Depression; EPDS: Edinburgh Postnatal Depression Scale.
3.1. Quantitative Synthesis Results
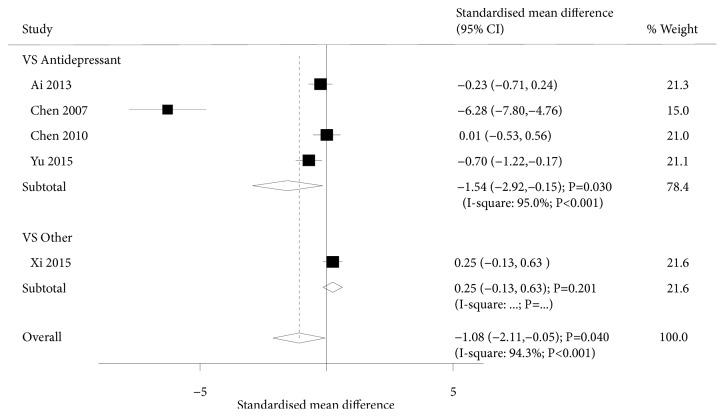
A total of 5 trials investigated the effect of acupuncture on HAMD scores in our meta-analysis. The summary results suggested that acupuncture was associated with lower levels of HAMD scores (SMD: -1.08; 95%CI: -2.11 to -0.05; P=0.040; Figure 2) despite significant heterogeneity being observed (P<0.001). Sensitivity analysis suggested that the pooled results were variable due to the small number of included trials. Subgroup analysis suggested that acupuncture significantly reduced the levels of HAMD scores compared to antidepressant drugs (SMD: -1.54; 95%CI: -2.92 to -0.15; P=0.030). However, there were no significant differences between acupuncture and non-drug intervention for HAMD scores (SMD: 0.25; 95%CI: -0.13 to 0.63; P=0.201).
Figure 2.
Forest plot displaying the overall effect of acupuncture versus controls in the Hamilton Rating Scale for Depression (HAMD).
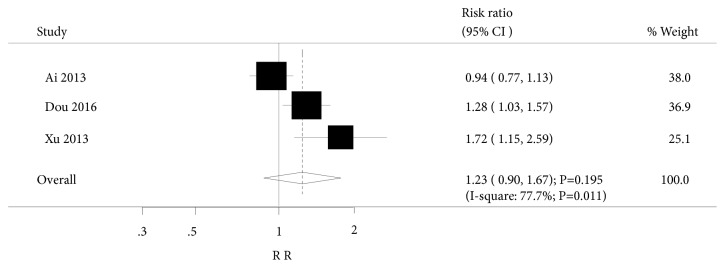
In addition, three trials in our meta-analysis investigated the effect of acupuncture on EPDS, and two trials of these included studies compared acupuncture with antidepressants, while one compared acupuncture with placebo. Pooled analysis suggested no beneficial effects of acupuncture were observed in postpartum women (RR: 1.23; 95%CI: 0.90 to 1.67; P=0.195; Figure 3) and were associated with higher heterogeneity (I2=77.7%; P=0.011). Additionally, subgroup analysis suggested that acupuncture was associated with a higher incidence of EPDS when compared to placebo (RR: 1.72; 95%CI: 1.15 to 2.59; P=0.009). This effect was not observed when compared to antidepressant drugs (RR: 1.09; 95%CI: 0.80 to 1.48; P=0.585).
Figure 3.
Forest plot displaying the overall effect of acupuncture versus controls in Edinburgh Postnatal Depression Scale (EPDS).
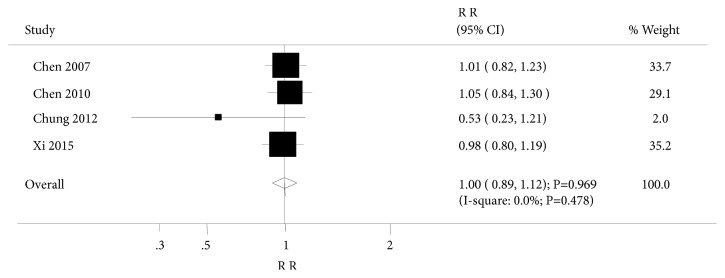
Four trials investigated the effect of acupuncture on clinical response. Summary results suggested no significant differences between acupuncture and controls for clinical response (RR: 1.00; 95%CI: 0.89 to 1.12; P=0.969; Figure 4). There was no evidence of heterogeneity across the studies. After sequential exclusion of every study, none of the studies affected the pooled analysis. Subgroup analysis was based on control types and consistent with the overall analysis results.
Figure 4.
Forest plot displaying the overall effect of acupuncture versus controls for clinical response.
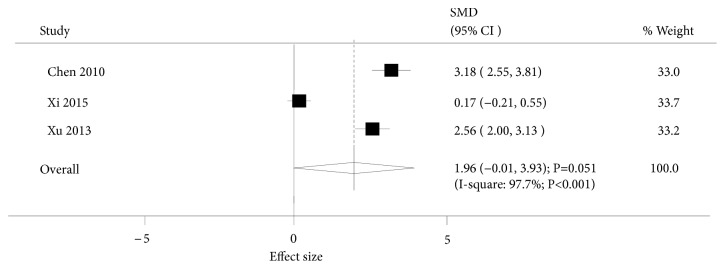
Three trials investigated the effect of acupuncture on serum estradiol levels. Pooled analysis results indicated that there was no association between acupuncture and the levels of serum estradiol (SMD: 1.96; 95%CI: -0.01 to 3.93; P=0.051; Figure 5). However, subgroup analysis suggested that women who received acupuncture treatment were associated with higher levels of serum estradiol (SMD: 3.18; 95%CI: 2.55 to 3.81; P<0.001) compared to women on antidepressant drugs. Conversely, no differences were observed when compared to women who did not receive drug intervention (SMD: 1.36; 95%CI: -0.99 to 3.70; P=0.257).
Figure 5.
Forest plot displaying the overall effect of acupuncture versus controls for serum estradiol levels.
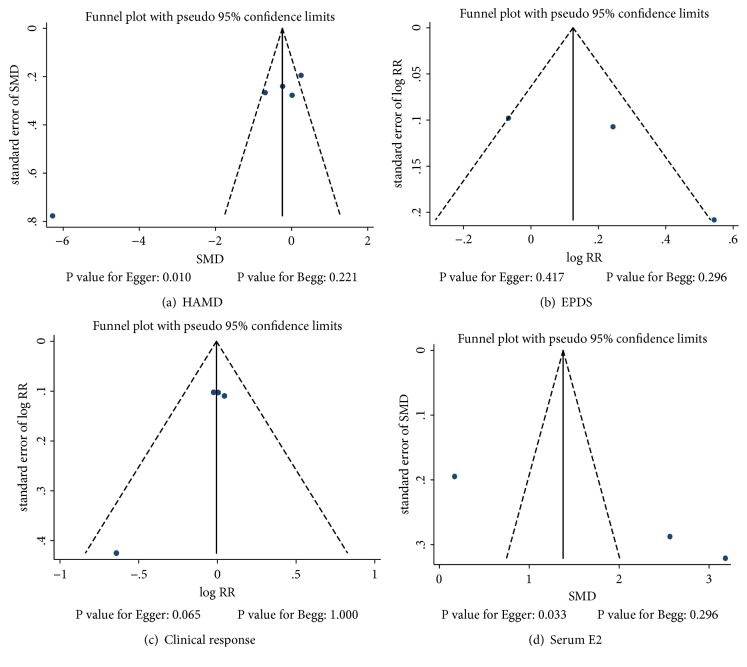
Review of the funnel plots could not rule out potential publication bias for HAMD scores, EPDS, clinical response, or serum estradiol levels (Figure 6). However, we did note potential evidence of publication bias for HAMD scores using Egger test (P=0.010). There was no evidence of publication bias for EPDS using Egger test. The Egger test showed potential publication bias (P=0.065) and potential evidence of publication bias for serum estradiol levels (P=0.033).
Figure 6.
Funnel plots for Hamilton Rating Scale for Depression (HAMD), Edinburgh Postnatal Depression Scale (EPDS), clinical response, and serum estradiol levels.
4. Discussion
Growing evidence has demonstrated the beneficial effect of acupuncture treatment for postpartum depression. A previous meta-analysis [6] suggested that acupuncture had a significantly greater overall effective rate compared to controls. Moreover, acupuncture significantly increased estradiol levels compared to controls. Regarding HAMD and EPDS scores, no differences were observed between the two groups. However, due to the limited number of participants, such associations remain controversial. Therefore, we aimed to further investigate the association between the effect of acupuncture treatment and postpartum depression in this meta-analysis. Our meta-analysis demonstrated that acupuncture could significantly reduce HAMD scores in postpartum women, but no additional benefits from acupuncture treatment were observed when compared to conventional treatments. The treatment effects of acupuncture on postpartum depression differed when compared to different controls. Subgroup analysis suggested that acupuncture could significantly reduce the levels of HAMD scores, and higher levels of serum estradiol were observed in acupuncture treated versus patients prescribed antidepressant drugs. Furthermore, acupuncture significantly increased the incidence of EPDS as compared to placebo. Unlike the efficacy of acupuncture on other depression diseases such as major depressive disorder and post-stoke depression or even depression related insomnia [29], the treatment efficacy of acupuncture on postpartum women was lower compared to other treatment methods.
More than half the selected studies (5/8) [21, 24, 27] reported on the details of randomization before treatment. Only one study performed allocation concealment, while the majority of the trials did not involve allocation information [27]. This uncertainty may lead to a bias for selection and detection and could have a negative consequence on interpreting the strength of the results. In addition, there was difficulty in utilizing the double-blind method to carry out acupuncture treatment; however, the sham needle acupuncture method could have been a viable alternative. In addition to these complications in interpreting the data, loss of follow-up of the participants happened in two studies.
Our meta-analysis showed that the overall effects of acupuncture were similar to other treatment methods when the data was summarized as absolute mean differences. Continuous data had higher variability than expected. Hence, SMD was used to evaluate the treatment efficacy of acupuncture. Several studies have reported inconsistent results in their summaries, which made the analysis more complicated. Ai et al. reported that there were no significant differences between acupuncture and psychotherapy versus antidepressant drugs for HAMD and EPDS; however, they maintained that combining acupuncture with psychotherapy would be regarded as an effective alternative treatment strategy [23]. Chen et al. suggested there were no significant differences between acupuncture and antidepressant drug treatment for HAMD levels; however they indicated that women who received acupuncture had a lower risk of adverse events [21]. Xi et al. reported no significant differences between acupuncture and psychotherapy in HAMD or serum estradiol levels. However, they suggested that combining acupuncture with psychotherapy would result in higher HADM, lower self-rating depression scale scores, and self-rating anxiety scale scores [22]. Dou et al. reported that women who received acupuncture had significant increase in the incidence of EPDS, but critical data was missing in their report to verify their conclusions [25]. The findings of the study conducted by Xu et al. were consistent with Dou et al. [28]. Although our analysis suggested no relationship between acupuncture and serum estradiol levels, two of the included trials reported higher levels of serum estradiol in women who received acupuncture. Previous studies had reported acupuncture treatment would result in the increase of estradiol levels. However, Xi et al. showed no such differences observed in their study [22], which may be due to the differences in the interventional or control groups.
Though our meta-analysis revealed that acupuncture had a lower efficacy compared to other antidepression treatments, symptoms of depression relief were observed in the majority of the studies analysed. These findings indicate that although the efficacy of acupuncture was lower compared to antidepressants, the benefits of acupuncture were still attractive to women with postpartum depression due to their negligible side-effects.
There were several limitations to our study: first, there was relative high heterogeneity among the studies, except for clinical response. We divided the studies into subgroups by way of controls in order to identify sources of heterogeneity. Heterogeneity still existed, suggesting that the source of heterogeneity could be due to participant selection rather than the controls. Second, the sample size of the studies was small, causing the power of summary results to be lower. This would result in over- or underestimating the interpretation of the results. Third, unpublished studies would likely include increased proportions of negative results, but by definition we were not aware of them and could not include them here. In addition, our analysis used pooled data, which restricted us from performing a more detailed analysis.
5. Conclusions
In summary, despite the limitations mentioned above, this current systematic review suggests that acupuncture could reduce HAMD scores. However, EPDS, clinical response, and serum estradiol levels were unaffected by acupuncture treatment. Furthermore, our analysis revealed that treatment efficacy was variable and depended on the control types used. Large-scale and well-designed RCTs are required before a conclusive statement could be made regarding the efficacy of acupuncture for the treatment of postpartum depression.
Acknowledgments
The study was partly supported by a grant awarded by the National Natural Science Foundation of China (No. 81704145), Shanghai Municipal Commission of Health and Family Planning (No. 201640026), and Shanghai Hospital Development Center (No. SHDC12016124).
Contributor Information
Lixing Lao, Email: lxlao1@hku.hk.
Shifen Xu, Email: xu_teacher2006@126.com.
Data Availability
The datasets supporting our results are included within this article.
Conflicts of Interest
The authors declare no conflicts of interest regarding the publication of this paper.
References
- 1.Lee D., Yip A., Chiu H., Leung T., Chung T. A psychiatric epidemiological study of postpartum Chinese women. The American Journal of Psychiatry. 2001;158(2):220–226. doi: 10.1176/appi.ajp.158.2.220. [DOI] [PubMed] [Google Scholar]
- 2.O'Hara M. W., McCabe J. E. Postpartum depression: current status and future directions. Annual Review of Clinical Psychology. 2013;9:379–407. doi: 10.1146/annurev-clinpsy-050212-185612. [DOI] [PubMed] [Google Scholar]
- 3.Cameron E. E., Hunter D., Sedov I. D., Tomfohr-Madsen L. M. What do dads want? Treatment preferences for paternal postpartum depression. Journal of Affective Disorders. 2017;215:62–70. doi: 10.1016/j.jad.2017.03.031. [DOI] [PubMed] [Google Scholar]
- 4.Milgrom J., Danaher B. G., Gemmill A. W., et al. Internet cognitive behavioral therapy for women with postnatal depression: A randomized controlled trial of MumMoodBooster. Journal of Medical Internet Research. 2016;18(3):p. e54. doi: 10.2196/jmir.4993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang Z.-J., Chen H.-Y., Yip K.-C., Ng R., Wong V. T. The effectiveness and safety of acupuncture therapy in depressive disorders: systematic review and meta-analysis. Journal of Affective Disorders. 2010;124(1-2):9–21. doi: 10.1016/j.jad.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Li S., Zhong W., Peng W., Jiang G. Effectiveness of acupuncture in postpartum depression: A systematic review and meta-analysis. Acupuncture in Medicine. 2018;36(5):295–301. doi: 10.1136/acupmed-2017-011530. [DOI] [PubMed] [Google Scholar]
- 7.Ormsby S. M., Smith C. A., Dahlen H. G., Hay P. J., Lind J. M. Evaluation of an antenatal acupuncture intervention as an adjunct therapy for antenatal depression (AcuAnteDep): Study protocol for a pragmatic randomised controlled trial. Trials. 2016;17(1) doi: 10.1186/s13063-016-1204-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moher D., Liberati A., Tetzlaff J., Altman D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine. 2009;6(7) doi: 10.1371/journal.pmed.1000097.e1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Higgins J., Altman D. G. Assessing risk of bias in included studies. In: Higgins J., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.1. Oxford, UK: Cochrane Collaboration; 2008. [Google Scholar]
- 10.DerSimonian R., Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 11.Ades A. E., Lu G., Higgins J. P. T. The interpretation of random-effects meta-analysis in decision models. Medical Decision Making. 2005;25(6):646–654. doi: 10.1177/0272989X05282643. [DOI] [PubMed] [Google Scholar]
- 12.Deeks J. J., Higgins J. P. T., Altman D. G. Analyzing data and undertaking meta-analyses. In: Higgins J., Green S., editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.1. Oxford, UK: The Cochrane Collaboration; 2008. (chapter 9). [Google Scholar]
- 13.Higgins J. P. T., Thompson S. G., Deeks J. J., Altman D. G. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tobias A. Assessing the influence of a single study in meta-analysis. Stata Tech Bull. 1999;47:15–17. [Google Scholar]
- 15.Egger M., Smith G. D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Begg C. B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 17.Zhang F., Zou W., Sun X., et al. Clinical observation of treating postpartum depression by musical electroacupuncture combined witll wuzang yumu matching acupoint. Journal of Clinical Acupuncture Medicine. 2016;32:44–46. [Google Scholar]
- 18.Li Z. The clinical research of Zangshi Wuyin Xiangtiao acupuncture treatment for postpartum depression. Jilin Journal of Traditional Chinese Medicine. 2015;35:88–90. [Google Scholar]
- 19.Manber R., Schnyer R. N., Allen J. J. B., Rush A. J., Blasey C. M. Acupuncture: A promising treatment for depression during pregnancy. Journal of Affective Disorders. 2004;83(1):89–95. doi: 10.1016/j.jad.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Xu F., Tang Q. Effect of renal aeration for the syndromes of postpartum depression nephrotic symdrome. Beijing Journal of Traditional Chinese Medicine. 2016;35:72–75. [Google Scholar]
- 21.Chen J., Zhang J., Pei Y. Effect of acupuncture for postpartum depression. Chinese Journal of Information on TCMvol. 2010;17:77–78. [Google Scholar]
- 22.Xi Y., Wang Y. Effect of acupuncture plus psychological intervention on 5-ht,ofq and e2 in patients with postpartum depression. Shanghai Journal of Acu-Mox. 2015;34:947–950. [Google Scholar]
- 23.Ai X. Therapeutic observation on acupuncture plus psychotherapy for postiartum depression. Shanghai Journal of Acupuncture and Moxibustion. 2013;32:711–712. [Google Scholar]
- 24.Yu S., Li X., Feng X. Therapeutic efficacy of acupuncture at the thirteen ghost points for postpartum depression and its effect on the quality of life. Shanghai Journal of Acu-Mox. 2015;34:14–16. [Google Scholar]
- 25.Dou Y. Effect of combined acupuncture and psychological intervention for postpartum depression. Maternal and child in the world 2016. 2016;33 [Google Scholar]
- 26.Chen H. Effectiveness Back-shu and Front-mu Network Points Therapy for Postpartum Depression: of A Clinical Study. Heilongjiang Chinese Medicine University; 2007. [Google Scholar]
- 27.Chung K.-F., Yeung W.-F., Zhang Z.-J., et al. Randomized non-invasive sham-controlled pilot trial of electroacupuncture for postpartum depression. Journal of Affective Disorders. 2012;142(1–3):115–121. doi: 10.1016/j.jad.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 28.Xu F. Clinical research of postpartum depression treated with xiaoyaosan, acupuncture and moxibustion. World Journal of Integrated Traditional and Western Medicin. 2013;8:896–899. [Google Scholar]
- 29.Dong Bo, Chen Zeqin, Yin Xuan, et al. The efficacy of acupuncture for treating depression-related insomnia compared with a control group: a systematic review and meta-analysis. BioMed Research International. 2017;2017:11. doi: 10.1155/2017/9614810.9614810 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting our results are included within this article.