A recent editorial in Addiction, It is premature to expand access to medical cannabis in hopes of solving the US opioid crisis’, has correctly identified a number of limitations of previous ecological studies assessing the relationship between medical cannabis laws and state overdose rates [1]. The authors are primarily concerned with the validity of ecological studies, sentiments that have been shared previously [2,3].
The authors argue that evidence-derived ecological studies is inherently weak due to two fundamental weaknesses. The first is that ecological studies do not directly show that individual-level increases in marijuana use correspond with a decreased risk of opioid overdose. Using the evidence from state-level findings to make inferences at the individual level is the definition of ecological fallacy. This question requires data on individuals, which ecological studies lack. However, this Limitation does not preclude the use of ecological studies to assess state-level relationships.
There is nothing inherently wrong with ecological studies. Aside from a higher unit of analysis, ecological studies are no different from observational studies using individual-level data, In fact, both types of studies share the same strengths and weaknesses. Unfortunately for ecological studies, their limitations can easily be misinterpreted.
For example, the second cited weakness is that ecological studies have limited capacity to control for important differences in the characteristics of states with and without medical cannabis laws that are also associated with opioid overdose rates. This potential bias is not limited to ecological studies, however. Uncontrolled confounding is also present when comparing non-comparable groups of individuals. Fortunately, methods such as stratification can help to reduce these sources of bias.
To wit, months with high ice cream sales can be positively correlated with monthly rates of drownings (and yes, eating ice cream does not cause drownings). However, high ice cream sale units may be disproportionately represented by summer months (compared to low ice cream sales units), and summer months may be characterized by high rates of drownings. Stratifying by season may remove any crude association.
Ecological studies, while not perfect, generally take considerable care and effort to limit potential confounding. A comparison of overdose rates between California, a state with a medical cannabis law, and West Virginia, a state without, is as informative as comparing months with high versus low ice cream sales. Instead, most of these ecological studies use fixed effects for states, which is analogous to a ‘difference-in-difference’ design. With this method, the difference in outcome pre- versus post-exposure is contrasted to the difference that would be expected had the intervention not been implemented. This design requires different assumptions, as exposure groups are typically non-comparable prior to the intervention. The main assumptions are: (1) any group-variant attributes do not vary by time; and (2) any time-variant attributes do not vary by group. In other words, the validity of these studies relies on the assumption that differences between the two groups are stable over time and changes in exposure are not associated with changes in these differences. These twin claims are known as the ‘common trends assumption’. Identifying any factors that may violate this assumption is helpful in allowing for a selection of control states where these claims hold.
The authors are also concerned that a focus on expanding medical marijuana access to combat opioid overdose is displacing policies with ‘far better evidence’ at reducing opioid overdose deaths; namely, increasing access to opioid dependence treatment, reducing rates of imprisonment for opioid possession and increasing naloxone distribution. While these policies undoubtedly reduce opioid overdose deaths, they ignore a major cause underlying the epidemic: the rise in prescription opioids dispensed [4].
In fact, the mechanism behind the negative association between medical marijuana legislation and opioid overdose mortality may address this root cause: both in Medicaid and Medicare, states with medical marijuana legislation have lower rates of opioid prescribing [5,6]. Further, while the evidence regarding the analgesic efficacy of marijuana is modest, the evidence regarding the efficacy of opioids for chronic pain is no better [7]. Focusing on addressing the consequences of rampant overprescribing (e.g. methadone treatment and expanded naloxone access) could be displacing policies that may help to curb this epidemic.
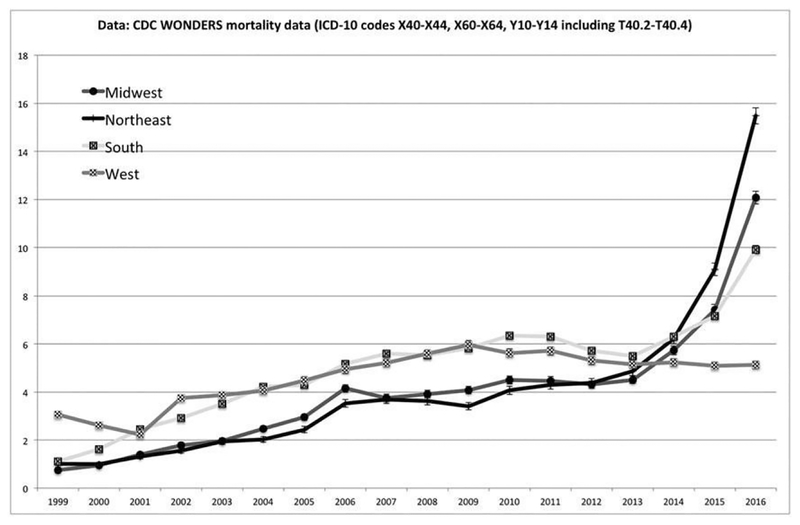
While ecological studies cannot tell us about individual-level substitution, it is evident from these studies that states with medical marijuana laws have a reduced rate of opioid overdose. In the West, a region characterized by liberal marijuana policies, age-adjusted opioid overdose rates have been declining since 2009 (Fig. 1). Well-designed studies have indicated that medical marijuana laws may be partially responsible for this decline. Future research should continue to investigate the mechanisms driving this association rather than dismissing the available evidence without proper cause.
Figure 1.
Regional trends in the age-adjusted opioid overdose mortality rate, 1999–2016
Acknowledgement
The study was supported by the National Institute on Drug Abuse (T32 DA007233B) through the Behavioral Science Training in Drug Abuse Research Training Program
Footnotes
Declaration of interests
None.
References
- 1.Hal W, West R, Marsden J, Humphreys K, Neale J, Petry N It is premature to expand access to medicinal cannabis in hopes of solving the US opioid crisis. Addiction 2018; 113: 987–8. [DOI] [PubMed] [Google Scholar]
- 2.Harris AH, Humphreys K, Finney JW State-level relationships cannot tell us anything about individuals. Am J Public Health 2015; 105: e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caputi TL, Sabet KA Population-level analyses cannot tell us anything about individual-level marijuana-opioid substitution. Am J Public Health 2018; 108: el2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Powell D, Pacula R, Taylor E How Increasing Medical Access to Opioids Contributes to the Opioid Epidemic: Evidence from Medicare Part D. Santa Monica, CA: RAND Corporation; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bradford AC, Bradford WD Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Aff (Millwood) 2016; 35:1230–6. [DOI] [PubMed] [Google Scholar]
- 6.Bradford AC, Bradford WD Medical marijuana laws may be associated with a decline in the number of prescriptions for Medicaid enrollees. Health Aff (Millwood) 2017; 36: 945–51. [DOI] [PubMed] [Google Scholar]
- 7.Krebs EE, Gravely A, Nugent S, Jensen AC, DeRonne B, Goldsmith ES et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: the space randomized clinical trial. JAMA 2018; 319: 872–82. [DOI] [PMC free article] [PubMed] [Google Scholar]