Abstract
Background:
While transient ischemic attack and minor stroke (TIAMS) are common conditions evaluated in the emergency department (ED), there is controversy regarding the most effective and efficient strategies for managing them in the ED. Some patients are discharged after evaluation in the ED and cared for in the outpatient setting, while others remain in an “observation unit” without being admitted or discharged, and others experience prolonged and potentially costly inpatient admissions.
Objective of the Review
The goal of this clinical review is to summarize and present recommendations regarding the disposition of TIAMS patients in the ED (e.g. admission versus discharge).
Discussion
An estimated 250,000–300,000 TIA events occur each year in the U.S, with an estimated near-term risk of subsequent stroke ranging from 3.5% to 10% at 2 days, rising to 17% by 90 days. While popular and easy to use, reliance solely on risk stratification tools such as the ABCD2 should not be used to determine if TIAMS patients can be safely discharged. Additional vascular imaging and advanced brain imaging done may improve prediction of short term neurologic risk. We also review various disposition strategies (e.g. inpatient versus outpatient/ED observation units) with regards to their association with neurological outcomes, such as 30 or 90-day stroke recurrence or new stroke, in addition to other outcomes such as hospital length of stay and healthcare costs.
Conclusion:
Discharge from the ED for rapid outpatient followup may be a safe and effective strategy for some forms of minor stroke without disabling deficit and TIA patients after careful evaluation and initial ED workup. Future research on such strategies has the potential to improve neurologic and overall patient outcomes, reduce hospital costs and ED length-of stay.
Keywords: TIA minor stroke, clinical review
Introduction
Stroke is the leading cause of serious disability and the fifth leading cause of death in the United States, with nearly 800,000 new cases annually.(1) The public health burden of stroke is high and is anticipated to increase dramatically by 2030.(2) Ischemic stroke makes up nearly 87% of all stroke.(3) One of the major precursors of ischemic stroke is a transient ischemic attack (TIA), defined as a “transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction”.(4) There are an estimated 250,000–300,000 TIA events occurring each year in the U.S., with a median survival of 8 years. The estimated near-term risk of subsequent stroke risk after TIA ranges from 3.5% to 10% at 2 days, rising to 17% by 90 days.(5)
TIA represents a significant healthcare burden in the emergency department (ED), with over 297,000 annual ED visits attributed to TIA in the United States,(6) nearly 200,000 total inpatient admissions (via the ED and outpatient direct admission), and annual associated healthcare costs totaling $2.6 billion.(1, 7) The number of patients with minor stroke has also grown considerably. While a consensus definition of “minor stroke” is lacking,(8) for the purpose of this paper we adopt a commonly used definition of stroke syndromes with nondisabling deficits and NIH stroke scale of ≤ 5).(9, 10) (11) In an analysis of the AHA Get with the Guidelines (GWTG) Stroke database, 7621 out of 33,995 patients (22.4%) arriving within 4.5 hours of symptom onset had an NIHSS of 5 or less.(12)
In approaching TIA and minor stroke (collectively referred to as TIAMS), it is appropriate to consider TIAMS together. For example, a brief episode of a focal neurological complaint that previously would have been classified as a TIA is now called a minor stroke if accompanied by abnormal findings on diffusion-weighted MRI sequences.(13) Recurrent stroke rates among patients with TIA are also very similar to those of patients with minor stroke.(14) From the stroke neurologist’s perspective, the duration of symptoms is often less important than the cause of the event and what can be done to prevent a recurrence.(15) Among minor stroke patients with non-disabling symptoms (e.g., isolated sensory loss, isolated facial droop, isolated dysarthria), moreover, it could be argued that the risks of thrombolytic therapy may outweigh potential benefits, and that such patients may be potentially treated conservatively, as are patients with TIA.(16) (10)
The ED is the primary clinical setting where TIAMS are frequently evaluated for the first time 12, and emergency clinicians play a critical role in the diagnosis and early management of TIAMS. While evidence-based guidelines for the emergency management of moderate to severe stroke are well-accepted within the medical community,(13, 14) there is less consensus regarding the optimal triage and management of TIAMS. Considering the potential risk of short-term (e.g. 30 or 90 day) mortality, or recurrent stroke after TIAMS,(15, 16) a key concern for treating physicians in the ED is the execution of a safe and appropriate disposition plan. While most studies agree that urgent and timely evaluation for TIAMS is warranted(17–19), variations in clinical practice exist between inpatient and outpatient disposition of patients with TIAMS.(20) Some patients are discharged after evaluation in the ED and cared for in the outpatient setting, others remain in an “observation unit” without being admitted or discharged, while others experience prolonged and potentially costly inpatient admissions.
Recent work by Edlow, along with a 2016 ACEP clinical policy on TIA provides an excellent overview of the approach to TIA evaluation and care in the ED. However questions remain regarding the ultimate disposition for these potentially high-risk patients.(21, 22) In addition, we expand on prior work by considering non-disabling minor strokes alongside TIA patients, and thus address the disposition of a larger population of ED patients. In this clinical review, we discuss current controversies regarding the management and disposition of patients with TIAMS presenting to the ED, namely whether such patients can be safely discharged home for urgent followup from the ED versus inpatient admission. We draw on data regarding the potential utility of common prediction tools, such as the ABCD and ABCD2 scores in helping to screen for such patients, and their association with near-term neurologic outcomes. We then summarize and describe previous studies on the safety and efficacy of different disposition approaches (e.g. hospital admission versus outpatient management, including ED observation unit management) for TIAMS patients evaluated in the ED, with regards to neurologic and overall patient outcomes.
Ultimately, our hope is by sharing our clinical review with the broader emergency medicine community, we may aid emergency clinicians and administrators in the safe and timely management of patients with TIAMS.
Weighing the Evidence for Discharging or Admitting TIAMS
Can we rely on risk stratification scores to guide ED disposition?
Several prediction scores have been developed using community and hospital based cohorts of TIA patients to determine which patients are at highest short-term risk for ischemic stroke and potentially which patients can safe for discharge.(23–27). Among the most commonly used prediction tools is the ABCD2 score, (24, 25, 28) which incorporates age, blood pressure, history of diabetes and clinical features of the event.(23, 24). Such scores are simple to use, do not require specialized skill to obtain;(23–25) and allow for easy scoring allowing the potential use of cut-point (e.g. score of ≥4), to identify high-risk patients who may require rapid diagnostic testing.(29)
Despite the advantages of its ease of use and simple interpretation, the utility of the ABCD2 score in helping guide admission versus discharge decisions for TIAMS is limited. Recommendations from the American Heart Association suggest that hospitalization may be reasonable for TIA patients with an ABCD2 score ≥3 presenting within 72 hours of symptoms, albeit with a low level of evidence (Class IIa recommendation, level C evidence).(4) However, the National Stroke Association does not endorse a specific cut-off in determining disposition.(30) Furthermore, following a systematic review of studies examining pretest probability for near term stroke risk in patients as assessed by the ABCD2, a clinical policy paper on TIA management in the ED by the American College of Emergency Physician concluded that adult patients with suspected TIA should not rely exclusively on screening instruments such as the ABCD2 in making decisions regarding admission or discharge from the ED(level B recommendation).(22) This conclusion was based in part on the concern that while the ABCD2 score accounts for history and symptoms, it excludes diagnostic test results that may identify the etiology and potential treatments of TIAMS. Approximately 20% of patients with ABCD2 scores <4 have high-risk conditions that require urgent treatment decisions, such as large artery atherosclerosis (LAA), which confers the highest risk of stroke recurrence and has the potential to be modified with early revascularization. (31–35) The ABCD2 score does not reliably distinguish among stroke subtypes,(36) and in patients with stroke attributable to LAA, a significant proportion of subsequent and recurrent strokes occur in patients who originally presented with low ABCD2 scores.(36–38) Thus, triage decisions based only on ABCD2, therefore, do not fully account for the cause or potential mechanism of ischemic injury, which largely determines the risk of recurrence following TIAMS.(39)
Considering the limitations of the ABCD2 score in identifying modifiable etiologies of ischemic stroke, and the fact that certain stroke mechanisms (such as large artery atherosclerosis or cardioembolism) have been associated with diffusion weighted imaging (DWI) positive lesions on brain magnetic resonance imaging (MRI), modified ABDC2 scores incorporating results of vascular or brain imaging, such as the ABCD3-I scores, have been developed. The ABCD3-I adds brain imaging, carotid imaging, and recurrent TIA to the traditional ABCD2 score,(40) assigning points for ipsilateral carotid stenosis of ≥50% (2 points), acute infarct on MRI (2 points), and “dual TIAs” (defined as two or more TIAs in the preceding 7 days, including the index event) (2 points). The 13-point ABCD3-I score improved prediction of recurrent stroke at 7 days compared with the ABCD2 score (C statistic for ABCD2 vs. ABCD3-I 0.54 vs. 0.61, p<.02). Th e ABCD3-I score does have several limitations for use in rapid triage, including few validation studies, as well as reliance on MRI and vessel imaging that may not be readily available in all EDs, or may result in prolonged ED evaluations, making widespread adoption of these approaches potentially challenging.(40–42) Ultimately, however, such strategies of integrating medical evaluation alongside diagnostic and vessel image may help identify TIAMS patients potentially safe for discharge from the ED.
Do we have to admit all TIAMS patients?
Given the significant near-term risk of recurrent cerebral ischemia in the first 24–72 hours following TIAMS,(16, 43) a broad consensus exists for the need for timely and expedited evaluation of TIAMS. A less clear consensus, however, exists around the care setting (such as inpatient or outpatient) in which the evaluation is conducted. Over the last decade, the overall proportion of inpatient admissions among patients presenting to the ED in the U.S. with TIA has risen from 70% to 91%.(44) Data from the National Emergency Department Sample found that 63.5% of patients presenting with a primary diagnosis of TIA to the ED were admitted from 2006–2008, compared to 36.5% that were discharged.(45) Multiple reasons have been proposed for the trend toward admission. Inpatient admission of patients with TIAMS may facilitate early and timely administration of thrombolytic therapy for recurrent cerebral ischemia following TIAMS, as well as the initiation of secondary prevention strategies specific to the underlying cause, theoretically making inpatient management of TIAMS both safer and more cost-effective. In a retrospective study of 1,687 TIA patients evaluated in the ED, factors associated with hospital admission in the 243 TIA patients that were admitted included atrial fibrillation, prior TIA, symptoms persisting on arrival to the ED, or persistent neurologic deficit.(39) In another study, the authors argued that the additional costs of inpatient hospitalization for TIA patients (estimated $588 net cost at a single academic site in Northern California) would be offset by the potential gains in quality of life from the rapid administration of thrombolysis and the reduction of long-term healthcare costs of untreated stroke.(46) However, the authors noted that other means of follow-up, including ED observation, could potentially be more cost-effective. For example, other research comparing rapid (24 hour) TIA clinic follow-up compared to inpatient admission found that in a cohort of TIA patients, hospitalization yielded only an added 0.00026 quality-adjusted life years at 1 year, with an additional cost of $5,573 per patient compared to urgent clinic evaluation, suggesting that hospitalization was not cost effective compared to rapid 24 hour TIA outpatient followup.(47)
A recent observational study of 8,540 patients with TIAMS either admitted or discharged from EDs in Canada showed that admitted patients were more likely to obtain recommended interventions (e.g. brain imaging, cardiac monitoring, secondary medication, etc.). The hazard of mortality in admitted patients was similar to that in discharged patients (adjusted hazard ratio [AHR] for admitted vs discharged patients 1.11; 95% confidence interval [CI] 0.92–1.34). Furthermore, in the subgroup of patients discharged from the ED, the adjusted hazard of mortality was 50% lower in those referred to stroke prevention clinics compared to those not referred (AHR 0.49; 95% CI 0.38– 0.64).(48)
A retrospective study reviewed 260 patients (176 admitted, 84 discharged; no significant difference in NIHSS scores between groups: chi-square p=.30) diagnosed with TIA in the ED to determine whether hospital admission improved 90-day readmission rates after TIA.(49) Of the 260 patients, 117 returned to the hospital within 90 days, 40% for neurologic reasons, and 11 (9%) ultimately were diagnosed with recurrent cerebrovascular events. Of the 117 patients that returned to the hospital, 58% had been admitted at their first ED encounter, suggesting that inpatient admission for TIA was not associated with a reduction in post-TIA outcomes such as 90-day readmission. Of note, the authors also found that patients who were evaluated in a specialized neurologic ED with emergency physicians with additional neurology training at the same institution had significantly lower inpatient admission rates for TIA compared to the main ED (35% versus 65%), as well as lower 90-day rehospitalization and stroke rates.(50)
Inpatient hospitalization of TIAMS may also potentially lead to the timely administration of secondary prevention strategies to reduce the risk of recurrent stroke. While several trials have examined both medical and surgical secondary prevention strategies after a stroke or TIA(51),(52),(53) in hospitalized patients, none of these strategies explicitly required hospital admission. For example, two studies carried out in Europe comparing expedited outpatient evaluation of all TIAs within 24 hours to delayed evaluation found a significant reduction in the risk of recurrent stroke in the intervention arm, a benefit that was felt to be driven by the detection and intervention on symptomatic extracranial internal carotid artery disease.(54, 55) These approaches relied on an infrastructure to rapidly identify large artery atherosclerosis, especially in the extracranial carotid artery, for which rapid and effective treatment is available.
Outpatient Management Strategies of TIAMS
There have been several prospective studies evaluating the utility and efficacy of rapid outpatient management strategies for TIA (and to a lesser degree, minor stroke). (see table 1).
Table 1:
Studies Evaluating Outpatient Management Strategies for TIA/minor stroke
| Study | Type of Study | Sample Size | Excluded Patients | Outcome | Findings |
|---|---|---|---|---|---|
| Early Use of Existing Strategies for Stroke (EXPRESS) Rothwell et al, 2007 |
Prospective Observational Pre-post |
1278 (644 post) | -None (all TIA or stroke patients included in study) | 90-day stroke risk | 90-day stroke Rate of 2.1% compared to 10.3% before implementation |
| SOS-TIA Lavellée, 2013 |
Prospective Observational | 1085 | -persistent symptoms - |
90-day stroke risk | 90-day stroke risk of 1.24% |
| Ross et al. 2007 | Randomized Control Trial | 149 | -persistent neurologic deficit -existing condition prohibiting reliable ED testing and outpatient follow-up |
90-day stroke risk, length of stay 90-day total direct costs Return Visit Major Clinical Event |
Lower 90-day total direct costs ($890 vs $1547) Shorter length of stay (26 v 61 hours) 12% return visits in both groups 4 major clinical events in both groups |
| Stead et al. 2009 | Prospective Observational | 418 | -Patients with symptoms lasting >24 hours -acute ischemic/hemorrhagic stroke |
48-hour and 7-day stroke risk | Risk of stroke of 0.96% at 48 hours and 1.2% at 7 days |
The UK-based Early Use of Existing Strategies for Stroke (EXPRESS) study sought to ascertain the effect on 90-day recurrent stroke risk of implementation of a rapid-access TIA clinic that included diagnostic testing (e.g. head CT, vascular ultrasound, EKG) and treatment initiation of secondary preventive measures (including antiplatelet and antihypertensive agents). (55) In the initial phase of the study, before implementation of the TIA clinic, the rate of stroke at 90 days was 10.3% (32/210 patients). After implementation, the stroke rate decreased to 2.1% (6/281 patients, P<.0001). Another study based around an outpatient clinic in France (SOS-TIA) followed 1,085 patients who presented with symptoms of a TIA and were referred to a specialized outpatient neurology clinic with access to vascular neurologists and diagnostic imaging (e.g. MRI/CT, ultrasound, and EKG) over 2 years.(54) Patients were discharged to home and treated as outpatients unless one or more specific conditions were met (increasing TIA frequency, duration, or severity, abnormal cardiac rhythm, high-grade stenosis, potential cardiac source of recurrent embolism). The 1,085 patients with suspected TIA were followed up for a median of 16 months and had a 90-day stroke rate of 1.24%, as compared with a predicted stroke rate of approximately 6% as estimated by ABCD2 score. The 1-year rate of myocardial infarction and non-stroke vascular death (both 1.1%) were also lower than annual risks for myocardial infarction (2.2%) and non-stroke vascular death (2.1%) based on previous studies.(56)
In the United States, ED observation and neurology observation units based in the ED have been developed in certain hospitals as an alternative to inpatient hospitalization for the expedited evaluation of TIA and minor stroke.(57, 58) Similar approaches using an outpatient/ED observation approach for patients with low to intermediate risk of acute coronary events(59) found that observation stays were associated with decreased length of stay and cost, while improving patient safety outcomes, and patient satisfaction.(60, 61) A prospective, randomized control study evaluated outcomes in 149 ED patients with TIA, randomized to either inpatient admission or ED observation stay for rapid diagnostic testing and imaging (e.g. vessel imaging, echocardiography).(62) Patients in both groups of the study had normal non-contrast CT head imaging, EKG, and laboratory studies; all participants received a neurology consultation, carotid vessel imaging (e.g. ultrasound), echocardiography, and cardiac monitoring. The ED observation group patients with positive testing results (e.g. carotid imaging suggestive of severe stenosis, evidence of thromboembolic source) were admitted. Compared to the inpatient group, patients in the ED observation group had shorter total lengths of stay (mean 26 vs. 61 hours), lower 90-day total direct costs ($890 vs. $1,547), and comparable 90-day clinical outcomes. Another prospective study of 418 ED patients with TIA evaluated in an ED observation unit found that patients treated in the observation unit had a risk of stroke of 0.96% at 48 hours and 1.2% at 7 days,(57) which was lower compared to the estimated overall risk of stroke estimated at 3.1% at 48 hours and 5.8% at 7 days in a systematic review and meta-analysis.(63) Further studies have shown that the use of ED observation units for the management of TIA is also associated with a reduction in length of stay and costs of treatment, as well as similar degree of adoption of secondary prevention medication strategies in comparison to patients who had been admitted for TIA.(58) (57–63)
Disposition of Patients with TIAMS: Summarizing the Evidence
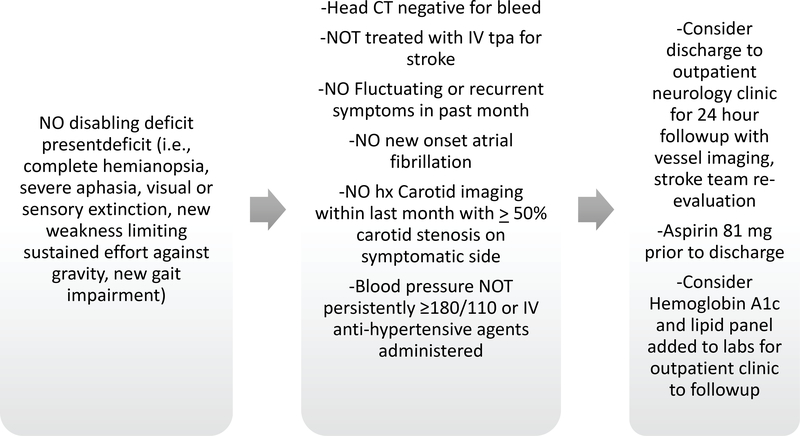
Current National Stroke Association TIA guidelines recommend that hospitalization be “considered” for patients presenting with a first TIA within the past 24 to 48 hours; hospitalization is “generally recommended” for patients with crescendo TIAs, duration of symptoms greater than 1 hour, symptomatic carotid stenosis greater than 50%, a known cardiac source of embolus, or a known hypercoagulable state. (64) Regardless of inpatient versus outpatient management of TIAMS, National Stroke Association guidelines recommend “timely” brain and vascular imaging, as assessed in follow-up, although no specific timeframe is defined.(64, 65) Our review of the literature suggests that while current TIAMS risk prediction schemes are promising in their potential to predict near-term adverse neurologic events, significant limitations (e.g., inability to address etiology of symptoms, inconsistent risk stratification) constrain their ability to guide TIAMS management without additional monitoring and diagnostic studies. Furthermore, indiscriminate admission of all patients with suspected TIAMS is likely to be costlier than outpatient evaluation, without a clear benefit in terms of patient outcomes. An initial evaluation approach focused on identifying those at highest risk for recurrent stroke based on diagnostic testing rather than based on symptoms is likely to identify those who stand the most to benefit from admission vs. discharge to rapid followup (see Figure 1). For example, a patient with short-lived dizziness due to cardioembolism to the posterior circulation from undiagnosed atrial fibrillation may have a higher risk of recurrence than a patient with resolved asymmetric weakness secondary to less than 50% internal carotid artery stenosis. Finally, recent studies have supported the notion that dedicated rapid outpatient neurology follow-up clinics or ED observation protocols may reduce overall length of stays and nosocomial risks, while improving patient satisfaction and neurologic outcomes.(66, 67) ED overcrowding has been associated with multiple negative outcomes, including delayed time to treatment in stroke,(68) patient dissatisfaction,(69) unfavorable perception of clinician-patient communication,(70, 71) and the development of adverse psychological effects such as post-traumatic stress disorder (PTSD) in stroke survivors, which is associated with increased morbidity and mortality.(71–75) The timely and safe disposition from the ED of TIAMS patients may reduce ED overcrowding, enhance the patient’s experience of their ED visit, and improve their overall neurologic outcomes.
Figure 1:
TIA/Minor Stroke Evaluation Pathway
In summary, while the evidence in support of ED observation protocols and specialized stroke observation units suggest that some TIAMS may be considered for discharge after ED evaluation, further rigorous study is needed to evaluate more closely the efficacy of such interventions in these population of patients. Future work evaluating strategies such as shared decision making and coordination with outpatient primary care providers may help complement the ongoing efforts in the ED. Additionally, given that broad availability is currently limited for such specialized neurologic observation units, strategies are needed to help guide admission versus discharge approaches in the settings where no such units are available. Future prospective cohort and randomized trials evaluating the safety and utility of rapid outpatient/ED observation strategies versus inpatient admission may guide the development of approaches to the management of TIAMS in the ED that improve both primary and secondary outcomes.
Conclusions
TIAMS are common conditions evaluated in the ED and are associated with significant morbidity and mortality. The management of such patients in the ED should emphasize timely and safe comprehensive evaluation. Strategies aimed at identifying TIAMS patients who would benefit from ED observation or rapid outpatient follow-up rather than inpatient admission have the potential to not only improve patient neurologic outcomes, but also to reduce hospital costs and ED length-of stay. Future research evaluating the potential effectiveness of such strategies is critical and may improve both general stroke knowledge and care for TIAMS in the acute setting.
Article Summary.
1). Why is this topic important?
Transient ischemic attack (TIA) and minor stroke are common conditions evaluated in the emergency department (ED). The most effective and efficient strategies for managing them in the ED remain undefined.
2). What does this clinical review attempt to show?
Rapid outpatient care and followup may be a safe and effective management strategy for some minor stroke patients without disabling deficit and TIA patients after focused ED evaluation.
3). What are the key findings?
While risk prediction schemes such as the ABCD2 score have been validated in observational studies as predictors of short-term risk for stroke in the ED they should not be used in isolation to determine discharge from the ED. The addition of brain/vascular imaging may help identify etiologic factors of TIA and minor stroke. Several prospective studies evaluating the efficacy of rapid outpatient management strategies for TIA and minor stroke have found such ED observation/outpatient strategies associated with shorter total lengths of stay, lower 90-day total direct costs, and comparable 90-day clinical outcomes.
4). How is patient care impacted?
Future research evaluating the safety and utility of rapid outpatient/ED observation strategies for TIA and minor stroke may improve primary and secondary stroke outcomes.
Acknowledgments
Grant: BC is supported by a mentored career development grant by the National Institute of Health/NCAT (KL2 TRANSFORM: KL2TR0001874) and the NY Empire Clinical Research Investigator Program. EM is supported by a NIH/NINDS StrokeNet Training Fellowship.
Footnotes
Meetings: None
Contributor Information
Bernard P. Chang, 622 West 168th Street, Department of Emergency Medicine, VC 2nd Floor Suite 260, New York, NY 10032, 212-305-2995
Sara Rostanki, Department of Neurology, 240 38th St, New York, NY 10016
Joshua Willey, 710 West 168th St, Department of Neurology, New York, NY 10032
Benjamin Kummer, 710 West 168th St, Department of Neurology, New York, NY 10032
Eliza Miller, 710 West 168th St, Department of Neurology, New York, NY 10032,
Mitchell Elkind, 710 West 168th St, Department of Neurology, New York, NY 10032
References:
- [1].Mozaffarian D, Benjamin EJ, Go AS, et al. Executive summary: Heart Disease and Stroke Statistics-2016 update: A report from the American Heart Association. Circulation. 2016;133:447. [DOI] [PubMed] [Google Scholar]
- [2].Ovbiagele B, Goldstein LB, Higashida RT, et al. Forecasting the future of stroke in the united states. Stroke; a journal of cerebral circulation. 2013;44:2361–75. [DOI] [PubMed] [Google Scholar]
- [3].Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. Circulation. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke; a journal of cerebral circulation. 2009;40:2276–93. [DOI] [PubMed] [Google Scholar]
- [5].Wu CM, McLaughlin K, Lorenzetti DL, Hill MD, Manns BJ, Ghali WA. Early risk of stroke after transient ischemic attack: a systematic review and meta-analysis. Archives of internal medicine. 2007;167:2417–22. [DOI] [PubMed] [Google Scholar]
- [6].Edlow JA, Kim S, Pelletier AJ, Camargo CA Jr. National study on emergency department visits for transient ischemic attack, 1992–2001. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2006;13:666–72. [DOI] [PubMed] [Google Scholar]
- [7].Tong X, George MG, Gillespie C, Merritt RK. Trends in Hospitalizations and Cost Associated with Acute Ischemic Stroke by Age, United States 2003–2012. Am Heart Assoc; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Fischer U, Baumgartner A, Arnold M, et al. What is a minor stroke? Stroke; a journal of cerebral circulation. 2010;41:661–6. [DOI] [PubMed] [Google Scholar]
- [9].Park TH, Hong KS, Choi JC, et al. Validation of minor stroke definitions for thrombolysis decision making. Journal of stroke and cerebrovascular diseases : the official journal of National Stroke Association. 2013;22:482–90. [DOI] [PubMed] [Google Scholar]
- [10].Demaerschalk BM, Kleindorfer DO, Adeoye OM, et al. Scientific Rationale for the Inclusion and Exclusion Criteria for Intravenous Alteplase in Acute Ischemic Stroke: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke; a journal of cerebral circulation. 2016;47:581–641. [DOI] [PubMed] [Google Scholar]
- [11].Khatri P, Kleindorfer DO, Yeatts SD, et al. Strokes with minor symptoms: an exploratory analysis of the National Institute of Neurological Disorders and Stroke recombinant tissue plasminogen activator trials. Stroke; a journal of cerebral circulation. 2010;41:2581–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Romano JG, Smith EE, Liang L, et al. Outcomes in mild acute ischemic stroke treated with intravenous thrombolysis: a retrospective analysis of the Get With the Guidelines–Stroke registry. JAMA neurology. 2015;72:423–31. [DOI] [PubMed] [Google Scholar]
- [13].Price CI, Clement F, Gray J, Donaldson C, Ford GA. Systematic review of stroke thrombolysis service configuration. Expert review of neurotherapeutics. 2009;9:211–33. [DOI] [PubMed] [Google Scholar]
- [14].Gorelick PB. Primary and comprehensive stroke centers: history, value and certification criteria. J Stroke. 2013;15:78–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kleindorfer D, Panagos P, Pancioli A, et al. Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke; a journal of cerebral circulation. 2005;36:720–3. [DOI] [PubMed] [Google Scholar]
- [16].Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. Jama. 2000;284:2901–6. [DOI] [PubMed] [Google Scholar]
- [17].Sulter G, Elting JW, Langedijk M, Maurits NM, De Keyser J. Admitting acute ischemic stroke patients to a stroke care monitoring unit versus a conventional stroke unit. Stroke; a journal of cerebral circulation. 2003;34:101–4. [DOI] [PubMed] [Google Scholar]
- [18].Candelise L, Gattinoni M, Bersano A, et al. Stroke-unit care for acute stroke patients: an observational follow-up study. The Lancet. 2007;369:299–305. [DOI] [PubMed] [Google Scholar]
- [19].Brady BK, McGahan L, Skidmore B. Systematic review of economic evidence on stroke rehabilitation services. International journal of technology assessment in health care. 2005;21:15–21. [DOI] [PubMed] [Google Scholar]
- [20].Coben JH, Owens PL, Steiner CA, Crocco TJ. Hospital and demographic influences on the disposition of transient ischemic attack. Academic Emergency Medicine. 2008;15:171–6. [DOI] [PubMed] [Google Scholar]
- [21].Edlow JA. Managing Patients With Transient Ischemic Attack. Annals of Emergency Medicine. 2017. [DOI] [PubMed] [Google Scholar]
- [22].Brown MD, Byyny R, Diercks DB, et al. Clinical policy: critical issues in the evaluation of adult patients with suspected transient ischemic attack in the emergency department. Annals of emergency medicine. 2016;68:354–70. e29. [DOI] [PubMed] [Google Scholar]
- [23].Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. Jama. 2000;284:2901–6. [DOI] [PubMed] [Google Scholar]
- [24].Rothwell PM, Giles MF, Flossmann E, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005;366:29–36. [DOI] [PubMed] [Google Scholar]
- [25].Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369:283–92. [DOI] [PubMed] [Google Scholar]
- [26].Giles MF, Albers GW, Amarenco P, et al. Addition of brain infarction to the ABCD2 Score (ABCD2I): a collaborative analysis of unpublished data on 4574 patients. Stroke. 2010;41:1907–13. [DOI] [PubMed] [Google Scholar]
- [27].Merwick A, Albers GW, Amarenco P, et al. Addition of brain and carotid imaging to the ABCD(2) score to identify patients at early risk of stroke after transient ischaemic attack: a multicentre observational study. The Lancet Neurology. 2010;9:1060–9. [DOI] [PubMed] [Google Scholar]
- [28].Josephson SA, Sidney S, Pham TN, Bernstein AL, Johnston SC. Higher ABCD2 score predicts patients most likely to have true transient ischemic attack. Stroke; a journal of cerebral circulation. 2008;39:3096–8. [DOI] [PubMed] [Google Scholar]
- [29].(NICE). NIfHaCE. Stroke: The Diagnosis and Acute Management of Stroke and Transient Ischemic Attacks. London: National Institute for Health and Clinical Excellence; 2008. [Google Scholar]
- [30].Johnston SC, Albers GW, Gorelick PB, et al. National Stroke Association recommendations for systems of care for transient ischemic attack. Annals of neurology. 2011;69:872–7. [DOI] [PubMed] [Google Scholar]
- [31].Purroy F, Montaner J, Molina CA, Delgado P, Ribo M, Alvarez-Sabin J. Patterns and predictors of early risk of recurrence after transient ischemic attack with respect to etiologic subtypes. Stroke; a journal of cerebral circulation. 2007;38:3225–9. [DOI] [PubMed] [Google Scholar]
- [32].Amarenco P, Lavallee PC, Labreuche J, et al. One-Year Risk of Stroke after Transient Ischemic Attack or Minor Stroke. The New England journal of medicine. 2016;374:1533–42. [DOI] [PubMed] [Google Scholar]
- [33].Coutts SB, Simon JE, Eliasziw M, et al. Triaging transient ischemic attack and minor stroke patients using acute magnetic resonance imaging. Annals of neurology. 2005;57:848–54. [DOI] [PubMed] [Google Scholar]
- [34].Yaghi S, Rostanski SK, Boehme AK, et al. Imaging Parameters and Recurrent Cerebrovascular Events in Patients With Minor Stroke or Transient Ischemic Attack. JAMA neurology. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Calvet D, Touze E, Oppenheim C, Turc G, Meder JF, Mas JL. DWI lesions and TIA etiology improve the prediction of stroke after TIA. Stroke. 2009;40:187–92. [DOI] [PubMed] [Google Scholar]
- [36].Sheehan OC, Kyne L, Kelly LA, et al. Population-based study of ABCD2 score, carotid stenosis, and atrial fibrillation for early stroke prediction after transient ischemic attack: the North Dublin TIA study. Stroke. 2010;41:844–50. [DOI] [PubMed] [Google Scholar]
- [37].Walker J, Isherwood J, Eveson D, Naylor AR. Triaging TIA/minor stroke patients using the ABCD2 score does not predict those with significant carotid disease. European journal of vascular and endovascular surgery : the official journal of the European Society for Vascular Surgery. 2012;43:495–8. [DOI] [PubMed] [Google Scholar]
- [38].Koton S, Rothwell PM. Performance of the ABCD and ABCD2 scores in TIA patients with carotid stenosis and atrial fibrillation. Cerebrovascular diseases (Basel, Switzerland). 2007;24:231–5. [DOI] [PubMed] [Google Scholar]
- [39].Josephson SA, Sidney S, Pham TN, Bernstein AL, Johnston SC. Factors associated with the decision to hospitalize patients after transient ischemic attack before publication of prediction rules. Stroke; a journal of cerebral circulation. 2008;39:411–3. [DOI] [PubMed] [Google Scholar]
- [40].Song B, Fang H, Zhao L, et al. Validation of the ABCD3-I score to predict stroke risk after transient ischemic attack. Stroke; a journal of cerebral circulation. 2013;44:1244–8. [DOI] [PubMed] [Google Scholar]
- [41].Kiyohara T, Kamouchi M, Kumai Y, et al. ABCD3 and ABCD3-I scores are superior to ABCD2 score in the prediction of short- and long-term risks of stroke after transient ischemic attack. Stroke. 2014;45:418–25. [DOI] [PubMed] [Google Scholar]
- [42].Purroy F, Jimenez-Caballero PE, Mauri-Capdevila G, et al. Predictive value of brain and vascular imaging including intracranial vessels in transient ischaemic attack patients: external validation of the ABCD3-I score. European journal of neurology. 2013;20:1088–93. [DOI] [PubMed] [Google Scholar]
- [43].Panagos PD. Transient ischemic attack (TIA): the initial diagnostic and therapeutic dilemma. The American journal of emergency medicine. 2012;30:794–9. [DOI] [PubMed] [Google Scholar]
- [44].Durrani-Tariq S, Eskin B, Allegra JR. Admission rates of ED patients with transient ischemic attack have increased since 2000. The American journal of emergency medicine. 2013;31:1349–51. [DOI] [PubMed] [Google Scholar]
- [45].Chaudhry SA, Tariq N, Majidi S, et al. Rates and factors associated with admission in patients presenting to the ED with TIA in the United States—2006 to 2008. The American journal of emergency medicine. 2013;31:516–9. [DOI] [PubMed] [Google Scholar]
- [46].Nguyen-Huynh MN, Johnston SC. Is hospitalization after TIA cost-effective on the basis of treatment with tPA? Neurology. 2005;65:1799–801. [DOI] [PubMed] [Google Scholar]
- [47].Joshi JK, Ouyang B, Prabhakaran S. Should TIA patients be hospitalized or referred to a same-day clinic? A decision analysis. Neurology. 2011;77:2082–8. [DOI] [PubMed] [Google Scholar]
- [48].Kapral MK, Hall R, Fang J, et al. Association between hospitalization and care after transient ischemic attack or minor stroke. Neurology. 2016;86:1582–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Lesenskyj AM, Maxwell CR, Veznedaroglu E, Liebman K, Hakma Z, Binning MJ. An Analysis of Transient Ischemic Attack Practices: Does Hospital Admission Improve Patient Outcomes? Journal of Stroke and Cerebrovascular Diseases. 2016;25:2122–5. [DOI] [PubMed] [Google Scholar]
- [50].Greenberg K, Maxwell CR, Moore KD, et al. Improved door-to-needle times and neurologic outcomes when IV tissue plasminogen activator is administered by emergency physicians with advanced neuroscience training. The American journal of emergency medicine. 2015;33:234–7. [DOI] [PubMed] [Google Scholar]
- [51].Chen Z, Sandercock P, Pan H, et al. Indications for early aspirin use in acute ischemic stroke. Stroke; a journal of cerebral circulation. 2000;31:1240–9. [DOI] [PubMed] [Google Scholar]
- [52].Amarenco P, Labreuche J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. The Lancet Neurology. 2009;8:453–63. [DOI] [PubMed] [Google Scholar]
- [53].Kastrup A, Gröschel K, Krapf H, Brehm BR, Dichgans J, Schulz JB. Early outcome of carotid angioplasty and stenting with and without cerebral protection devices. Stroke; a journal of cerebral circulation. 2003;34:813–9. [DOI] [PubMed] [Google Scholar]
- [54].Lavallée P, Amarenco P. TIA clinic: a major advance in management of transient ischemic attacks. TIA as Acute Cerebrovascular Syndrome: Karger Publishers; 2013. p. 30–40. [DOI] [PubMed] [Google Scholar]
- [55].Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. The Lancet. 2007;370:1432–42. [DOI] [PubMed] [Google Scholar]
- [56].Touzé E, Varenne O, Chatellier G, Peyrard S, Rothwell PM, Mas J-L. Risk of myocardial infarction and vascular death after transient ischemic attack and ischemic stroke. Stroke; a journal of cerebral circulation. 2005;36:2748–55. [DOI] [PubMed] [Google Scholar]
- [57].Stead LG, Bellolio MF, Suravaram S, et al. Evaluation of transient ischemic attack in an emergency department observation unit. Neurocritical care. 2009;10:204. [DOI] [PubMed] [Google Scholar]
- [58].Nahab F, Leach G, Kingston C, et al. Impact of an emergency department observation unit transient ischemic attack protocol on length of stay and cost. Journal of Stroke and Cerebrovascular Diseases. 2012;21:673–8. [DOI] [PubMed] [Google Scholar]
- [59].Roberts RR, Zalenski RJ, Mensah EK, et al. Costs of an Emergency Department—Based Accelerated Diagnostic Protocol vs Hospitalization in Patients With Chest Pain: A Randomized Controlled Trial. Jama. 1997;278:1670–6. [PubMed] [Google Scholar]
- [60].Rydman RJ, Zalenski RJ, Roberts RR, et al. Patient satisfaction with an emergency department chest pain observation unit. Annals of emergency medicine. 1997;29:109–15. [DOI] [PubMed] [Google Scholar]
- [61].Gomez MA, Anderson JL, Karagounis LA, Muhlestein JB, Mooders FB, Group RS. An emergency department-based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). Journal of the American College of Cardiology. 1996;28:25–33. [DOI] [PubMed] [Google Scholar]
- [62].Ross MA, Compton S, Medado P, Fitzgerald M, Kilanowski P, O’Neil BJ. An emergency department diagnostic protocol for patients with transient ischemic attack: a randomized controlled trial. Annals of emergency medicine. 2007;50:109–19. [DOI] [PubMed] [Google Scholar]
- [63].Giles MF, Rothwell PM. Risk of stroke early after transient ischaemic attack: a systematic review and meta-analysis. The Lancet Neurology. 2007;6:1063–72. [DOI] [PubMed] [Google Scholar]
- [64].Johnston SC, Nguyen‐Huynh MN, Schwarz ME, et al. National Stroke Association guidelines for the management of transient ischemic attacks. Annals of neurology. 2006;60:301–13. [DOI] [PubMed] [Google Scholar]
- [65].Adams HP, Del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke. Circulation. 2007;115:e478–e534. [DOI] [PubMed] [Google Scholar]
- [66].Rudd AG, Wolfe CD, Tilling K, Beech R. Randomised controlled trial to evaluate early discharge scheme for patients with stroke. Bmj. 1997;315:1039–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. The Lancet Neurology. 2009;8:235–43. [DOI] [PubMed] [Google Scholar]
- [68].Chatterjee P, Cucchiara BL, Lazarciuc N, Shofer FS, Pines JM. Emergency department crowding and time to care in patients with acute stroke. Stroke; a journal of cerebral circulation. 2011;42:1074–80. [DOI] [PubMed] [Google Scholar]
- [69].Pines JM, Iyer S, Disbot M, Hollander JE, Shofer FS, Datner EM. The effect of emergency department crowding on patient satisfaction for admitted patients. Academic Emergency Medicine. 2008;15:825–31. [DOI] [PubMed] [Google Scholar]
- [70].Chang BP, Sumner JA, Haerizadeh M, Carter E, Edmondson D. Perceived clinician-patient communication in the emergency department and subsequent post-traumatic stress symptoms in patients evaluated for acute coronary syndrome. Emergency medicine journal : EMJ. 2016;33:626–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Chang BP, Carter E, Suh EH, Kronish IM, Edmondson D. Patient treatment in ED hallways and patient perception of clinician-patient communication. The American journal of emergency medicine. 2016;34:1163–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Edmondson D An Enduring Somatic Threat Model of Posttraumatic Stress Disorder Due to Acute Life-Threatening Medical Events. Social and personality psychology compass. 2014;8:118–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Sundquist K, Chang BP, Parsons F, Dalrymple N, Edmondson D, Sumner JA. Treatment rates for PTSD and depression in recently hospitalized cardiac patients. Journal of psychosomatic research. 2016;86:60–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].White M, Edmondson D, Umland R, Sanchez G, Chang BP. Patient perceptions of stress during evaluation for acute coronary syndrome in the emergency department. The American journal of emergency medicine. 2016. [Google Scholar]
- [75].Homma K, Chang B, Shaffer J, et al. Association of social support during emergency department evaluation for acute coronary syndrome with subsequent posttraumatic stress symptoms. Journal of behavioral medicine. 2016;39:823–31. [DOI] [PMC free article] [PubMed] [Google Scholar]