Abstract
Obesity is a worldwide epidemic that carries significant morbidity and mortality. There are many weight loss strategies available, yet to this date, none are risk-free. Intragastric balloons have been used for decades as a temporary measure for weight reduction and can be a useful approach for specific patients. Serious complications related to the device remain rare; however, prompt intervention is usually needed when they arise. We present the case of a 38-year-old female patient, she was using an intragastric balloon to treat her obesity. Regretfully, the balloon deflated causing intestinal migration and obstruction. After a successful surgery, the patient completely recovered.
INTRODUCTION
Obesity has a major impact on both the duration and quality of life of patients, prompting the development of numerous treatments [1, 2]. Surgical and non-surgical approaches are available to treat obese and overweight patients, and although these strategies can greatly improve their quality of life, they can be associated with life-threatening complications [2–4].
We present a case of a patient who suffered bowel obstruction due to the migration of a deflated intragastric balloon. After an adequate surgical intervention, patient fully recovered.
CASE REPORT
The patient is a 38-year-old female with past medical history of obesity, for which she was treated with a saline-filled intragastric balloon 5 months prior. The patient’s initial body mass index (BMI) was 33.18, and during this time, she had lost 12 kg of weight, reaching a BMI of 31.85. She presented to the emergency room with a 4-day history of lower abdominal pain, nausea and severe vomiting. She also reported that she was unable to pass gas or stool. On clinical examination she was found to be dehydrated and tachycardic, her abdomen was distended and she had generalized abdominal tenderness. On auscultation, tinkling bowel sounds associated with gurgles and rushes were identified. After adequate reanimation, a CBC (complete blood count) revealed leukocytosis and neutrophilia, and a contrast-enhanced abdominal computed tomography (CT) unveiled a 10 × 2 × 1.5 cm3 metallic foreign body located in the lumen of the terminal ileum and the cecum. The intestinal loops proximal to the ileum were dilated, showing clear signs of bowel obstruction proximal to the aforementioned foreign body (Fig. 1).
Figure 1:
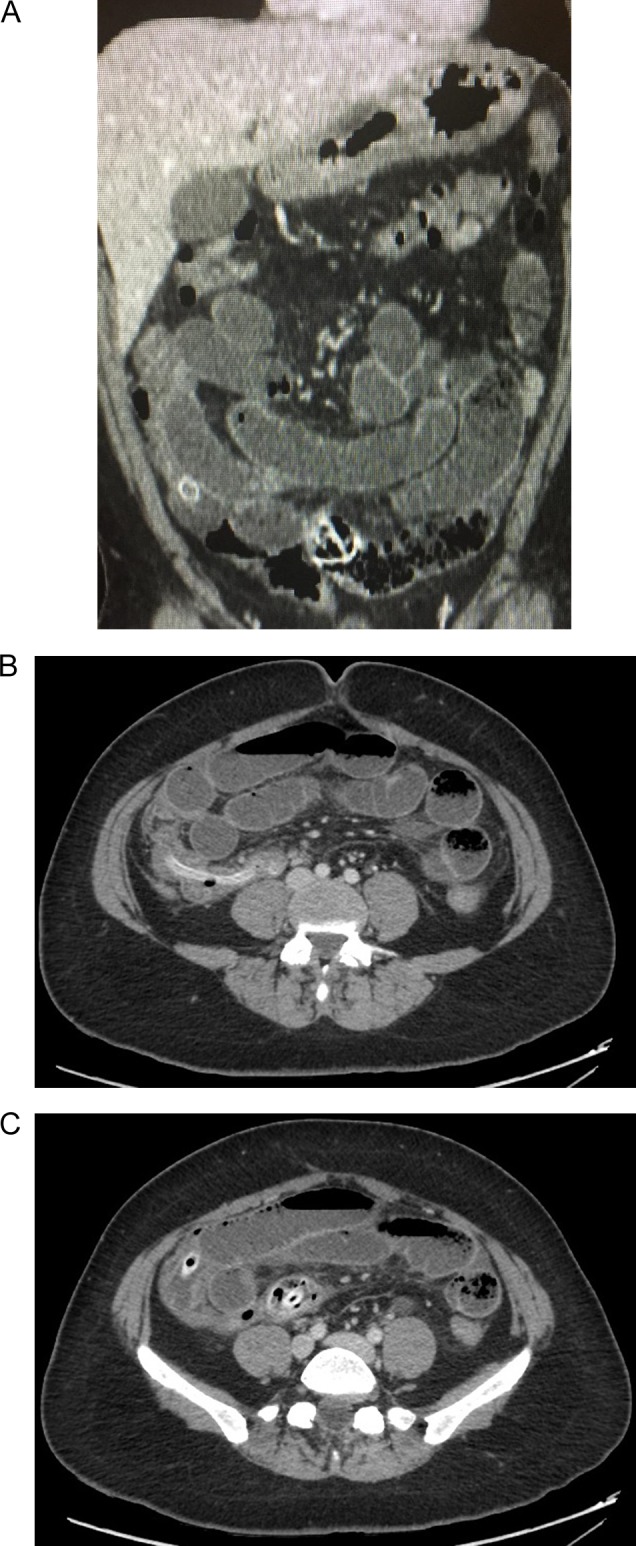
(A) Contrast-enhanced abdominal CT: intestinal loops are dilated. (B) Contrast-enhanced abdominal CT: a metallic foreign body is seen in the ileum. (C) Contrast-enhanced abdominal CT: showing clear signs of bowel obstruction.
Bowel obstruction due to the migration of the deflated intragastric balloon was suspected. Following a laparoscopic approach, the intestinal loops were dilated, and 100 ml of inflammatory fluid were noticed in the abdominal cavity. However, the definite site of obstruction could not be accessed (Fig. 2). Due to this, a laparotomy was decided. There was an important dilatation of all the loops of the small bowel, and the bowel walls were thickened but no perforation was detected. Near the ileocecal valve, a clear bulging of the bowel wall caused by the deflated impacted balloon was externally visible. A 3 cm transverse enterotomy was performed and the deflated gastric balloon was gently pulled out. The enterotomy was subsequently closed and the rest of the procedure was completed without complications (Fig. 3).
Figure 2:
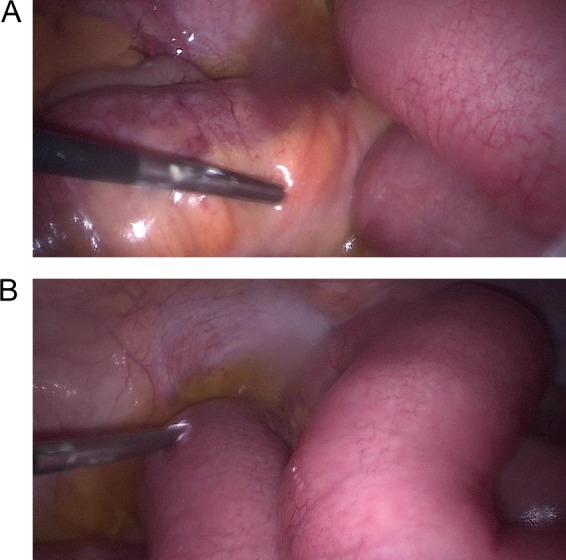
(A) Laparoscopy, showing dilated intestinal loops. (B) Laparoscopy, showing dilated intestinal loops and free inflammatory fluid.
Figure 3:
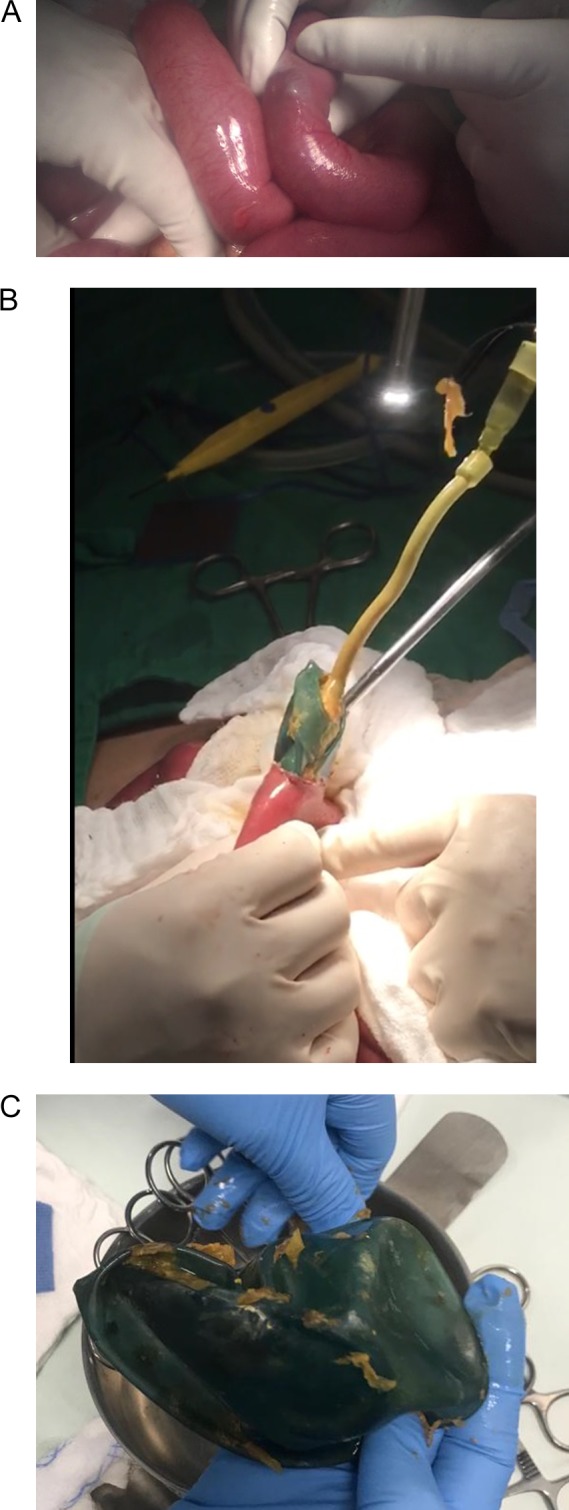
(A) Laparotomy, showing gastric balloon within the bowel. (B) Removal of the deflated gastric balloon. (C) Deflated gastric balloon.
The gastric balloon was completely deflated with a small tear in its wall, but the mechanism of rupture of the balloon is not known. However, it is clear that after the balloon deflated, and intestinal migration and subsequent obstruction occurred. The postoperative course of this patient was uneventful, the nasogastric tube was removed at the second postoperative day, and after observing good oral tolerance to sips of liquids, a full diet was started. She completed a 7-day antibiotic course and was discharged without complications. On follow-up controls, the patient shows signs of recovery.
DISCUSSION
Obesity is currently considered as a worldwide epidemic, with more than 1900 million adults over 18 years of age reported as overweight in 2016, where almost half were obese [1]. Currently, the only effective long-term intervention is bariatric surgery [2], with other treatment modalities including lifestyle changes, dietary modifications, and intragastric balloons [3]. Intragastric balloons have been in use since Nieben and Harboe [4] described them in 1982. They can achieve a weight reduction in obese patients who do not meet the criteria for bariatric surgery and thanks to its easy insertion, modification and removal, it remains a viable option for some patients [5], as was the case with our patient. These balloons are placed endoscopically in the stomach and then filled with either air, saline solution or methylene blue [2]. Their mechanism of action promotes weight loss as they increase the perception of fullness [5]. However, balloons can have adverse effects such as vomiting, electrolyte imbalances, abdominal pain, reflux symptoms, esophagitis and weight regain if no long-term lifestyle changes are adopted [3, 5, 6]. Other severe complications, such as gastric ulceration and perforation have also been reported, but they are fortunately rare (2.2%) [3, 4]. Intestinal obstruction is a quite rare complication of intragastric balloons and has been described in few case reports throughout the literature [3, 7]. They occur due to the migration of a partially deflated balloon through the bowel [3, 5], and this risk increases after the sixth month of treatment. For this reason, a close follow-up is crucial [8]. Diagnosis mostly occurs in an emergency setting, where abdominal X-ray imaging is usually used to confirm the diagnosis, but CT scans are also a helpful tool, especially when complications arise [9] such as in our case. After establishing the diagnosis, conservative treatment can be reasonable if the patient is stable as the deflated balloon can pass through the bowels without complications [6, 10]. Nonetheless, if the patient is unstable or the balloon has not passed in more than 48 h, surgical removal must be performed [6]. Laparoscopic or open approaches have been described with the same objective, to remove the foreign body without further injuring the bowel [6, 7]
In our case, based on the results of the CT scan and the clinical findings, surgery was decided upon and the balloon was successfully extracted. A multidisciplinary approach involving surgeons, nutritionists and psychologists are needed when approaching a bariatric patient. Like any kind of treatment, intragastric balloons have their benefits and their risks. Close follow-up and patient education on the risks and their identification is needed, as complications may arise at any moment. Prompt and accurate treatment could prevent life-threatening complications.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Bray G, Kim K, Wilding J. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev 2017;18:715–23. 10.1111/obr.12551. [DOI] [PubMed] [Google Scholar]
- 2. Tate C, Geliebter A. Intragastric balloon treatment for obesity: review of recent studies. Adv Ther 2017;34:1859–75. 10.1007/s12325-017-0562-3. [DOI] [PubMed] [Google Scholar]
- 3. Al Shammari N, Alshammari A, Alkandari M, Abdulsalam A. Migration of an intragastric balloon: a case report. Int J Surg Case Rep 2016;27:10–2. 10.1016/j.ijscr.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gyring Nieben O, Harboe H. Intragastric balloon as an artificial bezoar for treatment of obesity. Lancet 1982;319:198–9. 10.1016/s0140-6736(82)90762-0. [DOI] [PubMed] [Google Scholar]
- 5. Al-Momen A, El-Mogy I. Intragastric balloon for obesity: a retrospective evaluation of tolerance and efficacy. Obes Surg 2005;15:101–5. 10.1381/0960892052993558. [DOI] [PubMed] [Google Scholar]
- 6. Mousavi Naeini S, Sheikh M. Bowel obstruction due to migration of an intragastric balloon necessitating surgical removal before completion of the recommended 6 months. Case Rep Med 2012;2012:1–3. 10.1155/2012/414095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alsabah S, Al Haddad E, Ekrouf S, Almulla A, Al-Subaie S, Al Kendari M. The safety and efficacy of the procedureless intragastric balloon. Surg Obes Relat Dis 2018;14:311–7. 10.1016/j.soard.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 8. Di Saverio S, Bianchini Massoni C, Boschi S, Biscardi A, Tugnoli G, Masetti M, et al. Complete small-bowel obstruction from a migrated intra-gastric balloon: emergency laparoscopy for retrieval via enterotomy and intra-corporeal repair. Obes Surg 2014;24:1830–2. 10.1007/s11695-014-1271-5. [DOI] [PubMed] [Google Scholar]
- 9. Matar Z, Mohamed A, Abukhater M, Hussien M, Emran F, Bhat N. Small bowel obstruction due to air-filled intragastric balloon. Obes Surg 2009;19:1727–30. 10.1007/s11695-009-9880-0. [DOI] [PubMed] [Google Scholar]
- 10. Doldi S, Micheletto G, Perrini M, Librenti M, Rella S. Treatment of morbid obesity with intragastric balloon in association with diet. Obes Surg 2002;12:583–7. 10.1381/096089202762252398. [DOI] [PubMed] [Google Scholar]


